Abstract
Objective:
To compare the efficacy and safety with a fixed dose of two parenteral iron preparations, iron sucrose complex and iron sorbitol citric acid as per the current practice.
Materials and Methods:
A prospective randomized open label study was conducted. In this study, 60 pregnant women with hemoglobin less than 8.5 g/dl received a fixed dose of either IV iron sucrose or IM iron sorbitol citric acid therapy. The efficacy of the therapy was assessed by laboratory parameters such as hemoglobin, hematocrit, MCV, MCH, and serum ferritin level after 14 and 28 days. To assess the safety, adverse drug reactions with both the therapies were recorded.
Results:
Hemoglobin concentration increased significantly (P < 0.001) with respect to time in both the groups. The rise in the hemoglobin level in third and fourth weeks was significantly higher in iron sucrose (0.92 g/dl) than iron sorbitol citric acid therapy (0.56 g/dl). There was no significant change in the rise of the serum ferritin level after both the therapies. Adverse events were common with iron sorbitol citric acid therapy. However, no serious adverse drug reactions were observed.
Conclusions:
No significant difference in the efficacy of both of the therapy. However, adverse events and dropout rates were much more common in the group of pregnant women who received iron sorbitol citric acid.
Keywords: Iron deficiency anemia, iron sucrose therapy, iron sorbitol citric acid therapy, pregnancy
INTRODUCTION
Anemia is widely prevalent in developing countries like India and the most common affected group is pregnant women with an estimate of nearly two-thirds of all pregnant women.[1] The main cause of anemia in pregnancy is found out to be iron deficiency, i.e. about 95%.[2] Because of that, iron deficiency anemia remains a major public health problem today in developing countries like India. In pregnancy, iron deficiency is exaggerated because of the ability of foetus to extract its requirement in obligatory direction, from a mother whose body iron levels are already depleted. Iron absorption may be adequate in healthy, iron-replete women. However, it is far below the iron requirement of an iron depleted or deficient pregnant women.[3,4] Therefore, more amount of iron, exceeding the daily requirement, is to be supplemented. This is aggravated by the adverse effect of pregnancy on the gastrointestinal tract which includes nausea and vomiting, motility disorder with reflux esophagitis, indigestion, constipation, and tendency to develop hemorrhoids.[5] These factors increase the severity of anemia. Therefore, anemia is a major contributory factor for maternal and fetal morbidity as well as mortality in developing countries like India.[6,7]
The first choice in the treatment of iron deficiency anemia for the majority of patients is the oral iron replacement therapy which is easily available at all peripheral health centers and subcenters. However, parenteral iron therapy is often required in many pregnant women. Situations like failure of oral iron therapy or increased demands in spite of regular oral iron therapy often necessitate parenteral iron therapy in anemic pregnant women. Iron dextran and iron sorbitol citric acid are widely used parenteral iron preparations since long time. However, threat of unpredictable anaphylactic reaction by these conventional parenteral iron preparations prevented their wide use. Some of the studies show that new parenteral iron preparation, iron sucrose, is safe and effective for the management of anemia and can administer without a test dose.[8–10] It suggests that it can be given at most peripheral health centers even with minimum facilities.
Routinely, the parenteral iron therapy is given as calculated total dose therapy. For that, multiple injections of iron sorbitol citric acid are required in a month, which is a common factor of decrease in compliance of recipients. Iron sucrose can be given as a single large dose infusion without any side effect. Iron sucrose is costlier preparation as compared to other preparations. These are the main reasons which are the hurdles of parenteral iron therapy in developing countries.
To overcome this, current practice is to give parenteral iron in a predefined fixed dose followed by oral or parenteral iron therapy according to the severity of anemia. This has shown to increase the compliance as well as decrease the economic burden on the pregnant women in rural areas.
Therefore, this study was aimed at comparing the efficacy and safety with a fixed dose of two parenteral iron preparations, iron sucrose complex (intravenous route) and iron sorbitol citric acid (intramuscular route), as per the current practice in this area.
MATERIALS AND METHODS
This was a prospective, randomized, open label study undertaken from August 2009 to October 2010. The study was carried out in H M Patel Research Centre at Shree Krishna Hospital and its attached peripheral centers: Rural Subcenter, Ardi; Primary Health Center, Bakrol; and Primary Health Center, Karamsad. The ethical approval was obtained from Human Research Ethics Committee of the Institute before starting of the study.
Sixty pregnant women were included during the study period. Pregnant women with gestational age between 12 and 32 weeks, diagnosed as iron deficiency anemia with hemoglobin < 8.5 g/dl, and specific indications for parenteral iron were selected for the study. Patients with other causes of anemia, infection, inflammation, liver or renal disease, recent administration of parenteral iron preparation and intolerance to iron derivatives were excluded from the study. A written informed consent was taken from each participant before enrolment into the study.
All the participants were randomized (ELECTERA version 2.23) in two groups. One group received 200 mg of elemental iron in the form of iron sucrose complex, administered as short intravenous infusion (in 100 ml of 0.9% normal saline) over half an hour. Another group received 300 mg of elemental iron in the form of iron sorbitol citric acid, which was administered intramuscularly in divided doses over 4 days (i.e. 75 mg daily). Because the iron sorbitol citric acid is highly dialyzable, 30–35% of elemental iron is excreted directly just after its administration.[11,12] Therefore, practically elemental iron would be similar in both the groups. However, the whole dose was calculated according to hemoglobin deficit by the following formula[13] and the remaining doses were continued orally after 1 month. The brand selected for iron sucrose complex was Imax-S (Brook Laboratories Ltd.) and for iron sorbitol citric acid was Jectocos (CFL Pharmaceuticals Pvt. Ltd.). The therapy was given free of cost to all recruited pregnant women.

Test dose was given before the therapy. If the patient did not show any reaction within 1 h, the remaining drug was administered. Whole therapy was monitored and each recipient was kept in observation in the hospital for at least 2 h after administration of parenteral iron.
Baseline investigations such as hemoglobin concentration, hematocrit level, MCV, MCH, and serum ferritin were performed before administering the iron therapy. After the therapy, each patient was followed twice, first follow-up after 14 days (i.e. 2 weeks) and second follow-up after 28 days (i.e. 1 month) of the parenteral iron therapy. On the day of first follow-up clinical examination and hemoglobin estimation were done. While on the day of second follow-up, i.e. after 28 days, all laboratory investigations were done as before administering the therapy. At the time of follow-up visits, patients were also inquired for any adverse drug reaction noted during this period.
Data were analysed according to Per Protocol Analysis (PPA). Statistical analysis was done by using MedCalc (version 9.2.0.1) and STATISTICA software (trial version). Data were analysed by using various statistical tests such as paired t-test for laboratory parameters of all patients before and after the therapy, independent t-test to compare both the groups, and repeated measure ANOVA test to compare the rise in the hemoglobin level in both the groups. All significance tests were two-tailed, with an α level of 0.05.
RESULTS
Between August 2009 and October 2010, from 893 pregnant women, 643 were detected as iron deficient anemia at various rural centers. Among them 97 number of pregnant women seem to be in need of parenteral iron therapy. Sixty pregnant women were included in the study according to selection criteria and randomly assigned in the one of the two groups, i.e. iron sucrose group (n = 30) or iron sorbitol citric acid group (n = 30). Eight pregnant women were lost to follow-up on the second follow-up visit, i.e. at 4 weeks. At 4 weeks, 29 pregnant women from the iron sucrose group and 23 pregnant women from the iron sorbitol citric acid group could be included for the analysis. One woman developed pregnancy-induced hypertension, one delivered prematurely, two withdrew the consent because of pain at the site of injection and others did not come for follow-up.
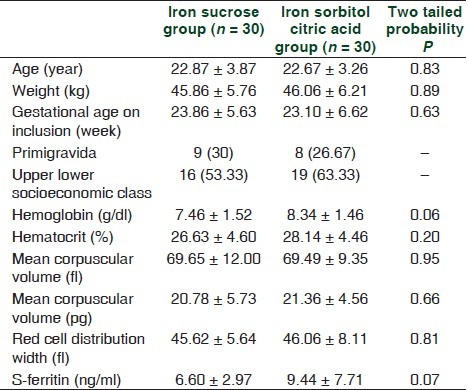
The initial demographic and laboratory characteristics were similar in both the groups [Table 1]. Age, weight, and gestational weeks were almost similar in both the groups with P > 0.05. Most women were multigravida while only 9 (30%) in iron sucrose and 8 (26.67%) in iron sorbitol citric acid groups were primigravida. According to the modified Prasad classification, most of the pregnant women belonged to upper lower socioeconomic class.[14] Hemoglobin concentration, haematocrit value, MCV, MCH and serum ferritin level of both the groups were also similar before the therapy (P > 0.05).
Table 1.
Baseline comparison of demographic and laboratory parameters between the iron sucrose group and iron sorbitol citric acid group
As seen in Figure 1 and Tables 2 and 3, the increase in hemoglobin in both the treatment groups was significant as compared to pre-treatment. Before the therapy, the mean hemoglobin level in the iron sucrose therapy group was 7.59 g/ dl (SD, 1.38), which was increased significantly up to 8.33 g/dl after 14 days and 9.25 g/dl (SD 1.91) after 28 days (P < 0.001). Similarly in the iron sorbitol citric acid therapy group hemoglobin was increased from 8.32 g/dl (SD 1.34) before therapy to 9.21 g/dl after 14 days and 9.77 g/dl (SD 1.64) after 28 days of the therapy. Tables 4 and 5 show that there was no significant difference in increase in the hemoglobin level in both the groups after 2 and 4 weeks. However, increment in the hemoglobin level from 2 to 4 weeks in the iron sucrose group was significantly more than the iron sorbitol citric acid group.
Figure 1.
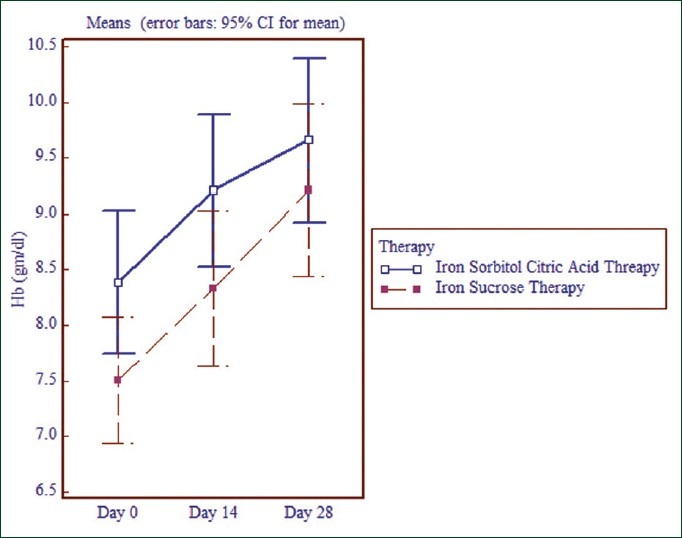
Mean increase in the hemoglobin concentration after iron sucrose and iron sorbitol citric acid therapy.
Table 2.
Comparison of the differences in laboratory parameters at the baseline and 28 days after iron sucrose therapy (n = 29)
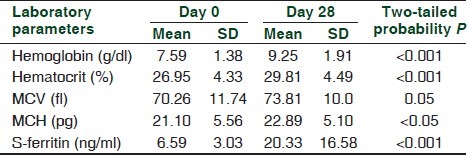
Table 3.
Comparison of the difference in laboratory parameters at the baseline and 28 days after iron sorbitol citric acid therapy (n = 23)
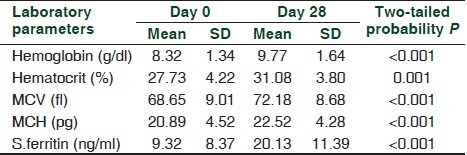
Table 4.
Comparison laboratory parameters of the iron sucrose group and the iron sorbitol citric acid group 28 days after the therapy
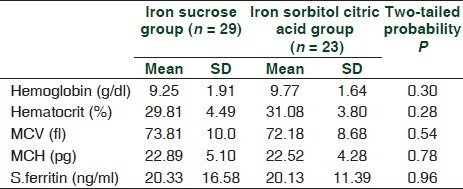
Table 5.
Hemoglobin differences during repeated measurement during different therapy

The ferritin level was found to be increased significantly across the time within both, iron sucrose (P < 0.001) and iron sorbitol citric acid (P < 0.001) groups. Before therapy, the serum ferritin level was 6.59 ng/ml in the iron sucrose therapy group and 9.32 ng/dl in the iron sorbitol citric acid therapy group, which was increased to 20.33 ng/dl and 20.12 ng/dl in iron sucrose and iron sorbitol citric acid therapy groups, respectively [Tables 2 and 3]. Ferritin value remained higher in the iron sorbitol citric acid group as seen in Figure 2. However, there was no significance difference in the serum ferritin level at day 28 after iron sucrose and iron sorbitol citric acid therapy (P > 0.05).
Figure 2.

Serum ferritin level before and after iron sucrose and iron sorbitol citric acid therapy.
Other parameters such as MCV, MCHC and hematocrit value were also increased significantly (P > 0.001) in both the groups as seen in Tables 2 and 3. However, there was no difference in increase in values of all laboratory parameters between two different iron therapies after 28 days (P > 0.05).
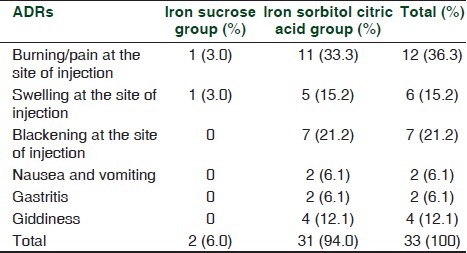
Sixty ampoules of iron sucrose injections (100 mg elemental iron each) and 116 ampoules of iron sorbitol citric acid injection (75 mg elemental iron each) were administered to 60 pregnant women. There was no serious adverse drug reactions, no episode of serious anaphylaxis or hypotensive attack was noted during the study period. As seen in Table 6, out of total 33 adverse events, only two events occurred in the iron sucrose group where one pregnant woman in the iron sucrose group complained of burning and swelling at the site of infusion. However, no other adverse event was noted in the iron sucrose group.
Table 6.
Adverse drug reactions
DISCUSSION
Iron deficiency anemia during pregnancy is common and deserves special attention because of its potential consequences. Oral iron is the first line of therapy in pregnancy with anemia. However, the compliance of pregnant women is much less because of its untoward effects such as gastritis, constipation and blackening of stool. Cumulative effects of all these warrant the use of parenteral iron. However because of cost and compliance to injectable iron, the current practice in this area is to give one fixed dose of parenteral iron then switch over to oral iron or continuations of parenteral iron according to severity of anemia.
For the efficacy of parenteral iron therapy, laboratory parameters such as hemoglobin concentration, serum ferritin, MCV, MCH and haematocrit value were chosen, because they are commonly preferred by clinicians in their clinical practice and gives better idea for diagnosis, prognosis and also evaluation of the therapy.
As seen in Table 5 and Figure 1, the rise in hemoglobin was significant in both the groups after 14 days and after 28 days. The normal rise in the hemoglobin level usually starts after three days of the starting of iron therapy, and the rate in rise of the hemoglobin level in pregnant women is 0.8 g/dl per week as compared to non-pregnant women of 1.0-1.2 g/dl per week.[15] Although not up to the expectation, the rate of increase in the hemoglobin concentration was found to be significant in this study. The reason for less rise in the hemoglobin level is unidentified, as the dose of iron was sufficient according to requirement for 1 month. The daily iron requirement in pregnancy is 4 mg/day (2.5 mg/day in early pregnancy, increasing up to 6 mg/day after 32 weeks)[16] and so for 1 month 120 mg to maximum of 150 mg iron is required. Instead, they were given 200 mg of elemental iron. Also during the antenatal visit, almost all the pregnant women were dewormed by a single dose of 400 mg albendazole.
However, the study by Breymann C et al.[17] showed a mean rise in the hemoglobin level was 1.7 g/dl, 25 days after the iron sucrose therapy. Also a study by Wali et al.[18] showed the hemoglobin level rise of 2.6 g/dl after 3.6 weeks. Therefore, the rise in the hemoglobin level in this study was almost similar to both these studies. That means practically increase in the hemoglobin level is not as much as expected. However, in this study with the limited dose of 200 mg of elemental iron, the initial rate of rise in the hemoglobin level is almost similar like in other studies with the full calculated dose.
The rise in the hemoglobin concentration in the iron sorbitol citric acid group was not similar to that of the iron sucrose group after the 14 days of the parenteral therapy. The reason might be that nearly 33-35% of iron sorbitol citric acid is excreted just after the injection and also its release from the reticuloendothelial system is much slower as compared to iron sucrose release from liver parenchymal cells.[19,20]
As seen in Tables 2 and 3 and Figure 2, the increase in the serum ferritin level was almost similar in both iron sucrose and iron sorbitol citric acid therapy groups. However, a study by Breymann C et al.[17] and Breymann C et al.[21] showed the rise in serum ferritin from 7 ng/ml to 342 ng/ml and from 8 ng/ml to 180 ng/ml, respectively. The reason for such a high increase in the ferritin level in these studies might be due to administration of the whole calculated therapeutic dose of parenteral iron as that of the conventional pattern. The dose in this study was sufficient for the production of adequate amount of red blood cells but for the store it is not sufficient.
Even though, similar efficacy as compared to laboratory parameters after the two different parenteral iron preparations, the main problem with the iron sorbitol citric acid was its side effects. Because iron sorbitol is much low molecular weight and has high transferrin saturation capacity, it cannot be given as high intravenous bolus or infusion.[22,23] Therefore, it is used only intramuscularly. However, the most common complaint in this study was pain at the site of injection, specifically with intramuscular injection of iron sorbitol citric acid, which was found to be similar to the study by Wali et al.[18] Similarly, other side effects such as swelling and blackening of skin were major complaints in the iron sorbitol citric acid therapy group. Also, the patient dropout rate was higher in the iron sorbitol citric acid therapy group, similar to the study by Wali et al.[18] Therefore, all these side effects of the iron sorbitol citric acid might be the main reason for decreasing the compliance of the pregnant women and increase in drop rates.
These adverse events were not seen with the iron sucrose complex therapy. However, the main problem with iron sucrose therapy was its cost. A total dose of therapy with the iron sucrose complex (inclusive of storage) costs between Rs. 2500 to 6000. In country like India the majority of the pregnant women suffering from iron deficiency anemia belong to middle to lower socioeconomic status and to purchase a complete dose of parenteral iron therapy is an economic burden for them. However, our study showed that the increases in all laboratory parameters are significant after the fixed single dose iron sucrose therapy.
CONCLUSION
In this study, all laboratory parameter levels increased significantly after both the iron sucrose and iron sorbitol citric acid therapy. The rise in hemoglobin was found to be slightly more in the iron sucrose group as compared to the iron sorbitol citric acid therapy after the second week. There was no other significant difference in the efficacy of both the groups in anemia therapy in pregnant women. However, in this study almost all adverse events such as pain, swelling and blackening at the site of injection were seen and because of the ADRs the dropout rate was much more in the iron sorbitol citric acid group. Giving iron sucrose in monthly divided doses decreases the economic burden to the patients and increases the compliance.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared
REFERENCES
- 1.Breymann C. Iron deficiency and anemia in pregnancy: Modern aspects of diagnosis and therapy. Blood Cells Mol Dis. 2002;29:506–16. [PubMed] [Google Scholar]
- 2.Yaqoob N, Abbasi SM. Nutritional iron deficiency in our population. J Coll Physicians Surg Pak. 2002;12:395–7. [Google Scholar]
- 3.Mukherji J. Iron deficiency anemia in pregnancy. Rational Drug Bulletin. 2002;12:2–5. [Google Scholar]
- 4.Bentley DP. Iron metabolism and anaemia in pregnancy. In: Letsky EA, editor. Clinics in Haematology. Vol. 14. London: WB Saunders; 1985. pp. 613–28. [PubMed] [Google Scholar]
- 5.Saeed M, Khan TA, Khan SJ. Evaluation of risk factors in antenatal care. Mother Child. 1996;34:139–42. [Google Scholar]
- 6.Kahrilas PJ, Hogan WJ. Gastroesopfiageal reflux disease. In: Sleisenger MH, Fordtran JS, editors. Gastrointestinal Disease. 5th ed. Philadelphia: WB Saunders; 1993. pp. 378–401. [Google Scholar]
- 7.Khan MM. Effects of maternal anemia on fetal parameters. J Ayub Med Coll Abbottabad. 2001;13:38–41. [PubMed] [Google Scholar]
- 8.Van Wyck DB, Cavallo G, Spinowitz BS, Adhikarla R, Gagnon S, Charytan C, et al. Safety and efficacy of iron sucrose in patients sensitive to iron dextran: North American clinical trial. Am J Kidney Dis. 2000;36:88–97. doi: 10.1053/ajkd.2000.8276. [DOI] [PubMed] [Google Scholar]
- 9.Silverstein SB, Rodgers GM. Parenteral iron therapy options. Am J Hematol. 2004;76:74–8. doi: 10.1002/ajh.20056. [DOI] [PubMed] [Google Scholar]
- 10.Faich G, Strobos J. Sodium ferric gluconate complex in sucrose: Safer intravenous iron therapy than iron dextrans. Am J Kidney Dis. 1999;33:464–70. doi: 10.1016/s0272-6386(99)70183-6. [DOI] [PubMed] [Google Scholar]
- 11.Tripathi KD. Haematinics and erythropoietin. 6th ed. New Delhi: Jaypee brothers medical publishers; 2008. Essentials of medical pharmacology; pp. 581–92. chapter 43. [Google Scholar]
- 12.Sharma A, Patnaik R, Garg S, Ramachandran P. Detection and management of anemia in pregnancy in an primary health care institution. Indian J Med Res. 2008;128:45–51. [PubMed] [Google Scholar]
- 13.Danielson BG, Geisser P, Schneider W. Iron therapy with special emphasis on intravenous administration. 1st ed. Switzerland(ECV): Vifor International; 1996. [Google Scholar]
- 14.Parashar SS. Principles of sociology in health care. In: Bhalwar R, Vaidya R, Tilak R, Gupta R, Kunte R, editors. Textbook of public health and community medicine. New Delhi: Dept of Community Medicine AFMC Pune; 2009. pp. 608–29. [Google Scholar]
- 15.Rutherford J, Strong J. Anemia and White Blood Cell Disorder. In: James DK, Steer PJ, Weiner CP, Gonik B, editors. High risk pregnancy: management options. Philadelphila: Elsevier; 2006. pp. 865–88. [Google Scholar]
- 16.Turmen T, Abouzahr C. Safe motherhood. Int J Gynecol Obstet. 1994;46:145–53. doi: 10.1016/0020-7292(94)90229-1. [DOI] [PubMed] [Google Scholar]
- 17.Breymann C, Perewusnyk G, Huch R, Huch A. Parenteral iron therapy in obstetrics: 8 years experience with iron-sucrose complex. Br J Nutr. 2002;88:3–10. doi: 10.1079/BJNBJN2002577. [DOI] [PubMed] [Google Scholar]
- 18.Wali A, Mushtaq A, Nilofar Comparative study-efficacy, safety and compliance of intravenous iron sucrose and intramuscular iron sorbitol in iron deficiency anemia of pregnancy. J Pak Med Assoc. 2002;52:392–5. [PubMed] [Google Scholar]
- 19.Johnson CA, Mason NA, Bailie GR. Intravenous iron products. ANNA J. 1999;26:522–4. [PubMed] [Google Scholar]
- 20.Beshara S, Lundquvist H, Sundin J, Lubberink M, Tolmachev V, Valind S, et al. 295 Kinetic analysis of 52Fe-labelled iron(III) hydroxide-sucrose complex following bolus administration using positron emission tomography. Br J Hematol. 1999;104:288–95. doi: 10.1046/j.1365-2141.1999.01170.x. [DOI] [PubMed] [Google Scholar]
- 21.Breymann C. The use of iron sucrose complex for anemia in pregnancy and postpartum period. Semin Hematol. 2006;43:28–31. [Google Scholar]
- 22.Pringle A, Goldber A, Macdonald E, Johnston S. 59Fe iron sorbitol citric-acid complex in iron-deficiency anaemia. Lancet. 1962;2:749–52. doi: 10.1016/s0140-6736(62)90573-1. [DOI] [PubMed] [Google Scholar]
- 23.Scott DE, Saltin AS, Pritchard JA. Iron sorbitex for treating iron-deficiency anaemia. Obstet Gynecol. 1967;30:679–82. [PubMed] [Google Scholar]


