Abstract
Pigmented basal cell carcinoma is a rare cutaneous neoplasm with only a few cases reported so far. Review of the literature yielded only an occasional fine-needle aspiration report of the cytologic features of the tumor.We report a rare case of pigmented basal cell carcinoma occurring on the thigh of a 55-year-old woman. The cytological features are described with discussion over the possible differential diagnoses.
Keywords: Basal cell carcinoma, cytology, fine needle aspiration cytology, pigmented
Introduction
Basal cell carcinoma (BCC) is a common skin cancer which is infrequently subjected to fine needle biopsy procedure. It is a slow growing malignant tumor which is locally aggressive but rarely metastasizes.[1] BCC generally occurs in adults, predominantly on the head and neck, followed by the trunk. Rare sites include genitalia, perianal skin and extremities.[2] Pigmented BCC (PBCC)is a rare variant with few cases described in English literature.[3] Biopsy or surgical excision of the lesion followed by histopathology has been the mainstay for diagnosis. Fine needle aspiration cytology (FNAC) is an important tool in diagnosing various cutaneous and subcutaneous tumors however review of literature revealed only an occasional case report of cytology of PBCC.[4] We report a case of PBCC occurring on the thigh of a 55-year-old woman, highlighting its cytological features.
Case Report
A 55-year-old female presented with a painless, non-hairy mole on the dorsal aspect of left thigh which had progressively increased over a period of 5 years. Local examination revealed a hyperpigmented polypoid swelling measuring 3 × 2 × 2 cm. It was firm, non-tender and the surface was focally ulcerated with bleeding points [Figure 1a]. General physical examination and systemic examinations were normal. There was no regional lymphadenopathy. FNA from the swelling yielded a brownish tinged hemorrhagic aspirate. Smears prepared were highly cellular showing many syncytial branching epithelial fragments laid in a clean background, with few having club-shaped edges. The cells were small basaloid, having scant cyanophilic cytoplasm, indistinct cell borders, and rounded hyperchromatic nuclei showing mild anisonucleosis, coarse granular chromatin and inconspicuous nucleoli. Occasional mitotic figures were seen. At places the fragments showedsmooth external contours with peripheral palisading of the nuclei. Many epithelial fragments showed cells embedded in abundant pink basement membrane like matrix. Fair amount of blue-black pigment was seen in the cellular fragments as well as in the macrophages scattered in the background [Figure 1b]. This pigment stained positive for Masson's Fontana stain. A cytological diagnosis of pigmented basal cell carcinoma was offered and excision biopsy advised.
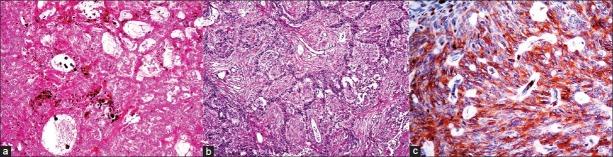
Figure 1.
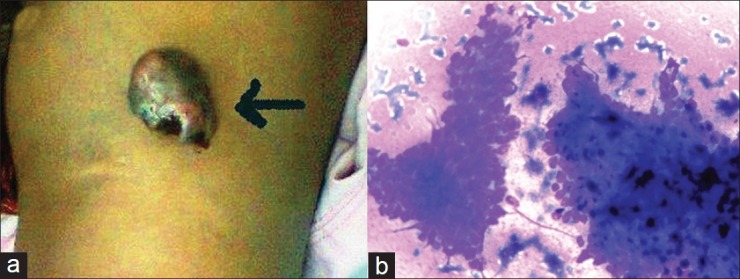
(a) Focally ulcerated, hyperpigmented polypoid swelling on the dorsal aspect of left thigh. (b) Cellular smear showing epithelial fragments containing small basaloid cells. Fair amount of blue-black pigment is seen in some of the cellular fragments (Giemsa, ×400)
Excision with 1 cm margin was performed under aseptic conditions. Gross specimen consisted of a skin covered polypoidal tissue measuring 3 × 2 × 2 cm. the cut surface was solid, firm, grey white with areas of brown-black pigmentation. Overlying skin was focally ulcerated with presence of hemorrhagic crusts.
Microscopic examination revealed a circumscribed dermal tumor, arising from the base of the epidermis, consisting of small basaloid cells exhibiting varied morphology. Predominant pattern was adenoid-basal with the tumor islands containing intertwining strands of epithelial cells forming gland-like structures at places (that contained loose mucoid stroma within them) [Figure 2a]. Other patterns included micronodular; infundibulocystic and fibroepithelioma-like [Figure 2b]. The cells were showing peripheral palisading at places. Some of the tumor cells showed melanin pigment production along with abundant melanin pigment in the melanophages present in the stroma surrounding the tumor cells. Occasional mitotic figures were seen however there was no necrosis, perineural/lymphovascular invasion. All surgical margins were free of tumor. On immunohistochemistry, the tumor cells were positive for Bcl-2, CD 10 and Ber EP-4 [Figure 2c], while EMA and HMB-45 was negative. S-100 was positive in the pigmented cells and melanophages while it was negative in rest of the cells. A final diagnosis of pigmented basal cell carcinoma (mixed histology) was rendered. The patient is well 6 months after the surgical excision with no recurrence.
Figure 2.
(a) Adenoid-basal pattern with intertwining strands of basaloid cells forming gland-like structures at places with some of the tumor cells showing melanin pigment production. (H and E, ×100). (b) Fibroepithelioma-like pattern seen in some areas. (H and E, ×100). (c) Tumor cells showing positivity for Ber EP-4 on immunohistochemistry (IHC, ×400)
Discussion
Basal cell carcinoma is a common type of skin cancer, making up more than 80% of the non-melanoma cancers. It is generally diagnosed on histopathological examination, however studies have suggested that cytology can be a useful alternative method of diagnosis.[5] Although BCC may arise without apparent reasons, predisposing factors include light skin color, chronic exposure to sunlight, large doses of X-rays or burn scars. PBCC is a rare variant in which melanin is produced by melanocytes that colonize the tumor and is present in melanophages located in the surrounding stroma.[6]
Naraghi et al.[7] performed an extensive study on 102 cases of BCC to examine the sensitivity and specificity of cytology inthe diagnosis of BCC. Of the 102 histopathologically proven cases of BCC, cytological study showed BCC in 89 (87.3%) however they did not encounter even a single case of PBCC.
Cytological diagnosis of PBCC is reliable if sufficient material is obtained. The smears are usually cellular showing cohesive sheets, syncytial branching fragments and club-shaped forms of small basaloid cells showing focal peripheral palisading. The cells are small, uniform, hyperchromatic and are seen embedded in basement membrane matrix. Melanin pigment is seen inside and outside the epithelial fragments which may be demonstrated on Masson Fontana stain.
The clinical differential diagnoses included melanoma and seborrheic keratosis. Cytology of melanoma shows dissociated single cells with occasional loosely cohesive groups of cells. The cells vary considerably in size and shape and may be bi- and multi-nucleated. The nuclei are often eccentric, hyperchromatic containing macronucleoli and atypical mitoses are often seen. The cells are positive for melanoma associated antigens, HMB-45, S-100 and Melan-A. Seborrheic keratosis is characterized by the presence of anucleate squames along with sheets of squamous cells and basaloid cells. There is no palisading of nuclei and no basement membrane matrix.[8]
Cytological differential diagnoses included tumors containing small basaloid cells i.e.; basaloid squamous cell carcinoma, adenoid cystic carcinoma, small cell neuroendocrine carcinoma and pilomatricoma. Basaloid squamous cell carcinoma shows clumped chromatin with parachromatin clearing, prominent nucleoli, mitoses and necrosis which were not seen in our case. Adenoid cystic carcinoma shows 3-dimensional clusters, finger-like tissue fragments, single cells and cribriform sheets enclosing hyaline globules. The fragments show intense crowding and overlapping of small hyperchromatic irregular nuclei. Small cell neuroendocrine carcinoma has atypical cells that are more dispersed (no club-shaped fragments seen) exhibiting nuclear molding. There is more pleomorphism, mitoses and necrosis. Basaloid component of pilomatricoma may resemble BCC but differs in clinical presentation, and contains “ghost cells”, multinucleate giant cells and calcific debris. Moreover, none of these lesions contain abundant melanin.[8]
On histopathological examination, the tumor showed a basal cell carcinoma with mixed histology (BCC-MH) with presence of four different patterns namely, adenoid-basal, micronodular, fibroepithelioma-like and infundibulo-cystic. The incidence of BCC-MH has been reported between 19-43% of cases of BCC. In a large study by Cohen et al.,[9] BCC-MH was observed in 43% (49/114) of the tumors. In their study, the location of BCC-MH was almost exclusively limited to the head and neck region with only 2 cases being present on distal lower extremities (ankle). No tumor was present on the thigh and none of them contained excess melanin pigment.
The report describes a rare variant of BCC, at a rare site, diagnosed on cytology. Knowledge of the cytological features of PBCC and its differentials can lead to correct diagnosis and allow for correct management of the patient.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Akinci M, Aslan S, Markoç F, Cetin B, Cetin A. Metastatic basal cell carcinoma. Acta Chir Belg. 2008;108:269–72. doi: 10.1080/00015458.2008.11680220. [DOI] [PubMed] [Google Scholar]
- 2.Newman JC, Leffell DJ. Correlation of embryonic fusion planes with the anatomical distribution of basal cell carcinoma. Dermatol Surg. 2007;33:957–65. doi: 10.1111/j.1524-4725.2007.33198.x. [DOI] [PubMed] [Google Scholar]
- 3.Kanitakis J, Arbona-Vidal E, Faure M. Extensive pigmented vulvar basal-cell carcinoma presenting as pruritus in an elderly woman. Dermatol Online J. 2011;17:8. [PubMed] [Google Scholar]
- 4.Calder CJ, Reynolds GM, Young FI, Marsden JR, Young JA. Cytological features of pigmented basal cell carcinoma-a potential diagnostic pitfall. Cytopathology. 1996;7:132–5. doi: 10.1046/j.1365-2303.1996.39582395.x. [DOI] [PubMed] [Google Scholar]
- 5.Vega-Memije E, De Larios NM, Waxtein LM, Dominguez-Soto L. Cytodiagnosis of cutaneous basal and squamous cell carcinoma. Int J Dermatol. 2000;39:116–20. doi: 10.1046/j.1365-4362.2000.00893.x. [DOI] [PubMed] [Google Scholar]
- 6.Kirkham N. Tumors and cysts of the epidermis. In: Elder DE, editor. Lever's histopathology of the skin. 10th ed. Philadelphia, USA: Lippincott 11 Williams and Wilkins; 2009. pp. 823–35. [Google Scholar]
- 7.Naraghi Z, Ghaninejad H, Akhyani M, Akbari D. Cytological diagnosis of cutaneous basal cell carcinoma. Acta Med Iran. 2005;43:50–4. [Google Scholar]
- 8.Bofin AM, Christensen E. In: Diagnostic cytopathology. 3rd ed. Gray W, Kocjan G, editors. China: Churchill Livingstone, Elsevier; 2010. pp. 745–6. [Google Scholar]
- 9.Cohen PR, Schulze KE, Nelson BR. Basal cell carcinoma with mixed histology: A possible pathogenesis for recurrent skin cancer. Dermatol Surg. 2006;32:542–51. doi: 10.1111/j.1524-4725.2006.32110.x. [DOI] [PubMed] [Google Scholar]