Abstract
Objective
To analyze change over 6 months in accelerometer-measured physical activity for participants with arthritis in a physical activity promotion trial. We tested the hypothesis that participants with the highest baseline functional capacity, regardless of their intervention status, experienced the greatest increases in physical activity levels at 6-month follow-up.
Design
At baseline, participants were interviewed in person, completed a 5-minute timed walk, and wore a biaxial accelerometer for 1 week, with a subsequent week of accelerometer wear at 6 months. We present data on the changes in accelerometermeasured physical activity across baseline function quartiles derived from participants’ walking speed. Analyses were controlled for sociodemographic, health status, and seasonal covariates as well as exposure to the study’s behavioral intervention.
Setting
A Midwest academic medical center.
Participants
Participants (N=226) with knee osteoarthritis or rheumatoid arthritis currently enrolled in the Improving Motivation for Physical Activity in Persons With Arthritis Clinical Trial.
Intervention
Counseling by physical activity coaches versus control group physician advice to exercise.
Main Outcome Measure
Change in average daily counts between baseline and 6-month follow-up.
Results
Contrary to our hypothesis, and after controlling for other predictors of change, the lowest quartile function participants had the largest mean absolute and relative physical improvement over baseline, regardless of intervention group status.
Conclusions
Participants at a higher risk of immanent mobility loss may have been more committed to improve lifestyle physical activity, reflecting the wisdom of targeting older adults at risk of mobility loss for physical activity behavior change interventions.
Keywords: Arthritis, Rehabilitation
Because of the graded association of functional status with physical activity,1 older, frail participants in physical activity promotion interventions may have more limited potential to increase their activity levels compared with younger, less disabled participants. Yet many behavioral interventions target functionally heterogeneous populations with a potentially wide range of functional capacity. While a mean percent improvement in physical activity in an intervention might appear to represent an average improvement for all participants, it could equally be because of large improvements by the most physically functional individuals, who potentially could increase their activity levels the most, combined with little change for more disabled participants.
This brief report provides insight into this issue by presenting 6-month changes in accelerometer-measured physical activity levels among functionally diverse individuals with arthritis enrolled in an on-going physical activity behavioral intervention study, the Improving Motivation for Physical Activity in Persons with Arthritis Clinical Trial (IMPAACT). We model changes in physical activity over 6 months after controlling for important sociodemographic, health status, and seasonal covariates as well as exposure to the study’s behavioral intervention. Our results test the hypothesis that inclusion of frail and disabled participants will reduce overall physical activity changes regardless of the success or failure of our intervention. Our findings inform targeting decisions for programs directed at increasing physical activity among functionally diverse, largely sedentary populations.
METHODS
IMPAACT Study
The IMPAACT study was approved by the Northwestern University Institutional Review Board. Participants with knee osteoarthritis or rheumatoid arthritis were randomized to receive a tailored physical activity counseling program or brief physician advice to increase physical activity.2 All participants had baseline and 6-, 12-, 18-, and 24-month scheduled follow-up as well as a week of accelerometer wear coinciding with each study wave. This report is based solely on the participants’ baseline and 6-month follow-up data; the trial is still underway and final results are not yet available. We present data on 226 participants with complete 6 months data accrued between 2006 and 2009.
Accelerometer Measures
Physical activity was monitored using a GT1M Actigraph accelerometer,a which measures the frequency and the magnitude of accelerations per 1-minute epochs. Participants were trained to wear it continuously on a waistline belt until going to bed at night for 7 consecutive days. Participants then mailed the device back at each study wave. The average daily accelerometer counts averaged across each week were computed following the National Cancer Institute accelerometer algorithm (http://riskfactor.cancer.gov/tools/nhanes_pam) developed for the National Health and Nutritional Examination Survey.3 A valid day was defined by 10 or more hours of wear time. Our analyses control for both baseline average daily wear hours and the change in average daily wear hours between baseline and 6-month follow-up.
Actigraph data were used to classify activity by intensity level.3 Because of a very high correlation between average daily counts and daily minutes of moderate or vigorous activity in our sample (r=.87), we also provide estimates of the changes in minutes of moderate or vigorous activity. The study focuses on total daily activity counts to analyze changes in physical activity of all intensities.
Walking Speed and Functional Capacity
Functional capacity was measured by a baseline 5-minute timed walk speed. Participants were asked to walk 5 minutes “at a brisk pace, like they were ‘late to a meeting’ or ‘trying to catch a bus.’” For ease of interpretation, we empirically divided participants by timed walk speed into 4 equal function quartiles, based on feet per second scores (<3.48, 3.48–4.00, 4.01– 4.60, >4.60). While timed walk speed measures only a single dimension of functional capacity, walking speed is closely associated with the trajectory of other functional tests,4 and is a frequent endpoint of lifestyle physical activity intervention studies.5
Sociodemographic Characteristics, Baseline Health, Intervention Status, and Season
Participant characteristics obtained at baseline interviews included age (4 categories), sex, race (white/other vs black), education (<high school vs ≥some college), current full- or part-time employment, and current smoking. Participants’ body mass index (BMI) was categorized into 3 categories: normative (>18.5 and ≤24.9), overweight (>24.9 and ≤29.9), or obese (≥30). The Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36) was used to compute baseline 0 to 100 summary scores for self-reported physical component summary (PCS) and mental component summary (MCS) scores.6 Participants were also classified as having been randomized to physical activity counseling or brief physician advice, and type of arthritis. We also controlled our analyses for the season each participant enrolled (and thus the season during which 6-month physical activity was measured).7
Statistical Analysis
Correlation coefficients were calculated between baseline timed walk speed and average daily counts. Changes in average daily counts and minutes of moderate or vigorous activity were calculated between the baseline and 6-month follow-up for each timed walk speed quartile. Multiple linear regression of 6-month change in average daily counts was used to test the effect of baseline walking speed function quartiles, after controlling for sociodemographic characteristics, health status, intervention status, and enrollment season covariates.
RESULTS
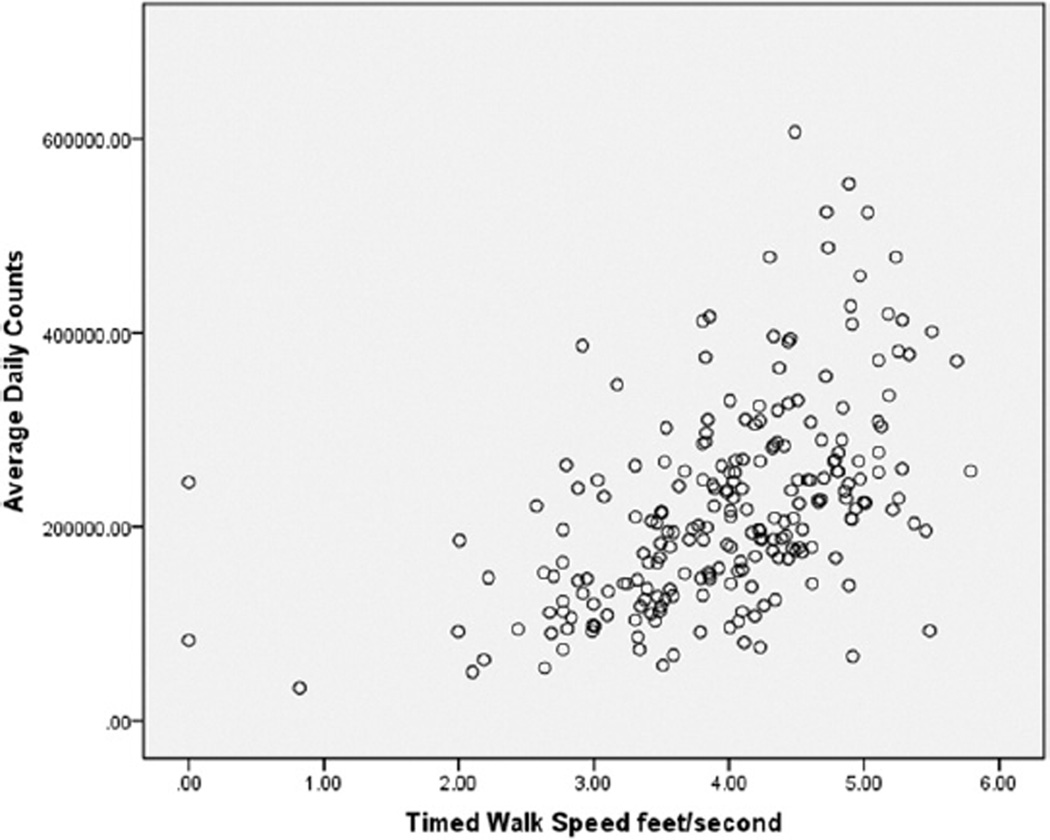
Baseline timed walk speeds had a mean of 3.98 feet per second, while daily counts (from a week of accelerometer use) were approximately normatve around a mean of 220,355 counts. This reflects a very sedentary population, with a mean of only about 19 minutes of average daily moderate or vigorous activity. Figure 1 provides a scatter plot of the association of baseline timed walk speed and average daily counts, showing an r equal to .50 (P<.0001) correlation.
Fig 1.
Baseline correlation of physical activity level and functional capacity for 226 participants in the IMPAACT.
Six-month change in daily activity counts indicated about equal proportions of participants increasing and decreasing their activity levels. Contrary to our hypothesized direction, the lowest function participants had by far the largest mean improvement (54,058) over baseline, while participants in the next highest function quartile had a mean decline (−12,719). Participants in the 2 higher function quartiles had similar, very modest, improvement rates (5255, 6241); 59.8% of the lowest function participants improved as compared with 50% in the highest function quartile.
Table 1 presents results of our multiple regression model of 6-month change in average daily counts. Being in the second lowest function quartile was associated with over 26,000 fewer average daily counts (P=.05) than the lowest (reference) quartile. Being in the highest 2 function quartiles was also associated with less change (~10,000 fewer counts) than the lowest quartile (not significant). Other significant variables included the negative effects of summer enrollment and being a current smoker. Each additional point of baseline SF-36 PCS was associated with an increase of over 1000 average daily counts at 6 months (P=.05). Change in average daily wear hours, which declined about 8 minutes between study waves, was also significantly correlated with change in average daily counts (P=.03). Other factors including intervention status were not significantly associated with 6-month physical activity change.
Table 1.
Multiple Regression Analysis of 6-Month Change in Average Daily Counts of 226 Participants in the IMPAACT (R2=.12)
| Participant Characteristics | Sample % or Mean ± SD |
B | SE | Significance |
|---|---|---|---|---|
| Constant | 41,925.86 | 63,022.68 | .51 | |
| Age <55y | 39.8 | Reference | ||
| Age 55–65y | 27.9 | −1666.70 | 11,539.90 | .89 |
| Age 66–75y | 21.2 | −10,469.18 | 14,501.12 | .47 |
| Age >75y | 11.1 | −7249.54 | 18,753.35 | .70 |
| Less than college education | 16.4 | 8407.70 | 12,750.65 | .51 |
| Black race | 18.1 | −11,221.75 | 13,887.88 | .42 |
| Women | 73.9 | −5406.22 | 10,926.54 | .62 |
| Employed full or part time | 51.3 | 4479.65 | 10,065.37 | .66 |
| Summer enrollment | 32.3 | −27,604.13 | 11,225.93 | .02 |
| Winter enrollment | 35.8 | 5114.81 | 11,290.20 | .65 |
| Spring/fall enrollment | 31.9 | Reference | ||
| Rheumatoid arthritis | 57.5 | −13,073.44 | 10,774.95 | .23 |
| Current smoker | 8.4 | −40,182.48 | 17,639.90 | .02 |
| Obese | 39.8 | −8185.32 | 12,691.97 | .52 |
| Overweight | 31.0 | −4572.00 | 12,070.65 | .71 |
| Normal weight | 29.2 | Reference | ||
| SF-36 MCS | 52.39±8.38 | −752.36 | 592.15 | .21 |
| SF-36 PCS | 44.54±8.49 | 1094.86 | 561.98 | .05 |
| Baseline average daily wear hours | 14.66±1.49 | −663.99 | 3742.44 | .86 |
| Change in average daily wear hours | −0.13±1.47 | 7442.66 | 3450.98 | .03 |
| Intervention group | 47.8 | 11,871.52 | 9009.34 | .19 |
| Timed walk velocity quartile 1 | 24.8 | Reference | ||
| Timed walk velocity quartile 2 | 25.2 | −26,123.46 | 13,319.02 | .05 |
| Timed walk velocity quartile 3 | 25.2 | −16,622.00 | 15,034.26 | .27 |
| Timed walk velocity quartile 4 | 24.8 | −17,124.56 | 15,937.34 | .28 |
DISCUSSION
We had hypothesized that change in physical activity for our largely sedentary participants would be greater for those with greater baseline functional capacity, whether participants were in the experimental or control groups. Our hypothesis was consistent with previous studies, finding that higher timed walking speed at baseline was a significant predictor of clinically important functional improvement for arthritis patients,8 as well as mobility improvement rates in a nationally representative study of older Americans.9 We, therefore, assumed that both absolute and relative (percent) change would probably be smallest among our participants with the lowest function at baseline.
The findings for the first 6 months of our study clearly contradict this hypothesis. The lowest quartile participants had by far the largest absolute gains and the largest proportion of participants who improved, including an impressive 23% improvement in minutes of moderate or vigorous activity. This pattern suggests that something was different about study participation among our most functionally challenged subjects. The major source of variation in our results was most likely the varying degree of motivation to participate in our study. Participation in the study may have meant more to a number of our older, frail participants with the most to lose if their mobility were to worsen. The relatively high rate of physical activity improvement among the lowest functioning individuals in the IMPAACT is consistent with outcomes for control subjects in other physical activity trials, for example, the LIFE study.4
Study Limitations
There are several major limitations to our findings. Our walking speed measure is a crude approximation of physical functioning, which is better measured by a more comprehensive battery of tests. A single 6-month follow-up, measured between 2 distinct seasons, may not capture the dynamics of long-term changes in activity levels, which are known to be highly sensitive to climate. Finally, our sample reflects largely older individuals with arthritis and may not be generalizable to younger populations with higher baseline levels of physical activity.
CONCLUSIONS
Contrary to our initial impression, the physical activity gains achieved by our lowest functioning participants add weight to the wisdom of targeting older adults at risk of mobility loss for physical activity behavior change interventions.10 As rehabilitation professionals know well, behavior change may be more likely when seen as vital to avoiding immanent disability.
Acknowledgments
We gratefully acknowledge Anh Chung and Leilani Lacson of Northwestern University for their assistance with database management and manuscript preparation.
Supported in part by the National Institutes of Health/National Institute of Nursing Research (grant no. P30 NR009014); the National Institute of Arthritis Musculoskeletal and Skin Diseases (grant nos. R01 AR052912, R01 AR055287, R01 AR054155), and the National Institute of Arthritis Musculoskeletal and Skin Diseases (grant no. P60 AR048098).
List of Abbreviations
- BMI
body mass index
- IMPAACT
Improving Motivation for Physical Activity in Persons with Arthritis Clinical Trial
- MCS
Mental Component Summary Score
- PCS
Physical Component Summary Score
- SF-36
Medical Outcomes Study 36-Item Short-Form Health Survey
Footnotes
No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit on the authors or on any organization with which the authors are associated.
Supplier
Actigraph, 49 E Chase St, Pensacola, FL 32502.
References
- 1.Dunlop DD, Song J, Semanik PA, Sharma L, Chang RW. Physical activity levels and functional performance in the osteoarthritis initiative: a graded relationship. Arthritis Rheum. 2011;63:127–136. doi: 10.1002/art.27760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ehrlich-Jones L, Mallinson T, Fischer H, et al. Increasing physical activity in patients with arthritis: a tailored health promotion program. Chronic Illn. 2010;6:272–281. doi: 10.1177/1742395309351243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 4.LIFE Study Investigators. Pahor M, Blair SN, et al. Effects of a physical activity intervention on measures of physical performance: results of the lifestyle interventions and independence for Elders Pilot (LIFE-P) study. J Gerontol A Biol Sci Med Sci. 2006;61:1157–1165. doi: 10.1093/gerona/61.11.1157. [DOI] [PubMed] [Google Scholar]
- 5.Keysor JJ. Does late-life physical activity or exercise prevent or minimize disablement? A critical review of the scientific evidence. Am J Prev Med. 2003;25(3 Suppl 2):129–136. doi: 10.1016/s0749-3797(03)00176-4. [DOI] [PubMed] [Google Scholar]
- 6.Ware JE, Kosinski M, Dewey JE. How to score version 2 of the SF-36 health survey. Lincoln: QualityMetric Inc; 2000. [Google Scholar]
- 7.Feinglass J, Lee J, Dunlop DD, Song J, Semanik P, Chang RW. The effects of daily weather on accelerometer-measured physical activity among adults with arthritis. J Phys Activ Health. 2011;8:934–943. doi: 10.1123/jpah.8.7.934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.White DK, Keysor JJ, Lavalley MP, et al. Clinically important improvement in function is common in people with or at high risk of knee OA: the MOST study. J Rheumatol. 2010;37:1244–1251. doi: 10.3899/jrheum.090989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feinglass J, Song J, Manheim LM, Semanik P, Chang RW, Dunlop DD. Correlates of improvement in walking ability in older persons in the United States. Am J Public Health. 2009;99:533–539. doi: 10.2105/AJPH.2008.142927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Evans WJ. Exercise as the standard of care for elderly people. J Gerontol A Biol Sci Med Sci. 2002;57:M260–M261. doi: 10.1093/gerona/57.5.m260. [DOI] [PubMed] [Google Scholar]