Abstract
Background
Communication interactions between nurses and mechanically ventilated patients in the intensive care unit (ICU) are typically brief. Factors associated with length of nurses’ communication have not been explored.
Objective
To examine the association between nurse and patient characteristics and duration of nurse talk.
Methods
In this secondary analysis, we calculated duration of nurse talk in the first 3-minutes of video-recorded communication observation sessions for each nurse-patient dyad (n=89) in the SPEACS study (4 observation sessions/dyad, n=356). In addition, we explored the association between nurses’ characteristics (age, gender, credentials, nursing experience, and critical care experience) and patients’ characteristics (age, gender, race, education, delirium, agitation-sedation, severity of illness, level of consciousness, prior intubation history, days intubated prior to study enrollment, and type of intubation) on duration of nurse talk during the 3-minute interaction observation.
Results
Duration of nurse talk ranged from 0–123 seconds and varied significantly over the 4 observation sessions (p=.007). Averaging the duration of nurse talk over the observation sessions, differences in talk time between the units varied significantly by study group (p<.001). Talk duration was negatively associated with a Glasgow Coma Scale ≤ 14 (p=.008). Length of intubation prior to study enrollment had a curvilinear relationship with talking duration (linear p=.002, quadratic p=.013); the point of inflection was at 23 days. Nurse characteristics were not significantly related to duration of nurse talk.
Conclusion
Length of time the patient is intubated, and the patient’s level of consciousness may influence duration of nurse communication in ICU.
Keywords: Nurse-patient communication, provide-patient communication, mechanical ventilation, intensive care unit, critical care
Introduction
In the United States, approximately 2.8 million adults require mechanical ventilation in an Intensive Care Units (ICU) each year1,2 and, as a consequence, are unable to communicate using natural speech.3 The inability to speak during mechanical ventilation can elicit negative emotions including, distress, anger, fear and isolation.4–20 In addition to emotional distress, patients in acute care settings who have communication problems are three times more likely to experience preventable adverse events.21
During an extended period of critical illness, it is essential that patients be provided the opportunity to communicate needs, symptoms, and emotions and participate in decision-making with their healthcare team members. Because of their unique care relationship with critically ill adults, nurses have the potential to mitigate the negative effects of impaired communication.22 However, observational studies suggest that nurse–patient communication interactions in the ICU typically last only one to five minutes in length.23–27
Clinician speaking time is a component of clinician-patient interaction and a well-documented communication measure in a variety of care settings.23,28–32 Duration of nurse talk is a valid indicator of communication interaction because nurses are the predominant initiators of communication in the ICU, and control communication opportunities with nonvocal patients.3,26 To date, factors associated with length of nurses’ communication interaction have not been explored.
Video recorded observations of nurse-patient interaction from the Study of Patient-Nurse Effectiveness with Assisted Communication Strategies (SPEACS)33, a three-group clinical trial, provided an opportunity to explore the factors associated with duration of nurse talk, which is one measure of the length and quality of nurse-patient communication interaction in the ICU. The majority of clinician-patient communication research has focused on a single interaction, which ignores the role that familiarity and continuity may play.29,31,32,34 When nurses spend more time caring for and communicating with their impaired patients, they perceived a greater sense of ease and success during the communication interaction.35 Secondary analysis of the SPEACS dataset provides a unique opportunity to evaluate consecutive communication interactions between nurses and mechanically ventilated, critically ill patients.
The primary aims of this secondary analysis were to: 1) describe the duration of nurse talk across four 3-minute interaction observations between nurses and mechanically ventilated (MV), critically ill adults, 2) investigate differences among the observations, study groups, and their combinations, and 3) explore the association between nurses’ and patients’ characteristics and duration of nurse talk during the 3-minute interaction observation. The University of Pittsburgh’s institutional review board approved this secondary analysis.
Methods
Design
This secondary analysis utilized data collected from adult ICU patients and their nurses enrolled in the SPEACS study.33 The SPEACS study employed a quasi-experimental sequential three-group design to test the impact of two interventions on nurse-patient communication compared to a usual care condition. The interventions included: A) basic communication skills training (BCST) for the study nurses, and B) basic communication skills training and electronic augmentative and alternative communication (AAC) device education with an individualized speech language pathologist (SLP) consultation (AAC-SLP). Low technology communication materials (e.g. alphabet boards, picture boards, writing materials) were available to the BCST group. In addition to low technology communication materials, patients in the AAC-SLP group received a SLP consultation and were offered high technology (electronic) AAC devices.33 The SPEACS study measured communication process outcomes, including ease, quality, frequency and success of communication. Baseline results have been reported3 and final results are forthcoming.
Setting
The SPEACS study was conducted in the 32-bed medical intensive care unit (MICU) and 22-bed cardiothoracic intensive care unit (CT-ICU) of a large academic medical center located in southwestern Pennsylvania.
Sample
Ten nurses were randomly selected from a pool of eligible nurses prior to the start of each study group for a total of 30 nurses. Patients (n=89) were selected by convenience sampling when a study nurse was available for observation on 2 consecutive day shifts. All nurse-patient dyads (n=89) who completed the parent study were included in this secondary analysis.3,33
Patient Participants
Eligible patients were: (1) nonspeaking due to oral endotracheal tube or tracheostomy, (2) intubated for 48 hours, (3) able to understand English, and (4) scored 13 or above on the Glasgow Coma Scale. The “verbal” score of the Glasgow Coma Scale was adapted to allow for patients to communicate words by nonverbal methods.3 Patients who were reported by family to have a diagnosed hearing, speech or language disability that could interfere with communication prior to hospitalization were excluded. Recruitment and eligibility have been previously described.33
Nurse Participants
Eligible nurses were selected for inclusion if they: (1) had at least 1 year of critical care nursing experience, (2) were full-time permanent staff in CT-ICU or MICU, (3) were English-speaking, and (4) were without hearing or speech impairment.
Intervention
The usual care group had access to writing supplies and, more rarely, communication boards however, no patients utilized the boards during observations and six patients used writing at least once.3 The BCST program intervention consisted of a 4-hour interactive educational session conducted primarily by a speech-language pathologist. BCST focused on assessment of the patient’s cognitive and motor function, basic interactive communication strategies, and the use of “low tech” communication tools (e.g., alphabet and picture communication boards, writing tools, etc.). These “low tech” communication tools were accessible to ICU staff and located in a designated “communication cart” on each unit. In addition to the basic educational program, study nurses in the third group (AAC-SLP) received a 2-hour educational session on the use of electronic AAC devices, which was delivered by a specially trained SLP. The SLP provided an individual assessment and developed a communication plan which included an electronic AAC device option for each study patient.33,37
Procedure and Data Collection
Observational data on 4 separate nurse-patient communication interactions were collected on two consecutive days, in the morning and afternoon/evening, when a nurse participant was assigned to the care of an enrolled patient. The patient-nurse encounters were naturally occurring observation sessions in which trained data collectors followed the nurse into the room during routine care with the exception of emergencies and intimate personal hygiene care. Medical chart review, researcher observations, and nurses’ self-report were used to obtain the clinical and demographic characteristics.
Outcome and Outcome Measurement
Duration of Nurse Talk
For this secondary analysis, duration of nurse talk was measured by calculating the amount of time in seconds that a nurse spoke to the patient during a 3-minute observation period. The 3-minute time unit was selected by the parent study researchers because the literature suggested that typical nurse–patient interactions in the ICU last 1–5 minutes in length23–25 and 3-minutes was determined, after viewing videotapes from prior research of gestural communication with nonspeaking ICU patients, to be an adequate amount of time to observe the communication interaction.33 While this timeframe limits the maximum length of possible nurse-patient communication, it does provide an equal observation time for all dyads. Total lengths of talking duration were calculated for each of the four interaction observations.
No intervention effect was noted on patient initiation of communication,36 which is an indicator of communication independence. On average, patients initiated 14% of communication exchanges. Given that patients’ level of communication independence remained constant over the study groups and since patients’ responses were nonvocal and difficult to accurately measure in time increments, it was reasonable to confine our measure of communication time to duration of nurse talk.
Inter-rater reliability of duration of nurse talk was calculated using percent agreement for time calculations performed by a second coder on a random selection of 10% of all cases from the study (n = 9). Reliability was ascertained at the 3-minute mark of each observation session. Coders achieved time measurement agreements ranging from 67–96% with an overall agreement of 92.4%.
Patient Characteristics and Clinical Characteristics
Patient demographic variables included in this analysis were: patient’s age in years, gender (male/female), race (White/Black), prior intubation history (yes/no) and total number of years of education. Demographic variables were self-reported by the patient or a family member. Patient clinical characteristics utilized for this secondary analysis were chosen for the potential to influence communication length3,25,27 and were selected from the Symptom Communication, Management, and Outcomes model, which was used in the SPEACS study.38
Patient clinical characteristics included delirium, agitation/sedation, severity of illness, level of consciousness, prior intubation history, days intubated prior to study enrollment, and type of intubation.
Presence of delirium was measured by the Confusion Assessment Method for ICU (CAM-ICU).39 TheCAM-ICU was adapted from the Confusion Assessment Method (CAM) for use with nonverbal ICU patients.40 The CAM-ICU demonstrated excellent inter-rater reliability (κ= .96, 95% CI, .92 – .99) and high criterion validity with excellent sensitivity, specificity, and accuracy when compared to the reference standard.41 Inter-rater reliability for the CAMU- ICU was checked by an independent rater for 10% of observation sessions, with > .90% agreement. Sedation-agitation was measured by the Richmond Agitation and Sedation Scale (RASS). The score yielded by the RASS was based on a 10-point scale with four levels of agitation, one level to denote a calm and alert state, and 5 levels of sedation.42 In 290 paired observations of critically ill adults admitted to a MICU, nurse inter-rater reliability was very high (κ = .91).43 In an independent cohort of 275 patients receiving MV, the RASS demonstrated excellent criterion, context, and face validity.43 An inter-rater agreement of > .90% was achieved on independent ratings of 10% of the observation sessions. Due to the lack of variability among the categories, a derived two-category variable was utilized denoting whether the patient was calm or had some degree of agitation or sedation.
Level of consciousness was measured by using the Glasgow Coma Scale (GCS). The GCS was developed in 1974 as a measurement tool to assess impaired consciousness and coma. It is based on three categories including eye opening, verbal, and motor responsiveness.44 Scores can range from 3 to 15 with lower scores denoting impaired consciousness and coma. In 290-paired observations by nurses, GCS demonstrated substantial inter-rater reliability (κ= 0.64; P=.001).43 In the parent study, the GCS was adapted to provide a verbal score, which represented a patient’s ability to communicate words using nonvocal methods.3 Because GCS scores lacked variability in this sample, both baseline and observation-dependent scores was converted to a derived binary variables where 15 (awake and completely oriented) or 14 and below (compromised). CAM-ICU, RASS, and GCS were obtained through researcher assessment and observation of the study patients.
Severity of illness was obtained by using the Acute Physiology and Chronic Health Evaluation (APACHE III) scoring system at enrollment and each study day. APACHE III has a total score range of 0–299.45 APACHE II tool was shown to be highly reproducible with an intra-class correlation coefficient of .90 and when reanalyzed with the APACHE III tool, results were similar. The predictive accuracy of first-day APACHE III scores is high.46 APACHE III is also commonly used to determine a daily severity of illness measure.45 In the parent study, APACHE III scores were obtained on enrollment and for the two consecutive days of observation. All APACHE III ratings for the parent study were checked by a second reviewer to achieve > .90 agreement.33
Type of intubation (oral endotracheal tube or a tracheostomy) was identified at each observation session. Finally, length of intubation prior to study enrollment was measured as the total number of days a patient was intubated during the current admission and was obtained by medical chart review.
Nurse Demographic Characteristics
Nurse demographic characteristics utilized for this secondary analysis included: age, gender, education/credentials, nursing experience, and critical care experience. Age was measured in years and gender was identified as a binary variable (male/female). Education was represented as a derived variable with two categories including 1) Diploma or Associates in Nursing and 2) Bachelor’s degree in nursing. Nursing experience was measured as total years of nursing practice and years of practice in a critical care setting (critical care experience).
Statistics
Data analysis was conducted using IBM SPSS Statistics (version 20.0, IBM Corp., Armonk, NY) and SAS (version 9.2, SAS Institute, Inc. Cary, NC). Descriptive statistics were computed to describe duration of nurse talk and nurse and patient characteristics. The data were screened for accuracy, missing values, outliers, and underlying statistical assumptions. Distribution of continuous variables was summarized using frequencies, means, and standard deviations. Frequency counts, percentages, and range were calculated for nominal variables. For ordinal variables, medians and interquartile ranges were also computed. Duration of nurse talk was found to be positively skewed across all four observation sessions therefore a square root data transformation was applied resulting in more normally distributed data. F-test from a two-way Analysis of Variance and binary logistic regression with exact conditional inference methods were used to compare nurse and patient characteristics across the units, study groups, and their combinations.
Some missing data were encountered in the dataset but appeared to be missing at random. Of the 89 patient participants, 7% (n=6) were missing CAM-ICU data for 1 to 3 observation sessions and 2% (n=2) were missing data for all observation sessions. The missing data occurred because the patient either refused to complete a section of the CAM-ICU or was unable to answer the questions because of a decreased level of consciousness or emotional state at time of assessment. When examining observation session-dependent CAM-ICU data as a predictor variable, the subjects who were missing all of their CAM-ICU data were dropped and subjects missing partial CAM-ICU data were retained for those time-points were CAM-ICU data was present. In addition to the missing CAM-ICU data, one patient did not report their level of education; hence when examining patient education as a predictor, this subject was dropped from the analysis.
Repeated measures analysis via linear mixed modeling was used to both describe groups and observation session effects and evaluate if there were difference in nurse talk time among observation sessions and/or study groups. This approach was taken because it allowed for the handling of data that were missing at random as well as accommodating for nurse and patient characteristics that were fixed or time-dependent covariates. Linear mixed modeling allowed for the modeling of the covariance matrix for the repeated measure assessments. The Kenward-Roger method was used for the estimation of degrees of freedom given the overall small sample size of the study. As an initial step the covariance matrix for the repeated assessment over the observation sessions was examined to determine the best fitting covariance structure, which was determined to be compound symmetric. F-tests and t-tests were used to assess main and interaction effects at a significance level of .05 for two-sided hypothesis testing. Least square means were estimated to describe the pattern based on the fitted model. The association between the patient and nurse characteristics and duration of nurse talk were assessed through an expanded version of the linear mixed model generated by the repeated measure analysis for aim 2 whereby each nurse and patient characteristic was added to the repeated measures model. The statistical significance of the association of the patient and nurse characteristics of interest with duration of nurse talk was evaluated using t-tests or F-tests with corresponding p-values as appropriate. The estimated regression coefficient with its standard error was reported to summarize the association between each characteristic with the duration of nurse talk adjusting for other covariates in the model
The characteristics were screened in a univariate manner using a p-value of .20 to identify candidate predictor variables for the multivariate modeling. Continuous predictors were evaluated for their functional form (linear, and non-linear quadratic). Nurse and patient characteristics that met screening criteria of a p≤.20 were then considered jointly via a multivariate model. Two-way interactions were explored by adding products of screened predictors in the multivariate model one by one. Finally, backwards elimination was applied to construct the parsimonious model, which included nurse and patient characteristics that were significant at p <.05 in the multivariate model.
Results
The nurses (N=30) ranged from 22 to 55 years of age (Mean±SD=35.40±9.99) and were predominantly female (80%). The majority held a Bachelor’s degree in nursing (BSN) (83%). Years in nursing practice and specifically in critical care ranged from 1 to 33 with a mean of 10.1 (SD=10.37) and 7.20 years (SD=8.58), respectively. Patients (N=89) ranged from 24 to 87 years of age (Mean±SD =56.81±15.68). Patients were predominantly white (89%) and had 8 to 21 years of formal education (Mean±SD=13.15±2.60). Patients were evenly distributed between males (49%) and females (51%). While patients (n=66) had multiple diagnoses upon admission to the ICU, the most common admitting diagnosis were pulmonary disease/infection (n=54), cardio, thoracic, or vascular surgery (n=32), and postoperative complications (n=30). All patients required mechanical ventilation for respiratory insufficiency. (See Table 1 and Table 2 for the breakdown of patient and nurse characteristics by study groups and unit within each study group)
Table 1.
Baseline Nurse Characteristics
| Usual Care | BCST | AAC-SLP | Total | P-value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| CTICU (n=5) | MICU (n=5) | CTICU (n=5) | MICU (n=5) | CTICU (n=5) | MICU (n=5) | CTICU (n=15) | MICU (n=15) | Group | Unit | Group by Unit | |
| Total (n=10 | Total (n=10) | Total (n=10) | Total (N=30) | ||||||||
| Characteristic | |||||||||||
|
| |||||||||||
| Age (years) | 43.2±11.7 | 40.4±5.3 | 30.0±12.4 | 30.4±12.3 | 29.6±4.6 | 38.8±1.9 | 34.3±11.5 | 36.5±8.5 | .03 | .50 | .33 |
| 41.8±8.7 | 30.2±11.6 | 34.2+5.9 | 35.4+10.0 | ||||||||
|
| |||||||||||
| Female* | 3 (60) | 5 (100) | 4 (80) | 4 (80) | 5 (100) | 3 (60) | 12 (80) | 12 (80) | 1.00 | NA | .49 |
| 8 (80) | 8 (80) | 8 (80) | 24 (80) | ||||||||
|
| |||||||||||
| Bachelors degree* | 4 (80) | 4 (80) | 5 (100) | 5 (100) | 3 (60) | 2 (40) | 12 (80) | 11 (73) | .08 | NA | 1.00 |
| 8 (80) | 10 (100) | 5 (50) | 23 (77) | ||||||||
|
| |||||||||||
| Nursing Experience (years) | 13.4±12.1 | 17.8±6.1 | 8.8±13.6 | 7.8±14.1 | 5.0±3.7 | 7.8±7.9 | 9.1±10.5 | 11.1±10.5 | .13 | .59 | .84 |
| 15.6±9.3 | 8.3±13.1 | 6.4±6.0 | 10.2±10.3 | ||||||||
|
| |||||||||||
| Critical Care Experience (years) | 12.0±12.4 | 10.6±5.5 | 8.0±12.4 | 5.6±9.2 | 2.4±0.6 | 4.6±5.3 | 7.5±10.2 | 6.9±6.9 | .15 | .87 | .82 |
| 11.3±9.1 | 6.8±10.3 | 3.5±3.7 | 7.3±8.5 | ||||||||
Note: Mean and Standard Deviation reported for continuous data (Mean + SD) and count and percentages (n, (%)) reported for categorical data.
Abbreviations: BCST- Basic Communication Skills Training, AAC-SLP- Basic Communication Skills Training and electronic augmentative and alternative communication device education with an individualized speech language pathologist consultation, p-value from an F-test from two-way Analysis of Variance
p-value using exact estimation in binary logistic regression
Table 2.
Baseline Patient Characteristics
| Usual Care | BCST | AAC-SLP | Total | p-value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| CTICU (n=15) | MICU (n=15) | CTICU (n=14) | MICU (n=15) | CTICU (n=15) | MICU (n=15) | CTICU (n=44) | MICU (n=45) | Group | Unit | Group by Unit | |
| Total (n=30) | Total (n=29) | Total (n=30) | Total (N=89) | ||||||||
| Characteristic | |||||||||||
|
| |||||||||||
| Age (years) | 54.1±15.6 | 58.5±16.1 | 58.4±16.9 | 57.8±14.7 | 58.4±10.1 | 53.7±20.8 | 57.0±14.2 | 56.7±17.1 | .87 | .93 | .55 |
| 56.3±15.7 | 58.1±15.5 | 56.1±16.2 | 56.8±15.7 | ||||||||
|
| |||||||||||
| Female* | 5 (33) | 11 (73) | 8 (57) | 8 (53) | 6 (40) | 7 (47) | 19 (43) | 26 (58) | .64 | .25 | .23 |
| 16 (53) | 16 (55) | 13 (43) | 45 (51) | ||||||||
|
| |||||||||||
| White* | 12 (80) | 11 (73) | 13 (93) | 13 (87) | 15 (100) | 15 (100) | 40 (91) | 39 (87) | .03 | NA | 1.00 |
| 23 (77) | 26 (90) | 30 (100) | 79 (89) | ||||||||
|
| |||||||||||
| Education (years) | 13.1±2.2 | 12.9±1.9 | 13.6.±2.8 | 12.4±2.1 | 14.1±3.7 | 12.8±2.7 | 13.6±2.9 | 12.7±2.2 | .74 | .11 | .61 |
| 13.0±2.0 | 13.0±2.5 | 13.5±3.2 | 13.2±2.6 | ||||||||
|
| |||||||||||
| Clinical Characteristic | |||||||||||
|
| |||||||||||
| APACHE III score | 48.6±9.9 | 50.3±16.2 | 55.9.±11.7 | 56.3±25.6 | 59.0±13.3 | 50.5±17.7 | 54.5±12.3 | 52.4±20.0 | .27 | .56 | .44 |
| 49.5±13.2 | 56.1±19.8 | 54.8±16.0 | 53.4±16.6 | ||||||||
|
| |||||||||||
| Days intubated prior to enrollment | 62.8±63.5 | 24.8±13.5 | 64.3±49.7 | 66.1±78.3 | 80.4±46.7 | 97.1±119.9 | 69.3±53.2 | 62.7±86.5 | .02 | .73 | .72 |
| 12.6±11.7 | 27.9±24.0 | 28.7±31.0 | 23.0±24.5 | ||||||||
|
| |||||||||||
| Prior history of intubation* | 6 (40) | 4 (26.7) | 2 (14.3) | 7 (46.7) | 8 (53.3) | 8 (53.3) | 16 (36.4) | 19 (42.2) | .13 | .57 | .18 |
| 10 (33) | 9 (31) | 16 (53) | 35 (39) | ||||||||
|
| |||||||||||
| CAM-ICU*-Delirium Present | 2 (13) | 5 (33) | 3 (21) | 6 (40) | 3 (20) | 2 (13) | 8 (18) | 13 (29) | .68 | .48 | .53 |
| 7 (23) | 9 (45) | 5 (23) | 21 (32) | ||||||||
|
| |||||||||||
| RASS*-Sedated/Agitated | 12 (80) | 11 (73) | 12 (86) | 7 (47) | 13 (87) | 11 (73) | 37 (84) | 14 (64) | .80 | .12 | .55 |
| 7 (23) | 19 (66) | 24 (80) | 66 (74) | ||||||||
|
| |||||||||||
| Pulmonary Disease/Infection | 10 (67) | 13 (87) | 2 (14) | 11 (73) | 7 (47) | 11 (73) | 19 (43) | 35 (78) | .03 | .00 | .44 |
| 23 (76) | 13 (45) | 18 (60) | 54 (60) | ||||||||
|
| |||||||||||
| Cardio, Thoracic, or Vascular Surgery | 4 (27) | 0 (0) | 13 (93) | 2 (13) | 10 (67) | 3 (20) | 27 (61) | 5 (11) | .00 | .00 | .37 |
| 4 (13) | 15 (52) | 13 (43) | 32 (36) | ||||||||
|
| |||||||||||
| Postoperative Complications | 6 (40) | 1 (7) | 13 (93) | 2 (13) | 4 (27) | 4 (27) | 23 (52) | 7 (16) | .04 | .00 | .00 |
| 7 (23) | 15 (52) | 8(27) | 30 (34) | ||||||||
Note: Mean and Standard Deviation reported for continuous data (Mean + SD) and count and percentages (n, (%)) reported for categorical data. Abbreviations: BCST- Basic Communication Skills Training, AAC-SLP- Basic Communication Skills Training and electronic augmentative and alternative communication device education with an individualized speech language pathologist consultation, APACHE- Acute Physiology and Chronic Health Evaluation, CAM-ICU- Confusion Assessment Method for the ICU, RASS- Richmond Agitation and Sedation Scale
p-value from an F-test from two-way Analysis of Variance
p-value using exact estimation in binary logistic regression
Duration of Nurse Talk
Duration of nurse talk, the primary outcome for this secondary analysis, ranged from 0 to 98 seconds for first observation (Median=23, Interquartile Range=22), 0–107 seconds for the second observation session (Median=26, Interquartile Range=25), 0–118 seconds for the third observation session (Median=35, Interquartile Range=27), and 0–123 seconds for the fourth observation session. Median=30, Interquartile Range=28). While nurse silence was rare, it did occur in 5 observed sessions during the first three minutes. During the observation sessions with nurse silence, the nurse was conversing with family members, other healthcare professionals, or silently performing technical procedures. There were 3 instances of nonverbal communication (e.g. touch, eye contact) during these 5 observed sessions.
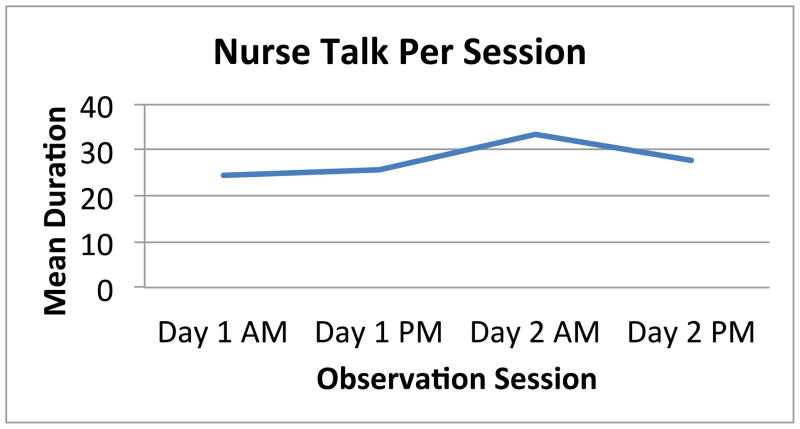
Duration of nurse talk varied significantly over the four observation sessions and generally tended to increase in length over the 2-day observation period (F(3, 228)=4.14, p=.007). Observation session three had the largest mean duration of nurse talk (seconds) (session 3=33.20 vs. session 1=24.45, session 2=25.72, session 4=27.91). (See Figure 1) Duration of nurse talk did not vary significantly between groups or between units. However when averaging the duration of nurse talk over the observation sessions, differences in talk duration between the units varied significantly by study groups (p<.001). In the usual care group, the MICU had a significantly longer mean duration of nurse talk (35.52 vs. 18.23 seconds) compared to the CTICU. Conversely in AAC-SLP group, the CTICU had significantly longer mean duration of nurse talk when compared to the MICU (34.18 vs. 25.77 seconds). There was no significant difference in duration of talk between the units in the BCST group.
Figure 1.
Mean Duration of Nurse Talk per Observation Session (In seconds)
Results of univariate modeling analyses (i.e. considering one characteristic at a time) are presented in Table 3. Patient characteristics including number of days intubated prior to study enrollment, observation session RASS and observation session GCS, and nurse characteristics including credentials, and years in critical care practice were identified as candidate predictors for the multivariate modeling using the screening criteria of p<.20 (See Table 4). Two of these candidate predictor variables, number of days intubated prior to study enrollment and critical care years of experience, were nonlinearly related to duration of nurse talk and were best modeled as a quadratic relationship (linear-quadratic). Two-way interactions were explored and none were deemed statistically significant.
Table 3.
Associations between Characteristics and Duration of Nurse Talk (Univariate Results)
| b | SE | t-value | p-value | |
|---|---|---|---|---|
|
|
||||
|
Baseline Nurse Characteristics
| ||||
| Age (years) | −0.006 | 0.015 | −0.39 | .698 |
| Gender- Male | 0.416 | 0.331 | 1.26 | .2125 |
| Credentials- Diploma or Associate Degree | −0.520 | 0.319 | −1.66 | .103* |
| Years in Nursing Practice | −0.004 | 0.013 | −0.28 | .781 |
|
| ||||
| Years in Critical Care Practice (Linear) | 0.016 | 0.032 | 0.51 | .6141* |
|
| ||||
| Years in Critical Care Practice (Quadratic) | −0.003 | 0.002 | −1.66 | .103* |
|
| ||||
| Baseline Patient Characteristics | ||||
|
| ||||
| Age (years) | 0.008 | 0.008 | 1.02 | .311 |
|
| ||||
| Gender- Male | 0.239 | 0.245 | 0.95 | .348 |
|
| ||||
| Race- White | −0.502 | 0.419 | −1.20 | .237 |
|
| ||||
| Education (years) (n=88) | 0.035 | 0.047 | 0.75 | .4582 |
|
| ||||
|
Baseline Patient Clinical Characteristics
| ||||
| CAM-ICU- Delirium Present | 0.113 | 0.292 | 0.39 | .701 |
|
| ||||
| RASS- Sedated or Agitated | −0.1719 | 0.288 | −0.60 | .553 |
|
| ||||
| APACHE III | 0.007 | 0.007 | 1.01 | .314 |
|
| ||||
| Prior Intubation History- Yes | −0.239 | 0.255 | −0.94 | .352 |
|
| ||||
| Days Intubated Prior to Enrollment (Linear) | −0.024 | 0.008 | −3.14 | .003* |
|
| ||||
| Days Intubated Prior to Enrollment (Quadratic) | <0.001 | <0.001 | 2.53 | .015* |
|
| ||||
|
Session-Dependent Patient Clinical Characteristics
| ||||
| CAM-ICU– Delirium Present (n=87) | −0.182 | 0.242 | −0.75 | .452 |
|
| ||||
| RASS- Sedated or Agitated | −0.5129 | 0.230 | −2.23 | .027* |
|
| ||||
| GCS- Score ≤14 | −0.801 | 0.312 | −2.57 | .011* |
|
| ||||
| APACHE III (calculated by day) | 0.007 | 0.006 | 1.11 | .271 |
|
| ||||
| Type of Intubation- Oral Intubation | −0.070 | 0.335 | −0.21 | .835 |
|
| ||||
|
Covariate
| ||||
| Time elapsed from nurse enrollment to first session (Days) | 0.002 | 0.002 | 1.05 | .299 |
Note: Variable (Referent)- Gender (Female), Race (Black), CAM-ICU (Delirium Absent), RASS (Calm), GCS (Score of 15), Type of Intubation (Tracheostomy)
Abbreviations: APACHE- Acute Physiology and Chronic Health Evaluation, CAM-ICU- Confusion Assessment Method for the ICU, RASS- Richmond Agitation and Sedation Scale, GCS- Glasgow Coma Scale
Denote screened variables that were considered jointly in the univariate model.
Table 4.
Associations between Characteristics and Duration of Nurse Talk (Multivariate Results)
| b | SE | t-value | p-value | |
|---|---|---|---|---|
|
|
||||
|
Baseline Nurse Characteristics
| ||||
| Credentials- Diploma or Associate Degree | −0.494 | 0.322 | −1.54 | .132 |
|
| ||||
| Years in Critical Care Practice (Linear) | 0.027 | 0.033 | 0.83 | .411 |
|
| ||||
| Years in Critical Care Practice (Quadratic) | −0.003 | 0.002 | −1.70 | .096 |
|
| ||||
| Baseline Patient Clinical Characteristics | ||||
|
| ||||
| Days Intubated Prior to Enrollment (Linear) | −0.022 | 0.008 | −2.78 | .007 |
|
| ||||
| Days Intubated Prior to Enrollment (Quadratic) | <0.001 | <0.001 | 2.50 | .016 |
|
| ||||
| Session-Dependent Patient Clinical Characteristics | ||||
|
| ||||
| RASS- Sedated or Agitated | −0.290 | 0.240 | −1.21 | .228 |
|
| ||||
| GCS- Score ≤14 | −0.610 | 0.325 | −1.88 | .062 |
Note: Variable (Referent)- Gender (Female), Race (Black), CAM-ICU (Delirium Absent), RASS (Calm), GCS (Score of 15), Type of Intubation (Tracheostomy)
Abbreviations: APACHE- Acute Physiology and Chronic Health Evaluation, CAM-ICU- Confusion Assessment Method for the ICU, RASS- Richmond Agitation and Sedation Scale, GCS- Glasgow Coma Scale
The number of days intubated prior to the observation period and GCS were jointly associated with duration of nurse talk in the parsimonious multivariate model. GCS of ≤14 at each session were negatively associated with talk duration (t=−2.70, p=.008). Days intubated prior to study enrollment had a curvilinear relationship with talking duration (linear t=−3.24, p=.002, quadratic t=2.50, p=.013). The point of inflection was at 23 days of intubation prior to study enrollment
Discussion
To our knowledge, we were the first to explore the association between nurse and patient characteristics and duration of nurse talk with MV patients in the ICU. As nurses are the main initiators and controllers of communication opportunities in the ICU, it is imperative to understand what can influence nurse communication. Longer duration of nurse talk may help facilitate patient interactions by providing them with more opportunities to interact thus strengthening the nurse-patient relationship and mitigating the negative emotions that patients experience.
This secondary analysis showed that as the number of days that ICU patients were intubated prior to observation increased, talk duration decreased; however at 23 days, the point of inflection, duration of nurse began to increase. The shift in nurse talk at 23 days may be reflective of the patient status in their illness-recovery trajectory. Earlier in the trajectory, nurses may encounter multiple barriers to talking with MV patients, such as surgery, sedation, patient’s illness acuity, interruptions for tests and procedures, whereas later in the trajectory patients are typically more medically stable and the nurse may have become familiar with the patient and their communication methods. Nurses should be aware that attention to communication during the early stage of a patient’s ICU stay might be valued by patients and families and may have a positive effect on the patient’s psychoemotional response to critical illness. Further research is needed to determine if increased and improved communication during this period has a significant impact on the patient’s emotional well being and adjustment to the hospitalization and post-discharge recovery..
The results of this analysis provide confirmation of findings from prior qualitative research that a patient’s level of consciousness is a significant factor influencing communication and length of care.,23,25 Our study is the first to provide an actual quantifiable measure of nurse communication demonstrating that nurses talked less to patients who were not completely alert and oriented during bedside care. Because the GCS’s verbal score was adapted to accommodate the patient’s ability to communicate using nonvocal methods, the difference in a score from 15 to 14 likely reflects a reduced level of consciousness or responsiveness. Clearly, nurses are inclined to talk more to patients who are awake, alert, and oriented during bedside care than patients who have to be aroused or reoriented.
Finally, ours was the first study to use video recording and microanalysis for accurate time measurement of nurse communication in the ICU. Duration of nurse talk ranged from 0 to 123 seconds per 3-minute observation session. Measures of duration of nurse talk as a component of nurse-patient communication were not conducted or reported in previous observational studies of nurse-patient communication. 23–27 Moreover, those studies occurred 10 to 25 years prior to the present study. It is likely that the environment of the ICU has changed over these last two decades as a response to increased technology and changing patient characteristics. For this analysis, measurement of nurse talk was limited to a 3-minute video recorded observation session for consistency, which limits the duration of interaction. Our median duration of nurse talk (23–35 seconds) in 3-minute periods (approximately 14%) may be proportionally similar to previous studies.23 Future studies should compare 3-minute sessions to longer interaction sessions to ensure that proportion of nurse talk is similar and that artificially limiting sessions does not bias estimation of the proportion of nurse talk time.
A consistent intervention effect across the study groups was not seen in this analysis. The only intervention effect identified was for the AAC-SLP study group and the effect was not seen across both units. The lack of intervention effect on duration of nurse talk is somewhat expected because the interventions implemented in the SPEACS study focused on enabling and facilitating patient communication. Nurses were taught techniques to more actively engage and interpret patient communication, which should not necessarily lead to the nurse talking for longer periods of time.
Limitations
One of the main concerns in secondary analysis is the quality of the data.47,48 To ensure data quality, the SPEACS study maintained an inter-rater reliability of r >.90 on several of the measures, including APACHE III, GCS, CAM-ICU, RASS and duration of nurse talk, that were used in this secondary analysis. Although inclusion in this study was not restricted by race, all patient participants were either White or Black thus limiting the external generalizability to other racial groups. With limited variability in the GCS and RASS scores, collapsing of the categories was necessary. This resulted in some loss of information and inability to analyze more discriminatory aspects of these two variables. In addition, the missing CAM-ICU data in each observation session could have impacted statistical power when examining the associations between delirium and duration of nurse talk. Finally, the video recorded observation sessions were limited to 3 minutes in length for this analysis. While all observation sessions lasted at least three minutes, there were sessions that lasted in excess of five minutes. Limiting the interaction to three minutes for this analysis provided an equal timeframe for measuring nurse talk duration but in doing so artificially limits and censored actual duration of nurse-patient interaction.
Clinical Implications
Nurses can use these findings to be more deliberative in communication interactions with patients who are in the early stages of critical illness and those who are experiencing a decreased level of consciousness. Therapeutic nurse communication with these patients may help reduce the negative emotions patients experience during mechanical ventilation and critical illness. In addition, improved communication may result in reduced need for sedation, thereby impacting length of stay and other untoward clinical outcomes, a more satisfying experience for patients and family members and a more satisfying practice for ICU nurses.
Conclusions
These findings have the potential to significantly impact the future research on critically ill, mechanically ventilated adults. Length of time intubated, and level of cognition influences nurse-patient communication and should be considered when developing studies aimed at enhancing communication between nurses and mechanically ventilated patients. In addition, more research is needed into the role that the illness-recovery trajectory has on communication. Specifically, understanding changes in patient communication patterns and needs over time in the ICU can help tailor communication interventions to best meet patient-nurse communication needs. Finally, nurses should allow and prioritize time for communication during the early stages of ICU admission and focus on methods of communicating with patients with decreased responsiveness.
Acknowledgments
Funding: National Institute of Child Health and Human Development (5R01-HD043988) (PI: M. Happ), National Institute of Nursing Research (K24-NR010244) (PI: M. Happ), National Institute of Nursing Research (F31 NR012856) (Nilsen)
We would like to thank the SPEACS team, including Dr. Judith Tate and Dana Divirgillo Thomas, for their excellent maintenance of the dataset and for providing essential information about the dataset throughout this analysis. Special thanks to Jill Radtke for performing the original computation of nurse talk time and performing reliability testing on this data.
Abbreviation List
- ICU
Intensive care unit
- MV
Mechanically Ventilated
- SPEACS
Study of Patient-Nurse Effectiveness with Assisted Communication Strategies
- BCST
Basic Communication Skills Training
- AAC
Augmentative and Alternative Communication
- SLP
Speech-language pathologist
- AAC-SLP
Basic communication skills training and electronic augmentative and alternative communication device education with an individualized speech language pathologist consultation
- MICU
Medical intensive care unit
- CT-ICU
Cardiothoracic intensive care unit
- GCS
Glasgow Coma Scale
- CAM-ICU
Confusion Assessment Method for ICU
- RASS
Richmond Agitation and Sedation Scale
- APACHE III
Acute Physiology and Chronic Health Evaluation III
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Marci Lee Nilsen, University of Pittsburgh, School of Nursing, Acute and Tertiary Care, 336 Victoria Building, 3500 Victoria Street, Pittsburgh, PA 15261.
Susan Sereika, Email: ssereika@pitt.edu, Associate Director for Statistical Support Services, School of Nursing, Health and Community Systems, 360 Victoria Building, 3500 Victoria St Pittsburgh, PA 15261, Phone: 412-624-0799, Fax: 412-624-1201.
Mary Beth Happ, Email: happ.3@osu.edu, Distinguished Professor of Critical Care Research, College of Nursing, The Ohio State University, 378 Newton Hall, 1585 Neil Ave, Columbus, OH 43210, Phone: 614-292-8336, Fax: 614-292-7976.
References
- 1.Angus D, Kelley M, Schmitz R, White A, Popovich J, Jr Committee on Manpower for Pulmonary and Critical Care S. Caring for the critically ill patient. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population? JAMA. 2000;284(21):2762–2770. doi: 10.1001/jama.284.21.2762. [DOI] [PubMed] [Google Scholar]
- 2.Angus D, Shorr A, White A, et al. Critical care delivery in the United States: distribution of services and compliance with Leapfrog recommendations. Critical Care Medicine. 2006;34(4):1016–1024. doi: 10.1097/01.CCM.0000206105.05626.15. [DOI] [PubMed] [Google Scholar]
- 3.Happ M, Garrett K, Thomas DD, et al. Nurse-Patient Communication Interactions in the Intensive Care Unit. American Journal of Critical Care. 2011;20(2):e28–e40. doi: 10.4037/ajcc2011433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bergbom-Engberg I, Haljamae H. Patient experiences during respirator treatment--reason for intermittent positive-pressure ventilation treatment and patient awareness in the intensive care unit. Critical Care Medicine. 1989;17(1):22–25. doi: 10.1097/00003246-198901000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Menzel LK. A comparison of patients’ communication-related responses during intubation and after extubation. Heart & Lung. 1997;26(5):363–371. doi: 10.1016/s0147-9563(97)90023-6. [DOI] [PubMed] [Google Scholar]
- 6.Rotondi AJ, Chelluri L, Sirio C, et al. Patients’ recollections of stressful experiences while receiving prolonged mechanical ventilation in an intensive care unit. Critical Care Medicine. 2002;30(4):746–752. doi: 10.1097/00003246-200204000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Wunderlich RJ, Perry A, Lavin MA, Katz B. Patients’ perceptions of uncertainty and stress during weaning from mechanical ventilation. Dimensions of Critical Care Nursing. 1999;18(1):2–12. [PubMed] [Google Scholar]
- 8.Patak L, Gawlinski A, Fung NI, Doering L, Berg J. Patients’ reports of health care practitioner interventions that are related to communication during mechanical ventilation. 2004;33(5):308–320. doi: 10.1016/j.hrtlng.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 9.Menzel LK. Factors related to the emotional responses of intubated patients to being unable to speak. Heart & Lung. 1998;27(4):245–252. doi: 10.1016/s0147-9563(98)90036-x. [DOI] [PubMed] [Google Scholar]
- 10.Gries ML, Fernsler J. Patient Perceptions of the mechanical ventilation experience. focus on Critical Care. 1988;15(2):52–59. [PubMed] [Google Scholar]
- 11.Fitch M. The patient’s reaction to ventilation. Canadian Critical Care Nursing Journal. 1989;6(2):13–16. [PubMed] [Google Scholar]
- 12.Riggio RE, Singer RD, Hartman K, Sneider R. Psychological issues in the care of critically-ill respirator patients: differential perceptions of patients, relatives, and staff. Psychological Reports. 1982;51(2):363–369. doi: 10.2466/pr0.1982.51.2.363. [DOI] [PubMed] [Google Scholar]
- 13.Frace RM. Mechanical ventilation: the patient’s viewpoint. Todays Or-Nurse. 1982;4(6):16–21. [PubMed] [Google Scholar]
- 14.Belitz J. Minimizing the psychological complications of patients who require mechanical ventilation. Critical Care Nurse. 1983;3(3):42–46. [PubMed] [Google Scholar]
- 15.Jablonski R. The experience of being mechanically ventilated. Qualitative Health Research. 1994;4(2):186–207. [Google Scholar]
- 16.Rier D. The missing voice of the critically ill: A medical sociologist’s first-hand account. Sociology of Health and illness. 2000;22(1):68–93. [Google Scholar]
- 17.Happ MB. Interpretation of nonvocal behavior and the meaning of voicelessness in critical care. Social Science & Medicine. 2000;50(9):1247–1255. doi: 10.1016/s0277-9536(99)00367-6. [DOI] [PubMed] [Google Scholar]
- 18.Cooper MC. The intersection of technology and care in the ICU. Advances in Nursing Science. 1993;15(3):23–32. doi: 10.1097/00012272-199303000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Robillard A. Commmunication problems in the intensive care unit. Qualitative Sociology. 1994;17(4):383–395. [Google Scholar]
- 20.Carroll S. Silent, slow lifeworld: the communication experience of nonvocal ventilated patients. Qualitative Health Research. 2007;17(9):1165–1177. doi: 10.1177/1049732307307334. [DOI] [PubMed] [Google Scholar]
- 21.Bartlett G, Blais R, Tamblyn R, Clermont RJ, MacGibbon B. Impact of patient communication problems on the risk of preventable adverse events in acute care settings. CMAJ Canadian Medical Association Journal. 2008;178(12):1555–1562. doi: 10.1503/cmaj.070690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Happ MB, Baumann BM, Sawicki J, Tate JA, George EL, Barnato AE. SPEACS-2: intensive care unit “communication rounds” with speech language pathology. Geriatric Nursing. 2010;31(3):170–177. doi: 10.1016/j.gerinurse.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 23.Ashworth P. Care to Communicate: An Investigation into Problems of Communication Between Patients and Nurses in Intensive Therapy Units. London: Royal College of Nursing of United Kingdom; 1980. [Google Scholar]
- 24.Leathart AJ. Communication and socialisation (1): An exploratory study and explanation for nurse-patient communication in an ITU. Intensive & Critical Care Nursing. 1994;10(2):93–104. doi: 10.1016/0964-3397(94)90004-3. [DOI] [PubMed] [Google Scholar]
- 25.Hall DS. Interactions between nurses and patients on ventilators. American Journal of Critical Care. 1996;5(4):293–297. [PubMed] [Google Scholar]
- 26.Salyer J, Stuart BJ. Nurse-patient interaction in the intensive care unit. Heart & Lung. 1985;14(1):20–24. [PubMed] [Google Scholar]
- 27.Bergbom-Engberg I, Haljamae H. The communication process with ventilator patients in the ICU as perceived by the nursing staff. Intensive & Critical Care Nursing. 1993;9(1):40–47. doi: 10.1016/0964-3397(93)90008-l. [DOI] [PubMed] [Google Scholar]
- 28.Roter DL, Hall JA. Physician gender and patient-centered communication: a critical review of empirical research. Annu Rev Public Health. 2004;25:497–519. doi: 10.1146/annurev.publhealth.25.101802.123134. [DOI] [PubMed] [Google Scholar]
- 29.Friedman D, Hahn S, Quigley H, et al. Doctor-patient communication in glaucoma care: analysis of videotaped encounters in community-based office practice. Ophthalmology December. 2009;116(12):2277–2285. doi: 10.1016/j.ophtha.2009.04.052. [DOI] [PubMed] [Google Scholar]
- 30.Burgio LD, Allen-Burge R, Roth DL, et al. Come talk with me: improving communication between nursing assistants and nursing home residents during care routines. Gerontologist. 2001;41(4):449–460. doi: 10.1093/geront/41.4.449. [DOI] [PubMed] [Google Scholar]
- 31.Brown AS, Cofer-Chase L, Eagan CA. Linguistic analysis of in-office dialogue among cardiologists, primary care physicians, and patients with mixed dyslipidemia. Am J Cardiol. 2010;106(1):51–55. doi: 10.1016/j.amjcard.2010.02.014. [DOI] [PubMed] [Google Scholar]
- 32.Tai-Seale M, McGuire T, Colenda C, Rosen D, Cook MA. Two-minute mental health care for elderly patients: inside primary care visits. Journal of the American Geriatrics Society. 2007;55(12):1903–1911. doi: 10.1111/j.1532-5415.2007.01467.x. [DOI] [PubMed] [Google Scholar]
- 33.Happ MB, Sereika S, Garrett K, Tate J. Use of the quasi-experimental sequential cohort design in the Study of Patient-Nurse Effectiveness with Assisted Communication Strategies (SPEACS) Contemporary Clinical Trials. 2008;29(5):801–808. doi: 10.1016/j.cct.2008.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Beattie PF, Pinto MB, Nelson MK, Nelson R. Patient Satisfaction With Outpatient Physical Therapy: Instrument Validation. Physical Therapy. 2002;82(6):557–565. [PubMed] [Google Scholar]
- 35.Hemsley B, Balandin S, Worrall L. Nursing the patient with complex communication needs: time as a barrier and a facilitator to successful communication in hospital. Journal of Advanced Nursing. 2012;68(1):116–126. doi: 10.1111/j.1365-2648.2011.05722.x. [DOI] [PubMed] [Google Scholar]
- 36.Happ MB, Garrett KL, Sereika S, DiVirgilio-Thomas D, Tate J, George E. Changes in ICU Communication Following Nurse Education and AAC Interventions. Paper presented at: 2009 Clinical AAC Research Conference Proceedings; October, 2009; Pittsburgh, PA. [Google Scholar]
- 37.Radtke JV, Baumann BM, Garrett KL, Happ MB. Listening to the voiceless patient: case reports in assisted communication in the intensive care unit. Journal of Palliative Medicine. 2011;14(6):791–795. doi: 10.1089/jpm.2010.0313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Campbell GB, Happ MB. Symptom identification in the chronically critically ill. AACN Advanced Critical Care. 2010;21(1):64–79. doi: 10.1097/NCI.0b013e3181c932a8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ely E, Margolin R, Francis J, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) Critical Care Medicine. 2001;29(7):1370–1379. doi: 10.1097/00003246-200107000-00012. [DOI] [PubMed] [Google Scholar]
- 40.Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Annals of Internal Medicine. 1990;113(12):941–948. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 41.Ely E, Inouye S, Bernard G, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU) JAMA. 2001;286(21):2703–2710. doi: 10.1001/jama.286.21.2703. [DOI] [PubMed] [Google Scholar]
- 42.Sessler C, Gosnell M, Grap M, et al. The Richmond Agitation–Sedation Scale: validity and reliability in adult intensive care unit patients. American Journal of Respiratory and Critical Care Medicine. 2002;166:1338–1344. doi: 10.1164/rccm.2107138. [DOI] [PubMed] [Google Scholar]
- 43.Ely E, Truman B, Shintani A, et al. Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS) JAMA. 2003;289(22):2983–2991. doi: 10.1001/jama.289.22.2983. [DOI] [PubMed] [Google Scholar]
- 44.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 45.Wagner DP, Knaus WA, Harrell FE, Zimmerman JE, Watts C. Daily prognostic estimates for critically ill adults in intensive care units: results from a prospective, multicenter, inception cohort analysis. Critical Care Medicine. 1994;22(9):1359–1372. doi: 10.1097/00003246-199409000-00004. [DOI] [PubMed] [Google Scholar]
- 46.Knaus WA, Wagner DP, Draper EA, et al. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100(6):1619–1636. doi: 10.1378/chest.100.6.1619. [DOI] [PubMed] [Google Scholar]
- 47.Babbie ER. The basics of social research. 4. Belmont, CA: Thomson Wadsworth; 2008. [Google Scholar]
- 48.Bibb S. Issues associated with secondary analysis of population health data. Applied Nursing Research. 2007;20(2):94–99. doi: 10.1016/j.apnr.2006.02.003. [DOI] [PubMed] [Google Scholar]