Abstract
Background:
Duration of treatment in tuberculosis of spine has always been debatable in the absence of marker of healing. The objective of the study was to evaluate the efficacy of extended DOTS regimen (2 months of intensive phase and 6 months of continuation phase) as recommended by WHO, by using MRI observations as the healing marker.
Materials and Methods:
51 (Group A -28 prospective and Group B- 23 retrospective) patients of spine TB with mean age of 26.8 years (range 15-54 years) diagnosed clinico radiologically/imaging (n=36), histopathology or by PCR (n=15) were enrolled for the study. They were treated by extended DOTS regimen (2 months of HRZE and 6 months of HR) administered alternate day. The serial blood investigations and X-rays were done every 2 months. Contrast MRI was done at the end of 8 months and healing changes were recorded. Criteria of healing on the basis of MRI being: complete resolution of pre and paravertebral collections, resolution of marrow edema of vertebral body (VB), replacement of marrow edema by fat or by calcification suggested by iso- intense T1 and T2 weighted images in contrast enhanced MRI. Patients with non healed status, but, responding lesion on MRI after 8 months of treatment were continued on INH and rifampicin alternate day and contrast MRI was done subsequently at 12 months and 18 months till the healed status was achieved .
Results:
9 patients had paraplegia and required surgical intervention out of which 1 did not recover neurologically. All patients have completed 8 months of extended DOTS regimen, n=18 achieved healed status and duration of treatment was extended in rest (n=33) 5 were declared healed after 12 months, 8 after 18 months and one after 36 months of treatment, thus 32 were declared healed at varying periods.
Conclusion:
35.2% patients demonstrate MRI based healed vertebral lesion at the end of 8 months of extended category 1 DOTS regimen. It is unscientific to stop the ATT by fixed time frame and MRI evaluation of the patients is required after 8 months of ATT and subsequently to decide for the continuation stoppage of treatment.
Keywords: Anti tubercular drugs, DOTS regimen, magnetic resonance imaging, TB spine
INTRODUCTION
Spinal TB is a medical disease and surgery is primarily indicated for complications like spinal deformity and neurological deficit.1 poor patient compliance lead to emergence of drug resistance.1–9 The daily and intermittent dosage regimens have been used for 6, 9, 18, or 24 month. The short course chemotherapy is reported as equally effective as 18 months.1,2–26
The compliance to antitubercular treatment (ATT) is enhanced with introduction of Directly Observed Treatment Short course (DOTS) regimen. The duration of treatment is decided by sputum conversion from smear positive to smear negative in pulmonary TB.3,9 The osteoarticular TB is a paucibacillary disease and the development of bacteriological sterility of the lesion cannot be ascertained. The endpoint of the disease is not yet established; hence the optimum duration of ATT in osteoarticular TB remain unresolved.3,9
The clinicoradiological and hematological evidence with no evidence of recurrence at 2 years or more is considered a healed status.1,7,27 There is insufficient data to support the role of short course intermittent chemotherapy in TB of spine. The observations on the progressive healing pattern on magnetic resource imaging (MRI) have been reported, however, no large scale analysis has been documented. Hence this study was conducted to evaluate the efficacy of extended category 1 DOTS regimen in cases of spinal TB as assessed by contrast enhanced MRI and to document the percentage of cases who continue to have active disease at the end of 8 months of drug therapy.
MATERIALS AND METHODS
A total of 51 cases of TB spine with age more than 15 years of either sex with paradiscal lesion, with/without paraplegia diagnosed clinicoradiologically and by MRI/ histopathology/fine needle aspiration cytology (FNAC)/bacteriology/serology/molecular tests were enrolled for the study. The cases were divided into two groups. Group A: freshly diagnosed cases of TB spine and prospectively treated and group B: patients who are in various stages of treatment and had a pretreatment MR scan. Patients with atypical presentations of TB spine such as isolated intraspinal granuloma, isolated posterior complex involvement, single vertebral body lesion, isolated craniovertebral junction TB, isolated sacral TB or patients without a classical clinicoradiological diagnosis, known cases of chronic illness, and patients not having pretreatment MRI were excluded from the study. Neurological assessment was performed by Jain and Sinha scoring system.28 Full blood count, erythrocyte sedimentation rate (ESR), liver function test (LFT), and kidney functional test (KFT) were performed on admission.
The radiological diagnosis was made on observation of demineralization of the vertebra, fuzzy paradiscal margin, reduction/obliteration of disc space, along with one or more of the following: destruction of end plates, wedging of vertebra, obvious kyphotic deformity, paravertebral shadows, and anterior scalloping of vertebral body.27,29 The aspirate of paraspinal and psoas abscesses (n=9) was sent for Z–N staining, pus culture, and polymerase chain reaction (PCR). Computerized tomography (CT) guided biopsy was done in two patients. The surgical decompression (with or without instrumented stabilization) was done for severe neurological deficits, developing or progressive neural deficits on treatment, panvertebral disease and severe kyphotic deformity. The MR imaging was performed at Institute of Nuclear Medicine and Allied Sciences (INMAS) on systems with magnetic field strengths of 3 Tesla. Sagittal, axial and coronal T1-weighted spin-echo images and T2-weighted fast spin-echo images were obtained using phased array coils. Additional coronal and sagittal STIR fat suppression sequence images were also obtained. On MRI the characteristic picture comprised of marrow edema of vertebral body with end plate erosions and discitis along with pre- and paravertebral septate loculated collection (including intraosseous abscess) with subligamentous collection and epidural extension.27,29,30–34
All cases were put on extended DOTS Category I ATT regimen which consisted of alternate day dosage (thrice weekly) of the following drugs: Cap Rifampicin [R] 450 mg (10 mg/ kg), (maximum 600 mg), Tab Isoniazid [H] 600 mg (10 mg/ kg) (maximum 600 mg), Tab Pyrazinamide [Z] 1500 mg (35 mg/kg) (maximum 2000 mg), and Tab Ethambutol [E] 1200 mg (30 mg/kg) (maximum 1600 mg) for the first 2 months followed by HR for the next 6 months. All patients were evaluated by X-rays and hematological tests at the end of 2nd, 4th, 6th, and 8th month of DOTS therapy.
Contrast enhanced MRI was done at the end of 8 months of DOTS regimen, which was evaluated by a radiologist blinded to the treatment duration and outcome. ATT was extended when MRI did show regression of lesion without evidence of complete healing. The MRI, X-rays, and hematological investigations were repeated at 12 and 18 months. ATT was stopped on the basis of changes suggestive of healed status on MRI at every evaluation.
The healing was assessed clinically as reduction in pain with improvement in constitutional symptoms, weight gain, improvement in daily activity, reduction in cold abscess, and healing of sinuses; hematologically as reduction in ESR and rise in hemoglobin. The radiological healing was labeled as the remineralization and reappearance of bony trabeculae, sharpening of articular margin, sharpening of cortical margin, sclerosis of vertebral body and end plates, fusion of vertebral bodies on plain X-rays; and on contrast MR as complete absence of paravertebral collection, complete resolution of enhanced vertebral body, fatty replacement of marrow seen as enhanced intensity in both T1 and T2 weighted images, and isointense STIR fat suppressed MRI sequence
Patients having healed vertebra with persistent paravertebral collection or having heterogeneous VB signal intensity in T1 and T2 WI on contrast enhanced MRI were subjected to 18F-FDG PET-CT whole body scan at INMAS (Department of Cyclotron).35 Sixty minutes following intravenous injection of 370 MBq of 18F-FDG (fluorinated deoxyglucose), Positron emission tomography and computerized tomography (PET/CT) scan from the skull to mid-thigh was acquired in a whole-body Full Ring PET-CT Scanner (Discovery STE16 camera). A low dose CT was obtained on the same area without IV contrast for attenuation correction and coregistration. Images were reconstructed using a 3D VUE algorithm and slices were reformatted into transaxial, coronal and sagittal views. Lesions showing active uptake of 18F-FDG were considered to be active lesions. In patients who had completed treatment, the basis of declaring them healed was documented. Neural improvement in the outcome was documented. These patients were evaluated every 6 months till 2 years after completion of treatment.
RESULTS
A total of 51 patients (17 M:34 F) with mean age 26.8 years (+ SD 10.57) (range 15–54 years) of TB Spine were enrolled. 28 patients were in group A while 23 patients were in group B. All the patients had a history of constitutional symptoms (evening rise of temperature, back pain, loss of weight, and appetite). The mean duration of symptoms was 8.9 months before reporting.
The diagnosis was made clinicoradiologically and on MRI in 36 patients. Tissue was procured in 15 patients with histopathology, in 9 patients and PCR and culture were done. In five patients aspirate from the soft tissue abscess was sent for acid-fast bacilli (AFB) smear, culture and PCR; and in one patient CT guided biopsy was done. PCR and AFB smear was found to be positive in all cases while there was no growth on culture. The diagnostic yield of histopathology or PCR was 100%.
One hundred and forty-seven VB were diseased in 51 patients (mean 2.88 VB range 1–7 VB). Lumbar vertebra was the most commonly involved (n= 27), followed by dorsal spine (n=19) and cervical spine (n=5). There were twenty-four 2-VB lesions, nine 3-VB lesions, and 17 with multiple VB involved. Kyphosis of spine was observed in 18 patients with the mean angle of 29.4° (10–60°).
Eleven patients had different grades of neurological deficit. The mean pretreatment motor score was 66.5 (50–90) which improved to 96.80 (–100) after 8 months of ATT. The mean pretreatment sensory score was 137.4 (–168), which improved to 163.8 (144–168) after 8 months of ATT. Two patients were treated nonoperatively while in nine patients operative intervention was done, one patient showed no neurological recovery and on further followup MRI showed myelomalacia. All other patients had normal neurological status at the end of treatment. All these nine patients had canal encroachment of mean of 65% (range 50–80%) as seen on MRI.
Mean pretreatment hemoglobin level (n=51) was 11.5 + SD 1.25 g/dL with a significant increase to 12.3 + SD1.00 g/dL at the end of 8 months of treatment (P<0.01). The mean ESR level (n=51) was 50 + 16.75 mm First hour reading (FHR) (range 25–110) before treatment with a significant decrease to 25.71 + 12.596 mm FHR, (range 9–55) at 8 months (P <0.01). The mean total protein level (n=51) was found to be 7.07 gm/dL which increased to 7.63 gm/dL at 8 months.
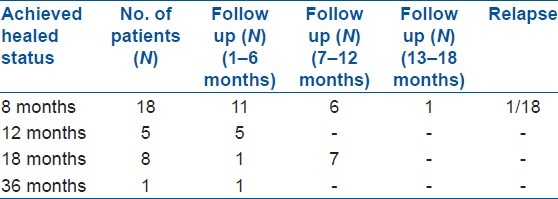
All patients (n=51) completed 8 months of extended category 1 DOTS regimen [Table 1]. Eighteen patients achieved healed status at 8 months while the duration of treatment was increased in 33 patients with persistent active lesions. Treatment was stopped at 8 months in 18 patients. Five patients achieved healing after 12 months of ATT, eight patients after 18 months and one patient was declared healed at 36 months. Thus 32 patients were declared healed at varying periods. The mean duration of treatment in 32 patients, whose treatment was completed, was 12 months (range 8–36 months). Nineteen patients are still on followup.
Table 1.
Details of patients achieved healed status
Overall forty eight patients responded on extended DOTS Category I treatment and were responsive to treatment as seen on clinical, radiological, imaging, and hematological parameters. Three patients were started on category 2 DOTS regimen. One of them had persistence of paravertebral collection and marrow edema after 8 months of ATT. He was advised surgical decompression. But the patient defaulted, refused surgery, and succumbed to acute renal failure after 4 months. The second patient had an appearance of a new lesion in the pectoral muscles on treatment; pus was aspirated and sent for PCR, BACTEC mycobacterial growth indicator tube 960 system culture and sensitivity, and smear examination which showed tubercular bacilli with no growth on Bactec culture. The third patient had grade-4 paraplegia that did not improve after surgical decompression. After 8 months of ATT (category 1) there was appearance of a new vertebral lesion in the cervical spine. This patient was advised category 2 DOTS regimen but was lost to followup.
Out of 18 patients who showed evidence of healing at 8 months have been followed up for the mean duration of 14.4 months (range 10–42 months). They are still being followed up regularly. Recrudescence of disease was seen in one patient after 12 months of completion of treatment, with the appearance of new lesion.
Out of 5 patients who achieved healed status at the end of 12 months of ATT, three patients were followed for the period of 1–3 months, and two patients for the period of 4–6 months. No relapse of disease was seen in this group. Eight patients achieve healed status after 18 months of ATT. Five patients were followed for 12 months, two patients for 10 months, and one patient for 6 months, postcompletion of treatment. One patient was declared healed at 36 months.
DISCUSSION
Before the advent of ATT nearly 75% of patients when treated in sanatorium, used to die or were severely crippled from further complications of disease.1 The introduction of effective ATT allowed bacterial control of the disease and healing of TB spine with residual kyphosis and sequelae of neural complications. The early diagnosis with the introduction of newer imaging modalities and effective antitubercular drugs has reduced the sequelae of neurological deficit and kyphotic deformity.
Both daily dosage drug regimen and intermittent short course chemotherapy are currently in vogue. The duration of regimens varies between 6, 9, 12, or 18 months.5–14 6 or 9 months of chemotherapy with surgical excision had comparable result as that of 18 months of chemotherapy with or without surgery.24 A short course regimen of 9 months was found to be effective in patients with paraplegia.25 Recurrence after 6 months of regimen in patients of TB spine has also been described while no relapses were seen after 9 months of regimen.27 In the absence of reliable serological and immunological markers of healing, the healed status was defined on the basis of clinical and radiological parameters which lags behind the clinical improvement by 3 months by most of the studies.1,4–14 The optimum length of ATT intake can be scientifically established only if the healed status is defined. MRI can demonstrate inflammation early, hence it is useful to diagnose tubercular lesion earlier than other imaging modalities and healing also. We considered MR-based observations as the best evidence of healing and conducted this study.
MRC trials included X-rays of spine and chest, Mantoux test, gastric lavage, pus culture from abscesses, and sinuses in pretreatment evaluation. We established the diagnosis by FNAC/histopathology/culture/PCR. The diagnostic features of TB of spine on MRI were a combination of marrow edema of VB, pre- and paravertebral septate loculated collections, subligamentous collections, epidural extension, end plate erosions and intraosseous abscesses.1,17,21–23,32 MRI criteria for healed status considered are complete resolution of pre- and paravertebral abscess, replacement of marrow edema of the VB by fat or calcification, no residual marrow edema on STIR images. Smith et al.,34 Sharif et al.,31 and Hoffman et al.36 suggested similar features. Gillams et al.37 suggested that high signal intensity rim on T1WI at the edge of lesion and reconstituted fatty marrow which appeared to have equal intensity at both T1 and T2WI phases was suggestive of healing. They also added that progressive reduction and complete disappearance of gadolinium enhancement of bone lesions and of soft tissue as strong evidence of the healing of the lesion. Nene et al.26 (n=69) reported imaging signs of healing on MRI as: regression in size of abscess and granulation tissue, total marrow reconversion and its replacement by fat. We separately evaluated bony lesion and abscess.
Kotil et al.8 reported regression of spondylodiscitis in 30 of 44 patients as the criteria for healing after 12-15 months of chemotherapy. Cormican et al.38 in a retrospective analysis reported mean duration of ATT for 13 months (range of 9–24 months) in 31 patients. MRI evaluation was not done in all patients at followup; diagnostic criteria of healing were not defined. Also variable treatment duration was used. The end point of treatment and criteria of treatment were not defined.
Our 51 patients had characteristic features of TB spine on X-rays and MRI. The histogical/bacteriologies/PCR proof of diagnosis was obtained in 15 cases only. Rajeshwari et al.4 (n=33) obtained specimens during surgery in 23 patients for bacteriological and histopathological examination, wherein only smear was positive in one patient and culture in another while both smear and culture were positive in 12 patients. Kotil et al.8 (n=44) reported positive bacterial culture in 19 patients (43%).
The average number of vertebrae involved in the present study was 2.88 (range 1–7) with total VB as 147. Moon23 (n=56) reported involvement of average 1.78 vertebra (range 1-5). Nene et al. (n=69) involvement of 2.5 vertebrae (range 1–5).26 In the MRC trials average number of vertebra involved was not discussed.
Eighteen patients (35%) in our series had kyphotic deformity with mean angle of 29.4K (range 10–60K). Pathasarthy et al.5 (n=100) reported kyphosis in (42.5%), mean angle of 30° (range 10–60°). MRC trial (n=51) in Korea,20 observed in (100%) mean angle of 20.8° (range 10–60°). Thoracolumbar spine was found to be most commonly involved in the study by, Pathasarthy et al.,5 Kotil et al.,8 and MRC series.
We used PET scan on three occasions where we observed heterogeneous replacement of marrow edema by fat or fatty replacement of vertebral lesion with persistent pre- or paravertebral collection. In one case there was no sign of activity of disease. The disease was found to be active in the vertebral body while in other case vertebral body was found to be healed with persistent psoas abscess showing activity. Use of 18 fluoro-2-deoxy-D-glucose positron emission tomography in assessing the process of tuberculous spondylitis was reported by Schmitz et al. who reported that it can be used to quantify the pathologic increase in glucose metabolism in inflamed tissues. It has a high level of specificity and sensitivity in detecting and identifying chronic osteomyelitis. It has the advantage of higher spatial resolution compared with other nuclear medicine procedures. In addition, it can differentiate between bone and soft tissue infection and allows imaging in the presence of metal implants.39
Treatment was completed in our 32 patients and ATT was stopped and the mean duration of treatment in these patients was 12 months (range 8–36 months). Nene et al.26 (12–27 months), Kotil et al.8 (11–15 months), Ramachandran et al.24 mean 11.2 months (range 6–18 months), Cormican et al.38 mean 13 months (9–24 months) also reported variable duration of treatment. Indian Council of Medical Research and British Medical Research Council in Madras (1989) compared the role of 6 and 9 months of chemotherapy with and without surgery and concluded that 6 or 9 months of HR regimen had better results than previous regimens and surgical debridement did not have favorable result over ambulatory therapy.20,22
In a MRC trial in Korea (1989), radical excision of pathological vertebra was done and patients were given 6 and 9 months of chemotherapy. At the end of 18 months of treatment 76% of patient on 6 months of ATT had favorable results and 85% on 9 months of ATT had favorable results.19 All patients were surgically intervened, while in our study, only patients with severe grade of paraplegia, acute paraplegia, on treatment deterioration of symptoms, no improvement in neurological status after 4–6 weeks on conservative treatment and severe kyphotic deformity were operated. If similar criteria such as no modification in drug regimen, full physical activity, radiologically quiescent spinal disease, no clinically evident sinus, abscess, and no central nervous system involvement would have been used by us then 100% patients would have had a favorable result. In Korea (1993), another MRC trial found that shorter duration of therapy of 6 or 9 months was equally effective as 18 months of chemotherapy. However, once again, the end point of treatment was not defined and even after 36 months of follow up only 82% of patients had achieved favorable status.18
Rajeshwari et al.4 (n=33) emphasized the role of 9 months of short course chemotherapy (SCC) in patients with recent onset paraplegia. They were divided in two phases: Phase 1 (n=10) underwent Hong Kong procedure and then continued on ATT while phase 2 (n=23), 13 patients were given chemotherapy alone while in others (n=10) surgical intervention was also done. Four died during the course of study, thus out of 29 patients 21 were surgically intervened, and 8 patients were kept on chemotherapy only. Thus the number of cases who were treated by chemotherapy was small to define the role of chemotherapy alone. In our study surgical intervention was done in four, out of those declared healed (n=32).
Ramachandran et al.24 (n=38) retrospectively documented that patients of spinal TB on 6 months of ATT have higher relapse rate than in patient given 9 months or more of ATT. However, consecutive cases were not taken and there were no definitive criteria defined for stopping the ATT.
Kotil et al. gave standard chemotherapy (2 months of HRZE+ 13 months of HRE or longer). Cormican et al.38 (n=31) showed mean duration of 13 months (range 9–24). Data were collected retrospectively; treatment was completed in 17 patients. However, the criteria for radiological healing were not defined and the treatment duration was variable. The end point of treatment and criteria of treatment were again not specified.
Moon et al.23 recommended 18 months of chemotherapy in TB of spine. The healed status was defined on X-rays and on improvement of hematological parameters (ESR, CRP). Resolution of disease on X-rays was seen in 69.6% cases and radiological fusion was observed in 87.5% cases at 36 month to monitor progress in healing. We obtained X-rays and MRI at regular intervals till the lesion was declared healed. After completion of 8 months of treatment only 18 (n=51) of our patients (35.2%) had healed vertebral lesion. The improvement in hematological and clinical parameters was observed in all and in remaining 33, although the lesions have regressed with persistence of disease activity based on MRI observations.
With the introduction of DOTS regimen there has been consensus for the dosage of the drugs to be used, but duration is still the issue as relapses have been observed after 6 months of treatment in case of osteoarticular TB.24 One of our patient showed relapse after 12 months of stopping treatment. On treatment new lesions appeared in two patients and there was increase in paravertebral collection in one patient hence were investigated as therapeutically refractory disease.40
Cormican et al.38 had 50% healed patients at end of 9 months of ATT intake, but in this study MRI was not done in all consecutive cases and number of cases were small (n=14). Ramachandran et al.24 reported relapse in five out of eight patients after 6 months of chemotherapy, while no relapse was observed after 9 months of ATT, however, they used clinical examination and X-rays as their diagnostic parameters. MRC trials showed favorable response of 77% after 6 and 9 months of chemotherapy at 18 months followup.
Twelve months of treatment was completed in 38 patients, 5 more patients achieved healed status and thus 23 out of 38 patients were declared healed (60.5%). Nene et al.26 showed 48.5% of 69 patients achieved healed status after 12 months of ATT. Eighteen months of treatment was completed in 33 patients, 8 more patients showed healed lesion. Thus, 31 (93.3%) patients were declared healed out of 33 at the end of 18 months. The result was found to be better than the MRC trials which showed 66% favorable response (no modification in drug regimen, full physical activity, radiologically quiescent spinal disease, no clinically evident sinus, abscess, and no central nervous system involvement) at the end of 18 months, while favorable status was 77% at the end of 18 months in patients given 6 or 9 months of short course chemotherapy.18 In cases where surgical intervention along with chemotherapy was given had favorable status of 84% at the end of 18 months.16,17
In conclusion only 18 (35.2%) patients in our study demonstrated MRI-based healed vertebral lesion at the end of 8 months of extended Category 1 DOTS regimen, while 65% of patients had persistent disease activity and only 60% of those who completed 12 months DOTs category I had shown healed status, in spite of clinical and hematological improvement. Hence, it is suggested not to stop ATT by fixed time frame and we need to evaluate spinal lesions clinically, hematologically, radiologically, and by contrast MRI to document healing of vertebral lesion, after 8 months of ATT and subsequently to decide for the continuation or stoppage of treatment.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Jain AK. Tuberculosis of spine: A fresh look at an old disease. J Bone Joint Surg Br. 2010;92:905–13. doi: 10.1302/0301-620X.92B7.24668. [DOI] [PubMed] [Google Scholar]
- 2.Global Tuberculosis Control: WHO Report. 2010:1–7. [Google Scholar]
- 3.Treatment of tuberculosis: guidelines. 4th ed. 2010. pp. 95–8. [PubMed] [Google Scholar]
- 4.Rajeswari R, Balasubramaniam R, Venkatesan P. Short course chemotherapy in treatment of pott's paraplegia. Int J Tuberc Lung Dis. 1997;1:152–8. [PubMed] [Google Scholar]
- 5.Parthasarthy R, Sriram K, Santha T. Short course chemotherapy for tuberculosis of spine- a comparison between treatment and radical surgery. J Bone Joint Surg Br. 1999;81:464–71. doi: 10.1302/0301-620x.81b3.9043. [DOI] [PubMed] [Google Scholar]
- 6.Guo LX, Ma YZ, Chen X, Bao D, Luo XB. Clinical study of short course chemotherapy in spinal tuberculosis. Zhogguo Gu Shang. 2010;23:491–4. [PubMed] [Google Scholar]
- 7.Tuli SM. Result of treatment of spinal tuberculosis by “middle path” regime. J Bone Joint Surg Br. 1975;57:13–23. [PubMed] [Google Scholar]
- 8.Kotil K, Alan MS. Medical management of pott disease in thoracic and lumbar spine: A prospective clinical study. J Neurosurg Spine. 2007;6:222–8. doi: 10.3171/spi.2007.6.3.222. [DOI] [PubMed] [Google Scholar]
- 9.Park K. Park’ textbook of preventive and social medicine. 18th ed. Jabalpur, India: Banarasidas Bhanot Publishers; 2008. p. 146. 61. [Google Scholar]
- 10.A controlled trial of ambulant out-patient treatment and in patient rest in bed in the management of tuberculosis of the spine in young Korean patients on standard chemotherapy. J Bone Joint Surg Br. 1973;55:678–97. [PubMed] [Google Scholar]
- 11.A controlled trial of plaster of paris jacket in the management of ambulant outpatient treatment of tuberculosis of the spine in children on standard chemotherapy. A study in Pusan. Tubercle. 1973;54:261–82. doi: 10.1016/s0041-3879(73)80030-3. [DOI] [PubMed] [Google Scholar]
- 12.A controlled trial of debridement and ambulant treatment in the management of tuberculosis of the spine in patient on standard chemotherapy in Bulawayo, Rhodesia. J Trop Med Hyg. 1974;77:72–92. [PubMed] [Google Scholar]
- 13.A controlled trial of anterior spinal fusion and debridement in the surgical management of tuberculosis of the spine in patient on standard chemotherapy. A study in Hong Kong. Br J Surg. 1974;61:853–66. doi: 10.1002/bjs.1800611102. [DOI] [PubMed] [Google Scholar]
- 14.A five years assessment of controlled trial of inpatient and outpatient treatment and plaster of Paris jackets in tuberculosis of the spine in children on standard chemotherapy. Studies in Masan and Pusan. J Bone Joint Surg Br. 1976;58-B:399–411. doi: 10.1302/0301-620X.58B4.1018027. [DOI] [PubMed] [Google Scholar]
- 15.A five years assessment of controlled trial of ambulatory treatment, debridement and anterior spinal fusion in the management of tuberculosis of the spine. J Bone Joint Surg Br. 1978;60-B:163–77. doi: 10.1302/0301-620X.60B2.350883. [DOI] [PubMed] [Google Scholar]
- 16.A controlled trial of anterior spinal fusion and debridement in the surgical management of tuberculosis of the spine in patient on standard chemotherapy. A study in two centres in South Africa. Tubercle. 1978;59:79–105. doi: 10.1016/0041-3879(78)90012-0. [DOI] [PubMed] [Google Scholar]
- 17.10 years assessement of anterior spinal fusion and debridement in the surgical management of tuberculosis of the spine in patient on standard chemotherapy in Hong Kong. J Bone Joint Surg Br. 1982;64:393–8. doi: 10.1302/0301-620X.64B4.7047536. [DOI] [PubMed] [Google Scholar]
- 18.A 10 years assessment of controlled trial of inpatient and outpatient treatment and plaster of Paris jackets in tuberculosis of the spine in children on standard chemotherapy. J Bone Joint Surg Br. 1985;67B:103–10. doi: 10.1302/0301-620X.67B1.2857181. [DOI] [PubMed] [Google Scholar]
- 19.A controlled trial of 6 months and 9 months regimens of chemotherapy in patients undergoing radical surgery for TB spine in Hong Kong. Tubercle. 1986;67:243–59. doi: 10.1016/0041-3879(86)90014-0. [DOI] [PubMed] [Google Scholar]
- 20.Controlled trial of short course regimen of chemotherapy in the ambulatory treatment of spinal tuberculosis. Results at 3 years of study in Korea. J Bone Joint surg Br. 1993;75:240–8. doi: 10.1302/0301-620X.75B2.8444944. [DOI] [PubMed] [Google Scholar]
- 21.15 year assessment of controlled trials of short course chemotherapy regimens of 6, 9 and 18 months duration for spinal tuberculosis in patients ambulatory from the start of undergoing radical surgery. Int J Orthop. 1999;23:73–81. doi: 10.1007/s002640050311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.A controlled trial of short course regimen of chemotherapy in patients receiving ambulatory treatment or undergoing radical surgery for tuberculosis of the spine. Indian J Tuberc. 1989;36(supp):1–21. [Google Scholar]
- 23.Moon MS, Moon YW, Moon JL, Kim SS, Sun DH. Conservative treatment of tuberculosis of the lumbar and lumbo sacral spine. Clin Orthop Relat Res. 2002;398:40–9. doi: 10.1097/00003086-200205000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Ramachandran S, Clifton IJ, Collyns TA, Watson JP, Pearson SB. The treatment of spinal tuberculosis: a retrospective study. Int J Tuberc Lung Dis. 2005;9:541–44. [PubMed] [Google Scholar]
- 25.Upadhyay SS, Saji MJ, Yau AC. Duration of antitubercular chemotherapy in conjunction with radical surgery in the management of spinal tuberculosis. Spine. 1996;21:1898–903. doi: 10.1097/00007632-199608150-00014. [DOI] [PubMed] [Google Scholar]
- 26.Nene A, Bhojraj S. Results of non surgical treatment of thoracic spinal tuberculosis in adults. Spine J. 2005;5:79–84. doi: 10.1016/j.spinee.2004.05.255. [DOI] [PubMed] [Google Scholar]
- 27.Tuli SM. Tuberculosis of the skeletal system. 4th ed. New Delhi: Jaypee Brothers; 2004. pp. 3–5. (25-41, 200-27, 239-99). [Google Scholar]
- 28.Jain AK, Sinha S. Evaluation of system of grading of neurological deficit in tuberculosis of spine. Spinal Cord. 2005;43:375–80. doi: 10.1038/sj.sc.3101718. [DOI] [PubMed] [Google Scholar]
- 29.Bhan S, Nag HL. Skeletal Tuberculosis. In: Sharma SK, Mohan A, editors. Tuberculosis. 2nd ed. New Delhi, India: Jaypee Brothers Medical Publishers; 2009. [Google Scholar]
- 30.Desai SS. Early diagnosis of spinal tuberculosis by MRI. J Bone Joint Surg Br. 1994;76:863–9. [PubMed] [Google Scholar]
- 31.Sharif HS, Clark DC, Aabed MY, Haddad MC, al Deeb SM, Yaqub B, et al. Granulomatous spinal infections: MR imaging. Radiology. 1990;177:101–7. doi: 10.1148/radiology.177.1.2399306. [DOI] [PubMed] [Google Scholar]
- 32.Andronikou S, Jadwat S, Douis H. Patterns of disease on MRI in 53 children with tuberculous spondylitis and the role of gadolinium. Pediatr Radiol. 2002;32:798–805. doi: 10.1007/s00247-002-0766-8. [DOI] [PubMed] [Google Scholar]
- 33.Jain AK, Sreenivasan R, Saini NS, Kumar S, Jain S, Dhammi IK. Magnetic resonance evaluation of tubercular lesion in spine. Int Orthop. 2012;36:261–9. doi: 10.1007/s00264-011-1380-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smith AS, Weinstein MA, Mizushima A, Coughlin B, Hayden SP, Lakin MM, et al. MR imaging characteristics of tuberculous spondylitis vs vertebral osteomyelitis. AJR Am J Roentgenol. 1989;153:399–405. doi: 10.2214/ajr.153.2.399. [DOI] [PubMed] [Google Scholar]
- 35.Lee IS, Lee JS, Kim SJ, Jun S, Suh KT. Fluorine-18-fluorodeoxyglucose positron emission tomography/computed tomography imaging in pyogenic and tuberculous spondylitis: Preliminary study. J Comput Assist Tomogr. 2009;33:587–92. doi: 10.1097/RCT.0b013e318187fef8. [DOI] [PubMed] [Google Scholar]
- 36.Hoffman EB, Crosier JH, Cremin BJ. Imaging in children with spinal tuberculosis. A comparison of radiography, computed tomography and magnetic resonance imaging. J Bone Joint Surg Br. 1993;75:233–9. doi: 10.1302/0301-620X.75B2.8444943. [DOI] [PubMed] [Google Scholar]
- 37.Gillams AR, Chaddha B, Carter AP. MR appearance of temporal evolution and resolution of infectious spondylitis. Am J Roentgenol. 1996;166:903–7. doi: 10.2214/ajr.166.4.8610571. [DOI] [PubMed] [Google Scholar]
- 38.Cormican L, Hammal R, Messenger J, Milburn HJ. Current difficulties in the diagnosis and management of spinal tuberculosis. Postgrad Med J. 2006;82:46–51. doi: 10.1136/pgmj.2005.032862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schmitz A, Kälicke T, Willkomm P, Grünwald F, Kandyba J, Schmitt O. Use of fluorine-18 fluoro-2-deoxy-D-glucose positron emission tomography in assessing the process of tuberculous spondylitis. J Spinal Disord. 2000;13:541–4. doi: 10.1097/00002517-200012000-00016. [DOI] [PubMed] [Google Scholar]
- 40.Jain AK, Dhammi IK, Modi P, Kumar J, Sreenivasan R, Saini NS. Tuberculosis spine: Therapeutically refractory disease. Indian J of Orthop. 2012;46:171–8. doi: 10.4103/0019-5413.93685. [DOI] [PMC free article] [PubMed] [Google Scholar]


