Abstract
Background:
Posterior heel pain due to retrocalcaneal bursitis, is a disabling condition that responds well to the conventional methods of treatment. Patients who do not respond to conservative treatment may require surgical intervention. This study evaluates the outcome of endoscopic decompression of retrocalcaneal bursitis, with resection of posterosuperior eminence of the calcaneum.
Materials and Methods:
This present study included 25 heels from 23 consecutive patients with posterior heel pain, who did not respond to conservative treatment and underwent endoscopic decompression of the retrocalcaneal bursae and excision of bony spurs. The functional outcome was evaluated by comparing the pre and postoperative American Orthopedic Foot and Ankle Society (AOFAS) scores. The Maryland ankle and foot score was used postoperatively to assess the patient's satisfaction at the one-year followup.
Results:
The University of Maryland scores of 25 heels were categorized as the nonparametric categories, and it was observed that 16 patients had an excellent outcome, six good, three fair and there were no poor results. The AOFAS scores averaged 57.92 ± 6.224 points preoperatively and 89.08 ± 5.267 points postoperatively (P < 0.001), at an average followup of 16.4 months. The 12 heels having noninsertional tendinosis on ultrasound had low AOFAS scores compared to 13 heels having retrocalcaneal bursitis alone. At one year followup, correlation for preoperative ultrasound assessment of tendoachilles degeneration versus postoperative Maryland score (Spearman correlation) had shown a strong negative correlation.
Conclusion:
Endoscopic calcaneal resection is highly effective in patients with mild or no degeneration and yields cosmetically better results with fewer complications. Patients with degenerative changes in Achilles tendon had poorer outcomes in terms of subjective satisfaction.
Keywords: Endoscopic decompression, noninsertional Achilles tendinosis, retrocalcaneal bursitis, ultrasound
INTRODUCTION
Retrocalcaneal bursitis (RCB) is a disabling condition characterized by pain that is anterior to the Achilles tendon, and just superior to its insertion in the os calcis.1 The retrocalcaneal bursa lies between the anterior aspect of the tendon and the posterosuperior aspect of the calcaneum.
Patrick Haglund (1928) was credited for the first description of enlargement of the posterosuperior portion of the calcaneus;2 the syndrome bearing his name has come to represent a painful condition of the heel caused by mechanically induced inflammation of the retrocalcaneal and / or supracalcaneal bursae, which become inflamed, hypertrophied, and adherent to the underlying tendon.3
Examination reveals painful dorsiflexion of the ankle and tenderness on either side or anterior aspect of the Achilles tendon. The lateral view radiograph of the ankle joint shows posterosuperior bony prominence and intratendinous calcification that confirms the diagnosis. The tendon degenerative changes can also be demonstrated by using an ultrasound scan.4
Various modalities of conservative treatment have been recommended, including change of footwear, use of heel pads, moist heat, stretching exercises, local steroid injections, and extracorporeal shock wave therapy.5–7 In cases where conservative treatment fails, surgery may be indicated. Several methods of surgical treatment have been described previously including excision of the retrocalcaneal bursa, calcaneal osteotomy, and endoscopic decompression of the retrocalcaneal space.8–10
Minimally invasive surgeries allow early postoperative recovery, minimal pain, and better cosmetic appearance, but the results are inconsistent.11 We report the outcome of the endoscopic decompression of retrocalacaneal bursa and posterosuperior bony spur and compared the results in patients with retrocalcaneal bursitis alone, with those having additional limited intratendinous calcifications (X-ray finding), and noninsertional tendinosis (ultrasound finding).
MATERIALS AND METHODS
Patients
This prospective study was conducted from May 2008 to August 2011 and included 25 heels of 23 patients (two patients with both heels) in 9 men and 14 women attending the Outpatient Department at our hospital, with posterior heel pain, who did not respond to conservative treatment and had symptomatic Haglunds spur and / or noninsertional Achilles tendinosis. Endoscopic decompression was performed on these patients. The mean age was 51.44 ± 7.92 years (range 38 – 66 years). The average duration of the nonoperative treatment before the surgery was 13.40 ± 6.67 months (range 6 – 30 months). Failed conservative treatment included modified footwear, nonsteroidal anti inflammatory agents (NSAID), physical therapy, and steroid injections (in other institutions). No patient had previous hind foot surgery. Patients were evaluated with preoperative clinical examination, routine blood investigations, X-rays, and ultrasound scan, to rule out insertional tendinitis and degenerative changes. Patients with severe calcific deposits and insertional tendinitis were excluded from the study.12 Functional outcome was evaluated AOFAS. The Maryland ankle and foot score was used postoperatively to assess patient satisfaction.
A standing, lateral view of plain X-ray was taken preoperatively, to assess the posterosuperior bony spur,13 (which was present in all patients) and to calculate the extent of bony resection required. Out of 23 patients, seven had Achilles tendon calcification ranging from minima to moderate grade.
The parallel pitch lines (PPLs) determine the prominence of the bony projection on preoperative X-ray [Figure 1a]. The lower PPL (A) is the baseline, drawn from the anterior tubercle to the medial posterior tubercle. The upper PPL (B) is drawn parallel to the baseline at a distance D, starting from the talar articular surface anteriorly to the posterior tuberosity. A bony projection touching or below line B is normal and not prominent (PPL-negative) and a bony projection above B is considered prominent (PPL-positive), which needs surgical excision. Both preoperative and postoperative x-rays were compared, to determine the extent of resection.
Figure 1.
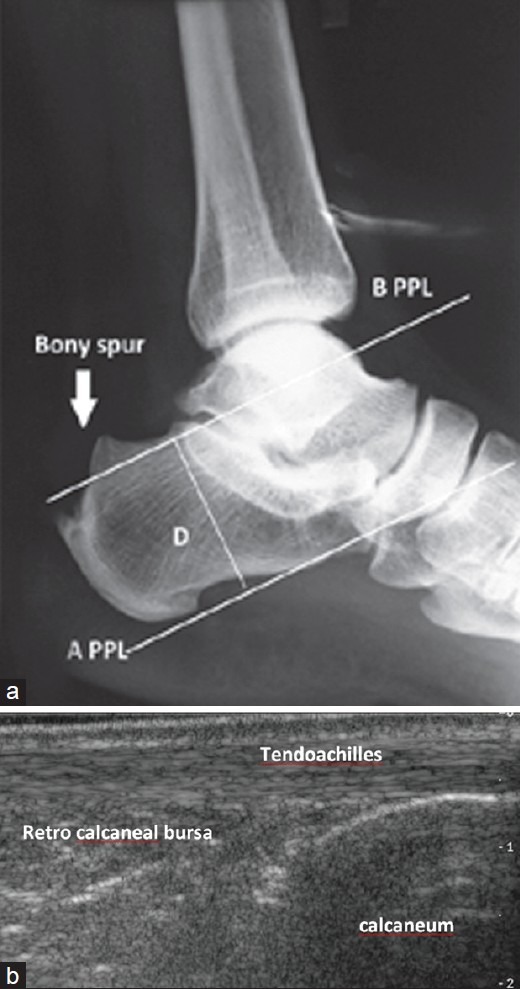
Preoperative X-ray ankle joint lateral view showing (a) the parallel pitch lines (PPLs) determine the prominence of the bony projection. (b) Ultrasound ankle showing Achilles Tendon, Retrocalcaneal bursa and Calcaneum
Ultrasound evaluation
Achilles tendon and the surrounding tissues were examined with the patient in a prone position by the same radiologist using high-frequency (13 MHz) linear transducer (Siemens Medical Systems) [Figure 1b]. Based on the hypoechoic areas in the tendon substance, grading was done using the ordinal scale,12 whereby, 0 represented normal echogenicity, 1 represented mild hypoechogenicity, 2 represented moderate hypoechoic regions, and 3 represented marked hypoechogenicity.
The presence or absence of intratendinous calcification was documented by identifying the linear areas of hyperechogenicity within the tendon proper.12 Patients with grade 3 tendinosis (degeneration) and severe calcification were excluded from the study.
Scoring
The AOFAS ankle-hindfoot scale was used to evaluate patients preoperatively and postoperatively at three weeks, six weeks, six months, and twelve months respectively. The AOFAS score evaluates pain (40 points), function (50 points), and alignment (10 points).14
The Maryland 100 point foot score was used only postoperatively at the six and 12-month followups. For validation of the subjective satisfaction of the patients for better patient understanding10 the Maryland foot score was translated to the local language. Both preoperative and postoperative evaluations were performed by a single investigator, to avoid interobserver errors.
Statistical analysis
The data was analyzed using the Statistical Package for Social Sciences (SPSS) version 11.0. Frequencies and proportions were calculated and the mean (± Standard Deviation) values were calculated for continuous variables, such as, age, duration of conservative treatment before surgery, preoperative and postoperative scores, duration of surgery, and followup.
The paired ‘t’ test was done wherever applicable, to compare the preoperative and postoperative scores. Spearman correlation was performed to evaluate the relationship between preoperative ultrasound findings and postoperative Maryland scores.
Operative procedure
The endoscopic procedure was performed with the patient in a prone or semi-prone position, with the foot hanging down the table, under spinal anesthesia and tourniquet control [Figure 2]. A medial portal (working portal) was made and an arthroscopic shaver (4.0 mm Stryker) was introduced for removing the fat and retrocalcaneal bursa, and the lateral portal was used for visualization, (Stryker endoscopy video system and 30° scope). Osseous resection was done with a burr under endoscopic guidance, to avoid injury to the Achilles tendon. The resection was carried out distally and anteriorly, to meet the preoperative goals. The fragments were irrigated and suctioned from the wound. The tendon was then visualized with an endoscope and if necessary, the diseased Achilles tissue was debrided with the shaver. Up to 50% of the Achilles tendon could be released safely for complete removal of the spur.15 Wound closure was done with 2-O nylon in a single layer and tight compressive dressing was applied till a middle third of the leg. Postoperatively, weight bearing was not allowed for two weeks. Subsequently, the patients were allowed to walk with modified footwear for three months, followed by normal footwear.
Figure 2.

Peroperative clinical photograph showing medial and lateral portals with patient's foot hanging free in a prone position
RESULTS
Radiographs
The post operative X-rays in all patients showed adequate resection of the bony spur. The resection angle was not measured on postoperative X-rays [Figure 3a]. Minimal bony debris, which was not removed during surgery, was visible in a few postoperative radiographs and there was no evidence of heterotrophic calcification at one year followup.
Figure 3.
(a) The postoperative fluoroscopy view showing adequate resection of the bony spur. (b and c) Clinical photograph showing postoperative scar at the one-year followup
Scores
The mean followup was 16.4 months (range 12-30 months). The average preoperative AOFAS score of 57.92 ± 6.224 points and postoperative score of 89.08 ± 5.267 points, indicating a significant increase in the scores after the operation (P < 0.01).
The University of Maryland scores averaged 90.28 ± 5.77 during followup at 12 months. The University of Maryland scores were categorized into nonparametric categories, with 100 to 90 points indicating an excellent score; 89 to 80 points – good; 79 to 70 points – fair; and < 70 points – poor.10 It was observed that 16 patients had an excellent outcome, six good, three fair, and there were no poor results.
In our study, there were 12 heels having noninsertional tendinosis on ultrasound and they had low AOFAS scores compared to 13 heels having retrocalcaneal bursitis alone. The six patients who demonstrated calcification on radiographs, in addition to ultrasound changes, had less pain relief at the one year followup, compared to those with ultrasound changes alone.
At the one year followup, correlation for preoperative USG assessment of tendoachilles degeneration versus a postoperative Maryland score (Spearman correlation) has shown a strong negative correlation. As the USG grade of degeneration (grade 2) increased, the postoperative score decreased and the association was significant (P < 0.01). One patient had postoperative wound infection, which healed with secondary intention, two had sural neuropathy probably due to improper lateral port placement and one had DVT that resolved in two weeks, after a medical line of management [Figure 3b].
DISCUSSION
Posterior heel pain is multifactorial and the causes include, retrocalcaneal bursitis, insertional tendinosis, noninsertional tendinosis, superficial retroachilles bursitis, and gastrocnemius contracture. Achilles tendinopathy is a degenerative process within the tendon substance causing microtears and reactive fibrotic scar formation that causes mechanical irritation of the surrounding tissues, followed by inflammatory reaction and attenuated repair.16
The tendon disease can be more proximal (noninsertional) or at the level of insertion, adjacent to the prominent bone. After the initial inflammatory stage, the tendinopathy progresses to a tendonosis (intrasubstance tendon fiber degeneration), where conservative measures are less likely to have a significant effect.17 Histopathologically, noninsertional Achilles tendinitis is classified into three subgroups: paratendinitis, paratendinitis with tendinosis, and tendinosis by Puddu et al.18 It is clinically difficult to differentiate the contribution of insertional Achilles tendinitis, noninsertional tendinosis (tendon substance degeneration), and retrocalcaneal bursitis to cause pain in most patients, as they often co-exist. Treatment of Achilles tendinosis can be planned depending on the stage of degeneration, eccentric calf strengthening for mild and moderate tendinosis and debridement of tendon with reconstruction for severe tendinosis. Radiographs can give an idea about the bony morphology (posterosuperior spur) and tendon calcification, but not the tendon substance details. Ultrasound is used commonly to examine Achilles tendon disorders,19–21 and it is a better option when compared to magnetic resonance imaging (MRI), as it allows dynamic assessment and reveals the details of the tendon and inflamed bursae more accurately.22 It also picks degeneration (calcification) of the tendon before the changes appear on the radiographs.
In our series, radiographs of noninsertional tendinosis of 12 heels demonstrated six normal, five mild, and one moderate calcification, while the ultrasound demonstrated moderate degeneration in six and mild in the rest, proving that the ultrasound can help in diagnosing noninsertional tendinosis before the changes appear on the radiographs.
The group with ultrasound changes alone had a better functional outcome than the group with calcification on radiographs, in addition to ultrasound changes. Hence, we strongly believe that ultrasound examination preoperatively is helpful in getting the finer details of the Achilles tendon, than those that appear on radiographs and it helps in choosing the ideal patient for endoscopic decompression.
Leitz et al.10 performed a prospective study comparing open resection in 17 patients with the endoscopic technique in 33 patients. They found that in the endoscopic group, the AOFAS scores averaged 61.8 points preoperatively and 87.5 points postoperatively, and the results were similar to ours. Ortmann et al.16 reported on 30 patients (32 heels), who were managed with endoscopic osseous and soft tissue decompression for the treatment of retrocalcaneal bursitis. Twenty five patients had an excellent result, and three had a good result. Our study showed similar results, in terms of patient satisfaction with the use of the Maryland score at the one year followup. A limitation of this study was that the sample size was very small and the average followup was only-16.4 months.
In conclusion, endoscopic calcaneal resection is highly effective in patients with no degeneration than the patients with degenerative changes. It yields cosmetically better results with fewer complications as the procedures allow better visualization of the bony spur and resect adequately. Preoperative ultrasound is very helpful in identifying the ideal patient for endoscopic procedure and helps to predict the prognostic outcome following endoscopic decompression to a certain extent.
ACKNOWLEDGMENT
Thanks to Dr. Rajeshwar Rao for helping with statistics.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Sharma SC, Singh R, Piplani H, Sharma A. Radiological Evaluation and Role of Surgery in Retrocalcaneal Bursitis. Hong Kong J Orthop Surg. 2005;9:8–15. [Google Scholar]
- 2.Haglund P. BeitragzurKlinik der Achillessehne. Z Orthop Chir. 1928;49:49–58. [Google Scholar]
- 3.Schepsis AA, Wagner C, Leach RE. Surgical management of Achilles tendon overuse injuries. A long term followup study. Am J Sports Med. 1994;22:611–9. doi: 10.1177/036354659402200508. [DOI] [PubMed] [Google Scholar]
- 4.Carolyn MS, Ronald SA, Rock P, Helene P, Jonathan SL. Haglund's syndrome: Diagnosis and treatment using sonography. HSS J. 2006;2:27–9. doi: 10.1007/s11420-005-0129-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lowdon A, Bader DL, Mowat AG. The effect of heel pads on the treatment of Achilles tendinitis: A double blind trial. Am J Sports Med. 1984;12:431–5. doi: 10.1177/036354658401200605. [DOI] [PubMed] [Google Scholar]
- 6.Fredberg U. Local corticosteroid injection in sport: Review of literature and guidelines for treatment. Scand J Med Sci Sports. 1997;7:131–9. doi: 10.1111/j.1600-0838.1997.tb00129.x. [DOI] [PubMed] [Google Scholar]
- 7.Furia JP. Highenergy extracorporeal shock wave therapy as a treatment for insertional Achilles tendinopathy. Am J Sports Med. 2006;34:733–40. doi: 10.1177/0363546505281810. [DOI] [PubMed] [Google Scholar]
- 8.Anderson JA, Suero E, O’Loughlin PF, Kennedy JG. Surgery for retrocalcaneal Bursitis a Tendon splitting versus a lateral approach. Clin Orthop Relat Res. 2008;466:1678–82. doi: 10.1007/s11999-008-0281-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brunner J, Anderson J, O’Malley M, Bohne W, Deland J, Kennedy J. Physician and patient based outcomes following surgical resectionof Haglund's deformity. Acta Orthop Belg. 2005;71:718–23. [PubMed] [Google Scholar]
- 10.Leitze Z, Sella EJ, Aversa JM. Endoscopic decompression of the retrocalcaneal space. J Bone Joint Surg Am. 2003;85:1488–96. doi: 10.2106/00004623-200308000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Weil LS. Minimal invasive surgery of the foot and ankle. J Foot Ankle Surg. 2001;40:61. doi: 10.1016/s1067-2516(01)80046-6. [DOI] [PubMed] [Google Scholar]
- 12.Ryan M, Wong A, Taunton J. Favorable outcomes after sonographically guided intratendinous injection of hyperosmolar dextrose for chronic insertional and midportion Achilles tendinosis. AJR Am J Roentgenol. 2010;194:1047–53. doi: 10.2214/AJR.09.3255. [DOI] [PubMed] [Google Scholar]
- 13.van Sterkenburg MN, Muller B, Maas M, Sierevelt IN, van Dijk CN. Appearance of the weight-bearing lateral radiograph in retrocalcaneal bursitis. Acta Orthop. 2010;81:387–90. doi: 10.3109/17453674.2010.487245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349–53. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 15.Kolodziej P, Glisson RR, Nunley JA. Risk of avulsion of the Achilles tendon after partial excision for treatment of insertional tendonitis and Haglund's deformity: A biomechanical study. Foot Ankle Int. 1999;20:433–7. doi: 10.1177/107110079902000707. [DOI] [PubMed] [Google Scholar]
- 16.Ortmann FW, McBryde AM. Endoscopic bony and soft-tissue decompression of the retrocalcaneal space for the treatment of Haglund deformity and retrocalcaneal bursitis. Foot Ankle Int. 2007;28:149–53. doi: 10.3113/FAI.2007.0149. [DOI] [PubMed] [Google Scholar]
- 17.Giza E, Sullivan M. Endoscopic calcaneo-bursectomy. Foot Ankle Spec. 2008;1:112–4. doi: 10.1177/1938640008316556. [DOI] [PubMed] [Google Scholar]
- 18.Puddu G, Ippolito E, Postacchini F. A classification of Achilles tendon disease. Am J Sports Med. 1976;4:145–50. doi: 10.1177/036354657600400404. [DOI] [PubMed] [Google Scholar]
- 19.Maffulli N, Regine R, Angelillo M, Capasso G, Filice S. Ultrasound diagnosis of Achilles tendon pathology in runners. Br J Sports Med. 1987;21:158–62. doi: 10.1136/bjsm.21.4.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fornage BD. Achilles tendon: US examination. Radiology. 1986;159:759–64. doi: 10.1148/radiology.159.3.3517959. [DOI] [PubMed] [Google Scholar]
- 21.Paavola M, Paakkala T, Kannus P, Järvinen M. Ultrasonography in the differential diagnosis of Achilles tendon injuries and related disorders. A comparision between preoperative ultrasonography and surgical findings. Acta Radiol. 1998;39:612–9. doi: 10.3109/02841859809175485. [DOI] [PubMed] [Google Scholar]
- 22.Warden SJ, Kiss ZS, Malara FA, Aoi AB, Cook J, Crossley KM. Comparative accuracy of magnetic resonance imaging and ultrasonography in confirming clinically diagnosed patellar tendinopathy. Am J Sports Med. 2007;35:427–36. doi: 10.1177/0363546506294858. [DOI] [PubMed] [Google Scholar]



