Abstract
Background:
The Bankart lesion represents the most common form of labro-ligamentous injury in patients with traumatic dislocations of the shoulder leading to shoulder instability. We report the clinical outcome of arthroscopic repair of Bankart lesion in 50 patients.
Materials and Methods:
Sixty five patients with posttraumatic anterior dislocation of shoulder were treated by arthroscopic repair from Jan 2005 to Nov 2008. Fifty patients, with an average age of 26.83 years (range 18-45 years), were reviewed in the study. The average followup period was 27 months (range 24-36 months). University of California Los Angeles shoulder rating scale was used to determine the outcome after surgery. The recurrence rates, range of motion, as well as postoperative function and return to sporting activities were evaluated.
Results:
Thirty six patients (72.0%) had excellent results, whereas seven patients (14.0%) had good results. The mean pre- and postoperative range of external rotation was 80.38° and 75.18°, respectively. Eighty-six percent patients had stability compared with the normal sided shoulder and were able to return to sports. There were no cases of redislocation observed in this study; however, three cases had mild laxity of the joint.
Conclusion:
Arthroscopic Bankart repair with the use of suture anchors is a reliable treatment method, with good clinical outcomes, excellent postoperative shoulder motion and low recurrence rates.
Keywords: Arthroscopic repair, Bankart lesion, shoulder instability
INTRODUCTION
Shoulder, by virtue of its anatomy and biomechanics, is one of the most unstable and frequently dislocated joints in the body.1 Bankart2 (1920) published a paper stating that in acute dislocations the humeral head is forced anteriorly out of the glenoid cavity and tears not only the fibrocartilaginous labrum from almost the entire anterior half of the rim of glenoid cavity, but also the capsule and periosteum from anterior surface of the neck of scapula. This traumatic detachment of glenoid labrum has been called the Bankart lesion. The Bankart lesion represents the most common form of labro-ligamentous injury in patients with traumatic dislocations of the shoulder. Surgical treatment is by reattachment of the labro-ligamentous complex to the glenoid either arthoscopically or during an open procedure (Bankart repair).3
Several open and arthroscopic techniques have been described to address anterior shoulder instability. These procedures address both capsulo-ligamentous laxity and labral pathologies via a variety of instruments, suture passages, knot-tying techniques, and fixation devices. With the debate continuing regarding the indications for arthroscopic shoulder stabilization, several studies have shown favorable outcomes with regard to the arthroscopic method.4–6 Moreover, with continuing criticisms with regard to the wide dissection, loss of external rotation, and postoperative pain associated with the open repair, the demand for arthroscopic surgery has increased over the past two decades. Arthroscopic Bankart repair for the treatment of instability of the shoulder has become increasingly popular as it is less invasive than open surgery and produces a better surgical outcome including range of movement and function.6
We report here a retrospective analysis of arthroscopic Bankart repair in posttraumatic recurrent anterior dislocation of shoulder.
MATERIALS AND METHODS
Sixty five non consecutive patients with posttraumatic anterior dislocation of shoulder were treated by arthroscopic repair from January 2005 to November 2008, out of them fifty patients who fulfilled the inclusion criterion were reviewed in the study.
Patients of both the sexes, in the age group of 15-50 years, with anterior instability of the glenohumeral joint, which interfered with activities of daily living or athletic activity and having at least two episodes of dislocations, a positive clinical apprehension test and radiological evidence of glenohumeral dislocation were taken up for the study.
Patients who were excluded from the study were those who were medically unfit for surgery or had either posterior, inferior, or multidirectional instability or habitual dislocation. Those with previously failed arthroscopic or open surgery or with fractures involving >30% of articular surface of gleniod or posterolateral humeral head (engaging Hill Sachs lesion), and having other unrelated conditions like rotator cuff tears were also not included in the study.
Patients who presented to the hospital with acute dislocation were managed by immediate close reduction under general anesthesia using the traction-countertraction technique. The reduction was confirmed radiologically and the shoulder joint was immobilized by using a shoulder immobilizer and the patients were asked to return for review in the sports injury center of the hospital.
On followup visit at the sports injury center, the patients were subjected to a through history and clinical examination, which gave a good idea about the etiology, direction, and frequency of dislocation. This was supplemented by good quality radiographs in antero-posterior, lateral, axillary, and scapular Y view to rule out any bony Bankart or significant Hill Sachs lesion. During the study, 18 patients needed magnetic resonance imaging (MRI), due to a discrepancy between the clinical history, examination findings, and the radiographs. MRI detected a high grade Hill Sachs lesion in four patients and rotator cuff tear in three patients, which led to their exclusion. The clinical and radiological findings in all the patients were supported by a diagnostic arthroscopy performed before the procedure. In none of the study subjects were the findings contrary to what we had thought of preoperatively.
The patients were explained regarding the procedure, its outcome, complications, and the prolonged rehabilitation protocol. The patients were included in the study after obtaining written, informed consent. Preoperatively we compared the laxity of the affected shoulder with the other side. This comparison was also done postoperatively giving us a baseline against which the results were evaluated.
Modified University of California Los Angeles (UCLA)7–9 scale was used to evaluate the effectiveness of the arthroscopic Bankart repair. The scale was used to evaluate the patient's pain, function, active forward flexion, strength in forward flexion, and patient satisfaction. The maximum total score possible is 35, with a higher score indicating better shoulder function. We assigned a score of 34-35 points as excellent, 28-33 points as good, 21-27 as mild, and 20 or less as poor. Excellent and good scores were taken as satisfactory.
The patients were followed up at 2 weeks, 1 month, and then at 6 monthly intervals. All patients had a minimum of 2 years followup. Treatment failure was regarded as recurrent shoulder dislocation, any sensation of subluxation or instability preventing return to full activity or requiring a further stabilizing procedure.
OPERATIVE PROCEDURE
After induction of general anesthesia, a thorough clinical examination was performed to assess the magnitude and direction of instability. The patient was placed in a lateral decubitus position with arm position between 40° and 60° of abduction and 20° to 30° of forward flexion. All pressure points were padded and traction of 10-13 lb was applied. Peripheral pulses and pulse oximeter readings were evaluated to ensure that axillary structures were not compromised. The shoulder was prepared and draped in a sterile manner, and the bony landmarks were marked carefully to maintain orientation throughout the procedure.
A standard posterior viewing portal was established approximately 2 cm inferior and 1 cm medial to the acromial angle. Two anterior portals were established using outside-in technique with a spinal needle to establish the most appropriate placement of the cannulas. The antero-superior portal was made in the rotator interval just inferior to the anterior edge of the acromion, and the anterior midglenoid portal was made just over the superior border of the subscapularis tendon. A small cannula (internal diameter 5.5 mm) was inserted into the antero-superior portal, and a large (internal diameter 8.2 mm) threaded cannula was placed in the anterior midglenoid portal. Complete diagnostic arthroscopy was done through the posterior and anterior portals, with assessment of the glenoid labrum, capsule, rotator cuff, and the humeral head for possible Hill Sachs lesions. The Bankart lesion was mobilized from the anterior glenoid surface using a periosteal elevator. The goal was to mobilize the labrum such that it could be shifted superiorly and laterally. The glenoid neck was lightly abraded using a rasp.
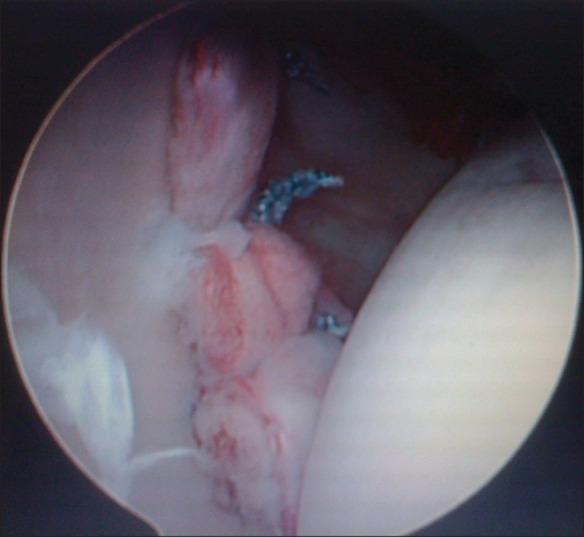
All suture anchors used in the study were obtained from Arthrex. The Bio-suture Tak is a 3 mm diameter by 14.5 mm long bio-absorbable “push-in” anchor. This suture anchor is molded from poly L-lactide-co-D, L-lactide (PLDLA), which is a noncrystalline, bio-absorbable copolymer. The anchor was loaded with No.2 Fibrewire, which is a braided, nonabsorbable, polyblend suture. The first anchor was placed at the 5.00 o’clock position for the left shoulder and 7.00 o’clock for the right shoulder, care was taken to ensure that the suture anchors are placed on the glenoid face, centered about 2-3 mm from the edge of the glenoid cartilage. Anchors placed more medial than this risk restoration of the glenoid labrum in a nonanatomic medialized position that will not restore the normal bumper effect of the anterior labrum. The suture anchor used required drilling a pilot hole or using a punch to create the pilot hole prior to impaction of the implant to a countersunk position in the bone. A suture passer was then passed under the Bankart lesion. The strand of the suture anchor nearer the labrum was brought out through the antero-superior portal, and in turn through the labrum in a retrograde fashion using the suture passer and retrieved from the midglenoid portal. This suture limb remained as the post during suture tying and this would ensure that the knot rest on the capsular side of the glenoid labrum and not on the articular side. This technique would effectively push the labrum up toward the glenoid socket, restoring labral height and thereby recreating the labral bumper [Figures 1–4]. The second and third suture anchors were done at the 4.00 and 3.00 o’clock positions for the left shoulder and 8.00 and 9.00 o’clock position for the right, in the same manner. The sutures were tied using the Tennessee slider knot, which is easy to tie, has a low profile, and possesses good holding strength10 secured by a series of three reversing half-hitches on alternating posts.
Figure 1.

Arthroscopic view showing probe under the torn anterior labrum of a Bankart lesion
Figure 4.
Arthroscopic view showing a completed repair with anchors in positions, Note the position of the knots on the capsular side of the repair and the restoration of an anterior bumper effect by the labrum
Figure 2.

Arthroscopic view showing inserting the bioabsorbable suture anchor preloaded with nonabsorbable suture through the anterior-inferior portal
Figure 3.
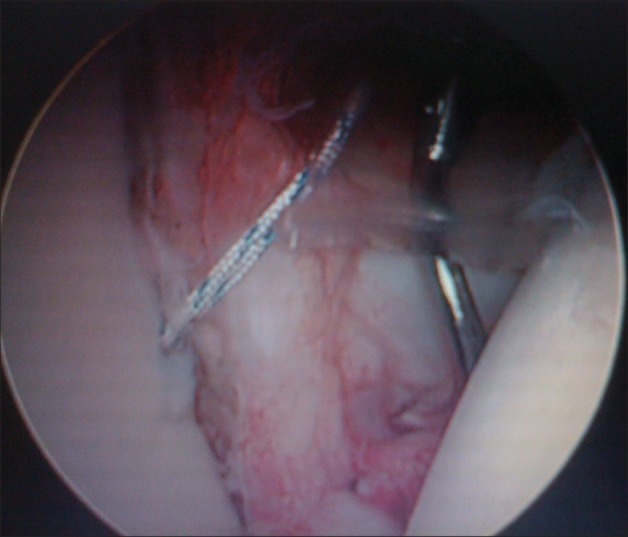
Arthroscopic view showing a curved, sharp suture-passing device is used to pierce the capsule and labrum lower than the anchor position, ensuring that the capsule and labrum will be shifted up to an anatomic position
When there was evidence of antero-inferior capsular laxity, the suture passer was passed through the perilabral capsule 1 cm anterior and 1 cm inferior to the Bankart lesion to plicate the redundant capsule. This laxity is assessed by the ability to pass the arthroscope between the humeral head and the glenoid at the level of the anterior band of the inferior glenohumeral ligament.
Postoperatively, we focused on building up their confidence and resorted to a gradual mobilization protocol, conditioning the patient toward increasing level of physical activities. The patients were placed in a sling for 6 weeks. They were allowed to do pendular motion exercises for the first 3 weeks, followed by elevating the elbow to shoulder level (forward active flexion to 90°) from the third to the sixth week. They were also taught to do isometric rotator cuff exercises during these 6 weeks. Full shoulder mobilization was allowed after 6 weeks. Noncontact sports activities were allowed at 3 months and contact sports at 4 months.
Data analysis comparing the scores before and after surgery was performed using the Wilcoxon Sign Rank Test. A P value of < 0.05 was taken as statistically significant.
RESULTS
The average followup period was 27 months (range 24-36 months). The mean age was 26.83 years (range 18-45 years). There was no statistical relation between the age of the patient and return to sports. Eighty percent of the patients were amateurs, indulging only in occasional sports like golf, football, badminton, and lawn tennis and 10 patients were professional sports person, 3 from kabaddi, 3 from basketball, and 4 from cricket. The average number of dislocations before surgery was 2.42 (range 2-5). The mean pre- and postoperative range of external rotation was 80.38° and 75.18°, respectively.
At the end of our study 86% patients (43 cases) had stability compared with the normal sided shoulder and were able to return to sports, three patients involved in professional sports were not able to return back to the game, two because of apprehension and one because of residual instability. Four amateurs were not able to return to sports, two because of apprehension or limitation of motion and two because of residual instability.
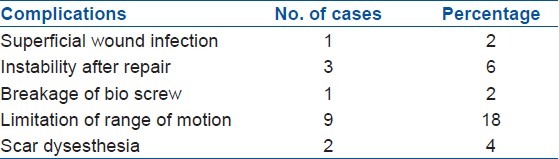
Only two patients (4%) had poor results [Table 1]. There were no cases of redislocation in our study, however, subluxation (Grade I) was observed in three patients. The total UCLA score improved from a mean and SD of 18.45 ± 4.71 (range 9-28) preoperatively to 32.0 ± 2.64 (range 14-35) postoperatively (P < 0.05) [Table 2]. In one patient, there was breakage of a bio anchor (at 3 o’clock) during insertion and we had to do with only two bio anchors (at 5 and 4 o’clock) in that patient. But the postoperative scores, range of motion and stability in that patient were good. Two had some scar dysesthesia. One of the patients had a superficial wound dehiscence, subsequently healing by secondary intention. However, there has been no concern over this individual's range of movement [Table 3].
Table 1.
Final clinical results at twenty four months followup
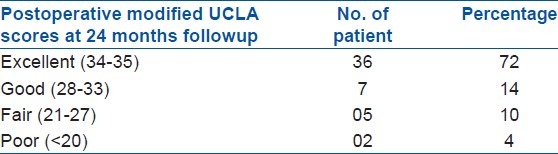
Table 2.
Pre- and postoperative modified UCLA scores
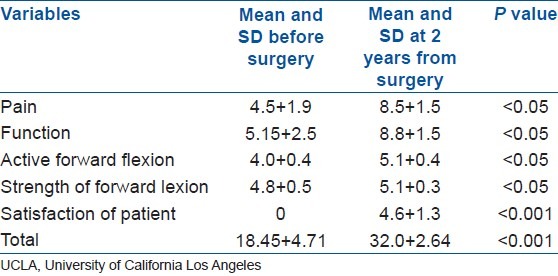
Table 3.
Complications encountered in the study
DISCUSSION
Anterior glenohumeral instability is the most common form of instability around the shoulder joint.11,12 It usually affects young adults and most of the cases arise secondary to traumatic dislocations. Rowe and Zarins reported a rate of 95.6% traumatic origin to anterior dislocation in their study that included 500 patients.13 Similarly, all patients in our study had recurrent anterior glenohumeral instability following initial traumatic anterior dislocation.
Detachment of the antero-inferior labrum (the Bankart lesion) facilitates recurrent anterior instability. The socket-deepening effect of the glenoid labrum has been proved to be an important factor in maintaining stability.14,15 Reattaching the labrum onto the articular surface restores its socket-deepening bumper effect. This is accomplished using sutures and suture anchors, which can be done either open or arthroscopically.15,16 Capsular laxity is the other reason for glenohumeral instability. Lack of diagnosing and treating variable capsular laxity accompanying Bankart lesions may cause failure of repair.17,18 For a perfect shoulder instability repair result, all the facts causing instability must be understood and treated appropriately.
Historically, arthroscopic repair for the treatment of the Bankart lesion had been less satisfactory than the open technique.5 Arthroscopic techniques described previously were using transglenoid sutures or bio-absorbable tacks19 In the past few years, newer techniques involving suture anchor fixation and capsular plication have evolved, with promising results. Suture anchors are low-profile fixation devices that minimize articular surface damage of the humeral head, offering anatomic reconstruction of the glenoid labrum as well as the glenohumeral ligament complex. Any redundant or loose capsule is also addressed during the same operation, allowing one to address any capsular laxity, restoring tension in the anterior-inferior glenohumeral ligament and stability to the glenohumeral joint.
Open method of Bankart repair has several limiting factors, which renders it a less favorable option. It causes an increased blood loss during surgery, a prolonged period of stay in the hospital and a significant loss of range of motion. In the classic open Bankart repair there is disruption of the subscapularis tendon, which may result in postoperative subscapularis insufficiency;20 in addition, there have been reported cases of postoperative subscapularis tendon rupture.20,21 The arthroscopic Bankart repair offers minimally invasive approach with less surgical trauma and blood loss, with improvements in operating time, perioperative morbidity, narcotic use, hospital stay, time loss from work, and decrease number of complications together with a lower cost of surgery.22–24 Postoperative recovery and rehabilitation is faster than open surgical techniques. Postoperative range of motion is also not sacrificed for the sake of stability. Patients are able to have a good range of motion functionally, especially external rotation, which allows them to return to their sports or high-demand jobs.25–27 We have also shown that postoperative range of motion is not sacrificed for the sake of stability, with a mean of 80.38° of external rotation.
We used the UCLA system because it was one of the first shoulder outcome measures that was introduced, the test is easy to administer and clinicians who want to quickly and simply evaluate outcomes for a variety of diagnoses find UCLA to be helpful.28–30 We found a lot of research papers based on this score3,6,31 and so a formal comparison between different studies could be performed. Although it lacks formal validation, we have included it because of its historic standing and continued popularity.
In one patient, there was breakage of a bio anchor (at 3 o’clock) during insertion. Bio anchor's composition makes it vulnerable to break. Care during insertion has to be observed to avoid this problem. Bottoming out of the anchor in the tunnel should be avoided, one must insure that the hole is properly drilled and oriented and the drill guide is properly seated and does not move when the screw is being inserted and one should avoid impacting the anchor beyond the mark of the inserter.32 Shane et al.33 observed a number of bio-absorbable suture anchors that break with screw in insertion and also reported that there was an inconsistency in the quality of the bio-absorbable material in the suture anchors. Cole and Provencher34 believed that insertion techniques are of utmost importance when using bio anchors.
There were nine patients with limitation of shoulder movements. Out of these nine, six were those whose physiotherapy sessions were not supervised. We have not encountered any problems with either subscapularis muscle dysfunction or rupture. There were no cases of dislocation observed in our study, however, three cases had mild laxity (Grade I) of the joint, which was asymptomatic and not associated with any difficulty in lifting the arm up or limitation of the ability to throw.
Gartsman et al. performed arthroscopic Bankart repair, capsular plication, and if necessary thermal capsuloraphy in 53 patients with antero-inferior shoulder instability. After 2 years followup good and excellent results were 92%, and 7.5% of them had recurrence.27 Mishra and Fanton reported a failure rate of 7% with arthroscopic Bankart repair combined with thermal treatment.35 Sedeek et al. reached at a 92.5% successful rate after arthroscopic treatment of 40 shoulders.3 Our results with instability in 6.0% patients was similar to the above mentioned studies.
In a prospective study by Karlsson et al. comparing arthroscopic and open methods, after a mean duration of 28 months, external rotation was 80° in open group and 90° in arthroscopic group postoperatively.36 Gartsman et al.26 and Synder et al.37 both reported a 5° degree decrease in external rotation and Kim et al.24 reported 4° in their series. Similarly mean external rotation limitation was 5° in our patients postoperatively.
This study has some limitations. Full details of the events in the postoperative period and the period of supervised physiotherapy were not always available. The study population was small and also the study did not take up any comparison between the open and the arthroscopic procedure.
To conclude arthroscopic Bankart repair with suture anchors for recurrent anterior glenohumeral instability is a useful option.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Erkoçak ÖF, Yel M. The functional results of arthroscopic bankart repair with knotless anchors for anterior glenohumeral instability. Eur J Gen Med. 2010;7:179–86. [Google Scholar]
- 2.Bankart AS. Recurrent or habitual dislocation of the shoulder. BMJ. 1920;1:1132–3. doi: 10.1136/bmj.2.3285.1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sedeek SM, Tey IK, Tan AH. Arthroscopic bankart repair for traumatic anterior shoulder instability with the use of suture anchors. 2008;49:676-81. Singapore Med J. 2008;49:676–81. [PubMed] [Google Scholar]
- 4.Sperling JW, Smith AM, Cofield RH, Barnes S. Patient perceptions of open and arthroscopic shoulder surgery. Arthroscopy. 2007;23:361–6. doi: 10.1016/j.arthro.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 5.Fabbriciani C, Milano G, Demontis A, Fadda S, Ziranu F, Mulas PD. Arthroscopic versus open treatment of Bankart lesion of the shoulder: A prospective randomized study. Arthroscopy. 2004;20:456–62. doi: 10.1016/j.arthro.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 6.Ee GW, Mohamed S, Tan AH. Long term results of arthroscopic bankart repair for traumatic anterior shoulder instability. J Orthop Surg Res. 2011;6:28. doi: 10.1186/1749-799X-6-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Amstutz HC, Sew Hoy AL, Clarke IC. UCLA anatomic total shoulder arthroplasty. Clin Orthop Relat Res. 1981;155:7–20. [PubMed] [Google Scholar]
- 8.Ellman H, Hanker G, Bayer M. Repair of rotator cuff. End-result study of factors influencing reconstruction. J Bone Joint Surg Am. 1986;68:1113–44. [PubMed] [Google Scholar]
- 9.Ellman H. Arthroscopic subacromial decompression: Analysis of one- to three-year results. Arthroscopy. 1987;3:173–81. doi: 10.1016/s0749-8063(87)80061-0. [DOI] [PubMed] [Google Scholar]
- 10.Baumgarten KM, Wright RW. Ease of tying arthroscopic knots. J Shoulder Elbow Surg. 2007;14:438–42. doi: 10.1016/j.jse.2006.10.013. [DOI] [PubMed] [Google Scholar]
- 11.Baker CL, Uribe JN, Whitman C. Arthroscopic evaluation of acute initial anterior shoulder dislocation. Am J Sports Med. 1990;18:25–8. doi: 10.1177/036354659001800104. [DOI] [PubMed] [Google Scholar]
- 12.Liu SH, Henry MH. Anterior shoulder instability. Current review. Clin Orthop. 1996;323:327–37. [PubMed] [Google Scholar]
- 13.Rowe CR, Zarins B. Recurrent transient subluxation of the shoulder. J Bone Joint Surg. 1981;63A:863–72. [PubMed] [Google Scholar]
- 14.Cooper DE, Arnoczky SP, O’Brien SJ, Warren RF, DiCarlo E, Allen AA. Anatomy histology and vascularity of the glenoid labrum. J Bone Joint Surgery Am. 1992;74:46–51. [PubMed] [Google Scholar]
- 15.Lippitt SB, Vanderhooft JE, Harris SL, Sidles JA, Harryman DT, 2nd, Matsen FA., 3rd Glenohumeral stability from concavity compression: A quantitative analysis. J Shoulder Elbow Surg. 1993;2:27–35. doi: 10.1016/S1058-2746(09)80134-1. [DOI] [PubMed] [Google Scholar]
- 16.Kirkley A, Griffin S, Richards C, Miniaci A, Mohtadi N. Prospective randomized clinical trail comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocation of the shoulder. Arthroscopy. 1999;15:507–14. doi: 10.1053/ar.1999.v15.015050. [DOI] [PubMed] [Google Scholar]
- 17.Levine WN, Arroyo JS, Pollock RG, Flatow EL, Bigliani LU. Open revision stabilization surgery for recurrent anterior glenohumeral instability. Am J Sports Med. 2000;28:156–60. doi: 10.1177/03635465000280020401. [DOI] [PubMed] [Google Scholar]
- 18.Zabinski SJ, Callaway GH, Cohen S, Warren RF. Revision shoulder stabilization: 2 to 10 year results. J Shoulder Elbow Surg. 1999;8:58–65. doi: 10.1016/s1058-2746(99)90057-5. [DOI] [PubMed] [Google Scholar]
- 19.Freedman KB, Smith AP, Romeo AA, Cole BJ, Bach BR., Jr Open bankart repair versus arthroscopic repair with transglenoid sutures or bioabsorbable tacks for recurrent anterior instability of the shoulder. Am J Sports Med. 2004;32:1520–7. doi: 10.1177/0363546504265188. [DOI] [PubMed] [Google Scholar]
- 20.Scheibel M, Tsynman A, Magosch P, Schroeder RJ, Habermeyer P. Postoperative subscapularis muscle insufficiency after primary and revision open shoulder stabilization. Am J Sports Med. 2006;34:1586–93. doi: 10.1177/0363546506288852. [DOI] [PubMed] [Google Scholar]
- 21.Bottoni CR, Smith EL, Berkowitz MJ, Towle RB, Moore JH. Arthroscopic versus open shoulder stabilization for recurrent anterior instability. Am J Sports Med. 2006;34:1730–7. doi: 10.1177/0363546506288239. [DOI] [PubMed] [Google Scholar]
- 22.Wang C, Ghalambor N, Zarins B, Warner JJ. Arthroscopic versus open bankart repair: Analysis of patient subjective outcome and cost arthroscopy. Arthroscopy. 2005;21:1219–22. doi: 10.1016/j.arthro.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 23.O’Neill BD. Arthroscopic Bankart repair of anterior detachments of the glenoid labrum. A prospective study. Arthroscopy. 2002;18:755–63. [PubMed] [Google Scholar]
- 24.Kim SH, Ha KI, Cho YB, Ryu BD, Oh I. Arthroscopic anterior stabilization of the shoulder: Two to six year followup. J Bone Joint Surg Am. 2003;85:1511–8. [PubMed] [Google Scholar]
- 25.McIntyre LF, Caspari RB, Savoie FH., 3rd The arthroscopic treatment of multidirectional shoulder instability: Two-year results of a multiple suture anchor. Arthroscopy. 1997;13:418–25. doi: 10.1016/s0749-8063(97)90118-3. [DOI] [PubMed] [Google Scholar]
- 26.Savoie FH, 3rd, Miller CD, Field LD. Arthroscopic reconstruction of traumatic anterior instability of the shoulder. The Caspari technique. Arthroscopy. 1997;13:201–9. doi: 10.1016/s0749-8063(97)90155-9. [DOI] [PubMed] [Google Scholar]
- 27.Gartsman GM, Roddey TS, Hammerman SM. Arthroscopic treatment of anterior-inferior glenohumeral instability. Two to five-year followup. J Bone Joint Surg Am. 2000;82:991–1003. doi: 10.2106/00004623-200007000-00011. [DOI] [PubMed] [Google Scholar]
- 28.Plancher KD, Lipnick SL. Analysis of evidence-based medicine for shoulder instability, arthroscopy. Arthroscopy. 2009;25:897–908. doi: 10.1016/j.arthro.2009.03.017. [DOI] [PubMed] [Google Scholar]
- 29.Wright RW, Baumgarten KM. Shoulder outcomes measures. J Am Acad Orthop Surg. 2010;18:436–44. doi: 10.5435/00124635-201007000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Godfrey J, Hamman R, Lowenstein S, Briggs K, Kocher M. Reliability, validity, and responsiveness of the simple shoulder test: Psychometric properties by age and injury type. J Shoulder Singapore Med J. 2008;49:681. doi: 10.1016/j.jse.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 31.Mahmoud TA El-Aziz, Moiistafa MS, Sokker SM, El-Adawy M. Evaluation of the functional results of management of traumatic anterior glenohumeral instability by arthroscopic capsular shift using suture anchors. Suez Canal Univ Med J. 2008;11:103–14. [Google Scholar]
- 32.Barber FA. Arthroscopic management of shoulder instability: Bio anchor. In: Chow James CY, editor. Advanced Arthroscopy. New York: Springer; 2001. pp. 73–80. [Google Scholar]
- 33.Nho SJ, Provencher MT, Seroyer ST, Romeo AA. Bioabsorbable anchors in glenohumeral shoulder surgery. Arthroscopy. 2009;25:788–93. doi: 10.1016/j.arthro.2008.08.018. [DOI] [PubMed] [Google Scholar]
- 34.Cole BJ, Provencher MT. Safety profile of bioabsorbable shoulder anchors. Arthroscopy. 2007;23:912–3. doi: 10.1016/j.arthro.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 35.Mishra DK, Fanton GS. Two-years outcome of arthroscopic Bankart repair and electrothermal-assisted capsulorrhaphy for recurrent traumatic anterior shoulder instability. Arthroscopy. 2001;17:844–9. doi: 10.1016/s0749-8063(01)90008-8. [DOI] [PubMed] [Google Scholar]
- 36.Karlsson J, Magnusson L, Ejerhed L, Hultenheim I, Lundin O, Kartus J. Comparison of open and arthroscopic stabilization for recurrent shoulder dislocation in patients with a bankart lesion. Am J Sports Med. 2001;29:538–42. doi: 10.1177/03635465010290050201. [DOI] [PubMed] [Google Scholar]
- 37.Synder SJ, Banas MP, Belzer JP. Arthroscopic treatment of anterior shoulder instability using threaded suture anchors and nonabsorbable sutures. Instr Course Lect. 1996;45:71–81. [PubMed] [Google Scholar]


