Abstract
AIM: To explore age-related changes in symptoms and quality of life (QoL) of women with irritable bowel syndrome (IBS).
METHODS: Two-hundred and fifty-four female adult outpatients with IBS attending the Department of Gastroenterology at the First Affiliated Hospital of Nanjing Medical University between January, 2008 and October, 2008 were approached. Patients with a history of abdominal surgery, mental illness or those who had recently taken psychotropic drugs were excluded. A physician obtained demographic and abdominal symptom data. All patients were asked to complete the Zung Self-Rated Anxiety and Depression Scale (SDS/SAS) and the IBS-specific QoL questionnaire. The patients were divided into six groups according to age, in 10-year increments: 18-27 years, 28-37 years, 38-47 years, 48-57 years, 58-67 years and 68-75 years (maximum 75 years). Age-related differences of abdominal pain or discomfort were analyzed using rank-sum tests. Differences in SDS/SAS and IBS-QoL scores between age groups were analyzed using one-way analysis of variance. Pearson’s correlations evaluated potential associations between IBS symptoms, psychological factors and QoL in each age group.
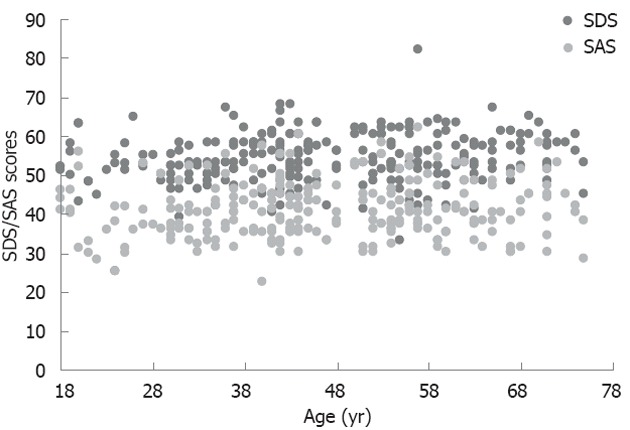
RESULTS: There were no differences in the distribution of IBS subtypes between age groups (χ2 = 20.516, P = 0.153). Differences in the severity of abdominal pain/discomfort with age were statistically significant (χ2 = 25.638, P < 0.001); patients aged 48-57 years, 58-67 years or 68-75 years had milder abdominal pain/discomfort than those in the younger age groups. The severity of anxiety or depressive symptoms did not differ between age groups (SDS, χ2 = 390.845, P = 0.110; SAS, χ2 = 360.071, P = 0.220). Differences of IBS-QoL scores were statistically significant between age groups (χ2 = 1098.458, P = 0.011). The scores of patients in the 48-57-year group were lower than those in the 18-27-year and 28-37-year groups (48-57-year group vs 18-27-year group, 74.88 ± 8.76 vs 79.76 ± 8.63, P = 0.021; 48-57-year group vs 28-37-year group, 74.88 ± 8.76 vs 79.04 ± 8.32, P = 0.014). The scores in the 68-75-year group were lower than those in the 18-27-year, 28-37-year and 38-47-year groups (68-75-year group vs 18-27-year group, 71.98 ± 9.83 vs 79.76 ± 8.63, P = 0.003; 68-75-year group vs 28-37-year group, 71.98 ± 9.83 vs 79.04 ± 8.32, P = 0.002; 68-75-year group vs 38-47-year group,71.98 ± 9.83 vs 76.44 ± 8.15, P = 0.039). Anxiety and depression were negatively correlated with QoL in all age groups (SDS and QoL: 18-27-year group, r = -0.562, P = 0.005; 28-37-year group, r = -0.540, P < 0.001; 38-47-year group, r = -0.775, P < 0.001; 48-57-year group, r = -0.445, P = 0.001; 58-67-year group, r = -0.692, P < 0.001; 68-75-year group, r = -0.732, P < 0.001. SAS and QoL: 18-27-year group, r = -0.600, P = 0.002; 28-37-year group, r = -0.511, P < 0.001; 38-47-year group, r = -0.675, P < 0.001; 48-57-year group, r = -0.558, 58-67-year group, P = 0.001; r = -0.588, P < 0.001; 68-75-year group, r = -0.811, P < 0.001). A negative correlation between abdominal pain severity and QoL was found in patients aged more than 58 years (58-67-year group, r = -0.366, P = 0.017; 68-75-year group, r = -0.448, P = 0.048 ), but not in younger patients (18-27-year group, r = 0.080, P = 0.716; 28-37-year group, r = -0.063, P = 0.679; 38-47-year group, r = -0.029, P = 0.812; 48-57-year group, r = -0.022, P = 0.876).
CONCLUSION: Factors affecting QoL should always be treated in IBS, especially emotional problems in young adults. Even mild abdominal pain should be controlled in elderly patients.
Keywords: Irritable bowel syndrome, Female, Age, Symptom, Quality of life
INTRODUCTION
Irritable bowel syndrome (IBS) is the most common functional gastrointestinal disorders. It is common in Chinese people, representing approximately 11% of outpatient cases in gastroenterology departments[1]. Patients with IBS have long-term symptoms including abdominal pain or discomfort related to defecation, accompanied by emotional disorders such as anxiety or depression, and often have a poor quality of life (QoL)[2,3]. The abdominal symptoms of IBS may be related to changes of gastrointestinal motility, visceral sensitivity and other factors[4,5], and affected by estrogen and progesterone levels and psychological factors[6-8]. Anxiety or depression in IBS patients may be associated with physical discomfort and mental stress, and related to the patient’s response to the disease and the degree of social support[9,10].
It is widely recognized that gastrointestinal motility, visceral sensitivity, and estrogen and progesterone levels differ between people of different ages[11,12], as do cognitive abilities and the response to disease[13]. Do abdominal pain or discomfort, anxiety and depression vary with age in IBS patients? Are there are age-related differences in the impact of these symptoms on QoL? In this study, we explored these two questions.
IBS is more common in women than in men, and female IBS patients report more severe symptoms and generally have lower QoL[1]. Therefore, we investigated age-related changes of symptoms and QoL in female patients with IBS in a Chinese population, with the aim of improving individual treatment.
MATERIALS AND METHODS
Subjects
First-time outpatients who attended the Department of Gastroenterology at the First Affiliated Hospital of Nanjing Medical University between January, 2008 and October, 2008 and met the Rome III criteria for IBS were recruited[14].
All patients were initially asked to undergo routine blood, urine and stool hemoccult tests, stool form examination, and endoscopy or radiographic examination of the gastrointestinal tract. Patients younger than 18 years, with a structural bowel disease or a history of abdominal surgery, diagnosed with mental illness by a psychiatrist or who had recently taken psychotropic drugs were excluded[1]. Pregnant patients were not included.
Measurements
The age of each subject was recorded. A physician obtained demographic and abdominal symptom data. All patients were asked to completed the Zung Self-Rated Anxiety and Depression Scale (SAS/SDS) and the IBS-specific QoL (IBS-QoL) questionnaire[15-19].
IBS subtypes: Based on the Rome III diagnostic criteria and Bristol Stool Form Scale[14], the patients were divided into the following groups: IBS with constipation (IBS-C), IBS with diarrhea (IBS-D), mixed IBS (IBS-M) and unsubtyped IBS (IBS-U).
IBS abdominal symptoms: The patients were asked about the severity of their abdominal pain/discomfort, which was rated on a three-point response scale as follows: mild (“can be ignored if I don’t think about it”), moderate (“cannot be ignored, but does not affect my lifestyle”) or severe (“affects my lifestyle”)[20].
SAS/SDS: Anxiety and depression were measured using the SAS and SDS assessment tools, respectively [15-17]. Each of the SAS and SDS comprises 20 questions with four possible responses to each: never, rarely/sometimes, frequently and always. Higher SAS/SDS scores indicate a greater degree of anxiety/depression.
IBS-QoL: The IBS-QoL[18,19] comprises 34 self-reported items; a higher total score indicates a better QoL. There are also eight subscale scores for dysphoria, interference with activities, body image, health concerns, food avoidance, social reaction, sexual issues and relationship problems.
Age groups: The patients were divided into six groups according to age, in 10-year increments: 18-27 years, 28-37 years, 38-47years, 48-57 years, 58-67 years and 68-75 years (maximum 75 years)[21-23].
Statistical analysis
All data were analyzed using SPSS Version 19.0. Statistical significance was set at P < 0.05. Categorical data and ratios were analyzed using the χ2 test. Rank-sum tests were used to analyze ranked data. All measurement data are reported as the mean ± SD. Differences in SDS/SAS and IBS-QoL scores between age groups were analyzed using one-way analysis of variance. Pearson’s correlations were used to evaluate the potential associations between IBS symptoms, psychological factors and QoL in each age group.
RESULTS
Patient background and clinical data
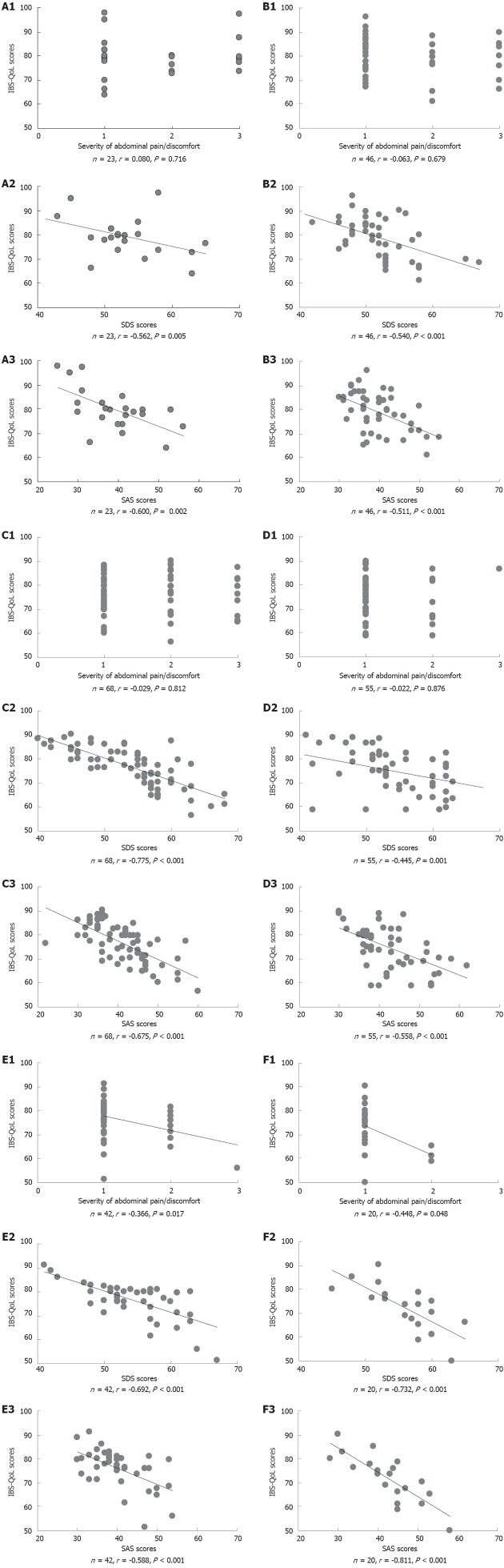
Two hundred and fifty-four women with IBS were approached for recruitment to this study. These patients were aged between 18 and 75 years (46.67 ± 14.26 years). The median duration of IBS was 3 years, and 8.4% of the patients had a history of IBS of more than 10 years. There were no differences in the duration of IBS between age groups (average duration of each group: 2.79 ± 2.48 years, 2.22 ± 2.27 years; 2.94 ± 3.29 years, 2.97 ± 3.32 years, 4.27 ± 4.79 years, 4.35 ± 6.55 years, respectively; χ2 = 129.4, P = 0.101). One hundred and twenty-three patients (48.4%) were diagnosed with IBS-D, 105 (41.3%) with IBS-C, 22 (8.7%) with IBS-M and 4 (1.6%) with IBS-U. There were no differences in the distribution of IBS subtypes between age groups (χ2 = 20.516, P = 0.153), as shown in Figure 1.
Figure 1.
Distribution of irritable bowel syndrome subtypes in each age group. IBS: Irritable bowel syndrome; IBS-C: IBS with constipation; IBS-D: IBS with diarrhea; IBS-M: Mixed IBS; IBS-U: Unsubtyped IBS.
Symptoms by age
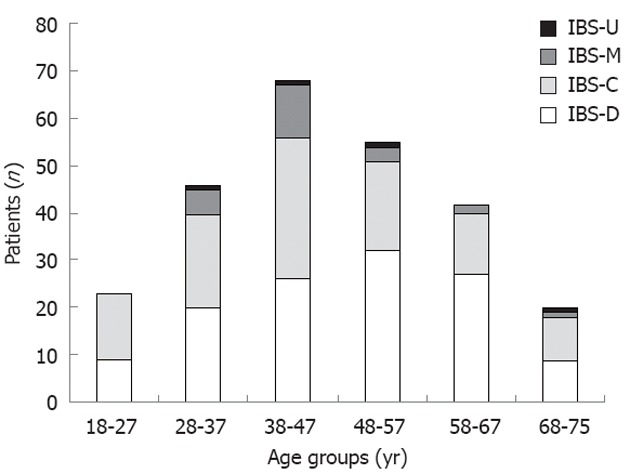
Abdominal pain/discomfort: Differences in the severity of abdominal pain/discomfort with age are shown in Figure 2. These differences were statistically significant (χ2 = 25.638, P < 0.001; Table 1); patients aged 48-57 years, 58-67 years or 68-75 years had milder abdominal pain/discomfort than those in the younger age groups.
Figure 2.
Severity of abdominal pain/discomfort by age. 1 = Mild; 2 = Moderate; 3 = Severe.
Table 1.
Severity of abdominal pain/discomfort and Zung Self-Rated Anxiety and Depression Scale scores in each age group
| Age group (yr) | Total (n) | Severity of abdominal pain/discomfort (n) | Mean rank | SDS score | SAS score | ||
| Mild | Moderate | Severe | |||||
| 18-27 | 23 | 12 | 5 | 6 | 150.74 | 52.17 ± 8.03 | 39.09 ± 8.18 |
| 28-37 | 46 | 29 | 10 | 7 | 133.84 | 51.83 ± 5.09 | 39.65 ± 6.16 |
| 38-47 | 68 | 34 | 22 | 12 | 149.66 | 54.03 ± 6.66 | 41.25 ± 7.17 |
| 48-57 | 52 | 45 | 9 | 1 | 106.90 | 54.24 ± 7.60 | 42.31 ± 7.37 |
| 58-67 | 42 | 33 | 8 | 1 | 110.82 | 54.60 ± 6.09 | 39.83 ± 6.82 |
| 68-75 | 20 | 17 | 3 | 0 | 102.53 | 56.15 ± 4.98 | 42.45 ± 7.81 |
The severity of abdominal pain/discomfort differed between age groups (χ2 = 25.638, P < 0.001). There were no differences in Zung Self-Rated Anxiety Scale (SAS) or Zung Self-Rated Depression Scale (SDS) scores between any age groups (SDS, χ2 = 390.845, P = 0.110; SAS, χ2 = 360.071, P = 0.220).
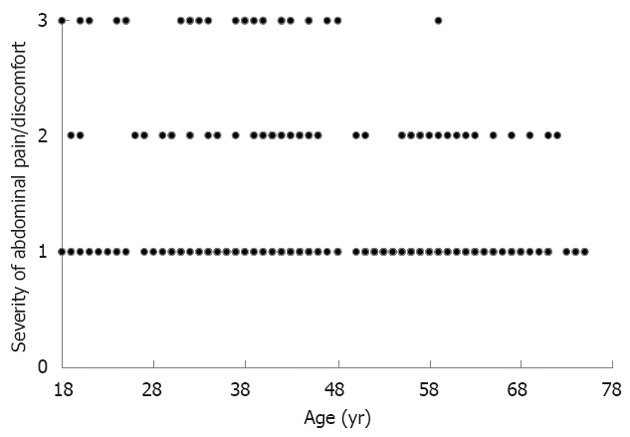
Anxiety and depression: SAS and SDS scores with age are shown in Figure 3. There were no statistically significant differences between any age groups (SDS, χ2 = 390.845, P = 0.110; SAS, χ2 = 360.071, P = 0.220; Table 1), indicating that the severity of anxiety and depression does not vary with age.
Figure 3.
Zung self-rated anxiety and depression scale scores according to age. SAS/SDS: Zung self-rated anxiety and depression scale.
QoL: IBS-QoL scores with age are shown in Figure 4A. These differences were statistically significant between age groups (χ2 = 1098.458, P = 0.011; Figure 4B). The scores of patients in the 48-57-year group were lower than those in the 18-27-year and 28-37-year groups (P = 0.021, P = 0.014). The scores in the 68-75-year group were lower than those in the 18-27-year, 28-37-year and 38-47-year groups (P = 0.003, P = 0.002 and P = 0.039, respectively).
Figure 4.
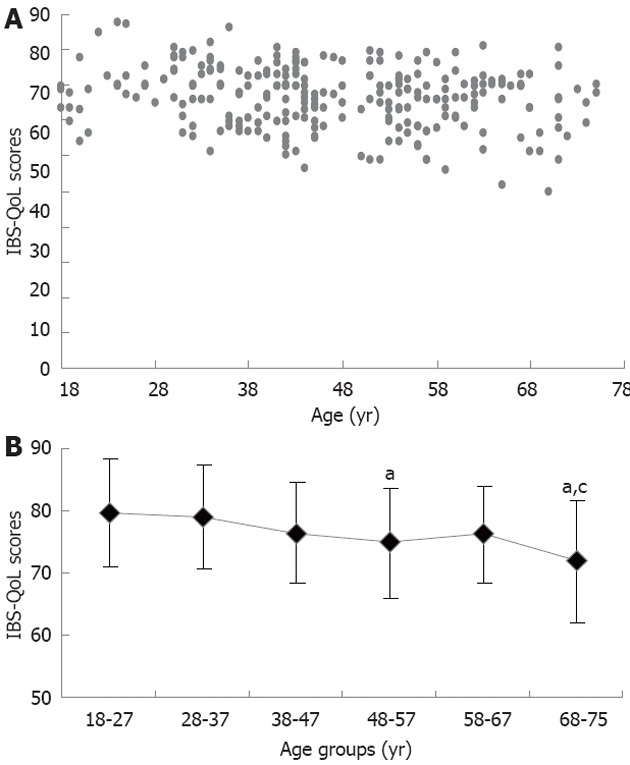
Specific quality of life questionnaire scores for patients with irritable bowel syndrome. A: Specific quality of life questionnaire scores for patients with irritable bowel syndrome (IBS) according to age; B: Specific quality of life questionnaire scores for patients with IBS in each age group. aP < 0.05 vs 18-27-year and 28-37-year groups; cP < 0.05 vs 48-57-year group. QoL: Quality of life; SAS/SDS: Zung self-rated anxiety and depression scale.
Association of abdominal pain, anxiety and depression with QoL
As shown in Figure 5, the severity of abdominal pain/discomfort was negatively correlated with IBS-QoL score in the 58-67-year and 68-75-year groups (P < 0.05), but there was no correlation in the 18-27-, 28-37-, 38-47- or 48-57-year groups. SAS and SDS scores were negatively correlated with IBS-QoL score in all age groups (P < 0.01).
Figure 5.
Association of abdominal pain/discomfort severity, and Zung self-rated anxiety and depression scale scores for patients with irritable bowel syndrome in each age group. A: Age 18-27 years; B: Age 28-37 years; C: Age 38-47 years; D: Age 48-57 years; E: Age 58-67 years; F: Age 68-75 years. A1 to F1, association of abdominal pain/discomfort with quality of life in each age group. Severity of abdominal pain/discomfort was negatively correlated with irritable bowel syndrome-specific quality of life questionnaire (IBS-QoL) scores in the 58-67-year and 68-75-year groups (P < 0.05), but there was no correlation in the 18-27-year, 28-37-year, 38-47-year or 48-57-year groups (P > 0.05); A2 to F2, association of Zung Self-Rated Depression Scale (SDS) scores with quality of life in each age group. SDS scores were negatively correlated with IBS-QoL scores in all age groups (P < 0.01); A3 to F3, association of Zung Self-Rated Anxiety Scale (SAS) scores with quality of life in each age group. SAS scores were negatively correlated with IBS-QoL scores in all age groups (P < 0.01).
DISCUSSION
In this study, most of the 254 women with IBS were middle-aged. IBS-D was the most common subtype, followed by IBS-C, IBS-M and IBS-U. The distribution of IBS subtypes showed no difference between any age groups, consistent with previous epidemiological studies[1,23,24].
Our study suggests that the severity of abdominal pain/discomfort differs in patients of different ages, but anxiety and depressive symptoms do not. Patients aged 48-57 years or 68-75 years had the worst QoL. Anxiety and depression were negatively correlated with QoL in all age groups, and a negative correlation between abdominal pain severity and QoL was found in patients aged more than 58 years, but not in younger patients.
Defecation-related abdominal pain/discomfort is the principal symptom of IBS[14]. In the present study, patients older than 48 years had milder abdominal pain/discomfort. Visceral hypersensitivity, psychological factors, motility, immunity and infection are the major pathophysiologic factors in abdominal pain/discomfort in IBS[4,5,25-27], and the role of visceral hypersensitivity in the pathogenesis of IBS has become commonly accepted in recent years. IBS patients have been reported to have a decreased intestinal pain perception threshold and are more likely to report feeling pain[28,29]. Some studies have shown visceral sensitivity to decrease with age[12]. Sanoja et al[7] found that estrogen and progesterone can regulate sensitivity to pain and temperature sensation, and Heitkemper et al[30], summarizing the results of recent research, found that estrogen and progesterone can affect the symptoms of IBS. Most women over the age of 48 years are in the menopause or perimenopausal period, and the decline of estrogen and progesterone levels may be accompanied by decreased visceral sensitivity.
In the modern bio/psychosocial medical model, IBS is recognized as a psychosomatic disorder accompanied by various emotional disorders, among which anxiety and depression are the most common. The present study found no differences in SAS/SDS scores between age groups, suggesting that the severity of anxiety and depression is similar in patients of differing ages.
Although it has been confirmed that coping capacity increases with age[13], ageing is accompanied by reduced sleep quality and blood hemoglobin concentration, and both of these are closely related to depression[31-33]. Negative life events, social support and other factors are also involved in the occurrence of anxiety and depression[10,34,35]. None of these factors showed any significant age-related differences in IBS patients.
QoL relates to the functional capabilities of individuals in social life and reflects subjective feelings. It is an important concept in biomedical and social psychology, but is of greatest concern in disease states and when evaluating treatments for disease-related symptoms. In patients with IBS, it is regarded as a major measure of clinical outcome and is widely used in clinical studies[18,19]. Previous studies have shown that bowel symptoms, anxiety and depression are important factors in the QoL of IBS patients[36-38]. The present study demonstrated age-related differences in the QoL of women with IBS; the QoL of patients aged 48-57 years or over 68 years was poorer than that of younger patients. However, the patients in the older age groups had milder abdominal pain, and their degree of anxiety and depression was similar to that of the other age groups. Thus, what caused the decline of their QoL? Pines et al[39] found that the reduction of hormone levels in menopausal women resulted in various physical symptoms that affected QoL, and hormone replacement therapy partially improved these symptoms. Menopause-related factors may have responsible for the poor QoL of the patients aged 48-57 years in our study. In addition, we speculate that multiple other factors such as decreased activity or social support, or impaired psychological status may lead to a poor QoL in older patients. It is necessary to identify other factors that affect QoL in these patients, in addition to bowel symptoms, anxiety and depression.
We also investigated changes with age in the correlation of abdominal pain, anxiety and depressive symptoms with QoL, and found that anxiety and depression were negatively correlated with QoL in all age groups.
Psychologists believe that IBS is a psychosomatic disorder; most IBS patients have core symptoms of anxiety or depression, while gastrointestinal symptoms such as abdominal pain and changes in bowel habit represent somatization[40]. In our previous study, we found that most IBS patients complained of nonspecific somatic symptoms such as dizziness, insomnia and fatigue[1]. We should therefore pay attention to the treatment of anxiety, depression and other negative emotions in IBS patients. In the present study, found that, in young and middle-aged patients (18-57 years), QoL was negatively correlated with anxiety and depression, but not associated with the severity of abdominal pain/discomfort. Therefore, improving gastrointestinal symptoms only may not improve QoL in these age groups, and antidepressant treatment may be more important. In IBS patients aged over 58 years, abdominal pain/discomfort was mild but closely associated with QoL. Thus, even slight abdominal pain should be controlled in the treatment of older patients. Although age-related physiological and psychological changes may be directly or indirectly related to ovarian function and female hormone levels, this was a retrospective study and thus we lack information on the patients’ hormone levels and menstrual history. Furthermore, the use of self-reported measures and individual differences in literacy and understanding may have affected the results. None of these limitations could be avoided.
In conclusion, the following points should be borne in mind when treating women with IBS. Firstly, in patients aged 48-57 years or over 68 years, factors other than IBS-related symptoms that affect QoL should be treated. Secondly, negative emotions should be treated in all patients; anti-anxiety and antidepressant treatment are especially important in young adults. Thirdly, to improve QoL, even mild abdominal pain should be controlled in elderly patients.
COMMENTS
Background
Irritable bowel syndrome (IBS) is the most common functional gastrointestinal disorder. IBS is more common in women than in men, and female IBS patients report more severe symptoms and generally have a lower quality of life (QoL). Age-related changes, such as gastrointestinal motility, visceral sensitivity, estrogen and progesterone levels, cognitive abilities and the response to disease may cause differences in abdominal pain or discomfort, anxiety and depression and reduced QoL levels. Therefore, the authors investigated age-related changes of symptoms and QoL levels in female patients with IBS in a Chinese population, with the aim of improving individual treatment profiles.
Research frontiers
The symptoms of IBS may be related to changes in gastrointestinal motility and visceral sensitivity and are affected by estrogen and progesterone levels, psychological factors, patient response to pain and the degree of social support. All of the above factors differ between people of different ages. In this study, authors demonstrate that differences in abdominal pain or discomfort levels, but not anxiety or depression, and their association with QoL exist in patients in different age groups.
Innovations and breakthroughs
Recent reports have highlighted the differences in IBS abdominal and psychological symptoms in different genders and IBS subtypes, which can guide individual treatment regimens. Other reports have referred to the different age distributions of IBS patients. However, no study has investigated age-related changes in symptoms and their association with QoL in IBS patients, particularly in an exclusively female patient cohort or in a Chinese population.
Applications
In this study, the authors have demonstrated the difference of IBS symptoms and their association with QoL in each patient age group. With this knowledge, the authors may improve individual treatment regimens for IBS according to the patient age.
Terminology
Zung self-rated anxiety and depression scale (SAS/SDS) are assessment tools that are used to measure anxiety and depression, respectively. Higher SAS/SDS scores indicate a greater degree of anxiety/depression. IBS-specific QoL questionnaire (IBS-QoL) is a QoL assessment tool, which was specifically set up for patients with IBS. A higher IBS-QoL score indicates a better QoL.
Peer review
The authors explored the age-related changes of symptoms, QoL and the correlations between these two parameters in a population of Chinese women. The results demonstrated that factors that affect QoL should always be treated in IBS, especially emotional problems in young adults, and even mild abdominal pain should be controlled in elderly patients. These findings will help to improve the treatment of individuals with IBS.
Footnotes
Supported by Open Project Program of the Jiangsu Key Laboratory of Molecular and Functional Imaging, No. PYZX 2011016; and the Medical Science and Technology Development Foundation of Nanjing Department of Health, No. YKK11199
Peer reviewer: Bruno Bonaz, MD, PhD, Clinique Universitaire d’Hépato-Gastroentérologie, CHU de Grenoble, BP 217, 38043 Grenoble Cedex 09, France
S- Editor Gou SX L- Editor A E- Editor Xiong L
References
- 1.Tang YR, Yang WW, Wang YL, Lin L. Sex differences in the symptoms and psychological factors that influence quality of life in patients with irritable bowel syndrome. Eur J Gastroenterol Hepatol. 2012;24:702–707. doi: 10.1097/MEG.0b013e328351b2c2. [DOI] [PubMed] [Google Scholar]
- 2.Gulewitsch MD, Enck P, Hautzinger M, Schlarb AA. Irritable bowel syndrome symptoms among German students: prevalence, characteristics, and associations to somatic complaints, sleep, quality of life, and childhood abdominal pain. Eur J Gastroenterol Hepatol. 2011;23:311–316. doi: 10.1097/MEG.0b013e3283457b1e. [DOI] [PubMed] [Google Scholar]
- 3.Agarwal N, Spiegel BM. The effect of irritable bowel syndrome on health-related quality of life and health care expenditures. Gastroenterol Clin North Am. 2011;40:11–19. doi: 10.1016/j.gtc.2010.12.013. [DOI] [PubMed] [Google Scholar]
- 4.Chey WY, Jin HO, Lee MH, Sun SW, Lee KY. Colonic motility abnormality in patients with irritable bowel syndrome exhibiting abdominal pain and diarrhea. Am J Gastroenterol. 2001;96:1499–1506. doi: 10.1111/j.1572-0241.2001.03804.x. [DOI] [PubMed] [Google Scholar]
- 5.Kanazawa M, Hongo M, Fukudo S. Visceral hypersensitivity in irritable bowel syndrome. J Gastroenterol Hepatol. 2011;26 Suppl 3:119–121. doi: 10.1111/j.1440-1746.2011.06640.x. [DOI] [PubMed] [Google Scholar]
- 6.Hogan AM, Kennelly R, Collins D, Baird AW, Winter DC. Oestrogen inhibits human colonic motility by a non-genomic cell membrane receptor-dependent mechanism. Br J Surg. 2009;96:817–822. doi: 10.1002/bjs.6612. [DOI] [PubMed] [Google Scholar]
- 7.Sanoja R, Cervero F. Estrogen-dependent abdominal hyperalgesia induced by ovariectomy in adult mice: a model of functional abdominal pain. Pain. 2005;118:243–253. doi: 10.1016/j.pain.2005.08.021. [DOI] [PubMed] [Google Scholar]
- 8.Nicholl BI, Halder SL, Macfarlane GJ, Thompson DG, O’Brien S, Musleh M, McBeth J. Psychosocial risk markers for new onset irritable bowel syndrome--results of a large prospective population-based study. Pain. 2008;137:147–155. doi: 10.1016/j.pain.2007.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sahdra BK, MacLean KA, Ferrer E, Shaver PR, Rosenberg EL, Jacobs TL, Zanesco AP, King BG, Aichele SR, Bridwell DA, et al. Enhanced response inhibition during intensive meditation training predicts improvements in self-reported adaptive socioemotional functioning. Emotion. 2011;11:299–312. doi: 10.1037/a0022764. [DOI] [PubMed] [Google Scholar]
- 10.Iannone M, Pennick L, Tom A, Cui H, Gilbert M, Weihs K, Stopeck AT. Prevalence of depression in adults with haemophilia. Haemophilia. 2012;18:868–874. doi: 10.1111/j.1365-2516.2012.02863.x. [DOI] [PubMed] [Google Scholar]
- 11.Arhan P, Devroede G, Jehannin B, Lanza M, Faverdin C, Dornic C, Persoz B, Tétreault L, Perey B, Pellerin D. Segmental colonic transit time. Dis Colon Rectum. 1981;24:625–629. doi: 10.1007/BF02605761. [DOI] [PubMed] [Google Scholar]
- 12.Phillips RJ, Walter GC, Powley TL. Age-related changes in vagal afferents innervating the gastrointestinal tract. Auton Neurosci. 2010;153:90–98. doi: 10.1016/j.autneu.2009.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karevold E, Ystrom E, Coplan RJ, Sanson AV, Mathiesen KS. A prospective longitudinal study of shyness from infancy to adolescence: stability, age-related changes, and prediction of socio-emotional functioning. J Abnorm Child Psychol. 2012;40:1167–1177. doi: 10.1007/s10802-012-9635-6. [DOI] [PubMed] [Google Scholar]
- 14.Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130:1480–1491. doi: 10.1053/j.gastro.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 15.Zhao Y, Ke M, Wang Z, Wei J, Zhu L, Sun X, Zhang J. Pathophysiological and psychosocial study in patients with functional vomiting. J Neurogastroenterol Motil. 2010;16:274–280. doi: 10.5056/jnm.2010.16.3.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zung WW. The Depression Status Inventory: an adjunct to the Self-Rating Depression Scale. J Clin Psychol. 1972;28:539–543. doi: 10.1002/1097-4679(197210)28:4<539::aid-jclp2270280427>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 17.Merz WA, Ballmer U. Demographic factors influencing psychiatric rating scales (Zung SDS and SAS) Pharmacopsychiatry. 1984;17:50–56. doi: 10.1055/s-2007-1017407. [DOI] [PubMed] [Google Scholar]
- 18.Drossman DA, Patrick DL, Whitehead WE, Toner BB, Diamant NE, Hu Y, Jia H, Bangdiwala SI. Further validation of the IBS-QOL: a disease-specific quality-of-life questionnaire. Am J Gastroenterol. 2000;95:999–1007. doi: 10.1111/j.1572-0241.2000.01941.x. [DOI] [PubMed] [Google Scholar]
- 19.Jamali R, Jamali A, Poorrahnama M, Omidi A, Jamali B, Moslemi N, Ansari R, Dolatshahi S, Ebrahimi Daryani N. Evaluation of health related quality of life in irritable bowel syndrome patients. Health Qual Life Outcomes. 2012;10:12. doi: 10.1186/1477-7525-10-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weinryb RM, Osterberg E, Blomquist L, Hultcrantz R, Krakau I, Asberg M. Psychological factors in irritable bowel syndrome: a population-based study of patients, non-patients and controls. Scand J Gastroenterol. 2003;38:503–510. doi: 10.1080/00365520310002166. [DOI] [PubMed] [Google Scholar]
- 21.Mezzani A, Grassi B, Giordano A, Corrà U, Colombo S, Giannuzzi P. Age-related prolongation of phase I of VO2 on-kinetics in healthy humans. Am J Physiol Regul Integr Comp Physiol. 2010;299:R968–R976. doi: 10.1152/ajpregu.00739.2009. [DOI] [PubMed] [Google Scholar]
- 22.Ladwig KH, Klupsch D, Ruf E, Meisinger C, Baumert J, Erazo N, Wichmann HE. Sex- and age-related increase in prevalence rates of death wishes and suicidal ideation in the community: results from the KORA-F3 Augsburg Study with 3,154 men and women, 35 to 84 years of age. Psychiatry Res. 2008;161:248–252. doi: 10.1016/j.psychres.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 23.Miwa H. Prevalence of irritable bowel syndrome in Japan: Internet survey using Rome III criteria. Patient Prefer Adherence. 2008;2:143–147. [PMC free article] [PubMed] [Google Scholar]
- 24.Lovell RM, Ford AC. Effect of gender on prevalence of irritable bowel syndrome in the community: systematic review and meta-analysis. Am J Gastroenterol. 2012;107:991–1000. doi: 10.1038/ajg.2012.131. [DOI] [PubMed] [Google Scholar]
- 25.Rogers J, Henry MM, Misiewicz JJ. Increased segmental activity and intraluminal pressures in the sigmoid colon of patients with the irritable bowel syndrome. Gut. 1989;30:634–641. doi: 10.1136/gut.30.5.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wouters MM, Boeckxstaens GE. Neuroimmune mechanisms in functional bowel disorders. Neth J Med. 2011;69:55–61. [PubMed] [Google Scholar]
- 27.Sachdeva S, Rawat AK, Reddy RS, Puri AS. Small intestinal bacterial overgrowth (SIBO) in irritable bowel syndrome: frequency and predictors. J Gastroenterol Hepatol. 2011;26 Suppl 3:135–138. doi: 10.1111/j.1440-1746.2011.06654.x. [DOI] [PubMed] [Google Scholar]
- 28.Faure C, Wieckowska A. Somatic referral of visceral sensations and rectal sensory threshold for pain in children with functional gastrointestinal disorders. J Pediatr. 2007;150:66–71. doi: 10.1016/j.jpeds.2006.08.072. [DOI] [PubMed] [Google Scholar]
- 29.Dorn SD, Palsson OS, Thiwan SI, Kanazawa M, Clark WC, van Tilburg MA, Drossman DA, Scarlett Y, Levy RL, Ringel Y, et al. Increased colonic pain sensitivity in irritable bowel syndrome is the result of an increased tendency to report pain rather than increased neurosensory sensitivity. Gut. 2007;56:1202–1209. doi: 10.1136/gut.2006.117390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Heitkemper MM, Chang L. Do fluctuations in ovarian hormones affect gastrointestinal symptoms in women with irritable bowel syndrome? Gend Med. 2009;6 Suppl 2:152–167. doi: 10.1016/j.genm.2009.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen HH, Yeh HL, Tsai SJ. Association of lower hemoglobin levels with depression, though not with cognitive performance, in healthy elderly men. Psychiatry Clin Neurosci. 2012;66:367–369. doi: 10.1111/j.1440-1819.2012.02347.x. [DOI] [PubMed] [Google Scholar]
- 32.Driscoll I, Martin B, An Y, Maudsley S, Ferrucci L, Mattson MP, Resnick SM. Plasma BDNF is associated with age-related white matter atrophy but not with cognitive function in older, non-demented adults. PLoS One. 2012;7:e35217. doi: 10.1371/journal.pone.0035217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mazzotti DR, Guindalini C, Sosa AL, Ferri CP, Tufik S. Prevalence and correlates for sleep complaints in older adults in low and middle income countries: a 10/66 Dementia Research Group study. Sleep Med. 2012;13:697–702. doi: 10.1016/j.sleep.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 34.Johnson DP, Whisman MA, Corley RP, Hewitt JK, Rhee SH. Association between depressive symptoms and negative dependent life events from late childhood to adolescence. J Abnorm Child Psychol. 2012;40:1385–1400. doi: 10.1007/s10802-012-9642-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Riso LP, Miyatake RK, Thase ME. The search for determinants of chronic depression: a review of six factors. J Affect Disord. 2002;70:103–115. doi: 10.1016/s0165-0327(01)00376-7. [DOI] [PubMed] [Google Scholar]
- 36.Walter S, Hjortswang H, Holmgren K, Hallböök O. Association between bowel symptoms, symptom severity, and quality of life in Swedish patients with fecal incontinence. Scand J Gastroenterol. 2011;46:6–12. doi: 10.3109/00365521.2010.513059. [DOI] [PubMed] [Google Scholar]
- 37.Jerndal P, Ringström G, Agerforz P, Karpefors M, Akkermans LM, Bayati A, Simrén M. Gastrointestinal-specific anxiety: an important factor for severity of GI symptoms and quality of life in IBS. Neurogastroenterol Motil. 2010;22:646–e179. doi: 10.1111/j.1365-2982.2010.01493.x. [DOI] [PubMed] [Google Scholar]
- 38.Cho HS, Park JM, Lim CH, Cho YK, Lee IS, Kim SW, Choi MG, Chung IS, Chung YK. Anxiety, depression and quality of life in patients with irritable bowel syndrome. Gut Liver. 2011;5:29–36. doi: 10.5009/gnl.2011.5.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pines A, Sturdee DW, MacLennan AH. Quality of life and the role of menopausal hormone therapy. Climacteric. 2012;15:213–216. doi: 10.3109/13697137.2012.655923. [DOI] [PubMed] [Google Scholar]
- 40.Mykletun A, Jacka F, Williams L, Pasco J, Henry M, Nicholson GC, Kotowicz MA, Berk M. Prevalence of mood and anxiety disorder in self reported irritable bowel syndrome (IBS). An epidemiological population based study of women. BMC Gastroenterol. 2010;10:88. doi: 10.1186/1471-230X-10-88. [DOI] [PMC free article] [PubMed] [Google Scholar]