Abstract
Radiation-induced gastritis is an infrequent cause of gastrointestinal bleeding. It is a serious complication arising from radiation therapy, and the standard treatment method has not been established. The initial injury is characteristically acute inflammation of gastric mucosa. We presented a 46-year-old male patient with hemorrhagic gastritis induced by external radiotherapy for metastatic retroperitoneal lymph node of hepatocellular carcinoma. The endoscopic examination showed diffuse edematous hyperemicmucosa with telangiectasias in the whole muscosa of the stomach and duodenal bulb. Multiple hemorrhagic patches with active oozing were found over the antrum. Anti-secretary therapy was initiated for hemostasis, but melena still occurred off and on. Finally, he was successfully treated by prednisolone therapy. We therefore strongly argue in favor of perdnisolone therapy to effectively treat patients with radiation-induced hemorrhagic gastritis.
Keywords: Hemorrhagic gastritis, Radiation, Prednisolone, Hepatocellular carcinoma, Gastrointestinal bleeding
INTRODUCTION
Radiation-induced gastritis is a serious complication of radiation therapy and can cause upper gastrointestinal bleeding. There have been no effective options to manage this complication. We encountered a 46-year-old male patient with hemorrhagic gastritis induced by external radiotherapy for the treatment of metastatic retroperitoneal lymph node of hepatocellular carcinoma (HCC). Successful hemostasis was achieved with treatment of prednisolone.
CASE REPORT
A 46-year-old man diagnosed with HCC received left lobectomy in December 2010. Two courses of transcatheter arterial chemoembolization with 5-fluorouracil, oxaliplatin, mitomycin and lipidol (5-10 mL) were administered from January 2011 to July 2011 for intrahepatic recurrence. He received liver transplantation in September 2011. He was treated with sorafenib 400 mg bid from January 2011. In November 2011, he received helical radiotherapy using tomotherapy (total 63.7 Gy) for the treatment of metastatic retroperitoneal lymph node. The dosages delivered to the stomach, intestine and liver were 18.70 Gy, 18.10 Gy and 10.78 Gy, respectively. During the course of radiotherapy, sirolimus was continued against transplantation rejection and sorafenib was discontinued. Three months after radiotherapy, the patient had hematemesis and melena. He was admitted to the emergency room. His vital signs were quite unstable: blood pressure was 84/56 mmHg; heart rate was 92 beats/min and respiratory rate was 20 breaths/min. Laboratory evaluation revealed severe anemia with a hemoglobin level of 37 g/L, prothrombin time was 11.4 s, activated partial thromboplastin time was 27.5 s, international normalization ratio was 0.98 and platelets was 68 × 109/L. Blood transfusion was administered. The endoscopic examination showed diffuse edematous hyperemicmucosa with telangiectasis in the whole muscosa of the entire examined stomach and duodenal bulb. Multiple hemorrhagic patches with active oozing were visible over the antrum (Figure 1A). He was diagnosed as having radiation-induced gastritis. Omeprazole (40 mg bid iv) and sucralfate (1 g tid oral) were given for a week. However, upper gastrointestinal bleeding still occurred off and on. Due to the inaccessibility of argon plasma coagulation, he was treated with prednisolone. The starting dose of prednisolone was 40 mg daily. Hematemesis and melena stopped 3 d later, and fecal occult blood test was negative. Then, he received oral prednisone, 25 mg daily. The dosage was gradually reduced by 5 mg every 3 d and down to zero within 15 d after hospital discharge. His hemoglobin levels improved to 60 g/L. Unfortunately, 2 wk after prednisone was discontinued, his melena recurred. The endoscopic examination still showed multiple hemorrhagic spot at antral mucosa (Figure 1B). The hemoglobin levels decreased to 34 g/L. We treated him with prednisolone again. Within 3 d, his hematocrit stabilized and the melena resolved. He then received maintenance prednisone (10 mg daily). One month later, he underwent follow-up endoscopy, which revealed some residual telangiectasias with no bleeding friability (Figure 1C). No gastrointestinal bleeding recurred. His hemoglobin levels improved to 88 g/L without blood transfusions or iron supplements.
Figure 1.
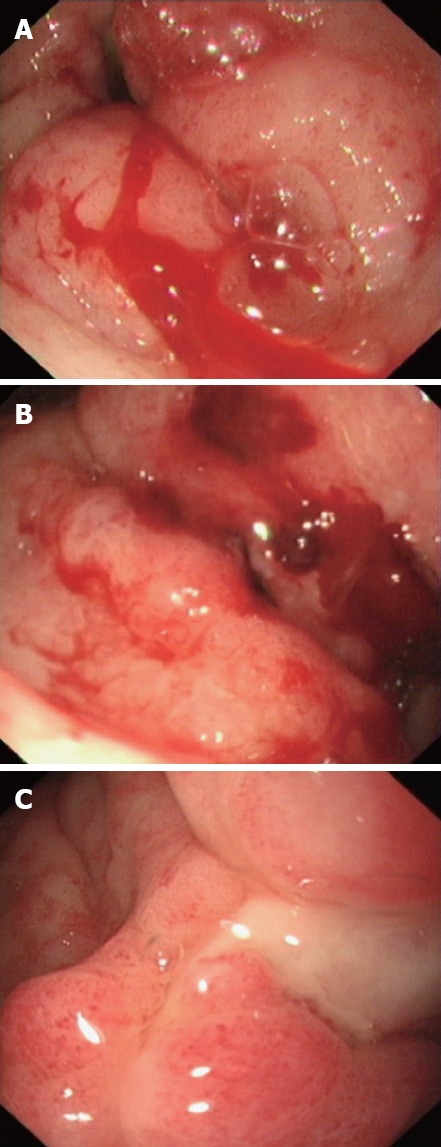
Endoscopic appearance of antral mucosa. A: Multiple telangiectasias spontaneously bleeding at diffuse antral mucosa after radiation therapy; B: After prednisone was discounted, multiple hemorrhagic spots were still visible at antral mucosa; C: After 1 mo of prednisone maintenance therapy, there were residual telangiectasias with no bleeding tendency.
DISCUSSION
Radiation-induced gastritis is a serious complication of radiation therapy and difficult to manage. It usually happens 2-9 mo after initial radiotherapy[1-3]. A high total dose and, above all, high daily fraction appear to be the main risk factors in gastric injuries. Radiologic durability dosage of the stomach and intestine is defined as 45 Gy, and that of rectum is defined as 55 Gy. The initial injury is characteristically acute inflammation of gastric mucosa. If injury progresses, vasculopathy may evolve to progressive obliterative endarteritis and endothelial proliferation, leading to mucosal ischemia, ulceration, and telangiectasias[4]. The characteristic endoscopic finding is the presence of telangiectasia. Other endoscopic findings include diffuse erythema of mucosa, shallow or deep ulcers and scar formation.
Radiation-induced hemorrhagic gastritis is a diffuse process with multiple bleeding sites[4]. The standard method has not been established. Repeated endoscopies and the anti-secretory agents all yielded unsatisfactory control of bleeding. Argon plasma coagulation had been reported for successful hemostasis of radiation-induced hemorrhagic gastritis, colitis and proctitis[1,2,5-7]. Surgery may be necessary if other treatment fails, but it is associated with a high morbidity.
Rectal steroids have often been recommended for the treatment of radiation-induced proctitis. Kochhar et al[8] reported that steroids successfully treated radiation-induced proctosigmoiditis. But only few instances of steroids therapy for radiation induced gastritis have been reported. In our case, we chose to use prednisolone because prednisolone can reduce inflammation. Although the pathogenesis of radiation-induced gastritis is not entirely clear, it was presumed to be an inflammatory process. A large number of cell types, interacting molecular signals including cytokines and growth factors, and various molecules on the endothelial cell surface are involved. It was reported that the mucosal levels of interleukin (IL)-2, IL-6, and IL-8 were significantly higher in patients with radiation proctitis[9]. Prednisolone can inhibit inflammation by a diverse array of mechanisms, including decreasing chemotaxis of monocytes and neutrophils, inhibiting adhesive molecule synthesis and decreasing eicosanoid production. Prednisolone’s anti-inflammatory functions may reduce gastric mucosa damage and degeneration as well.
In this case, the upper gastrointestinal bleeding recurred when prednisone was discounted. It indicated that sufficient time of prednisone administration is needed for the effective treatment. In fact, when the patient received prednisone for a prolonged duration, no gastrointestinal bleeding recurred. Therefore, the patients with radiation-induced hemorrhagic gastritis should continue with maintenance prednisone because the radiation-induced injury is a chronic course and may last a long time.
During radiotherapy, the patient continued taking sirolimus against transplantation rejection, which also has an anti-angiogenic effect. Many studies have shown that anti-angiogenetic agent in combination with radiotherapy produces a synergistic anti-tumor efficacy without increasing toxicity[10,11].
This report described a further potential treatment modality for radiation- induced hemorrhagic gastritis. More patients and longer follow-up are necessary to confirm the effectiveness of prednisolone in this form of gastritis.
Footnotes
Peer reviewers: Kevin Cheng-Wen Hsiao, MD, Assistant Professor, Colon and Rectal Surgery, Tri-Service General Hospital, No. 325, Sec. 2, Cheng-Kung Rd, Nei-Hu District, Taipei 114, Taiwan, China; Dr. Stéphane Supiot, MD, PhD, Department of Radiation Oncoology, Centre René Gauducheau, St-Herblain, 44800 Nantes, France
S- Editor Jiang L L- Editor Ma JY E- Editor Xiong L
References
- 1.Wada S, Tamada K, Tomiyama T, Yamamoto H, Nakazawa K, Sugano K. Endoscopic hemostasis for radiation-induced gastritis using argon plasma coagulation. J Gastroenterol Hepatol. 2003;18:1215–1218. doi: 10.1046/j.1440-1746.2003.03149.x. [DOI] [PubMed] [Google Scholar]
- 2.Shukuwa K, Kume K, Yamasaki M, Yoshikawa I, Otsuki M. Argon plasma coagulation therapy for a hemorrhagic radiation-induced gastritis in patient with pancreatic cancer. Intern Med. 2007;46:975–977. doi: 10.2169/internalmedicine.46.0076. [DOI] [PubMed] [Google Scholar]
- 3.Toyoda H, Jaramillo E, Mukai K, Saito T, Imai N, Naota H, Sase T, Mizuno T, Shiku H, Imoto I, et al. Treatment of radiation-induced hemorrhagic duodenitis with argon plasma coagulation. Endoscopy. 2004;36:192. doi: 10.1055/s-2004-814193. [DOI] [PubMed] [Google Scholar]
- 4.Grover N, Johnson A. Aminocaproic acid used to control upper gastrointestinal bleeding in radiation gastritis. Dig Dis Sci. 1997;42:982–984. doi: 10.1023/a:1018828801379. [DOI] [PubMed] [Google Scholar]
- 5.Taïeb S, Rolachon A, Cenni JC, Nancey S, Bonvoisin S, Descos L, Fournet J, Gérard JP, Flourié B. Effective use of argon plasma coagulation in the treatment of severe radiation proctitis. Dis Colon Rectum. 2001;44:1766–1771. doi: 10.1007/BF02234452. [DOI] [PubMed] [Google Scholar]
- 6.Venkatesh KS, Ramanujam P. Endoscopic therapy for radiation proctitis-induced hemorrhage in patients with prostatic carcinoma using argon plasma coagulator application. Surg Endosc. 2002;16:707–710. doi: 10.1007/s00464-001-8164-0. [DOI] [PubMed] [Google Scholar]
- 7.Tjandra JJ, Sengupta S. Argon plasma coagulation is an effective treatment for refractory hemorrhagic radiation proctitis. Dis Colon Rectum. 2001;44:1759–1765; discussion 1771. doi: 10.1007/BF02234451. [DOI] [PubMed] [Google Scholar]
- 8.Kochhar R, Patel F, Dhar A, Sharma SC, Ayyagari S, Aggarwal R, Goenka MK, Gupta BD, Mehta SK. Radiation-induced proctosigmoiditis. Prospective, randomized, double-blind controlled trial of oral sulfasalazine plus rectal steroids versus rectal sucralfate. Dig Dis Sci. 1991;36:103–107. doi: 10.1007/BF01300096. [DOI] [PubMed] [Google Scholar]
- 9.Indaram AV, Visvalingam V, Locke M, Bank S. Mucosal cytokine production in radiation-induced proctosigmoiditis compared with inflammatory bowel disease. Am J Gastroenterol. 2000;95:1221–1225. doi: 10.1111/j.1572-0241.2000.02013.x. [DOI] [PubMed] [Google Scholar]
- 10.Hu J, Chen LJ, Liu L, Chen X, Chen PL, Yang G, Hou WL, Tang MH, Zhang F, Wang XH, et al. Liposomal honokiol, a potent anti-angiogenesis agent, in combination with radiotherapy produces a synergistic antitumor efficacy without increasing toxicity. Exp Mol Med. 2008;40:617–628. doi: 10.3858/emm.2008.40.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mazeron R, Anderson B, Supiot S, Paris F, Deutsch E. Current state of knowledge regarding the use of antiangiogenic agents with radiation therapy. Cancer Treat Rev. 2011;37:476–486. doi: 10.1016/j.ctrv.2011.03.004. [DOI] [PubMed] [Google Scholar]


