Sir,
Microorganisms responsible for urinary tract infection (UTI) such as Escherichia coli and Klebsiella spp. have the ability to produce extended-spectrum ß-lactamases (ESBL) in large quantities. These enzymes are plasmid borne and confer multiple drug resistance, making urinary tract infection difficult to treat.[1] ESBLs are plasmid mediated, TEM- and SHV-derived enzymes, first isolated in Western Europe in mid-1980s, most commonly in Klebsiella spp., followed by E. coli.[2] ESBLs are enzymes capable of conferring bacterial resistance to the penicillins, first, second- and third-generation cephalosporins, and aztreonam (but not the cephamycins or carbapenems) by hydrolysis of these antibiotics.[3]
This study was undertaken to find out ESBL production in urinary isolates of E. coli and Klebsiella pneumoniae and to evaluate double disc synergy (DDS) test against Clinical and Laboratory Standards Institute (CLSI) recommended the phenotypic disc confirmatory test (PCT) test for detection of ESBLs.
A total of 229 isolates [E. coli (171) and K. pneumoniae (58)] with significant growth were studies. Screening for ESBL production was done by the disc diffusion test recommended by CLSI and screen positive isolates were confirmed by DDS and PCT.
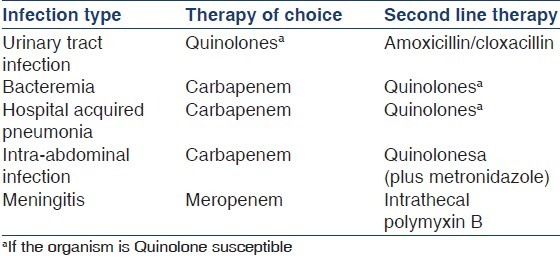
Of the 171 E. coli isolates, ESBL production was observed in 69 (40.4 %) whereas from 58 K. pneumoniae, ESBL production was found in 26 (44.9 %) isolates. Prevalence was more among K. pneumoniae. In a study conducted in 2003,[4] the prevalence was only 18.5% amongst E. coli isolates and 25.6% among K. pneumoniae isolates. Taneja et al.[5] have reported 40.2% E. coli isolates and 51.2% of K. pneumoniae to be ESBL producers. The prevalence of ESBL in this study is high and poses a threat to treatment of serious infections due to these isolates. Most ESBL producing isolates were resistant to ampicillin, co-trimoxazole, ciprofloxacin, and ceftazidime. Under such circumstances the only treatment options are carbapenems and tigecycline that are expensive and often not available in developing countries. However, quinolones may be regarded as the treatment of choice for UTI [Table 1] due to ESBL producing organisms if there is not in vitro resistance to these drugs.[3] Unfortunately, increasing resistance of quinolones will limit the role of these in future.
Table 1.
Recommended treatment for infections with ESBL-producing organism
This study evaluated DDS against CLSI recommended PCT for detection of ESBL. Of the two tests used in the study PCT was more sensitive. Eight six (90.5 %) of the 95 ESBL producing strains were detected by DDST. We found that PCT was an inexpensive alternative to DDS for detection of ESBL. DDS lacks sensitivity because of problem of the optimal disc space and correct storage of the clavulanate containing discs. This method is technically simple and inexpensive.[6] All the isolates positive by confirmatory methods should be reported as resistant to all cephalosporins even if the organism is susceptible by routine disc diffusion methods for antibiotic sensitivity.
References
- 1.Babypadmini S, Appalaraju B. Extended spectrum ß-lactamases in urinary isolates of Escherichia coli and Klebsiella pneumoniae - prevalence and susceptibility pattern in a tertiary care hospital. Indian J Med Microbiol. 2004;22:172–4. [PubMed] [Google Scholar]
- 2.Chaudhary U, Aggarwal R. Extended spectrum β-lactamases (ESBL) - An emerging threat to clinical therapeutics. Indian J Med Microbiol. 2004;22:75–80. [PubMed] [Google Scholar]
- 3.Paterson DL, Bonomo RA. Extended- spectrum ß-lactamases: a clinical update. Clin Microbiol Rev. 2005;18:657–86. doi: 10.1128/CMR.18.4.657-686.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tankhiwale SS, Jalgaonkar SV, Ahamad S, Hassani U. Evaluation of extended spectrum beta lactamase in urinary isolates. Indian J Med Res. 2004;120:553–6. [PubMed] [Google Scholar]
- 5.Taneja N, Rao P, Arora J, Dogra A. Occurrence of ESBL and Amp-C ß-lactamases and susceptibility to newer antimicrobial agents in complicated UTI. Indian J Med Res. 2008;127:85–8. [PubMed] [Google Scholar]
- 6.Shukla I, Tiwari R, Agrawal M. Prevalence of extended spectrum- β-lactamase producing Klebsiella pneumoniae in a tertiary care hospital. Indian J Med Microbiol. 2004;22:87–91. [PubMed] [Google Scholar]


