Abstract
Increased use of complementary and alternative herbal medicines in the treatment of various diseases.Some herbal therapies may be causes of potential toxicity that may be renal toxicity caused by the ingestion of herbs. The goal of this study is the toxic and beneficial effects of medicinal herbs on renal health by which evidence for benefit or toxicity has been found. Included are nephrotoxicity from aristolochic acid and other components within herbs, herb-drug interactions, heavy metal toxicity in herbs and adulterants during careless preparation of herbal medicine, resulting in adverse renal effects and renal toxicity from contaminants within the extracts. The review aims to provide knowledge and guide to encourage future toxicity studies on the kidney by medicinal herbs.
Keywords: Adverse effects, herbal medicines, nephrotoxicity
INTRODUCTION
Many problems in primary healthcare are due to lack of knowledge and sensitivity to local health practices, and due to the economic and cultural factors associated with these practices. However, available herbal products have no clear statement of content or medically related information on the package labels, and have not been validated or certified by any recognized body. This concerns consumers and medical practitioners who may unknowingly counter-prescribe these herbal products. Not all of the plants reported to be useful are harmless. These considerations underlie the study of ethno-medicinal plants.[1] In recent years, an increasing number of people have been using complementary and alternative medicines.[2] The herbal therapies appear most promising, thus encouraging the necessary toxicity studies to be performed on these therapies. The literature search was performed that the herbs are reported regarding renal toxicity if there is in vivo evidence of toxicity in animals or humans. The herbs will also be defined as “potentially beneficial” to the kidneys if there is strong in vivo evidence of renal protection from toxic substances or drugs. These herbal drugs mainly act as specific renal anti-oxidant, in vivo antiproliferative or in vivo evidence of being beneficial in renal disease or renal failure. This article presents information about the toxicity of medicinal herbs on kidney functions. This article focuses on the plants used for various diseases but also cause urinary problems.[3–7]
ARISTOLOCHIC ACID
The mostly renal toxicity caused by unadulterated medicinal herbs is aristolochic acid (AA) nephropathy.[8,9] The S. tetrandra had been inadvertently replaced by Aristolochiafangchi by the manufacturers of the weight-reducing formula.[7] A. fangchicontains AA, a plant alkaloid, which is nephrotoxic and carcinogenic in humans and animals.[10–12] The AA nephropathy is characterized by extensive renal interstitial fibrosis and tubular atrophy, which generally decreases in intensity from the outer to the inner cortex.[13] Endothelial cell swelling is often apparent with consequent thickening of interlobular and afferent arterioles. Uroepithelial malignancies are common, especially with total cumulative dose of A. fangchiin excess of 200 g.[14]
Although the reports have hypothesized that phytotherapy-associated interstitial nephritis is caused by a combination of phytotoxins within herbal medicines, in these cases there is rapidly progressing diffusely fibrosing interstitial nephritis and a lack of glomerular lesions. There was no supporting evidence for the existence of other phytotoxins. The endemic nephropathy is closely associated with chronic oral intake of food contaminated with the fungal mycotoxin, ochratoxin A (OTA).[15] While the researchers concluded that OTA was not involved in the nephropathy, it is possible that long-term consumption of small amounts of OTA combined with short-term exposure to AA may play a role in the urothelial malignancy. OTA is a widespread natural contaminant in foods.[16] The medicinal herbs containing S. tetrandaand other herbs that may be substituted with herbs from the genus Aristolochia, AA, have been detected. The AA nephropathy causes an increased risk of uroepithelial malignancies in patients.
Nephrotoxicity of herbs and herbal preparations
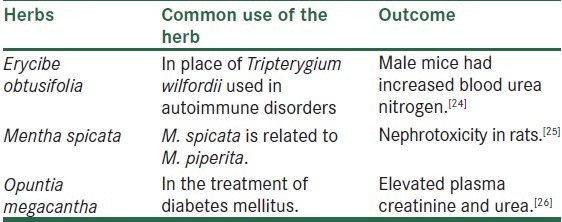
The herbal treatments for complications caused by dialysis and chronic renal failure and any use of medicinal herbs may be inappropriate for the renal patient.[17,18] Literature on herbs and the dialysis patient suggested the avoidance of borage (Boragoofficinalis), comfrey (Symphytumspp.), coltsfoot (Tussilagofarfara) and life root (Senecioaureus) because of their pyrrolizidine alkaloid content and hence hepatotoxic potential, and sassafras (Sassafras albidum) because of its safrole content.[19] This included the avoidance of chaparral (Larreatridentata), germander (Teucriumchamaedrys) and life root (Senecioaureus), also because of their potential hepatotoxic effects. The licorice (Glycyrrhizaglabra) has the ability to affect water retention, blood pressure and serum levels of electrolytes, and ephedrine from ephedra has vasoconstrictive actions. Star fruit (Averrhoacarambola) consumption should be completely avoided by uremic patients because of the rare but potentially fatal complications, and grapefruit juice is known to have antagonistic effects on the cytochrome P450 enzymes. Considerable work on the toxicity and actions of these and other herbs needs to be completed, and also on use of herbal remedies during dialysis. There is reported nephrotoxicity caused by specific medicinal herbs.[20] Aside from AA, adverse unadulterated herb reactions resulting in notable kidney manifestations are usually caused by an abuse of the substance or ignorance regarding the herb's intended administration. The most common example involves ephedra (Ephedra sinica spp.), which contains ephedrine. The adrenergic effects of ephedrine have led to several warnings regarding its potential toxicity and those effects combined with potential hepatotoxicity. Ephedra has been touted as a weight-loss and energy-enhancing agent, leading to frequent abuse, while adverse effects usually involve the cardiovascular and central nervous system, and its ability to cause ephedrine and ephedrine-metabolite nephrolithiasis [Tables 1 and 2].[27] Acute renal failure due to the herbal remedy,[28] CKLS (colon, kidneys, liver, spleen) comprises aloe (Aloe vera), chamomile (probably Chamaemelumnobile or Matricariarecutita), Cascara sagrada (Rhamnuspurshiana), chaparral (Larrea tridentate/L. divaricata), mullein (Verbascumthapsus), bearberry (Arctostaphylosuva-ursi), fenugreek (Trigonellafoenum-graecum), cayenne (Capsicum minimum/C. frutescens), dandelion (Taraxacumofficinale) and eucalyptus (Eucalyptus spp.). Salvia miltiorrhiza root, Pinellia spp. tuber, safflower, Trichosanthes spp., Ephedra spp., Corydalis spp. root, Paeonialactiflora root, Typha spp. pollen, Curcuma aromatica root, “Trifoliate orange peel,” Ganodermajaponicum and pigeon droppings also causes nephrotoxicities.[29]
Table 1.
Adverse renal reactions potentially caused by the ingestion of herbal preparations
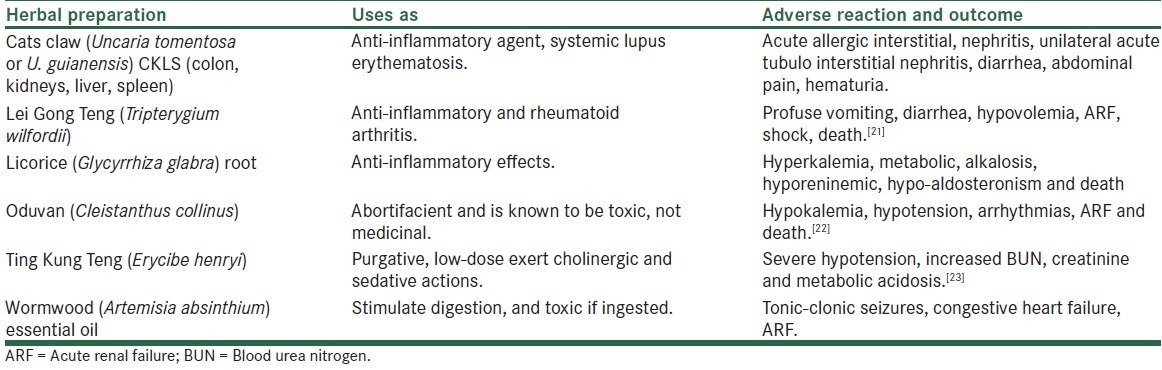
Table 2.
Animal studies showing potential renal toxicity
Herb–drug interactions
One of the dangers with any combination of medicinal substances is the potential interaction between the two agents. The potentially worst herb–drug reaction is that of Hypericumperforatum and drugs metabolized by cytochrome P450 CYP 3A4 isoenzymes. This is particularly important in patients awaiting renal transplant,[30,31] as cyclosporin, a commonly used immunosuppressant, is metabolized via the CYP 3A4 isoenzymes and co-administration of H. perforatum and cyclosporin results in the rapid depletion of the immunosuppressant. Another interaction of concern involves the polyherbal mixture, which increases blood concentrations of prednisolone.[32,33]
Toxicity from heavy metal adulterants in herbs
Heavy metals are present in foods and vegetables if they are grown in heavy metal-contaminated soils and other factors. Heavy metal toxicity is reported in any age with anemia, neuropathy, hypertension, kidney or liver dysfunction and cancer or other symptoms.[34] Adulteration of herbal preparations appears to be more common or may cause significant problems, especially in children.[35,36] Heavy metal poisoning in children consuming herbal preparations is reported, and while none of these resulted in acute renal toxicity, there is concern that these contaminants may have the potential to contribute to chronic or insidious health disorders.[29] Renal toxicities of various medicinal herbs in pharmaceutical products, on the basis reported the analysis of some products finding that few contained undeclared pharmaceuticals or heavy metals.[36,37] Ephedrine, chlorpheniramine, methyltestosterone, phenacetin, lead, arsenic and mercury were among the contaminants. Other reports of contamination include thallium intoxication caused by Chinese herbal medicine. When pharmaceuticals are placed within herbal mixtures, they are normally meant to enhance the medicinal properties of the mixture; however, serious adverse consequences can result.[38] In one example, they reported a patient with acute interstitial nephritis that was caused by the consumption of a Chinese herbal formula containing diazepam and mefanamic acid.[37,39,40]
In some cases, heavy metals in Chinese and Ayurvedic medicines originate from the heavily polluted soil and irrigation water in China and India, as plants take up heavy metals through their roots. Lead and cadmium levels in medicinal plants from India were highest in the leaves, and herbal medicines using that part of the plant generally have higher environmentally induced heavy metal contents. In other cases, the heavy metals or other adulterants are deliberately placed in the mixture. Within Chinese traditional medicines, small amounts of Realgar, a mineral containing mainly arsenic sulfide, and Cinnabaris, a mineral containing mainly mercuric sulfide, are deliberately used in some Chinese medicines. However, the high contamination in parts of China and India,[38,41,42] combined with the possibility of accidental contamination during manufacturing, demands continued analysis of imported herbal medicines.
Nutrition and chronic kidney disease
In summary, a diet rich in fruits and vegetables significantly reduces the risk of heart diseases, type-2 diabetes, some types of cancer, obesity, Alzheimer's disease and kidney toxicity. This effect can be further increased by including wholegrain foods, nuts and certain oils (omega-3 oils) in the diet. Diets high in fiber and low in fat can decrease heavy metal risks along with their other benefits.[43] Diets high in antioxidant plant foods and sulfur compounds may be protective against heavy metal toxicity in addition to other benefits such as decreasing risk of cancer. For the treatment of chronic kidney diseases, diet is an important part of the treatment. The recommended diet may change over time if kidney disease gets worse. Some things are important to the diet like getting the right amount of protein, calories, and other nutrients in right amount such as fluids, vitamins and minerals like sodium, phosphorus, calcium, and potassium that can help the kidney functions. High amount of protein may cause serious problem in chronic renal patients.
Kidney disease, hypertension and sodium are often related. Therefore, one may need to limit the amount of sodium in diet by selecting foods that are lower in sodium. Potassium helps the muscles and heart to work properly. Too much or too little sodium and potassium in the blood can be dangerous.[44] Generally there is no need to limit the amount of fluids drunk in the earlier stages of kidney disease. If kidney disease gets worse, one needs to limit fluids. Vitamins and minerals come from a variety of foods. If diet is limited, one may need to take special vitamins or minerals. Certain vitamins and minerals may be harmful to people with chronic kidney disease.
Goals for kidney healthcare
The kidneys are protected through adequate consumption of water. Bones and kidneys are aided through avoiding excess protein intake, except in special circumstances such as pregnancy and childhood. Foods high in fiber limit the uptake of heavy metals. Many heavy metals take part in creation of free radicals in the cellular environment. A diet high in anti-oxidants can reduce these effects, by use of more fruits and vegetables in the diet. The highly toxic levels of lead or cadmium may be treated with chelation therapy. A low-fat diet reduces cadmium uptake. Including high-sulfur foods in the diet may limit cadmium effects. It carries serious risks since it removes calcium and iron and other nutrients from the body.[45] Dietary factors affect heavy metal uptake. For example, an adequate level of dietary iron reduces uptake of cadmium and lead.[46] Dietary calcium reduces the uptake of cadmium. Good habits that can reduce the intake and uptake of toxic metals include eating a balanced diet that is high in fiber, eating organic foods and avoiding foods grown with pesticides and artificial fertilizers or in contaminated soils. Including high-sulfur foods such as onions, garlic, legumes, and eggs probably assists the body in blocking uptake and decreasing retention of many toxic metals.[47] This review reported evidencesof nephrotoxicities of many herbs or herbal products,inorganic and heavy metals that affect nephron activity. However, evidence continues to favor excessive AA nephropathy and heavy metal toxicities. These agents are also playing a leading role in causes other serious health problems. Many reports suggest that long-term benefits of reducing excessive intake of metals and heavy metals for reducing not only kidney diseases but also the risk of other diseases.[41,42]
CONCLUSIONS
Some herbal medicine may exert renal toxicity through their inherent properties. If found to have some degree of toxicity, the risks can be weighed against the benefits and decisions can be made regarding their continued availability, in a manner similar to that which is presently performed for nephrotoxic pharmaceutical agents. Importantly, the inherent properties of the herb are not the only source of herb-associated renal disorders, as herb-drug interactions, mistakes in dosage and identification, and contaminants within the mixture are all issues of concern. Strict controls on the presence of adulterants within herbal medicines, labeling of dosages and contraindications, and manufacturing techniques must be maintained to ensure the safety of those consuming herbal medicines.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Lans CA. Ethnomedicines used in Trinidad and Tobago for urinary problems and diabetes mellitus. J EthnobiolEthnomed. 2006;2:45. doi: 10.1186/1746-4269-2-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.MacLennan AH, Wilson DH, Taylor AW. The escalating cost and prevalence of alternative medicine. Prev Med. 2002;35:166–73. doi: 10.1006/pmed.2002.1057. [DOI] [PubMed] [Google Scholar]
- 3.Cheng S. Heavy metals in plants and phytoremediation. Environ SciPollut Res. 2003;10:335–40. doi: 10.1065/espr2002.11.141.3. [DOI] [PubMed] [Google Scholar]
- 4.Cosyns JP, Jadoul M, Squifflet JP, Wese FX, van Ypersele de Strihou C. Urothelial lesions in Chinese-herb nephropathy. Am J Kidney Dis. 1999;33:1011–7. doi: 10.1016/S0272-6386(99)70136-8. [DOI] [PubMed] [Google Scholar]
- 5.Gorey JD, Wahlqvist ML, Boyce NW. Adverse reaction to a Chinese herbal remedy. Med J Aust. 1992;157:484–6. doi: 10.5694/j.1326-5377.1992.tb137315.x. [DOI] [PubMed] [Google Scholar]
- 6.Hilepo JN, Bellucci AG, Mossey RT. Acute renal failure caused by ‘cat's claw’ herbal remedy in a patient with systemic lupus erythematosus. Nephron. 1997;77:61. doi: 10.1159/000190304. [DOI] [PubMed] [Google Scholar]
- 7.Vanherweghem LJ. Misuse of herbal remedies: The case of an outbreak of terminal renal failure in Belgium (Chinese herbs nephropathy) J Altern Complement Med. 1998;4:9–13. doi: 10.1089/acm.1998.4.1-9. [DOI] [PubMed] [Google Scholar]
- 8.Gillerot G, Jadoul M, Arlt VM, van Ypersele De Strihou C, Schmeiser HH, But PP, et al. Aristolochic acid nephropathy in a Chinese patient: Time to abandon the term ‘Chinese herbs nephropathy’.? Am J Kidney Dis. 2001;38:E26. doi: 10.1053/ajkd.2001.28624. [DOI] [PubMed] [Google Scholar]
- 9.Solez K, Daugirdas J, Gregory MC, Frohnert PP, Bhowmik DM, Jha V, et al. Is ‘Chinese herbs nephropathy’ a prejudicial term.? Am J Kidney Dis. 2001;38:1141–2. doi: 10.1053/ajkd.2001.29661. [DOI] [PubMed] [Google Scholar]
- 10.Bieler CA, Stiborova M, Wiessler M, Cosyns JP, van Ypersele de Strihou C, Schmeiser HH. 32P-post-labelling analysis of DNA adducts formed by aristolochic acid in tissues from patients with Chinese herbs nephropathy. Carcinogenesis. 1997;18:1063–7. doi: 10.1093/carcin/18.5.1063. [DOI] [PubMed] [Google Scholar]
- 11.Schmeiser HH, Bieler CA, Wiessler M, van Ypersele de Strihou C, Cosyns JP. Detection of DNA adducts formed by aristolochic acid in renal tissue from patients with Chinese herbs nephropathy. Cancer Res. 1996;56:2025–8. [PubMed] [Google Scholar]
- 12.Ioset JR, Raoelison GE, Hostettmann K. Detection of aristolochic acid in Chinese phytomedicines and dietary supplements used as slimming regimens. Food ChemToxicol. 2003;41:29–36. doi: 10.1016/s0278-6915(02)00219-3. [DOI] [PubMed] [Google Scholar]
- 13.Tanaka A, Nishida R, Maeda K, Sugawara A, Kuwahara T. Chinese herb nephropathy in Japan presents adult-onset Fanconi's syndrome: Could different components of aristolochic acids cause a different type of Chinese herb nephropathy? ClinNephrol. 2000;53:301–6. [PubMed] [Google Scholar]
- 14.Nortier JL, Vanherweghem JL. Renal interstitial fibrosis and urothelial carcinoma associated with the use of a Chinese herb (Aristolochiafangchi) Toxicology. 2002;181-2:577–80. doi: 10.1016/s0300-483x(02)00486-9. [DOI] [PubMed] [Google Scholar]
- 15.Arlt VM, Pfohl-Leszkowicz A, Cosyns J, Schmeiser HH. Analyses of DNA adducts formed by ochratoxin A and aristolochic acid in patients with Chinese herbs nephropathy. Mutat Res. 2001;494:143–50. doi: 10.1016/s1383-5718(01)00188-7. [DOI] [PubMed] [Google Scholar]
- 16.Jorgensen K. Survey of pork, poultry, coffee, beer and pulses for ochratoxin A. Food AdditContam. 1998;15:550–4. doi: 10.1080/02652039809374680. [DOI] [PubMed] [Google Scholar]
- 17.Wei L, Chen B, Ye R, Li H. Treatment of complications due to peritoneal dialysis for chronic renal failure with traditional Chinese medicine. J Tradit Chin Med. 1999;19:3–9. [PubMed] [Google Scholar]
- 18.Zhang DN. Treatment of chronic renal failure with ‘serial recipes for renal failure’: A report of 64 cases. J Tradit Chin Med. 1989;9:159–62. [PubMed] [Google Scholar]
- 19.Foote J, Cohen B. Medicinal herb use and the renal patient. J Renal Nutr. 1998;8:40–2. doi: 10.1016/s1051-2276(98)90036-x. [DOI] [PubMed] [Google Scholar]
- 20.Jha V, Chugh KS. Nephropathy associated with animal, plant, and chemical toxins in the tropics. SemNephrol. 2003;23:49–65. doi: 10.1053/snep.2003.50003. [DOI] [PubMed] [Google Scholar]
- 21.Chou WC, Wu CC, Yang PC, Lee YT. Hypovolemic shock and mortality after ingestion of Tripterygiumwilfordii hook F: A case report. Int J Cardiol. 1995;49:173–7. doi: 10.1016/0167-5273(95)02282-2. [DOI] [PubMed] [Google Scholar]
- 22.Eswarappa S, Chakraborty AR, Palatty BU, Vasnaik M. Cleistanthuscollinuspoisoning: Case reports and review of the literature. J Toxicol ClinToxicol. 2003;41:369–72. doi: 10.1081/clt-120022005. [DOI] [PubMed] [Google Scholar]
- 23.Lin CC, Chen JC. Medicinal herb ErycibehenriPrain (‘Ting Kung Teng’) resulting in acute cholinergic syndrome. J ToxicolClinToxicol. 2002;40:185–7. doi: 10.1081/clt-120004409. [DOI] [PubMed] [Google Scholar]
- 24.Hsu HY, Lin CC, Chen JY, Yang JJ, Zhang R. Toxic effects of Erycibeobtusifolia, a Chinese medicinal herb, in mice. J Ethnopharmacol. 1998;62:101–5. doi: 10.1016/s0378-8741(98)00005-1. [DOI] [PubMed] [Google Scholar]
- 25.Akdogan M, Kilinc I, Oncu M, Karaoz E, Delibas N. Investigation of biochemical and histopathological effects of MenthapiperitaL. & MenthaspicataL on kidney tissue in rats. Hum ExpToxicol. 2003;22:213–9. doi: 10.1191/0960327103ht332oa. [DOI] [PubMed] [Google Scholar]
- 26.Bwititi P, Musabayane CT, Nhachi CF. Effects of Opuntiamegacanthaon blood glucose and kidney function in streptozotocin diabetic rats. J Ethnopharmacol. 2000;69:247–52. doi: 10.1016/s0378-8741(99)00123-3. [DOI] [PubMed] [Google Scholar]
- 27.Powell T, Hsu FF, Turk J, Hruska K. Ma-huang strikes again: Ephedrine nephrolithiasis. Am J Kidney Dis. 1998;32:153–9. doi: 10.1053/ajkd.1998.v32.pm9669437. [DOI] [PubMed] [Google Scholar]
- 28.Adesunloye BA. Acute renal failure due to the herbal remedy CKLS. Am J Med. 2003;115:506–7. doi: 10.1016/s0002-9343(03)00427-3. [DOI] [PubMed] [Google Scholar]
- 29.Wojcikowski K, Johnson D, Gobe G. Medicinal herbal extracts–renal friend or foe? Part one: The toxicities of medicinal herbs. Nephrology. 2004;9:313–8. doi: 10.1111/j.1440-1797.2004.00310.x. [DOI] [PubMed] [Google Scholar]
- 30.Moschella C, Jaber BL. Interaction between cyclosporine and Hypericumperforatum(St. John’swort) after organ transplantation. Am J Kidney Dis. 2001;38:1105–7. doi: 10.1053/ajkd.2001.28617. [DOI] [PubMed] [Google Scholar]
- 31.Gaston RS. Maintenance immunosuppression in the renal transplant recipient: An overview. Am J Kidney Dis. 2001;38(Suppl 6):S25–35. doi: 10.1053/ajkd.2001.28923. [DOI] [PubMed] [Google Scholar]
- 32.Bauer S, Stormer E, Johne A, Krüger H, Budde K, Neumayer HH, et al. Alterations in cyclosporin A pharmacokinetics and metabolism during treatment with St John's wort in renal transplant patients. Br J ClinPharmacol. 2003;55:203–11. doi: 10.1046/j.1365-2125.2003.01759.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Windrum P, Hull DR, Morris TC. Herb-drug interactions. Lancet. 2000;355:1019–20. doi: 10.1016/s0140-6736(05)74767-x. [DOI] [PubMed] [Google Scholar]
- 34.Thevenod F. Nephrotoxicity and the proximaltube: Insight from cadmium. Nephron Physiol. 2003;93:87–93. doi: 10.1159/000070241. [DOI] [PubMed] [Google Scholar]
- 35.Ernst E. Harmless herbs? A review of the recent literature. Am J Med. 1998;104:170–8. doi: 10.1016/s0002-9343(97)00397-5. [DOI] [PubMed] [Google Scholar]
- 36.Ko RJ. Adulterants in Asian patent medicines. N Engl J Med. 1998;339:847. doi: 10.1056/nejm199809173391214. [DOI] [PubMed] [Google Scholar]
- 37.Liu SY, Woo SO, Koh HL. HPLC and GC-MS screening of Chinese proprietary medicine for undeclared therapeutic substances. J Pharm Biomed Anal. 2001;24:983–92. doi: 10.1016/s0731-7085(00)00571-9. [DOI] [PubMed] [Google Scholar]
- 38.Ernst E, Coon JT. Heavy metals in traditional Chinese medicines: A systematic review. ClinPharmacolTher. 2001;70:497–505. doi: 10.1067/mcp.2001.120249. [DOI] [PubMed] [Google Scholar]
- 39.Howard H, Berger A. Alopecia and Sensory Polyneuropathy from thallium in a Chinese herbal medication. JAMA. 1992;268:3430–1. [PubMed] [Google Scholar]
- 40.Abt AB, Oh JY, Huntington RA, Burkhart KK. Chinese herbal medicine induced acute renal failure. Arch Intern Med. 1995;155:211–2. [PubMed] [Google Scholar]
- 41.Dwivedi SK, Dey S. Medicinal herbs: A potential source of toxic metal exposure for man and animals in India. Arch Environ Health. 2002;57:229–31. doi: 10.1080/00039890209602941. [DOI] [PubMed] [Google Scholar]
- 42.Mandal BK, Chowdhury TR, Samanta G, Mukherjee DP, Chanda CR, Saha KC, et al. Impact of safe water for drinking and cooking on five arsenic-affected families for 2 years in West Bengal, India. Sci Total Environ. 1998;218:185–201. doi: 10.1016/s0048-9697(98)00220-4. [DOI] [PubMed] [Google Scholar]
- 43.Saito T, Tsuboi Y, Fujisawa G, Sakuma N, Honda K, Okada K, et al. An autopsy case of licoriceinduced hypokalemic rhabdomyolysis associated with acute renal failure: Special reference to profound calcium deposition in skeletal and cardiac muscle. Nippon JinzoGakkai Shi. 1994;36:1308–14. [PubMed] [Google Scholar]
- 44.Ascherio A, Rimm EB, Hernan MA, Giovannucci EL, Kawachi I, Stampfer MJ, et al. Intake of potassium, magnesium, calcium, and fiber and risk of stroke among US men. Circulation. 1998;98:1198–204. doi: 10.1161/01.cir.98.12.1198. [DOI] [PubMed] [Google Scholar]
- 45.Subat-Dezulovic M, Slavic I, Rozmanic V, Persic M, Medjimurec B, Scukanec-Spoljar M. Drug-induced acute tubulointerstitial nephritis: A case with elevated urinary cadmium. PediatrNephrol. 2002;17:382–5. doi: 10.1007/s00467-002-0839-9. [DOI] [PubMed] [Google Scholar]
- 46.Ige SF, Salawu EO, Olaleye SB, Badmus J, Adeleke AA. Onion (Allium cepa) extract preventcadmium induced renal dysfunction. Indian J Nephrol. 2009;19:140–4. doi: 10.4103/0971-4065.59334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kwok TC, Chan TY, Woo J. Relationship of urinary sodium/potassium excretion and calcium intake to blood pressure and prevalence of hypertension among older Chinese vegetarians. Eur J ClinNutr. 2003;57:299–304. doi: 10.1038/sj.ejcn.1601553. [DOI] [PubMed] [Google Scholar]


