Abstract
Background:
Melasma, a common disorder of hyperpigmentation, is often difficult to treat. Although 10% zinc sulfate solution has been reported to be useful for patients with melasma, controlled trials are lacking.
Materials and Methods:
72 women with moderate to severe melasma were divided randomly into 2 groups. Group A were treated with 10% zinc sulfate solution and group B with 4% hydroquinone cream twice-daily. The results were evaluated by photoevaluation by patients based on subjective satisfaction and a blinded dermatologist using MASI score. Assessments were obtained at baseline and at 2 and 6 months after starting treatment.
Results:
According to MASI score changes during treatment, there was a reduction in both groups at 2 months, however, the reduction in group B was more significant (the reduction in mean ± SD MASI was 0.7 ± 0.7 in group A vs. 2.7 ± 1.6 in group B). In addition, the patients in group B continued to decrease MASI score for the remainder of the study period at 6 months follow-up (0.3 ± 0.5) in comparison with patients in group A who did not show more reduction in MASI score.
Conclusions:
The study indicates that topical zinc sulfate is not as effective in treating disease as was observed in the previous open study. A comparative study with sunscreen and placebo is necessary to determine if topical zinc sulfate is truly superior to sunscreen and placebo in this respect.
Keywords: Hydroquinone, melasma, zinc sulfate
INTRODUCTION
Melasma is a disorder of pigmentation, commonly affecting sun-exposed areas of skin, the forehead, malar, and mandibular regions of face.[1] It presents as symmetric, hyperpigmented patches with an irregular demarcated border on the face.[1,2]
Although it is common in both sexes, the majority of patients, about 90%, are women of Asia and Latin America origin.[1,2]
Despite the fact that the exact origin of melasma is unknown, exposure to UV irradiation and genetic factors are the main proposed causes. In addition pregnancy, hormonal therapy (oral contraceptives or hormone replacement therapy), subclinical ovarian dysfunction, phenytoin, phototoxic drugs, and thyroid dysfunction are the other causes. The color of melasma lesion typically diminishes during winter months and aggravates in the summer.[2,3]
Melasma following pregnancy usually improves within a few months of delivery. However, it rarely clears after discontinuing of oral contraceptives.[2–4]
Before providing an effective treatment, it is thoroughly recommended to consider wood's light for distinguishing between increased melanin within the epidermis vs. an increase in the dermis on the presence or absence of light enhancement, respectively.[4] While epidermal pigmentation is somewhat more amenable to topical therapies and chemical peels, dermal pigmentation is appallingly difficult to treat.[4,5] Despite that, most cases show both epidermal and dermal melanin, and dermal melanophages are a common feature among Asian sun-exposed patients.[4] Separate from Wood's light study, a pragmatic therapeutic approach of hypopigmenting agents should be recommended if the patient demands it.[2–4]
As mentioned above, treatment of melasma can be very frustrating. Standard treatments include sun avoidance and sunscreens, hypopigmenting agents, chemical peels, lasers and dermabrasion.[1–5] Hypopigmenting agents are momentous in the treatment of melasma.[2–4,6,7] These agents not only act as tyrosinase inhibitors, but also scatter the melanin throughout the skin.[6–9] Hydroquinone, one of the most renowned topical treatments, displays its action through both the inhibition of tyrosinase and exclusive detriment to melanosomes and melanocytes.[6,7,9] Prescribing 2% to 4% hydroquinone is the approved treatment, while 4% hydroquinone is the gold criterion for melasma therapy. Hydroquinone can be used alone or in combination with a topical retinoid and corticosteroid (kligman formula). Although highly effective in the treatment of melasma, some adverse effects due to hydroquinone therapy include irritant and allergic contact dermatitis, post-inflammatory hyperpigmentation, and hypopigmentation of the surrounding skin.[6–10] Ochronosis is the rare side effect seen with prolonged use of concentration > 2%.[10]
Zinc is a main trace element and important nutrient, which exists in all organs, tissues and in fluids of the body. At the cellular level, zinc acts as vital component of both enzymes and cofactors.[11] The effect of zinc acquired through its action as anti-inflammatory, anti-oxidant, cytotoxic, and healing agent.[11,12] Zinc sulfate was found to be effective in treatment of many dermatological disorders, such as cutaneous leishmaniasis, recurrent herpes simplex, common and genital warts and recently melasma.[1,12,14,15] In fact, there is only one study that has been conducted on the efficacy of topical zinc sulfate for the treatment of melasma.[14,15] This study is the first, to our knowledge, to measure quantitatively the difference between the efficacy of conventional treatment with hydroquinone and the newly proposed agent, topical zinc sulfate solution in the treatment of melasma.
MATERIALS AND METHODS
This study was conducted at the outpatient department of Dermatology, Isfahan, Azahra Teaching Hospital. In this investigator-blinded, randomized, control trial study 72 subjects (aged 21 - 42 years) presenting with moderate to severe melasma were enrolled in the study between March 2010 and September 2011. This study was initially approved by the ethical committee of Isfahan University of Medical Science. The Research Project Number was 290113. Written informed consent was obtained from all participants before enrollment.
The diagnosis was established on the basis of clinical findings. A detailed history was taken from each patient concerning the involved or deteriorating factors (sun exposure, pregnancy and contraceptive pills or other causative drug consumption).
Inclusion criteria included women with moderate to severe facial melasma based on Wood's light examination. All patients had epidermal or mixed melasma based on Wood's light examination at time of screening. Patients with pregnancy, breast feeding, any medical treatment for melasma within 3 months of entry, and skin resurfacing by dermabrasion, chemical peels, or facial laser within the preceding 9 months were excluded from the study.
As mentioned in the guidelines for clinical trials in melasma,[16] a blinded dermatologist quantified the Melasma Area and Severity Index (MASI) from the photographs. MASI scores are used for clinical research studies of melasma and are not commonly used in the daily management of patients in the clinical setting. According to this method, the face in 4 areas of forehead, right and left malar, and chin is assessed on the basis of percentage of the total area involvement, darkness, and homogeneity. The MASI equation is given below:
MASI = 0.3 F (D + H)A + 0.3 RM (D + H) A + 0.3 LM (D + H) A + 0.1 C (D + H) A,
Where F is forehead, MR is right malar, ML is left malar, C is chin, and the values 0.3, 0.3, 0.3, and 0.1 stands for respective percentages of the total facial area. It ranges from 0 to 48.
Photographs taken with a digital camera (Canon Power Shot G12, Canon Components Inc, Japan) before treatment and during follow-up were used.
In order to perform patient satisfaction surveys, assessment of the treatment areas using comparative photographs were conducted by patient-based satisfaction, 2 and 6 months after starting of treatment (Patient Global Assessment [PGA]). The improvement of melasma was scored from 0 to 10 on a visual analog scale from (0 as no improvement and 10 as the best possible improvement).
The patients were divided into 2 different treatment groups, using a table of random numbers. 36 patients were enrolled in each group. The patients in group A received 10% zinc sulfate solution, and the patients in group B received 4% hydroquinone cream twice-daily. 10% zinc sulfate solution was prepared by dissolving 10 g of zinc sulfate crystals in 100 ml of distilled water. All patients of 2 groups have been received sunscreen cream (ARDEN, SPF: 30 or more) to control the doubts regarding the anti-solar effect of zinc sulfate and to prevent direct sun exposure during study.
The statistical analysis was done by SPSS for windows software (SPSS Inc., Chicago, IL, USA, version 18.0) by using repeated measures ANOVA,Chi-Square and independent t-test analysis. The significance level was set at P value of less than 0.05.
RESULTS
72 subjects (100%) with moderate to severe melasma were enrolled in the study to evaluate the difference between the therapeutic efficacy and safety of 4% hydroquinone and 10% zinc sulfate solution.
17 patients failed to complete the study, 5 subjects did not use the drugs according to the rules, and 12 subjects did not complete the study because they were unable to come in for visits due to scheduling difficulties. 8 of them were in group A, and 9 of them were in group B. None of them gave up the study due to the side effects. 55 completed the 2 and 6 months follow-up with no protocol deviation. The age of patients ranged from 21 to 42 years; the mean age of patients was 30.9 ± 4.9 years in group A and 31.7 ± 4.4 years in group B.
The independent t-test disclosed no statistically significant difference between the ages of two groups (P-value = 0.47).
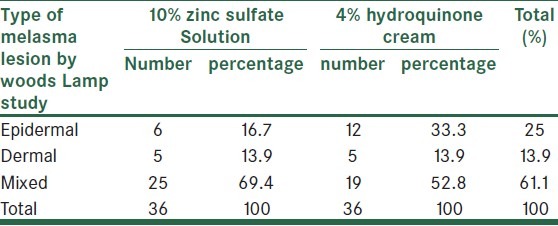
We used Chi-Square test to evaluate differences between the type of melasma lesion between 2 groups (P-value = 0.24), but there was no statistically significant difference between them [Table 1].
Table 1.
Patient characteristic of zinc sulfate and hydroquinone group
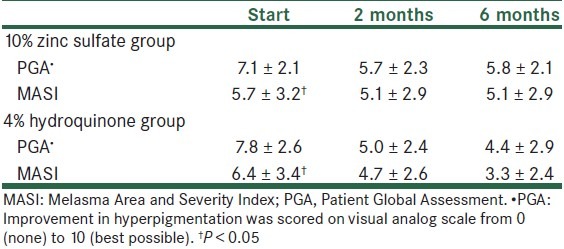
The patients reported a continuing clinical improvement at the 2 months follow-up in both groups. (P-value = 0.001).
In addition, there was a steady improvement in patients of group B in comparison with group A after 6th month of starting treatment (PGA).
The mean MASI score before treatment was not statistically different between the 2 groups (P-value = 0.434), but after 2 months, (P-value = 0.03) and 6 months (P-value = 0.006) of starting treatment, the MASI was obviously less in patients of group B in comparison with patients of group A.
Repeated Measure ANOVA test revealed that the mean MASI scores in both groups were not the same in the first 2 stages of study (P-value < 0.001). Furthermore, by means of this method, it is brought to light that the mean MASI scores in group A, 2 and 6 months after treatment, were lower than baseline (P-value < 0.001), but the results between 2nd and 6th months of follow-up were identical (P-value = 1) [Figure 1].
Figure 1.
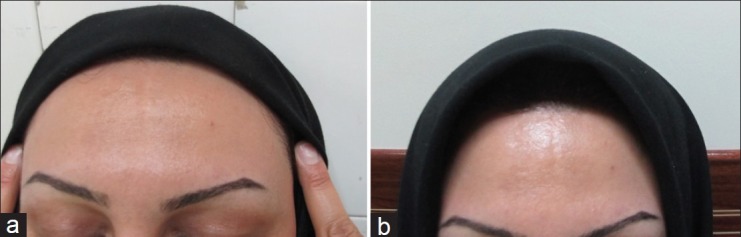
(a) A 34-year-old woman who comes due to melasma since 3 years ago.a.Before treatment. (b) After 8 weaks of tratment with 10 % zinc sulfate, there is not remarkable change in the colour of the lesion
In contrast, in group B, both the comparison between the baseline and 2nd and 6th monthsof follow-up (p-value < 0.001) and the comparison between 2nd and 6th months (P-value = 0.001) were unlike. Indeed, a continuous reduction in MASI score in group B was obvious [Table 2].
Table 2.
Melasma parameters of zinc sulfate and hydroquinone group
Although there was some reports of mild burning and erythema during treatment, no significant adverse effect has been notified in both groups.
DISCUSSION
Melasma, a common disorder of Latin American and Asian women, occurs because of unknown causes. However, genetic factors, UV irradiation, pregnancy, hormonal therapy, ovarian dysfunction, and using some drugs are the proposed factors.[1–3]
Since melasma is a prevalent, abiding, unruly, very distressing pigmentory disorder, the interest to find new modalities of treatment, which are cheap, safe, and readily-available, are non-stopping.
The conventional practices such as hypopigmenting agents, chemical peels, lasers and dermabrasion remains the benchmark that the new proposed modalities are compared with them. Among the common agents, hydroquinone products, alone or in combination with other depigmenting agents are widely used agents.[2–5] In fact, hydroquinone acts through not only the inhibition of tyrosinse enzyme, a main enzyme in the production of melanin, also by destroying the melanosomes.[6–9]
Recently, 10% zinc sulfate solution has been proposed as an alternative therapy for melasma.[14,15] It has been suggested that zinc elements play role by anti-inflammatory, anti-oxidant, and healing effect.[11] In the present study, to our knowledge, we provide the first clinical evidence that compares quantitatively the effectiveness of topical 10% zinc sulfate and 4% hydroquinone cream in the treatment of melasma. This study makes a comparison between the patients in group A (patients receiving 10% zinc sulfate solution) and in group B (patients receiving 4% hydroquinone cream).
For overcoming wide variability subjective assessment, a detailed comparison by using scoring indices such as MASI score helps to quantify the evaluation of melasma. The MASI score was produced to quantify the 3 key portions observed when examining a patient with melasma: Darkness of the pigmentation, homogeneity, and the area of involvement.
In our study, using MASI score indicates a reduction in both groups after 2 months of treatment. However, this reduction was significantly more in patients of group B than in group A (3.7 ± 2.6 in group A vs. 5.1 ± 2.9 in group B). The baseline of MASI score in group A and B were 5.7 ± 3.2 and 6.4 ± 3.4, respectively.
In the only previous study by Sharquie et al., it has been suggested that topical 10% solution was a new effective and safe formulation in the treatment of melasma. They evaluated the efficacy and safety of 10% zinc sulfate solution in 14 patients. Degree of improvement was graded using MASI score. The MASI score before treatment was 9.45, which changed to 4.70 after therapy. This corresponds to a percentage improvement of 49.78% and was statistically significant (P < .0005), and most of them maintained an improvement 3 months after cessation of therapy. The only reported side effect was mild stinging sensation in few patients.
The MASI in the present study continued to decrease in group B at the 6 months follow-up (compared with the baseline, P = 0.006 and 0.403, respectively). In comparison, the MASI did not indicate no difference between the 2-and 6 months follow-up in group A.
For increasing the confidence of findings and better understanding of the different dimensions of the disease, patient-reported outcomes (PGA), as an added parameter, entered in the present study. The results of MASI score changes supported by PGA.
According to mounting evidences of this study, the 10% zinc sulfate is not as effective as 4% hydroquinone cream in the treatment of melasma. Indeed, the mean improvement rate in patients of group B at 2 and 6 months was 42.2% and 48.8%, respectively while the improvement rate in group A was 10.5% at 2 months follow-up without any change at 6 months.
The conjectural hypothesis about the mechanisms of action of topical zinc sulfate are peeling, anti-oxidant, and sunscreen effects. Sharqui stated that zinc sulfate solution is significantly effective in the treatment of melasma, and this evidence is more attributable to its peeling effect. However, according to findings of this study , through the mechanisms of action of topical zinc sulfate, we assume the impression of zinc sulfate is only through sunscreen effect. As melasma is presumed a photodermatosis, sun protection is of value in both treatment and prevention.
Leenutaphong et al. showed a reduction of 60% in MASI score in patients receiving only sunscreen.[17]
In summary, although the previous study of Sharqui regarding treatment of melasma by topical zinc sulfate makes sense, thus far, the juxtaposition of topical zinc sulfate and hydroquinone in this study showed that the effect of topical zinc sulfate is only attributable to sunscreen effect and quantitatively was not significant.
In future studies, a comparison between other physical and chemical sunscreen and topical zinc sulfate in the treatment of melasma should be recruited to better compare treatment outcomes. In addition, clarification the exact mechanism of action of zinc component in cellular biology is an issue that helps us for designing more accurate models of study.
ACKNOWLEDGMENT
We thank all the patients who participated in this study and the staff dermatology department of the Alzahra hospital.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Pawaskar MD, Parikh P, Markowski T, McMichael AJ, Feldman SR, Balkrishnan R. Melasma and its impact on health-related Quality of life in Hispanic women. J Dermatolog Treat. 2007;18:5–9. doi: 10.1080/09546630601028778. [DOI] [PubMed] [Google Scholar]
- 2.Grimes PE. Melasma: Etiologic and therapeutic considerations. Arch Dermatol. 1995;131:1453–7. doi: 10.1001/archderm.131.12.1453. [DOI] [PubMed] [Google Scholar]
- 3.Grimes PE. Management of hyperpigmentation in darker racial ethnic groups. Semin Cutan Med Surg. 2009;28:77–85. doi: 10.1016/j.sder.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 4.Gupta AK, Gover MD, Nouri K, Taylor S. Treatment of melasma: A review of clinical trials. J Am Acad Dermatol. 2006;55:1048–65. doi: 10.1016/j.jaad.2006.02.009. [DOI] [PubMed] [Google Scholar]
- 5.Bukvić Mokos Z, LipozenČić J, Ceović R, Stulhofer Buzina D, Kostović K. Laser therapy of pigmented lesions: pro and contra. Acta Dermatovenerol Croat. 2010;18:185–9. [PubMed] [Google Scholar]
- 6.Kligman AM, Willis I. A new formula for depigmenting human skin. Arch Dermatol. 1975;111:40–8. [PubMed] [Google Scholar]
- 7.Taylor SC, Torok H, Jones T, Lowe N, Rich P, Tschen E, et al. Efficacy and safety of a new triple-combination agent for the treatment of facial melasma. Cutis. 2003;72:67–72. [PubMed] [Google Scholar]
- 8.Rendon M, Berneburg M, Arellano I, Picardo M. Treatment of melasma. J Am Acad Dermatol. 2006;54(Suppl):S272–81. doi: 10.1016/j.jaad.2005.12.039. [DOI] [PubMed] [Google Scholar]
- 9.Ennes SBP, Paschoalick RC. Mota de Avelar Alchorne M.A double-blind, comparative, placebo-controlled study of the efficacy and tolerability of 4% hydroquinone as a depigmenting agent in melasma. J Dermatolog Treat. 2000;11:173–9. [Google Scholar]
- 10.Palumbo A, d’ischia M, Misuraca G, Prota G. Mechanism of inhibition of melanogenesis by hydroquinone. Biochim Biophys Acta. 1991;1073:85–90. doi: 10.1016/0304-4165(91)90186-k. [DOI] [PubMed] [Google Scholar]
- 11.Rostan EF, DeBuys HV, Madey DL, Pinnell SR. Evidence supporting zinc as an important antioxidant for skin. Int J Dermatol. 2002;41:606–11. doi: 10.1046/j.1365-4362.2002.01567.x. [DOI] [PubMed] [Google Scholar]
- 12.Iraji F, Faghihi G. A randomized double-blind placebo controlled clinical trial of two strengths of topical zinc sulphate solution against recurrent herpes simplex. Arch Iran Med. 2003;6:13–5. [Google Scholar]
- 13.Shrquie KE, Khoesheed AA, Al-nuaimy AA. Topical zinc sulphate solution for treatment of viral wart. Saudi Med J. 2007;28:1418–21. [PubMed] [Google Scholar]
- 14.Shrquie KE, Al-Mashhadani SA, Salman HA. Topical 10% zinc sulfate solution for treatment of melasma. Dermatol Surg. 2008;34:1346–9. doi: 10.1111/j.1524-4725.2008.34287.x. [DOI] [PubMed] [Google Scholar]
- 15.Miot HA, Miot LD. Re:Topical 10%zinc sulfate solution for treatment of melasma. Dermatol Surg. 2009:352050–1. doi: 10.1111/j.1524-4725.2009.01333.x. [DOI] [PubMed] [Google Scholar]
- 16.Pandya A, Berneburg M, Ortonne JP, Picardo M. Guidelines for clinical trials in melasma: Pigmentation Disorders Academy. Br J Dermatol. 2006;156(Suppl):S21–8. doi: 10.1111/j.1365-2133.2006.07590.x. [DOI] [PubMed] [Google Scholar]
- 17.Leenutaphong V, Nettakul A, Rattanasuwon P. Topical isotretinoin for melasma in Thai patients a vehicle-controlled clinical trial. J Med Assoc Thai. 1999;82:867–75. [PubMed] [Google Scholar]


