Abstract
Background:
C-reactive protein (CRP) is useful as marker of severity in malaria. African studies have shown that serum CRP levels correlate with parasite burden and complications in malaria, especially falciparum. However, there are very few data on CRP levels in Indian malaria patients.
Materials and Methods:
We assessed CRP levels in malaria patients at presentation and studied for any relation of CRP levels with subsequent prognosis. Statistical tests included student's t-test, Mann Whitney U test, and chi square test, all with 2-tailed analyzes.
Results:
Of 71 patients in our study, 42 (59.1%) were infected with P. falciparum. 23 (32.4%) patients needed admission and 10 (14.1%) died. Average CRP levels were quite high in malaria patients (31.29 ± 20.4 mg/L). There was no significant difference in CRP between vivax and falciparum cases. Admitted patients had significantly higher CRP levels compared to those treated on outdoor basis (47.11 ± 19.13 vs. 23.71 ± 16.35 mg/L; P < 0.0001). 8 patients were admitted with multiple complications. They had significantly high CRP level compared to those with 1 complication (P = 0.015). Also, patients who died had higher CRP levels compared to survivors (P = 0.000346). CRP levels at presentation showed positive correlation with duration of hospital stay (r = 0.59; P < 0.05). CRP levels >35 mg/L was highly sensitive in predicting mortality.
Conclusion:
Our study in Indian population corroborates the findings in African studies regarding prognostic role of CRP in malaria. CRP is an effective biomarker in assessing malaria severity and also for follow-up.
Keywords: Biomarker, C-reactive protein, prognosis, falciparum malaria, mortality
INTRODUCTION
Malaria causes high mortality and morbidity in various tropical regions.[1] The indirect burden of malaria like malnutrition and anemia are also highly prevalent in these populations of endemic zones.[1] Thus, measures to identify severity of this disease are needed so as to institute timely therapy and avoid the complications.
Blood tests like total leukocyte count, liver function test, and blood glucose have been used for long to assess the malaria complications. But, these tests are not always sensitive in estimating disease severity. Thus, newer indicators, especially those related to the immune activation pathways in malaria are needed. A very recent study from Uganda has tested some of these inflammatory markers.[2] However, the tests done in this study were too costly and were time consuming. Similarly, a study showed serum angiopoietin as a marker of severity in malaria.[3] But, in endemic regions with a high caseload like India, such complicated and costly methods will not help in daily practice.
Now, C-reactive protein (CRP) is being studied as a biomarker in malaria patients.[4] It is especially important in highly endemic regions where conventional disease manifestations like fever may be absent even in patients with high parasite load.[4] In a study from Tanzania, CRP levels were found to correlate strongly with parasite density in blood of patients, whether they had clinical features or not.[4] Not only that, another study from Gambia found CRP levels helpful in study of malaria in a Community also.[5] This study used CRP levels as surrogate marker for malaria infection and complications. Hurt et al. in a Tanzanian study found that levels of CRP in malarial children correlated with morbidity, especially in falciparum-infected cases.[6]
CRP is an acute phase reactant. But, in malaria, it is said to have a pathogenic role as well. CRP is said to bind to infected erythrocytes and help in their clearance.[7] This immune activation towards infected RBCs also results in various deleterious manifestations.[7] Also, CRP activates complement pathway and platelet activation, and results in various untoward effects.[8] Thus, measurement of CRP can be useful in understanding the pathogenesis of severe malaria.
However, studies regarding CRP in malaria are very rare from India. Various regions of this country are hyper endemic for malaria with a high rate of mortality.[9] But, role of CRP in Indian population and whether the results of aforementioned African studies can be applied to this population is largely unknown.
Aim and Objective
We undertook this study to find the relation of CRP levels with prognosis in Malaria. Our study population was from a highly endemic region of India.[9]
Specific objectives included studying the CRP levels in different subsets of malaria patients, like those with one complication vs. those with multiple complications. We studied for any statistical difference in CRP levels in these subsets; also, analysis was done by ROC for sensitivity, specificity, and the predictive value of CRP in malaria mortality or morbidity.
MATERIALS AND METHODS
We selected patients coming to OPD of Department of Medicine, Medical College Kolkata between 1st May 2010 and 31st December 2010. Patients diagnosed with malaria by slide microscopy or rapid antigen assay were included [Figure 1]. All the patients were from Kolkata and in all, malaria infection was the only diagnosis. Clinical assessment was done including higher mental function assessment, and initial blood tests like complete hemogram, liver function test, urea/creatinine and blood glucose were done in all patients, OPD or indoors, to look for complications. Patients with any complication like jaundice, anemia, renal failure, or altered consciousness were admitted. CRP was measured at first presentation only, and the patients were followed up with full appropriate therapy. CRP was measured by immunoturbidimetic method (BS 400/HITACHI 902) with normal value ≤5 mg/L. An ethical clearance of the institution was obtained, and individual patient/next of kin consent was also taken. We only included patients above 14 years. Patients with other diseases that can alter CRP, like malignancy or rheumatological disorders and also patients on steroids or other immunosuppressants were excluded.
Figure 1.

Recruitment of the patients in our study
The data was arranged in Microsoft (Redmond, USA) Excel worksheet and analyzed using MedCalc, GraphPad (GraphPad Software, San Diego California USA) and epiInfo (ver. 3.5.1) statistical software (free). Continuous variables like CRP are expressed as mean ± S.D. Discreet variables are expressed as numbers/percentages. To compare discreet variables, 2*2 contingency tables are analyzed using Chi-Square test/Fisher's exact test as appropriate. To compare continuous variables, students’ T-test for independent samples was used. Also, in some cases where the number was small, non-parametric comparison tests like Mann Whitney U test was used. Correlation between variables is assessed by Pearson correlation coefficient. 2-tailed analyzes are used with 95% confidence interval. P value < 0.05 was considered significant.
RESULTS
In this study, we included a total of 71 patients [Figure 1]. Male female ratio was 51:20 [Table 1]. Of them, 42 were Plasmodium falciparum (Pf) and the rest 29 were vivax-infected [Table 1]. We got no patient with dual infection in our study. Of all 71 patients, 23 (32.4%) needed admission for various reasons. Of the admitted patients, 10 (43.5% of admitted patients) died from reasons attributable to malaria. It is seen from Table 1 that most of the admissions and deaths were due to P. falciparum. Altogether, 21 (50%) of the Pf patients needed admission, and 9 (21.4%) of Pf-infected patients died. For vivax, 6.9 % (n = 2) patients needed admission, and 1 died due to severe hematological disease. Thus for Pv, mortality was 3.4%. Mortality was thus significantly more for Pf cases (9 vs. 1; P = 0.04 by Fisher's exact Test). Also, admission rate was more for Pf cases (P = 0.0001 by Fisher's Test).
Table 1.
Profile of our patients according to the infecting species of malaria
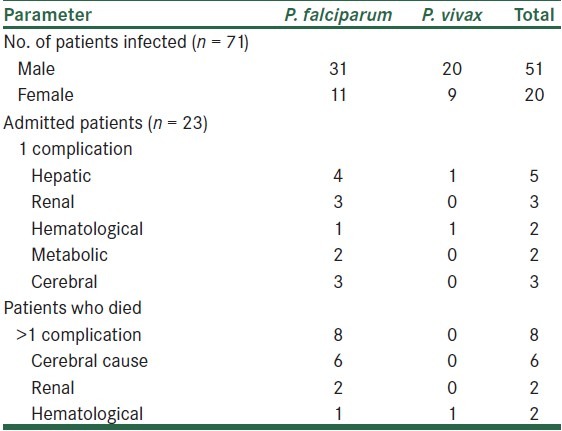
Table 2 shows the CRP levels in various patients. Average CRP was quite high (31.29 ± 20.4 mg/L). However, there was no significant difference between Pf and Pv cases [P = 0.08; Table 2]. Patients who ultimately needed an admission had significantly higher CRP levels compared to patients treated on OPD basis (P < 0.0001 by t-test). The patients who died (n = 10) had CRP levels significantly higher than survivors (P = 0.000346 by Mann Whitney U Test; z = 3.388). CRP levels showed strong correlation with duration of hospital stay (r = 0.59; P < 0.0001) [Figure 2]. The number of individual complications was very small for statistical analysis. However, admitted patients with multiple complications (n = 8) had significantly higher CRP level compared to patients with single complication (n = 14) (P = 0.015 by Mann Whitney U Test; U = 97). Average CRP levels in individual complications were not much different statistically. The commonest cause of death (n = 6; 60%) in our study was cerebral malaria.
Table 2.
CRP levels in our patients

Figure 2.
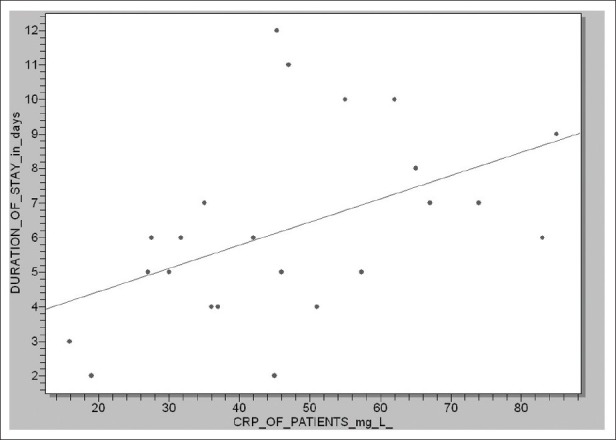
Correlation of initial CRP levels with duration of hospital stay
ROC analysis shows CRP level >31 mg/L has 92% sensitivity and 76% specificity to predict hospital stay >5 days (AUC = 0.893) [Figure 3]. Also, CRP > 35 mg/L has high sensitivity (>95%) in predicting mortality (P < 0.0001) [Figure 4]. Specificity was around 73% (AUC = 0.836).
Figure 3.

ROC for different CRP values in hospital stay >5 days
Figure 4.

ROC for mortality in malaria in different CRP values
DISCUSSION
In this observational prospective study, we found significantly high CRP levels in malaria patients. CRP levels were higher for patients who needed an admission and also patients who died, compared to others. Also, CRP levels were higher in patients with multiple complications, compared to single complication. High CRP also predicted prolonged hospital stay. CRP levels >35 mg/L were predictive of mortality with a high degree of sensitivity in ROC analysis.
CRP is known as a marker of morbidity and mortality in malaria.[6] This acute phase reactant level correlates closely with other complications in malaria and can be used to predict severity.[6] A study from Assam, India also came to the same conclusion.[10] They also found that patients with high CRP had protracted course of illness.[10] In our study, we found significantly high CRP levels in patients who died as a result of malaria [Table 2]. In this study, we have measured CRP only once, at first contact. However, serial CRP measurements in malaria patients can be even better at assessment of course of the disease.[11] In a study from London, they have shown that daily CRP levels in malaria patients correlated closely with clinical condition.[11] They also found a relation of CRP with recorded daily body temperature in these patients.[11] In our study, daily CRP could not be done due to cost factor.
We found CRP levels high in patients with multiple complications. Actually, in malaria, immune activation plays a very important role in pathogenesis.[7,12] This is the basis for a cascade of reactions that culminates in multiple organ failures. Other factors like serum amyloid P, TNF, and interleukins are also important in this regard, and their levels also correlate with disease activity.[11,12] However, these are difficult to measure and are not cost-effective in clinical practice. Another important marker in this regard is serum ferritin.[13] A study from Cote d’ Ivoire found that CRP levels correlate with disease burden, especially at high parasite density.[14]
A study from Cameroon has clearly shown that CRP levels rise in complicated malaria, compared to uncomplicated.[8] In that study, 87% of the subjects with cerebral malaria had high CRP[8] Most of the studies in malaria are done with only falciparum. However, in our study, the CRP levels in vivax and Pf groups were comparable [Table 1]. This acute phase reaction in vivax malaria has been recently elucidated in a study from Brazilian Amazon area.[12] Another study from Australia including 69% vivax cases found elevated CRP levels in 85% cases.[15] However, although the CRP levels were high in our vivax patients, hospital admission rates and mortality were significantly less compared to Pf cases. Falciparum cases are known to be more prone to complications and death, although vivax cases in south East Asia are also becoming virulent with an increasing drug resistance.[16]
In ROC analysis, we found that certain levels of CRP were sensitive enough to predict prolonged hospital stay and death from malaria [Figures 3 and 4]. This is in accordance with the observation that CRP levels directly track with the parasite burden in blood of patients.[6] In the study from Cameroon, the CRP levels recorded for complicated malaria were higher than ours, but the actual measurements depend on method used and the immunity of the population.[8]
CONCLUSION
In this prospective study, we found that CRP levels at presentation correlate significantly with morbidity and mortality in malaria. However, a larger study, involving more inflammatory biomarkers and including serial measurement of these parameters would better clarify their role, either singly or in combination, in severe malaria. CRP can be considered a new, cost-effective, and reliable tool in assessment of prognosis in malaria.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Rowe AK, Rowe SY, Snow RW, Korenromp EL, Schellenberg JR, Stein C, et al. The burden of malaria mortality among African children in the year 2000. Int J Epidemiol. 2006;35:691–704. doi: 10.1093/ije/dyl027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Erdman LK, Dhabangi A, Musoke C, Conroy AL, Hawkes M, Higgins S, et al. Combinations of host biomarkers predict mortality among Ugandan children with severe malaria: A retrospective case-control study. PLoS One. 2011;6:e17440. doi: 10.1371/journal.pone.0017440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Conroy AL, Lafferty EI, Lovegrove FE, Krudsood S, Tangpukdee N, Liles WC, et al. Whole blood angiopoietin-1 and -2 levels discriminate cerebral and severe (non-cerebral) malaria from uncomplicated malaria. Malar J. 2009;8:295. doi: 10.1186/1475-2875-8-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hurt N, Smith T, Tanner M, Mwankusye S, Bordmann G, Weiss NA, et al. Evaluation of C-reactive protein and haptoglobin as malaria episode markers in an area of high transmission in Africa. Trans R Soc Trop Med Hyg. 1994;88:182–6. doi: 10.1016/0035-9203(94)90287-9. [DOI] [PubMed] [Google Scholar]
- 5.McGuire W, D’Alessandro U, Olaleye BO, Thomson MC, Langerock P, Greenwood BM, et al. C-reactive protein and haptoglobin in the evaluation of a community-based malaria control programme. Trans R Soc Trop Med Hyg. 1996;90:10–4. doi: 10.1016/s0035-9203(96)90461-7. [DOI] [PubMed] [Google Scholar]
- 6.Hurt N, Smith T, Teuscher T, Tanner M. Do high levels of C-reactive protein in Tanzanian children indicate malaria morbidity. Clin Diagn Lab Immunol. 1994;1:437–44. doi: 10.1128/cdli.1.4.437-444.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ansar W, Bandyopadhyay SM, Chowdhury S, Habib SH, Mandal C. Role of C-reactive protein in complement-mediated hemolysis in malaria. Glycoconj J. 2006;23:233–40. doi: 10.1007/s10719-006-7928-0. [DOI] [PubMed] [Google Scholar]
- 8.Dongho Dongmo FF, Ngono Ngane RA, Gouado I, Pankoui Mfonkeu JB, Mbackop Kwemba V, Ngwa V, et al. Predictors of childhood severe malaria in a densely populated area: Douala, Cameroon. African Journal of Biotechnology. 2011;10:6319–24. [Google Scholar]
- 9.Bhattacharya S, Sharma C, Dhiman RC, Mitra AP. Climate change and malaria in India. Curr Sci. 2006;90:369–75. [Google Scholar]
- 10.Banik S, Adhikary AK. CRP Level as a prognostic indicator of morbidity and mortality in malaria. [Internet] [cited 2011 sept 2];JAPI. 2009 Available from: http://www.japi.org/march_2009/tropical_medicine_poster_sessions.html . [Google Scholar]
- 11.Gillespie SH, Dow C, Raynes JG, Behrens RH, Chiodini PL, McAdam KP. Measurement of acute phase proteins for assessing severity of Plasmodium falciparum malaria. J Clin Pathol. 1991;44:228–31. doi: 10.1136/jcp.44.3.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andrade BB, Reis-Filho A, Souza-Neto SM, Clarêncio J, Camargo LM, Barral A, et al. Severe Plasmodium vivax malaria exhibits marked inflammatory imbalance. Malar J. 2010;9:13. doi: 10.1186/1475-2875-9-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O’Donnell A, Fowkes FJ, Allen SJ, Imrie H, Alpers MP, Weatherall DJ, et al. The acute phase response in children with mild and severe malaria in Papua New Guinea. Trans R Soc Trop Med Hyg. 2009;103:679–86. doi: 10.1016/j.trstmh.2009.03.023. [DOI] [PubMed] [Google Scholar]
- 14.Felix Yh, Hugues A, David K, Adou Y, Brice BK, Dagui M, et al. Assessment of inflammatory and immunity proteins during falciparum malaria infection in children of Côte d’Ivoire. Am J Sci Ind Res. 2010;1:233–7. [Google Scholar]
- 15.Robinson P, Jenney AW, Tachado M, Yung A, Manitta J, Taylor K, et al. Imported malaria treated in Melbourne, Australia: Epidemiology and clinical features in 246 patients. J Travel Med. 2001;8:76–81. doi: 10.2310/7060.2001.24309. [DOI] [PubMed] [Google Scholar]
- 16.Malaria: Disease Burden in SEA Region [internet] [Updated 2011 Jan 18; Cited 2011 Sept 6];WHO publication. 2011 WHO Regional Office for South-East Asia; [about 2 screens]. Available online at http://www.searo.who.int/en/Section10/Section21/Section340_4018.htm . [Google Scholar]


