Abstract
Background:
Light-emitting diodes (LEDs) are light sources recently used for phototherapy in neonatal jaundice. We compared the efficacy and safety of LEDs with fluorescent phototherapy in the treatment of indirect hyperbilirubinemia.
Materials and Methods:
This controlled trial was conducted on preterm infants hospitalized in neonatal intensive care unit of Shahid Beheshti Hospital in Isfahan (Iran) who needed conventional phototherapy for uncomplicated indirect hyperbilirubinemia. Neonates received phototherapy through devices with LEDs or special blue fluorescent tubes. Primary outcomes included the rate of fall of total serum bilirubin (TSB, mg/dL/hour) and duration of phototherapy (hours). Secondary outcomes were treatment failure and side effects.
Results:
A total of 64 infants with gestational age of 33.5 ± 1.2 weeks, chronological age of 73.0 [SE = 7.3] hours, and weight of 1757.5 ± 147.6 gram were enrolled. The rates of fall of TSB were 0.20 [SE = 0.03] and 0.12 [SE = 0.01] mg/dL/hour in the LED and fluorescent groups, respectively (P = 0.472). Treatment duration was 37.5 ± 26.8 and 45.3 ± 32.1 hours in the LED and fluorescent groups, respectively (P = 0.292). There was no treatment failure in the two groups. Mild hyperthermia was occurred in 3.1% and 28.1% of infants in the LED and fluorescent groups, respectively (P = 0.006).
Conclusions:
LED light source is as effective as fluorescent tubes for phototherapy of preterm infants with indirect hyperbilirubinemia. Considering less frequent side effects, less energy consumption, longer life span, and lower costs, LED phototherapy seems to be a better option than current conventional phototherapy.
Keywords: Hyperbilirubinemia, jaundice, premature infant, phototherapy
INTRODUCTION
In neonates, high levels of total serum bilirubin (TSB) can cause severe and irreversible brain damages. Thus, prompt diagnosis and treatment of indirect hyperbilirubinemia is of great importance in this age group. Phototherapy and exchange blood transfusion are two major therapeutic strategies to prevent bilirubin-induced brain damage in neonates. The choice of therapy depends on the severity of hyperbilirubinemia, but phototherapy is the most frequently used treatment.[1]
Besides various clinical factors, characteristics of the light source including wavelength and irradiance along with exposed body surface area can affect the efficacy of phototherapy.[2] Commonly used light sources are fluorescent tubes and halogen spotlights. These light sources, however, have some important limitations. For example, they produce considerable heat and cannot be placed close to the infant. Although this problem can be solved by attaching fiberoptic blankets to the light source, it is not highly effective because of a limited exposure area.[3,4] Because of these limitations, light-emitting diodes (LEDs) have recently been investigated as possible alternatives in phototherapy units. LEDs produce low heat so that they can be placed very close to the infant. The life span of LEDs is longer and their energy consumption is lower than that of the conventional light sources, which make them more cost-effective. Also, gallium nitride LEDs provide a narrow spectral band of monochromatic light with a special wavelength of 458 nm and high intensity, which overlaps the absorption spectrum of bilirubin.[5]
Accordingly, LEDs are supposed to be more efficient than other light sources in phototherapy. There are, however, few available reports comparing the efficacy and safety of LED phototherapy with the conventional devices, only two of them used fluorescent tubes, and the results have been controversial.[6–11] Also, there is no sufficient data for preterm infants in this regard. In this study, we assessed and compared the efficacy and safety of LEDs with fluorescent phototherapy in the treatment of indirect hyperbilirubinemia in preterm infants.
MATERIALS AND METHODS
Patients and settings
This controlled trial was conducted in the neonatal intensive care unit of Shahid Beheshti Hospital in Isfahan (Iran) during the period August to February 2012. Preterm infants (32 to 35 weeks of gestation) with age of ≥48 hours, birth body weight between 1500 and 2000 grams, and a measured TSB of 8 mg/dL or more for whom the decision to use phototherapy was made by the attending neonatologist, were enrolled in the study. Those with the need for intensive phototherapy or blood exchange, direct-reacting component of bilirubin >2 mg/dL, G6PD deficiency, ABO incompatibility, evidence of hemolysis, sepsis, perinatal asphyxia (Apgar score <4 at 1 minute or <7 at 5 minutes), respiratory distress, and major congenital malformations were not included. To find a difference of 0.15 mg/dL/hour in the rate of fall of TSB under phototherapy, the required sample size was calculated as 32 infants in each group. The study protocol was approved by the Ethics Committee of Isfahan University of Medical Sciences and informed consent was obtained from the parents after explaining the aim and protocol of the study.
Interventions
Based on patient's document number, neonates were alternately allocated into two groups of receiving phototherapy with LEDs or fluorescent tube devices. The Bilitron 3006 super-LED phototherapy system (Fanem Medical Inc., Sao Paolo, Brazil) was used for one group and the Tosan phototherapy device (Tosan Co., Tehran, Iran) with four special blue compact fluorescent tubes (Philips TL 52/20W) was used for the other group. In both the groups, the distance between the infant and the light source was kept similar (25 cm). The decision to start phototherapy was made by the attending neonatologist according to the guidelines for management of hyperbilirubinemia in low birth weight infants based on birth weight and relative health.[1] Treatment was stopped when bilirubin dropped into half of the blood exchange level.
During phototherapy, all infants remained in open bassinettes equipped with warming devices at room temperature. They were being fed enterally alone or in combination with parenteral nutrition. Infants were unclothed except for a diaper and their eyes were covered with patches. For the infants receiving phototherapy with the LED device, nothing was placed between the infant and the light source. One single overhead unit was considered for each type of phototherapy and infants were enrolled into the trial if the phototherapy unit of each type was available at enrollment time. At the beginning of the study, new lamps were installed for fluorescent unit and were replaced during the study period after 1000 hours of use or if discolored or produced less light.
Assessments
Demographic data included age, body birth weight, gender, and gestational age. Laboratory examinations included total and direct serum bilirubin concentrations at the time of enrollment, blood groups of the infant and mother, blood tests (for hemolysis, unusually shaped red cells, or evidence of infection), and test for G6PD deficiency. Serum bilirubin concentrations were measured by capillary sampling at the initiation of phototherapy, and every 8, 12, and 24 hours within the first, second, and third days of phototherapy, respectively. Axillary body temperature was measured every 4 hours.
Primary outcomes included the rate of fall of TSB (mg/dL/hour) and duration of phototherapy (hours). Secondary outcomes were treatment failure defined as the need for exchange blood transfusion or intensive phototherapy, side effects like hypothermia (body temperature <36°C), hyperthermia (body temperature >37.5°C), skin rash, and burns.
Statistical analysis
Data were analyzed with the use of SPSS software for windows version 16.0 (SPSS Inc., Chicago, IL). Independent t-test and Mann–Whitney test were used for comparison of parametric and nonparametric continuous variables. Chi-square test was applied for qualitative variables. Multivariate analysis was done for controlling confounding factors. Data are presented as number (%), mean ± standard deviation (SD), and mean ± standard of error (SE) when data were not normally distributed. A P value of less than 0.05 was considered significant in all analyses.
RESULTS
A total of 64 newborn infants, consisted of 37 male and 27 female, were enrolled in the study with characteristics described in Table 1 and all of them completed the study [Figure 1]. The groups were similar regarding baseline characteristics except gestational age, which was about one week greater in the LEDs group (P = 0.002).
Table 1.
Demographic and baseline characteristics of the newborns
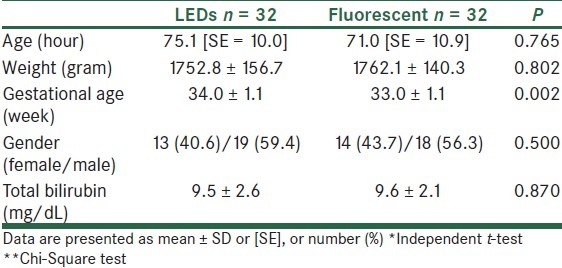
Figure 1.
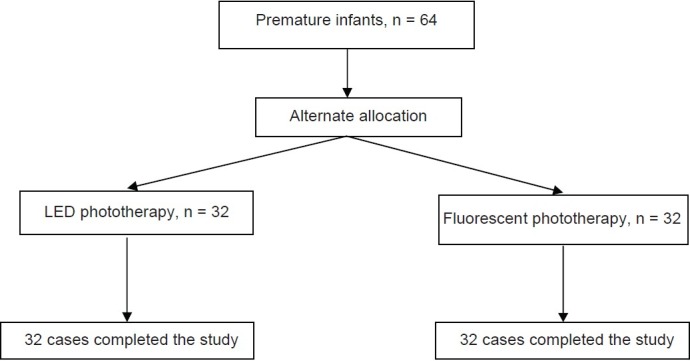
Patients flow diagram
The rate of fall of TSB during phototherapy was 0.20 [SE = 0.03] and 0.12 [SE = 0.01] mg/dL/hour in the LEDs and fluorescent groups, respectively (P = 0.472, Mann-Whitney Test); Figure 2. This resulted in a treatment duration of 37.5 ± 26.8 and 45.3 ± 32.1 hours in the LED and fluorescent group, respectively (P = 0.292); Figure 3.
Figure 2.
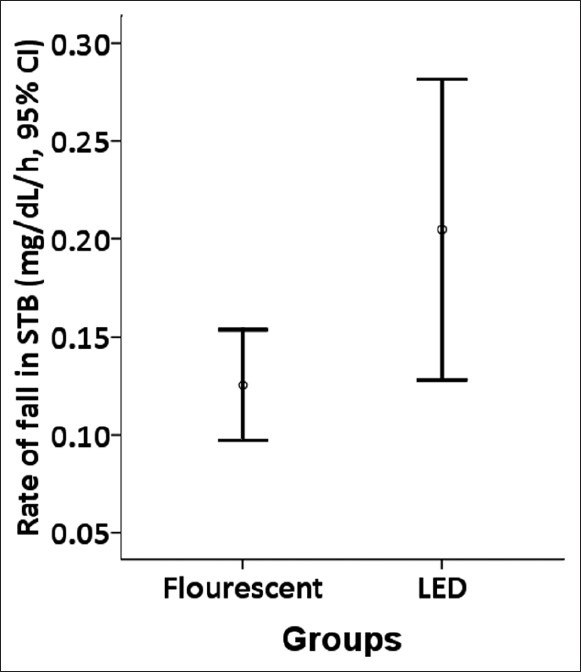
Rate of fall in serum total bilirubin in the LED and fluorescent phototherapy groups
Figure 3.
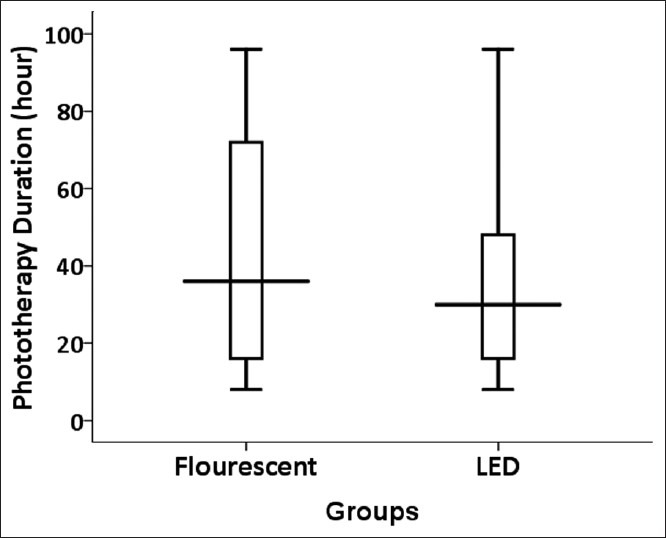
Phototherapy duration in the LED and fluorescent phototherapy groups
There was no treatment failure in two groups. Mild hyperthermia occurred in 3.1% and 28.1% of infants in the LEDs and fluorescent groups (P = 0.006). Hypothermia occurred only in two infants in the fluorescent group (P = 0.246).
Regarding difference between the two groups in gestational age, a linear regression analysis was done controlling for possible confounding factors including age, gestational age, weight, and the type of intervention. Multivariate analysis did not show any association of the mentioned factors with the rate of fall of bilirubin or with the duration of phototherapy.
DISCUSSION
Various characteristics of the light source, used in phototherapy for neonatal jaundice, can affect the efficacy of treatment. Regarding limitations of commonly used phototherapy units such as producing considerable heat and instability in wavelength output, LED phototherapy units have recently been investigated as possible alternatives. LED units produce very low heat, have longer life span, consume less energy, and produce more stable narrow wavelength high-intensity light.[2,4] We compared LEDs with fluorescent phototherapy unit in the treatment of preterm infants with neonatal jaundice. The results showed that duration of phototherapy was the same, and the nonsignificant difference between the two methods in the rate of fall of bilirubin was possibly related to the difference between groups in gestational age, as the multivariate analysis did not show any association between the type of treatment and outcomes. The LEDs unit, however, resulted in less frequent hyperthermia, while 28.1% of infants in the fluorescent group experienced hyperthermia (though mild). These results were similar with most of the previous reports indicating that LEDs units are as effective as conventional phototherapy units.[9–11]
The ‘rate of fall of bilirubin’ and ‘duration of phototherapy’ have been the two main outcomes investigated by the previous studies, as well as this study.[5] In the randomized controlled trial by Martins et al. on preterm neonates, comparing indium gallium nitrate LEDs with halogen phototherapy, results showed greater decrease in TSB levels and shorter duration of phototherapy in the LEDs group. These results could be attributed to the lesser irradiance of halogen lamps and broad spectrum of light emitted by them in comparison to LEDs.[8] A meta-analysis by Kumar and colleagues on available randomized trials indicated a comparable rate of fall of bilirubin as well as duration of treatment in the LEDs and nonLEDs phototherapy groups; but in separate analysis of studies comparing LEDs with halogen light sources, mean duration of phototherapy was significantly shorter with LEDs devices. This difference was not observed in the studies comparing LEDs with fluorescent light sources. Thus, it seems possible that LEDs light sources are more effective than halogen lamps for phototherapy in neonatal jaundice.[5]
Although most of the previous studies reported rare and comparable side effects in LEDs and nonLED phototherapy groups,[5] we found a higher incidence of hyperthermia with fluorescent tubes. However, all of the cases were mild and transient and we did not observe any severe side effect. Bertini and colleagues showed that conventional phototherapy units result in a significant increase of transepidermal water loss in preterm infants, and this side effect was not observed with LED units.[6] Therefore, regarding better safety and efficacy, LED phototherapy seems to be better than conventional phototherapy with halogen or fluorescent light sources in preterm infants, though further studies are required in this regard.
There are some limitations to our study. The sample size of our study was not large enough to find small differences between LEDs and fluorescent phototherapy methods with regards to rate of fall of bilirubin and duration of therapy. Also, our study was done only in one center and because blinding the clinical team about the type of phototherapy is somehow impossible, it is better for future studies to be conducted in multi centers. And the last, nonrandomized allocation of the cases in our study resulted in a difference between groups in gestational age, though we did a multivariate analysis and controlled this factor.
CONCLUSIONS
The results of this study showed that LED light source is as effective as fluorescent tubes for the phototherapy of preterm infants with indirect hyperbilirubinemia. Considering less frequent side effects, less energy consumption, longer life span, and lower costs, LED phototherapy seems to be a better option than current conventional phototherapy. More studies are warranted for evaluating the efficacy of LED phototherapy in infants with pathologic jaundice (e.g., hemolytic) and severe hyperbilirubinemia. Because LEDs produce low heat, studies are warranted to evaluate the efficacy of LED phototherapy when kept very close to the skin, e.g., in clothing or a blanket.
ACKNOWLEDGMENTS
This study was supported by the Isfahan University of Medical Sciences (project 389344). The authors thank the nursing staff of the Neonatal Intensive Care Units at teaching hospitals affiliated to Isfahan University of Medical Sciences, Isfahan, Iran. The authors also thank Dr Ali Gholamrezaei for helping them in the data analysis and editing this report.
Footnotes
Source of Support: Isfahan University of Medical Sciences
Conflict of Interest: None declared
REFERENCES
- 1.Ip S, Chung M, Kulig J, O’Brien R, Sege R, Glicken S, et al. American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. An evidence-based review of important issues concerning neonatal hyperbilirubinemia. Pediatrics. 2004;114:e130–53. doi: 10.1542/peds.114.1.e130. [DOI] [PubMed] [Google Scholar]
- 2.Bhutani VK Committee on Fetus and Newborn; American Academy of Pediatrics. Phototherapy to prevent severe neonatal hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2011;128:e1046–52. doi: 10.1542/peds.2011-1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mills JF, Tudehope D. Fibreoptic phototherapy for neonatal jaundice. Cochrane Database Syst Rev. 2001;(1):CD002060. doi: 10.1002/14651858.CD002060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vreman HJ, Wong RJ, Stevenson DK. Phototherapy: Current methods and future directions. Semin Perinatol. 2004;28:326–33. doi: 10.1053/j.semperi.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 5.Kumar P, Chawla D, Deorari A. Light-emitting diode phototherapy for unconjugated hyperbilirubinaemia in neonates. Cochrane Database Syst Rev. 2011:CD007969. doi: 10.1002/14651858.CD007969.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bertini G, Perugi S, Elia S, Pratesi S, Dani C, Rubaltelli FF. Transepidermal water loss and cerebral hemodynamics in preterm infants: Conventional versus LED phototherapy. Eur J Pediatr. 2008;167:37–42. doi: 10.1007/s00431-007-0421-3. [DOI] [PubMed] [Google Scholar]
- 7.Kumar P, Murki S, Malik GK, Chawla D, Deorari AK, Karthi N, et al. Light emitting diodes versus compact fluorescent tubes for phototherapy in neonatal jaundice: A multi center randomized controlled trial. Indian Pediatr. 2010;47:131–7. doi: 10.1007/s13312-010-0020-7. [DOI] [PubMed] [Google Scholar]
- 8.Martins BM, de Carvalho M, Moreira ME, Lopes JM. Efficacy of new microprocessed phototherapy system with five high intensity light emitting diodes (Super LED) J Pediatr (Rio J) 2007;83:253–8. doi: 10.2223/JPED.1637. [DOI] [PubMed] [Google Scholar]
- 9.Seidman DS, Moise J, Ergaz Z, Laor A, Vreman HJ, Stevenson DK, et al. A new blue light-emitting phototherapy device: A prospective randomized controlled study. J Pediatr. 2000;136:771–4. [PubMed] [Google Scholar]
- 10.Seidman DS, Moise J, Ergaz Z, Laor A, Vreman HJ, Stevenson DK, et al. A prospective randomized controlled study of phototherapy using blue and blue-green light-emitting devices, and conventional halogen-quartz phototherapy. J Perinatol. 2003;23:123–7. doi: 10.1038/sj.jp.7210862. [DOI] [PubMed] [Google Scholar]
- 11.Viau CJ, Rountree C, Destarac MA, Cui Y, Perez VM, Herrera CM, et al. Prospective randomized controlled study comparing low-cost LED and conventional phototherapy for treatment of neonatal hyperbilirubinemia. J Trop Pediatr. 2012;58:178–83. doi: 10.1093/tropej/fmr063. [DOI] [PubMed] [Google Scholar]


