Abstract
Objective
To identify mechanisms by which Smad3 maintains articular cartilage and prevents osteoarthritis.
Methods
A combination of in vivo and in vitro approaches was used to test the hypothesis that Smad3 represses Runx2-inducible gene expression to prevent articular cartilage degeneration. Col2-Cre;Smad3fl/fl mice allowed study of the chondrocyte-intrinsic role of Smad3, independently of its role in the perichondrium or other tissues. Primary Smad3fl/fl articular chondrocytes and ATDC5 chondroprogenitors were employed to evaluate Smad3 and Runx2 regulation of matrix metalloproteinase-13 (MMP-13) mRNA and protein expression.
Results
Chondrocyte-specific reduction of Smad3 causes progressive articular cartilage degeneration due to imbalanced cartilage matrix synthesis and degradation. In addition to reduced collagen II mRNA expression, Col2-Cre;Smad3fl/fl articular cartilage is severely deficient in collagen II and aggrecan protein, due to excessive MMP-13-mediated proteolysis of these key cartilage matrix constituents. Normally, TGF-β signals through Smad3 to confer a rapid and dynamic repression of Runx2-inducible MMP-13 expression. However, in the absence of Smad3, TGF-β signals through p38 and Runx2 to induce MMP-13 expression.
Conclusion
This work elucidates a mechanism by which Smad3 mutations in humans and mice cause cartilage degeneration and osteoarthritis. Specifically, Smad3 maintains the balance between cartilage matrix synthesis and degradation by inducing collagen II expression and repressing Runx2-inducible MMP-13 expression. Selective activation of TGF-β signaling through Smad3, rather than p38, may help to restore the balance between matrix synthesis and proteolysis that is lost in osteoarthritis.
In osteoarthritis, the tightly controlled balance of matrix synthesis and degradation is disrupted, resulting in progressive breakdown of articular cartilage. At the cellular level, normal articular chondrocytes express collagen II and aggrecan, two major components of healthy cartilage matrix (1). In osteoarthritic cartilage, chondrocyte function is deregulated, such that expression of Col2 in the superficial layer is reduced (2) and expression of the matrix degrading protease MMP-13 is increased (3, 4). As of yet, the inciting molecular events and pathways involved in this progressive loss of articular chondrocyte homeostasis in osteoarthritis are not completely understood.
TGF-β plays a well-established role in the control of chondrocyte differentiation, matrix synthesis, and homeostasis. Disruption of TGF-β signaling results in accelerated chondrocyte terminal differentiation, both in vitro and in vivo (5). Not only is an osteoarthritic phenotype observed in mice that express a dominant negative TGF-β type II receptor, but also in mice with systemic ablation of Smad3 (6), a key effector of TGF-β signaling. Other mouse models in which levels of functional Smad3 are reduced, such as mice that overexpress a Smad-degrading protease, Smurf2 (7), also exhibit an arthritic phenotype. Importantly, human polymorphisms in the Smad3 gene have been implicated in hip and knee arthritis, providing further evidence of the involvement of TGF-β/Smad3 in osteoarthritis (8).
The mechanism through which TGF-β/Smad3 regulates chondrocyte differentiation in the growth plate has been extensively studied. Smad3 plays a well-established role in the perichondrium, where it participates in a feedback loop that inhibits terminal differentiation of growth plate chondrocytes (9–11). Specifically, chondrocyte-derived Indian hedgehog (Ihh) stimulates TGF-β signaling through Smad2/3 in the perichondrium, which, in turn, induces parathyroid hormone-related protein (PTHrP)-mediated repression of chondrocyte hypertrophy. Though the progression of osteoarthritis recapitulates some aspects of growth plate chondrocyte differentiation, these two processes are not identical. Unlike growth plate chondrocytes, articular chondrocytes are not regulated by perichondrial signaling. A distinct, chondrocyte-intrinsic role of Smad3 is supported by the articular cartilage defects in Smad3-deficient mice. However, systemic loss of Smad3 affects multiple tissues and cell types (12–15), complicating the interpretation of results. Several in vitro studies provide further evidence for chondrocyte-intrinsic Smad3 signaling (11, 16), though mechanisms by which Smad3 mediates the effects of TGF-β, such as its ability to maintain chondrocyte homeostasis, remain unclear.
MMP-13, a matrix metalloproteinase (MMP), is expressed at high levels in osteoarthritic cartilage (3, 4). Since MMP-13 cleaves key extracellular matrix constituents, including collagen II and aggrecan, its expression and activity are tightly regulated. One of the important regulatory regions of the MMP-13 promoter is the Runx2 binding site, which has been implicated in the TGF-β-inducible expression of MMP-13 in breast cancer cells and osteoblasts (17, 18). TGF-β has also been shown to repress MMP-13 expression, though the mechanisms remain unclear (19). We previously showed that TGF-β activates Smad3 to repress Runx2-inducible Runx2 and osteocalcin expression in osteoblasts (20). This led us to hypothesize that Smad3 also represses Runx2-inducible gene expression in chondrocytes, and that this regulatory mechanism is required to prevent MMP-13-mediated degeneration of articular cartilage.
To test this hypothesis, we generated Col2-Cre;Smad3fl/fl mice, which are deficient in Smad3 in chondrocytes, but not in perichondrial cells or other tissues. Molecular analysis of articular cartilage phenotypes revealed an increase in MMP-13 levels in Smad3-deficient cartilage. Therefore, we utilized primary articular chondrocytes and ATDC5 chondroprogenitor cells to investigate the chondrocyte-intrinsic mechanisms by which Smad3 regulates the expression of MMP-13. Because MMP-13 is a driver of arthritic cartilage degeneration, understanding its regulation by Smad3 elucidates mechanisms by which Smad3 maintains chondrocyte homeostasis and prevents osteoarthritis.
MATERIALS AND METHODS
Col2-Cre and Smad3fl/fl Mice
Col2-Cre mice express Cre recombinase under control of a 3 kb segment of the collagen II promoter. Excision at floxed loci followed by recombination occurs specifically in chondrocytes but not in perichondrial cells (21). Smad3fl/fl mice, generously provided by Dr. Jonathan Graff, have been used to examine the role of Smad3 in ovarian tissues (22). Procedures involving mice were performed in accordance with UCSF Institutional Animal Care and Use Committee-approved protocols. To confirm specific recombination at the floxed Smad3 locus, DNA was isolated from homogenized liver, lung, femur, and articulating tail joints collected from 60 day old Col2-Cre;Smad3fl/fl mice. PCR was performed using primers that specifically amplify the floxed and recombined Smad3 alleles (22).
RNA isolation and analysis of gene expression
For analysis of gene expression, costal cartilage was isolated from post-natal day 60 (P60) mice (n=5) and frozen in liquid nitrogen. Smad3fl/fl littermates were used as controls. Costal cartilage was finely ground using a liquid nitrogen chilled mortar and pestle followed by Trizol extraction. RNA was column purified, including an on-column DNAse digestion, using the Purelink RNA Mini Kit (Invitrogen). RNA was purified from cultured cells using the RNeasy Mini Kit (Qiagen) and on-column DNAse digestion according to the manufacturer’s instructions. All in vitro data represent the average of experimental duplicates (n=2) performed on biological triplicates (n=3). RNA concentration and purity were determined using a Nanodrop spectrophotometer. cDNA was reverse transcribed using the iScript cDNA synthesis kit (BioRad).
Transcripts were amplified using the CFX96 Real-Time PCR Detection System (BioRad) with SYBR Green Master Mix (Applied Biosciences) and primer sets for Smad3, Agn, Col2, MMP-13, and Runx2 (Supplementary Table 1). Gene expression was normalized to L19 and fold expression analyzed using the Delta-Delta Ct method. Statistical analysis of gene expression was compared using the two-tailed Student’s t-test with a significance threshold of p < 0.05.
Histological analysis
Safranin-O staining and modified Mankin scoring: To visualize proteoglycan content, knee joints were isolated from P14, P60, P90, and P120 mice, fixed in 4% paraformaldehyde, decalcified in 19% EDTA, and embedded in paraffin. Sagittal sections (7.5 µm) were stained with safranin-O and counterstained with fast green. Representative images of stained sections are shown. The modified Mankin scoring system (23) was used by a blinded orthopaedic surgeon to assess the degree of cartilage degeneration on eight safranin-O-stained sections representing four mice per genotype. Immunohistochemistry: To visualize the localization of collagen II and aggrecan in mouse articular cartilage, immunohistochemistry was carried out on paraffin embedded sections after antigen retrieval with 2.5% hyaluronidase (Sigma) and as previously described (24), respectively. The following antibodies were used: mouse anti-aggrecan 12/21/1-C-6 (Developmental Studies Hybridoma Bank) and rabbit anti-collagen II (AbCam). The Mach4 universal detection system (Biocare Medical) and DAB Substrate Kit for Peroxidase (Vector Laboratories) were used to detect primary antibody binding. To visualize the localization of MMP-13, sections were incubated with goat anti-mouse-MMP-13 (Millipore). A donkey anti-goat secondary antibody (Santa Cruz) was used with the goat IgG Vectastain ABC Kit (Vector Laboratories) to detect primary antibody binding. As a negative control, the primary antibody was replaced with control IgG from the same species at the same concentration as the primary antibody. To visualize the localization of neoepitopes of collagen degradation (GPQG) or aggrecan degradation (VDIPEN) by MMP-13, antigen retrieval with 2.5% hyaluronidase was followed by incubation with the primary rabbit-derived antibodies, a gift from Dr. John Mort, at room temperature overnight (25, 26). Preimmune serum was used as a negative control. The rabbit IgG Vectastain ABC Kit (Vector Laboratories) was used to detect primary antibody binding. Images are representative of 3 or more immunohistochemistry experiments per condition.
Cell Culture
Primary Articular Chondrocytes
Femoral head, condyle, and tibial plateau articular cartilage was isolated from P5 Smad3fl/fl mice. Cells were isolated as described and cultured in DMEM with L-glutamine, penicillin/streptomycin, and 10% FBS (27). Spinfection was performed at 70% confluency with replication-deficient adenovirus expressing Cre recombinase to inactivate Smad3 in cultured Smad3fl/fl chondrocytes (28). As a negative control, cells were infected with adenovirus expressing GFP. After infection, cells were treated with 5 ng/ml TGF-β3 (Peprotech) for 8, 24 and 48 hours followed by isolation of RNA and protein.
ATDC5 chondroprogenitor cells
ATDC5 cells (RIKEN), were cultured in monolayer in DMEM high glucose with 5% FBS. In all experiments, TGF-β treatment of ATDC5s commenced upon confluence.
Transient Transfection and Reporter Gene Analysis
ATDC5 cells were transiently transfected using Fugene 6 (Roche) at 70% confluence with indicated expression and reporter constructs including p6OSE2-Luc (29), 3TP-Luc (30), -370 MMP-13-Luc (31), and pRK5-β-gal (32) in the presence or absence of pRK5-based expression plasmids for Smad3 or Runx2 (20). Cells were incubated for 24 hours post-transfection prior to TGF-β treatment for the indicated time. Lysates were harvested using Promega Lysis Buffer, clarified, and assayed for luciferase and β-galactosidase activity as described (20) using a plate reader luminometer (Molecular Devices). Luciferase activity was normalized to activity of a cotransfected, constitutively expressed β-galactosidase reporter construct. Figures are representative of three independent experiments, each of which was performed in triplicate.
Viral infection to ablate Smad3 and Runx2
ATDC5 cells were infected with viral vectors expressing siRNA against Runx2 (Sigma, nm004348) or shRNA against Smad3 (gift from Dr. Rik Derynck and produced by the UCSF Lentiviral RNAi Core) using a spinfection protocol. Briefly, viral particles, and siRNA oligonucleotides were added to cells at an MOI of 5 in 1 ml Optimem (Gibco) with 1 µg of polybrene (Sigma-Aldrich). Six-well plates were centrifuged at 1550 rpm for 45 minutes at 37°C. The virus-containing media was replaced with fresh DMEM with 5% FBS and incubated for 24 hours prior to TGF-β treatment and subsequent isolation of RNA or protein. Each viral infection and ablation culture was performed in triplicate (n=3).
Western Blot
Because FBS contains a protein that interferes with Western detection of secreted MMP-13, analyses were performed on whole cell lysates, a method that was validated by ELISA analysis of MMP-13 in conditioned media. Protein lysates were harvested using 1× RIPA Lysis Buffer (5mm Na3VO4, 10mM NaPPi, 100mM NaF, 500µM PMSF, 1 MiniComplete tablet (Roche)). Lysates were sonicated on ice prior to freezing on dry ice. Thawed lysates were clarified by centrifugation prior to Bradford quantification of protein concentration. Equal concentrations of protein were resolved using an 8.5% SDS-polyacrylamide gel with a 5% stacking gel prior to transfer to a nitrocellulose membrane. Western analysis was performed using a 1:1000 dilution of 200 µg/ml rabbit anti-mouse MMP-13 (Santa Cruz) and 1:500 of 200 µg/ml mouse anti-rabbit GFP (Santa Cruz). Secondary antibodies, IR tagged goat anti-rabbit and goat antimouse (Odyssey), were used at a dilution of 1:20,000. The infrared signal of secondary antibodies was detected, quantified, and normalized to beta-actin levels using the Odyssey Infrared Detection Scanner (Li-Cor). The blots shown are representative of three or more experiments.
Results
Chondrocyte-intrinsic Smad3 maintains normal articular cartilage
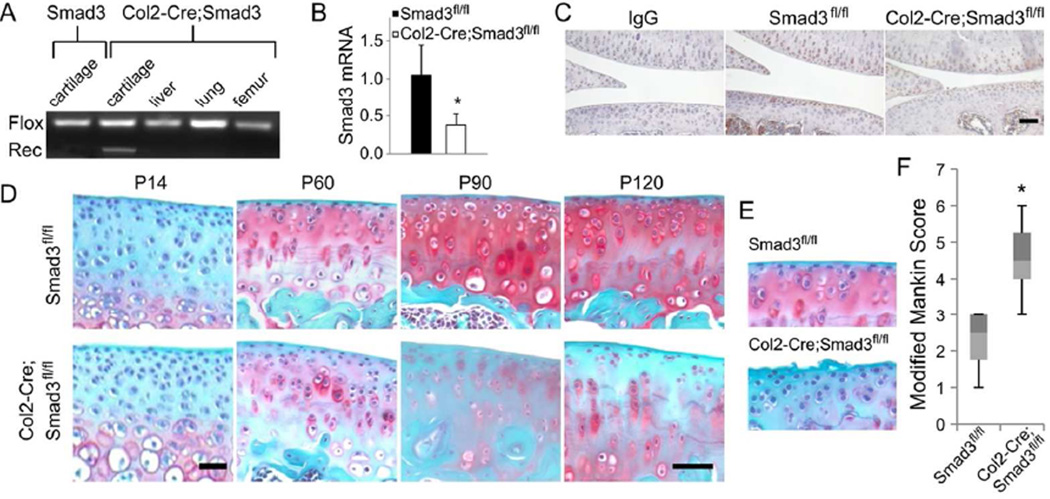
To evaluate the chondrocyte-intrinsic role of Smad3 in cartilage development and maintenance, we first generated mice with inactivation of Smad3 in Col2-expressing cells, targeting chondrocytes but not perichondrial cells (21). Mice with floxed Smad3 alleles (22) were crossed with Col2-Cre transgenic mice (21). The recombined Smad3 allele was detected in genomic DNA isolated from Col2-Cre;Smad3fl/fl articular cartilage but not from liver, lung, femoral bone, or articular cartilage isolated from control mice lacking the Col2-Cre allele, demonstrating the specificity of Smad3 ablation (Fig. 1A). The level of Smad3 mRNA expression in Col2-Cre;Smad3fl/fl mouse cartilage was reduced by 60% relative to Cre-negative, Smad3fl/fl littermates (Fig. 1B). Immunohistochemistry showed less Smad3 protein in articular cartilage from these mice (Fig. 1C). Smad3 levels were also reduced in the growth plate, which showed modest disorganization and a slight reduction in proteoglycan content (Supplementary Fig. 1A–B).
Figure 1. Chondrocyte-intrinsic Smad3 is required to maintain articular cartilage.
(A) PCR analysis of genomic DNA reveals that Cre-mediated recombination only occurs in Col2-expressing cartilage. (B) Real-time RT-PCR shows reduction of Smad3 mRNA expression in postnatal day 60 (P60) Col2-Cre;Smad3fl/fl mouse cartilage (*p-value < 0.02). (C) Immunohistochemistry for Smad3 confirms a reduction of Smad3 protein in articular cartilage of P60 Col2-Cre;Smad3fl/fl mice relative to Cre-negative Smad3fl/fl littermates. (D) Safranin-O staining shows no changes in articular cartilage until P60 and later. (E) Magnified safranin-O stained sections of the articular surface of P60 Col2-Cre;Smad3fl/fl mice show fibrillation and decreased staining compared to Smad3fl/fl littermates. (F) Col2-Cre;Smad3fl/fl cartilage displays an increased modified Mankin score for P60 Col2-Cre;Smad3fl/fl joints, indicative of osteoarthritis-like joint degeneration (* p-value < 0.002). (Bars = 50µm)
The phenotype of Col2-Cre;Smad3fl/fl mice was more pronounced in articular cartilage. Although differences in proteoglycan content were not detectable at post-natal day 14, Smad3-dependent differences became apparent by post-natal day 60, when Col2-Cre;Smad3fl/fl knee joints exhibited decreased overall safranin-O staining, which became more pronounced with age (Fig. 1D). Other hallmarks of osteoarthritis were observed in mutant joints by P60, including deterioration of the smooth articular cartilage surface and fibrillation of the superficial layer (Fig. 1E). Modified Mankin scoring (23) confirmed that chondrocyte-specific deficiency of Smad3 causes significant morphological changes that parallel the progression of osteoarthritis (Fig. 1F).
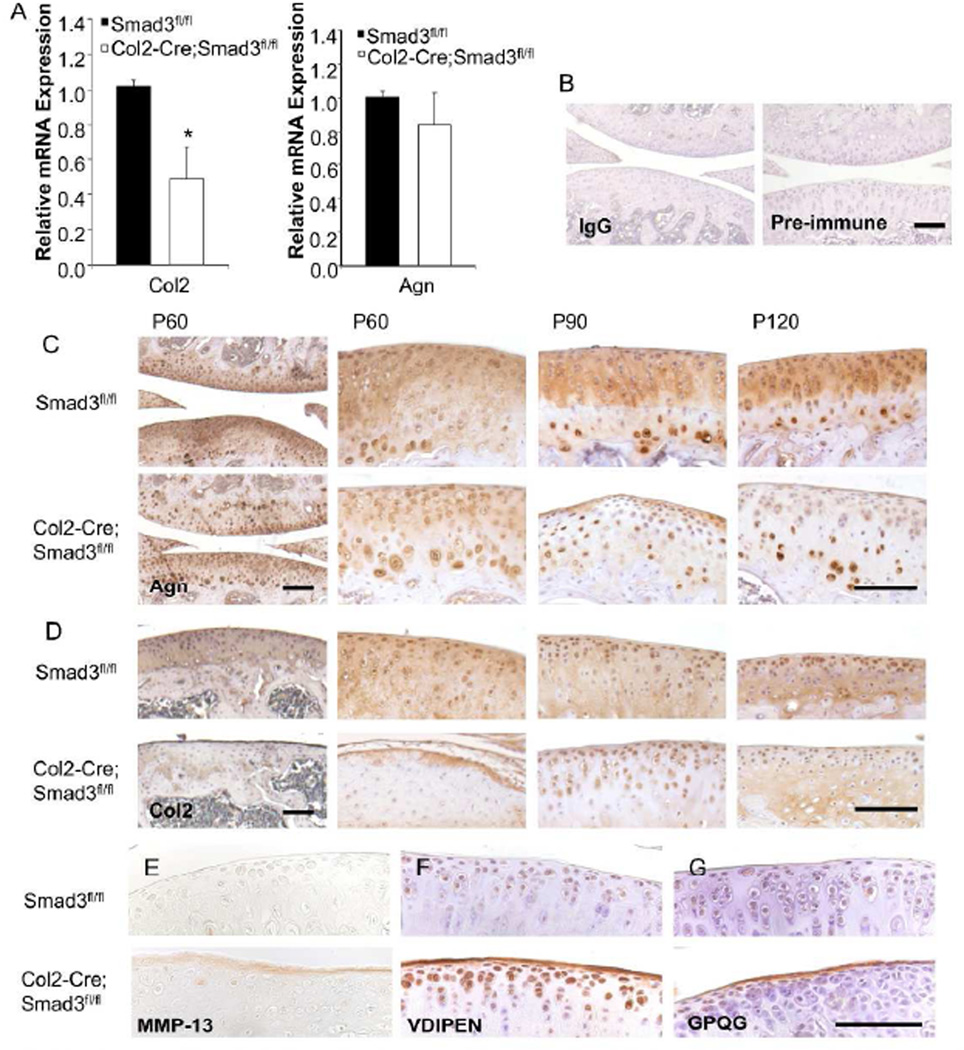
Smad3 maintains normal cartilage matrix composition
To investigate the molecular basis of the Smad3-dependent differences in cartilage matrix structure and composition, we evaluated the expression levels of key cartilage matrix constituents, collagen II (Col2) and aggrecan (Agn). Though we did not observe a decrease in Agn mRNA expression (Fig. 2A), immunohistochemical analysis showed a marked decrease and heterogeneity of staining for Agn protein in P60 and older Col2-Cre;Smad3fl/fl articular cartilage (Fig. 2C). This suggests that Agn protein levels may be regulated by a post-transcriptional mechanism or have an increased turnover rate in Smad3-deficient mice. Col2 mRNA expression was reduced by 50% in cartilage from p60 Col2-Cre;Smad3fl/fl mice relative to Cre-negative controls (Fig. 2A). The reduction in collagen II was even more apparent at the protein level, where immunohistochemistry revealed a progressive loss of collagen II protein in Col2-Cre;Smad3fl/fl articular cartilage (Fig. 2D). Therefore, chondrocyte intrinsic Smad3 is essential for the sustained expression of two key components of cartilage matrix, aggrecan and collagen II.
Figure 2. Molecular composition of articular cartilage is disrupted in Col2-Cre;Smad3fl/fl mice.
(A) To examine Col2 and Agn expression in costal cartilage of P60 mice, mRNA expression was quantified and normalized to L19 (n=5; *p-value < 0.02). (B) Immunohistochemistry (IHC) negative controls. Primary antibodies were replaced with either IgG (controls for C, D) or preimmune serum (controls for F, G) to confirm specificity of IHC staining. IHC in P60, P90, and P120 Col2-Cre;Smad3fl/fl mice revealed a progressive reduction in aggrecan (C) and collagen II (D), but an increase in MMP-13 (E) protein expression in articular cartilage of P90 Col2-Cre;Smad3fl/fl mice. IHC with antibodies to neoepitopes VDIPEN (F) and GPQG (G), MMP-13 cleavage products of Agn and Col2, respectively, shows increased MMP-13 cleavage of cartilage matrix in P90 Col2-Cre;Smad3fl/fl mice, particularly at the articular surface. (Bars = 100 µm.)
Elevated MMP-13 expression in Col2-Cre;Smad3fl/fl cartilage
Degenerative changes in cartilage matrix may result from reduced matrix synthesis, increased matrix degradation, or both. Thus, we investigated the expression level and localization of MMP-13, a matrix metalloproteinase that degrades aggrecan (33) and collagen II (26) and is elevated in osteoarthritis. Unlike control Smad3fl/fl littermates, MMP-13 expression in Col2-Cre;Smad3fl/fl cartilage was highly variable, though with no statistically significant up or down-regulation at the mRNA level (data not shown). However, intense expression of MMP-13 protein was consistently detected in the superficial zone of Col2-Cre;Smad3fl/fl cartilage by P90 (Fig. 2E). Furthermore, antibodies that specifically detect neoepitopes created by MMP-13 degradation of aggrecan (VDIPEN) and collagen II (GPQG) showed more intense articular cartilage staining in Col2-Cre;Smad3fl/fl mice (Fig. 2F–G). Notably, the loss of Agn staining is most evident at the articular surface (Fig. 2C), coinciding with the most intense VDIPEN staining and least safranin-O staining (Fig. 1D). While a striking increase in staining for MMP-13-cleaved proteins was observed on the articular surface in Col2-Cre;Smad3fl/fl mice, no differences were seen in the growth plate (Supplementary Fig. 1G–H). Therefore, chondrocyte-intrinsic Smad3 is required for normal transactivation of collagen II and suppression of MMP-13 expression, as well as for the MMP-13-mediated cleavage of aggrecan and collagen II that accompanies articular cartilage degeneration.
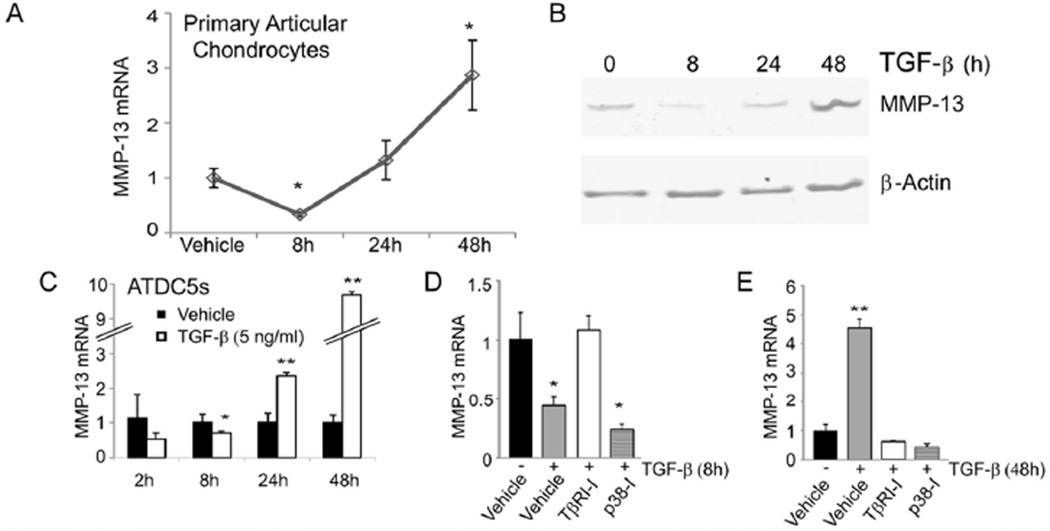
Dynamic regulation of MMP-13 expression by TGF-β
Understanding the role of Smad3 in suppressing MMP-13-mediated cartilage matrix degradation may elucidate the mechanisms by which TGF-β prevents loss of chondrocyte homeostasis as well as the mechanisms by which MMP-13 expression is deregulated in osteoarthritis. To that end, we employed in vitro models to more precisely examine the cell-intrinsic effects of TGF-β and Smad3 on MMP-13 expression. In primary articular chondrocytes, TGF-β repressed the expression of MMP-13 mRNA and protein within 8h, followed by a later induction at 24 and 48h (Fig. 3A–B). ATDC5 cells showed the same pattern of MMP-13 mRNA and protein regulation, with repression detectable as early as 2h after TGF-β treatment (Fig. 3C, 4F–G, 5C–D). Both the early repression and later induction of MMP-13 mRNA by TGF-β were lost upon treatment with the TGFβRI inhibitor SB431542 (Fig. 3D–E). Consistent with prior reports (18), TGF-β inducible MMP-13 expression at 48h was sensitive to p38 inhibition with SB203580 (Fig. 3E). However, the rapid repression of MMP-13 by TGF-β was maintained even following p38 inhibition (Fig. 3D). Unlike the well-documented induction of MMP-13 by TGF-β, the mechanism responsible for the rapid repression of MMP-13 by TGF-β was unknown.
Figure 3. TGF-β regulation of MMP-13 expression in chondrocytes is dynamic.
TGF-β (5 ng/ml) rapidly represses and later induces MMP-13 mRNA (A) and protein (B) expression in primary articular chondrocytes harvested from P5 wild type mice. (C) ATDC5 cells display the same trend. The repression of MMP-13 in ATDC5 cells treated for 8 h with TGF-β is sensitive to an inhibitor of the TGF-β type I receptor (TβRI-I, SB431542, 1 µM) but not to an inhibitor of p38 (p38-I, SB203580, 1 µM). (D). However, the TGF-β-mediated induction of MMP-13 at 48 h is sensitive to both the TβRI-I and the p38-I (E). Vehicle treated cells received an equivalent volume of DMSO. (*p < 0.05, **p < 0.001 relative to the vehicle treated controls at each time point.)
Figure 4. TGF-β-mediated repression and induction of MMP-13 is Runx2-dependent.
(A) Though TGF-β induces activity of the synthetic Smad3 reporter gene 3TP-Luc transiently transfected with pRK5 in ATDC5 cells, it represses Runx2-inducible p6OSE2-Luc activity, even more with cotransfected pRK5-Smad3 (B). The activity of -370-MMP-13-Luc is increased by co-transfection of Runx2, but decreased with TGF-β addition or with cotransfected Smad3 or constitutively active TβRI (C). Runx2-knockdown was sufficient to nearly abolish both the rapid 8 h repression (D, F) and delayed 24 h induction (E, G) of MMP-13 mRNA (D, E) and protein (F, G) by TGF-β (5 ng/ml). (*p < 0.05, **p < 0.001 relative to the vehicle-treated controls in A, C, E, and F, and relative to the scramble siRNA in D.)
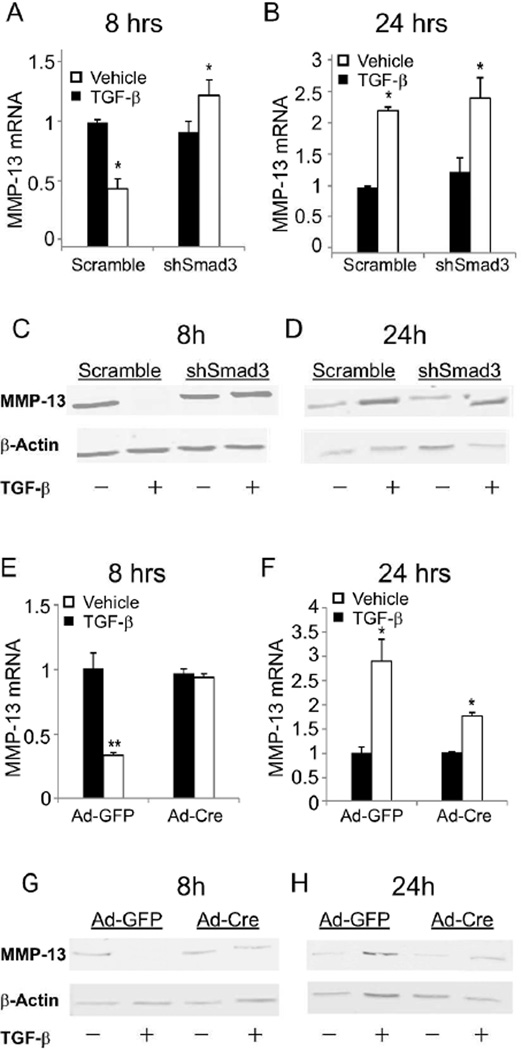
Figure 5. TGF-β-mediated repression of MMP-13 requires Smad3.
Smad3-deficient ATDC5 cells (A, C) and primary chondrocytes (E, G) do not show TGF-β mediated repression of MMP-13 mRNA (A, E) or protein (C, G) at 8 h. However, the induction of MMP-13 by TGF-β at 24 h is maintained in Smad3-deficient ATDC5 cells (B, D) and is reduced but present in primary articular chondrocytes (F, H). (*p < 0.05, **p < 0.001 relative to the vehicle-treated controls in A, B, E, and F.)
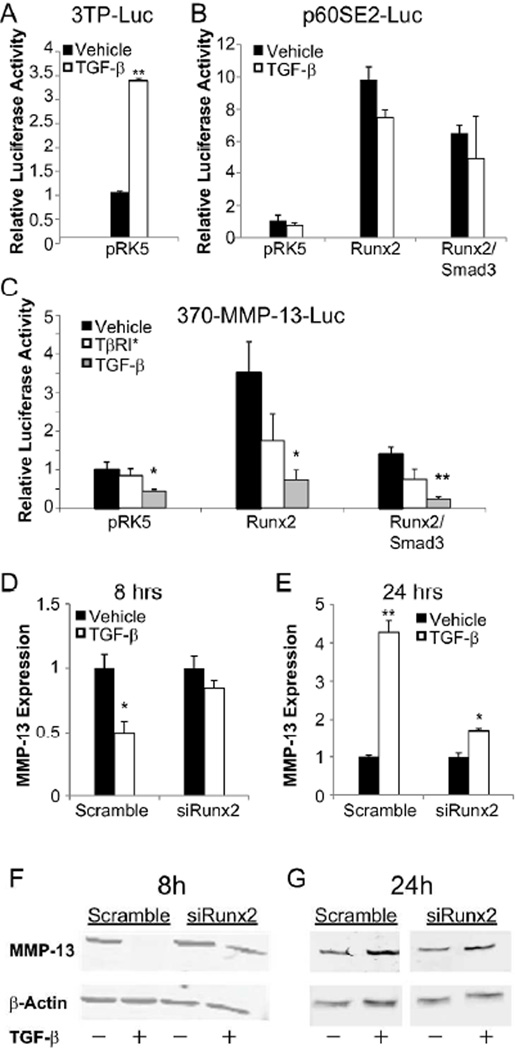
TGF-β-activated Smad3 represses Runx2 function in chondrocytes
In osteoblasts, Smad3 is required for TGF-β-mediated repression of Runx2-inducible genes (20). Since MMP-13 is also a Runx2-inducible gene (34), we hypothesized that this mechanism may confer rapid TGF-β-mediated repression of MMP-13 in chondrocytes. As expected, the synthetic TGF-β-inducible reporter construct 3TP-Luc was induced by TGF-β in ATDC5 cells (Fig. 4A). However, the Runx2-mediated activation of p6OSE2-Luc, a synthetic Runx2-inducible reporter construct, was repressed by TGF-β (Fig. 4B). Overexpression of Smad3 further repressed Runx-2-inducible transactivation in chondrocytes (Fig. 4B). Therefore, TGF-β can repress Runx2-mediated transactivation in chondrocytes as it does in osteoblasts.
To determine if this mechanism was sufficient to confer TGF-β-mediated repression of MMP-13 transcription, ATDC5 cells were transfected with -370-MMP-13-Luc (31), an MMP-13 promoter-reporter construct that retains Runx2-inducibility (Fig. 4C). Basal and Runx2-inducible -370-MMP-13-Luc activity was repressed by TGF-β or by overexpression of a constitutively active version of the TGF-β type I receptor. This repression was even greater upon co-transfection with Smad3 (Fig. 4C). These results demonstrate that in chondrocytes, TGF-β-activated Smad3 is sufficient to repress Runx2-inducible transactivation, specifically of an MMP-13 promoter-reporter construct.
TGF-β-mediated repression and induction of MMP-13 is Runx2-dependent
To determine if Runx2 is necessary for the dynamic regulation of endogenous MMP-13 by TGF-β, Runx2 siRNA was used to reduce Runx2 mRNA in ATDC5 cells to 60% of that in cells infected with a scrambled control siRNA (data not shown). The rapid repression of MMP-13 mRNA and protein expression following 8h of TGF-β was still apparent in control cells, but not in cells infected with siRNA against Runx2 (Fig. 4D, F). Reduction of Runx2 levels was also sufficient to diminish the TGF-β-inducible expression of MMP-13 at 24h (Fig. 4E, G). These results suggest that Runx2 is required for both the rapid repressive and delayed inductive effects of TGF-β on MMP-13 in ATDC5 cells.
Smad3 is essential for TGF-β-mediated repression of MMP-13
To examine the role of Smad3 in the regulation of endogenous MMP-13, ATDC5 cells were infected with lentiviral vectors expressing a Smad3-specific shRNA, which resulted in a 57% reduction in Smad3 mRNA levels relative to cells infected with virus expressing a control shRNA (data not shown). The rapid TGF-β-mediated repression of MMP-13 mRNA and protein expression, apparent in control shRNA expressing cells, was completely lost in cells expressing Smad3 shRNA (Fig. 5A, C). Interestingly, Smad3 shRNA expression did not significantly affect the TGF-β-inducible expression of MMP-13 at later time points (Fig. 5B, D).
To determine if this chondrocyte-intrinsic response corresponded to the increased MMP-13 expression in Col2-Cre;Smad3fl/fl cartilage (Fig. 2E), we examined the regulation of MMP-13 in primary articular chondrocytes from Smad3fl/fl mice. After in vitro infection with adenoviral Cre recombinase (Ad-Cre), Smad3fl/fl primary chondrocytes showed a 90% reduction of Smad3 mRNA relative to cells infected with a GFP-expressing adenovirus (Ad-GFP) (data not shown). As in ATDC5 cells, TGF-β repressed MMP-13 expression within 8h in GFP-infected chondrocytes. Inactivation of Smad3 completely blocked this TGF-β-mediated repression of MMP-13 mRNA and protein (Fig. 5E, G). In Cre-expressing Smad3fl/fl chondrocytes, the TGF-β-inducible expression of MMP-13 at 24h was diminished but intact (Fig. 5F, H). Therefore, TGF-β-activated Smad3 represses Runx2 function to rapidly inhibit MMP-13 expression. At later times, TGF-β induces MMP-13 through Runx2-dependent mechanisms that are more sensitive to the activity of p38 than Smad3 (Fig. 3E, 4E). This differential utilization of Smad and non-Smad pathways by TGF-β is essential for the dynamic regulation of MMP-13 expression and articular cartilage integrity.
Discussion
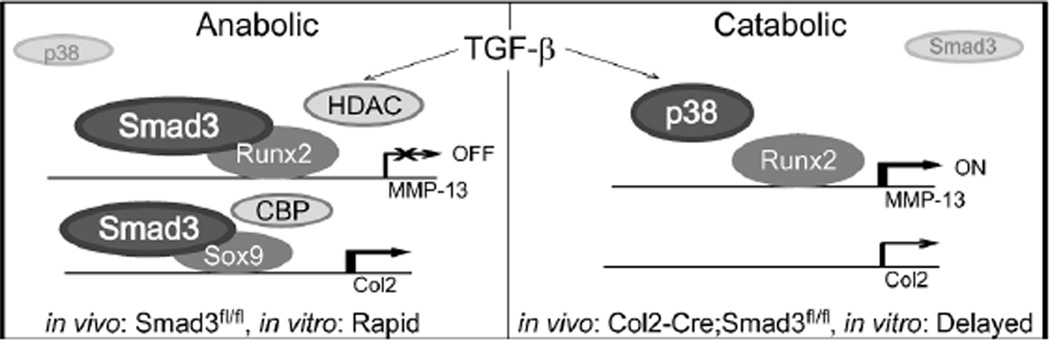
Here we elucidate critical mechanisms by which Smad3 maintains articular cartilage and prevents osteoarthritis. Using Col2-Cre;Smad3fl/fl mice in which chondrocyte, but not perichondrial, levels of Smad3 are reduced, we show that chondrocyte-intrinsic Smad3 is required to induce collagen II expression and to limit MMP-13-mediated articular cartilage matrix degradation. Further, we find that the response of articular chondrocytes to TGF-β is dynamic and can shift from one dominated by Smad3-mediated repression to one dominated by p38-mediated activation of MMP-13 expression (Fig. 6). Accordingly, Smad3-deficiency drives increased expression of MMP-13 protein both in vitro and in vivo, where MMP-13-mediated proteolysis of collagen II and aggrecan advances osteoarthritic cartilage degeneration. By identifying a transcriptional mechanism through which Smad3 represses chondrocyte expression of MMP-13, this study complements and extends the recent finding that human mutations in Smad3 are associated with osteoarthritis (35). Shifting the balance from TGF-β-activation of p38 to Smad3 may enhance the anabolic effects and reduce the catabolic effects of this growth factor, a finding that may have implications for the development of osteoarthritis therapies.
Figure 6. Proposed schematic of TGF-β signaling in articular cartilage.
TGF-β regulation of MMP-13 in articular chondrocytes is dynamic. In vitro, the early response is dominated by Smad3-repression of MMP-13 while the response at later time points is dominated by p38-mediated induction of MMP-13. The mechanisms may involve modulation of lineage-specific transcription factors Sox9 and Runx2, which form transcriptional complexes with CBP and HDACs, as previously reported in chondrocytes (37) and osteoblasts (38). Thus, loss of Smad3 in vivo results in cartilage degradation due to a reduction in Col2 synthesis and an increase in MMP-13-mediated degradation.
These studies of Col2-Cre;Smad3fl/fl mice are consistent with the previously described role of Smad3 in the perichondrium, while elucidating the chondrocyte-intrinsic role of Smad3. Chondrocyte-derived Ihh induces perichondrial TGF-β, which signals locally through Smad2 and Smad3 to induce PTHrP, an inhibitor of hypertrophic differentiation (9–11). Accordingly, the growth plate phenotype of Col2-Cre;Smad3fl/fl mice (Supplementary Fig. 1) in which perichondrial Smad3 is intact, is less severe than that in mice with systemic loss of Smad3 (6). However, the articular cartilage phenotypes of Col2-Cre;Smad3fl/fl and Smad3ex8/ex8 mice are similar in severity and timing. Although the 60% inhibition of Smad3 in the mice is likely insufficient to ablate canonical TGF-β signaling through Smad3, the pathway is crucial since even a partial loss of function disrupts chondrocyte homeostasis. We find that the degeneration of Smad3-deficient articular cartilage results from impaired anabolic activity and increased cartilage degradation. Col2-Cre;Smad3fl/fl chondrocytes synthesize less collagen II and express more of the collagen- and aggrecan-degrading enzyme MMP-13. Though MMP-13 protein expression was consistently increased in the superficial zone of articular cartilage, MMP-13 mRNA regulation was not statistically affected by Smad3 deficiency in vivo as it was in vitro. The highly variable expression of MMP-13 in Col2-Cre;Smad3fl/fl cartilage does suggest that Smad3 is required to maintain stable MMP-13 expression, a result that is consistent with the reported variability in MMP-13 expression in arthritic human articular cartilage (36). Therefore, our results demonstrate a key chondrocyte-intrinsic role for Smad3 that is independent of its perichondrial role, particularly in the maintenance of post-natal articular cartilage.
Both the anabolic and catabolic defects in Col2-Cre;Smad3fl/fl cartilage may be attributed to the role of Smad3 in modulating the activity of lineage-specific transcription factors in chondrocytes. The chondrogenic transcription factor Sox9 recruits Smad3 to the Col2 promoter where they cooperatively induce CBP/p300-mediated transactivation (37). In vitro, we show that a functional interaction of Smad3 with another lineage-specific transcription factor, Runx2, is required for repression of MMP-13 in chondrocytes. In osteoblasts, Smad3-mediated repression of Runx2 was sufficient to repress both Runx2 expression and function by recruiting class II histone deacetylases, HDAC4 and HDAC5, to repress Runx2-mediated transactivation (20, 38). HDAC4 can repress MMP-13 expression in osteoblasts (39) and likely plays the same role in articular chondrocytes. HDAC4-deficient mice exhibit increased Runx2 expression and activity in the growth plate and premature growth plate chondrocyte hypertrophy (40). Premature hypertrophy was also observed in Smad3-deficient mice and mice that overexpress Runx2 in chondrocytes (6, 41). Although these studies focused on the growth plate, articular cartilage degeneration was observed in mice that overexpress Smurf2 in chondrocytes, a defect that was attributed to lower levels of functional Smad3 in these cells (7). Smad3-mediated repression of Runx2 in chondrocytes is also likely responsible for the regulation of collagen X, another Runx2-inducible gene expressed in hypertrophic chondrocytes that is inhibited by TGF-β in a Smad3-dependent manner (16, 42–45). Together with our findings, these studies collectively suggest that baseline TGF-β signaling maintains articular cartilage by preventing the inappropriate expression of Runx2-inducible genes in articular chondrocytes through an HDAC4- and Smad3-dependent mechanism.
TGF-β both represses and induces MMP-13 expression in osteoblasts (18, 19) and in chondrocytes as shown here. In osteoblasts, Smad3 and p38 cooperate to induce MMP-13 expression. Though Smad3 may also contribute to the TGF-β-mediated induction of MMP-13 at 24 h, this induction is much less sensitive to the level of Smad3 than the TGF-β-mediated repression (Fig. 6). The mechanisms by which the MMP-13 response to TGF-β shifts from Smad3-mediated repression to p38-mediated activation remain unknown. A number of mechanisms have the potential to switch TGF-β from a Smad3-mediated repressing signal to an activating one. Interestingly, several of these possible mechanisms have also been implicated in chondrocyte differentiation or osteoarthritis. For example, TGF-β signals through two type I receptors, Alk1 and Alk5. Alk5 activates Smad2/3 whereas Alk1 signals through Smads 1, 5, and 8, which induce MMP-13 expression. In osteoarthritis, the balance shifts to Alk1/Smad1/5/8-mediated signaling because arthritic chondrocytes express higher relative levels of Alk1 (46), as well as of endoglin, a protein that enhances TGF-β mediated signaling through Alk1 (47). We hypothesized that Gadd45β, another protein that is overexpressed in arthritic chondrocytes, may act as a switch since it was rapidly induced by TGF-β in ATDC5 cells (data not shown) and is known to activate MMP-13 expression (48). However, siRNA ablation of Gadd45β did not prevent the shift from TGF-β-mediated repression to activation of MMP-13 at 48h (data not shown). Another attractive candidate is Zfp521, a PTHrP-inducible transcriptional coregulator that, like Smad3, associates with HDAC4 and Runx2 to repress hypertrophic gene expression (49). Given the important role of MMP-13 in cartilage degeneration, there is great motivation to better understand and control the mechanisms responsible for shifting cellular sensitivity to TGF-β signaling through Smad3 and non-Smad3 pathways.
Understanding mechanisms of TGF-β activity in chondrocytes may provide new targets for therapeutic strategies to treat osteoarthritis and other skeletal diseases. TGF-β has multiple effects on several joint tissues that can both promote and deter osteoarthritis progression (5). Selective manipulation of one arm of the TGF-β pathway may allow optimization of these effects to promote chondrocyte stability and matrix deposition. In addition to controlling cell differentiation and matrix synthesis, TGF-β may also affect the physical properties of cartilage matrix. In bone, TGF-β regulates ECM stiffness through a Smad3- and Runx2-dependent pathway (15, 50). Since this pathway also operates in chondrocytes, TGF-β may regulate cartilage ECM stiffness, which changes in osteoarthritis. Further dissection of mechanisms responsible for the beneficial and deleterious effects of TGF-β may enhance control of the biological and physical changes that accompany arthritic cartilage degeneration.
Supplementary Material
Acknowledgments
This research was supported by the Arthritis Foundation Hulda Irene Duggan Arthritis Investigator Award and NIH-NIDCR R01 DE019284 (TA) and NIH-NIDCR COHORT T32 Training Grant (CC). We thank C. Weber, D. Nguyen, E. Berthet, D. Zhang and E. Liebenberg for technical support. We thank S.A. Pangas and J.M. Graff for the Smad3fl/fl mice, J.S. Mort for the VDIPEN and GPQG antibodies, W. Chang for the Col2-Cre mice, H. J. Im for the -370 MMP-13-Luc construct, and M.B. Goldring for helpful discussion and critical input.
References
- 1.Goldring MB, Marcu KB. Cartilage homeostasis in health and rheumatic diseases. Arthritis Res Ther. 2009;11(3):224. doi: 10.1186/ar2592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aigner T, Vornehm SI, Zeiler G, Dudhia J, von der Mark K, Bayliss MT. Suppression of cartilage matrix gene expression in upper zone chondrocytes of osteoarthritic cartilage. Arthritis Rheum. 1997;40(3):562–569. doi: 10.1002/art.1780400323. [DOI] [PubMed] [Google Scholar]
- 3.Shlopov BV, Lie WR, Mainardi CL, Cole AA, Chubinskaya S, Hasty KA. Osteoarthritic lesions: involvement of three different collagenases. Arthritis Rheum. 1997;40(11):2065–2074. doi: 10.1002/art.1780401120. [DOI] [PubMed] [Google Scholar]
- 4.Mitchell PG, Magna HA, Reeves LM, Lopresti-Morrow LL, Yocum SA, Rosner PJ, et al. Cloning, expression, and type II collagenolytic activity of matrix metalloproteinase-13 from human osteoarthritic cartilage. J Clin Invest. 1996;97(3):761–768. doi: 10.1172/JCI118475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blaney Davidson EN, van der Kraan PM, van den Berg WB. TGF-beta and osteoarthritis. Osteoarthritis Cartilage. 2007;15(6):597–604. doi: 10.1016/j.joca.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 6.Yang X, Chen L, Xu X, Li C, Huang C, Deng CX. TGF-beta/Smad3 signals repress chondrocyte hypertrophic differentiation and are required for maintaining articular cartilage. J Cell Biol. 2001;153(1):35–46. doi: 10.1083/jcb.153.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu Q, Kim KO, Sampson ER, Chen D, Awad H, O'Brien T, et al. Induction of an osteoarthritis-like phenotype and degradation of phosphorylated Smad3 by Smurf2 in transgenic mice. Arthritis Rheum. 2008;58(10):3132–3144. doi: 10.1002/art.23946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Valdes AM, Spector TD, Tamm A, Kisand K, Doherty SA, Dennison EM, et al. Genetic variation in the SMAD3 gene is associated with hip and knee osteoarthritis. Arthritis Rheum. 2010;62(8):2347–2352. doi: 10.1002/art.27530. [DOI] [PubMed] [Google Scholar]
- 9.Alvarez J, Sohn P, Zeng X, Doetschman T, Robbins DJ, Serra R. TGFbeta2 mediates the effects of hedgehog on hypertrophic differentiation and PTHrP expression. Development. 2002;129(8):1913–1924. doi: 10.1242/dev.129.8.1913. [DOI] [PubMed] [Google Scholar]
- 10.Serra R, Karaplis A, Sohn P. Parathyroid hormone-related peptide (PTHrP)-dependent and -independent effects of transforming growth factor beta (TGF-beta) on endochondral bone formation. J Cell Biol. 1999;145(4):783–794. doi: 10.1083/jcb.145.4.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alvarez J, Serra R. Unique and redundant roles of Smad3 in TGF-beta-mediated regulation of long bone development in organ culture. Dev Dyn. 2004;230(4):685–699. doi: 10.1002/dvdy.20100. [DOI] [PubMed] [Google Scholar]
- 12.Ashcroft GS, Yang X, Glick AB, Weinstein M, Letterio JL, Mizel DE, et al. Mice lacking Smad3 show accelerated wound healing and an impaired local inflammatory response. Nat Cell Biol. 1999;1(5):260–266. doi: 10.1038/12971. [DOI] [PubMed] [Google Scholar]
- 13.Zhu Y, Richardson JA, Parada LF, Graff JM. Smad3 mutant mice develop metastatic colorectal cancer. Cell. 1998;94(6):703–714. doi: 10.1016/s0092-8674(00)81730-4. [DOI] [PubMed] [Google Scholar]
- 14.Tomic D, Miller KP, Kenny HA, Woodruff TK, Hoyer P, Flaws JA. Ovarian follicle development requires Smad3. Mol Endocrinol. 2004;18(9):2224–2240. doi: 10.1210/me.2003-0414. [DOI] [PubMed] [Google Scholar]
- 15.Balooch G, Balooch M, Nalla RK, Schilling S, Filvaroff EH, Marshall GW, et al. TGF-beta regulates the mechanical properties and composition of bone matrix. Proc Natl Acad Sci U S A. 2005;102(52):18813–18818. doi: 10.1073/pnas.0507417102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ferguson CM, Schwarz EM, Reynolds PR, Puzas JE, Rosier RN, O'Keefe RJ. Smad2 and 3 mediate transforming growth factor-beta1-induced inhibition of chondrocyte maturation. Endocrinology. 2000;141(12):4728–4735. doi: 10.1210/endo.141.12.7848. [DOI] [PubMed] [Google Scholar]
- 17.Selvamurugan N, Kwok S, Partridge NC. Smad3 interacts with JunB and Cbfa1/Runx2 for transforming growth factor-beta1-stimulated collagenase-3 expression in human breast cancer cells. J Biol Chem. 2004;279(26):27764–27773. doi: 10.1074/jbc.M312870200. [DOI] [PubMed] [Google Scholar]
- 18.Selvamurugan N, Kwok S, Alliston T, Reiss M, Partridge NC. Transforming growth factor-beta 1 regulation of collagenase-3 expression in osteoblastic cells by cross-talk between the Smad and MAPK signaling pathways and their components, Smad2 and Runx2. J Biol Chem. 2004;279(18):19327–19334. doi: 10.1074/jbc.M314048200. [DOI] [PubMed] [Google Scholar]
- 19.Rydziel S, Varghese S, Canalis E. Transforming growth factor beta1 inhibits collagenase 3 expression by transcriptional and post-transcriptional mechanisms in osteoblast cultures. J Cell Physiol. 1997;170(2):145–152. doi: 10.1002/(SICI)1097-4652(199702)170:2<145::AID-JCP6>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 20.Alliston T, Choy L, Ducy P, Karsenty G, Derynck R. TGF-beta-induced repression of CBFA1 by Smad3 decreases cbfa1 and osteocalcin expression and inhibits osteoblast differentiation. EMBO J. 2001;20(9):2254–2272. doi: 10.1093/emboj/20.9.2254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ovchinnikov DA, Deng JM, Ogunrinu G, Behringer RR. Col2a1-directed expression of Cre recombinase in differentiating chondrocytes in transgenic mice. Genesis. 2000;26(2):145–146. [PubMed] [Google Scholar]
- 22.Li Q, Pangas SA, Jorgez CJ, Graff JM, Weinstein M, Matzuk MM. Redundant roles of SMAD2 and SMAD3 in ovarian granulosa cells in vivo. Mol Cell Biol. 2008;28(23):7001–7011. doi: 10.1128/MCB.00732-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu L, Flahiff CM, Waldman BA, Wu D, Olsen BR, Setton LA, et al. Osteoarthritis-like changes and decreased mechanical function of articular cartilage in the joints of mice with the chondrodysplasia gene (cho) Arthritis Rheum. 2003;48(9):2509–2518. doi: 10.1002/art.11233. [DOI] [PubMed] [Google Scholar]
- 24.Shibata S, Fukada K, Suzuki S, Ogawa T, Yamashita Y. Histochemical localisation of versican, aggrecan and hyaluronan in the developing condylar cartilage of the fetal rat mandible. J Anat. 2001;198(Pt 2):129–135. doi: 10.1046/j.1469-7580.2001.19820129.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Singer II, Kawka DW, Bayne EK, Donatelli SA, Weidner JR, Williams HR, et al. VDIPEN, a metalloproteinase-generated neoepitope, is induced and immunolocalized in articular cartilage during inflammatory arthritis. J Clin Invest. 1995;95(5):2178–2186. doi: 10.1172/JCI117907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Billinghurst RC, Dahlberg L, Ionescu M, Reiner A, Bourne R, Rorabeck C, et al. Enhanced cleavage of type II collagen by collagenases in osteoarthritic articular cartilage. J Clin Invest. 1997;99(7):1534–1545. doi: 10.1172/JCI119316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thirion S, Berenbaum F. Culture and phenotyping of chondrocytes in primary culture. Methods Mol Med. 2004;100:1–14. doi: 10.1385/1-59259-810-2:001. [DOI] [PubMed] [Google Scholar]
- 28.Suter SE, Gouthro TA, McSweeney PA, Nash RA, Haskins ME, Felsburg PJ, et al. Optimized transduction of canine paediatric CD34(+) cells using an MSCV-based bicistronic vector. Vet Res Commun. 2006;30(8):881–901. doi: 10.1007/s11259-006-3356-7. [DOI] [PubMed] [Google Scholar]
- 29.Ducy P, Karsenty G. Two distinct osteoblast-specific cis-acting elements control expression of a mouse osteocalcin gene. Mol Cell Biol. 1995;15(4):1858–1869. doi: 10.1128/mcb.15.4.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carcamo J, Zentella A, Massague J. Disruption of transforming growth factor beta signaling by a mutation that prevents transphosphorylation within the receptor complex. Mol Cell Biol. 1995;15(3):1573–1581. doi: 10.1128/mcb.15.3.1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Im HJ, Pacione C, Chubinskaya S, Van Wijnen AJ, Sun Y, Loeser RF. Inhibitory effects of insulin-like growth factor-1 and osteogenic protein-1 on fibronectin fragment- and interleukin-1beta-stimulated matrix metalloproteinase-13 expression in human chondrocytes. J Biol Chem. 2003;278(28):25386–25394. doi: 10.1074/jbc.M302048200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Feng XH, Filvaroff EH, Derynck R. Transforming growth factor-beta (TGF-beta)-induced down-regulation of cyclin A expression requires a functional TGF-beta receptor complex. Characterization of chimeric and truncated type I and type II receptors. J Biol Chem. 1995;270(41):24237–24245. doi: 10.1074/jbc.270.41.24237. [DOI] [PubMed] [Google Scholar]
- 33.Fosang AJ, Last K, Knauper V, Murphy G, Neame PJ. Degradation of cartilage aggrecan by collagenase-3 (MMP-13) FEBS Lett. 1996;380(1–2):17–20. doi: 10.1016/0014-5793(95)01539-6. [DOI] [PubMed] [Google Scholar]
- 34.Jimenez MJ, Balbin M, Lopez JM, Alvarez J, Komori T, Lopez-Otin C. Collagenase 3 is a target of Cbfa1, a transcription factor of the runt gene family involved in bone formation. Mol Cell Biol. 1999;19(6):4431–4442. doi: 10.1128/mcb.19.6.4431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.van de Laar IM, Oldenburg RA, Pals G, Roos-Hesselink JW, de Graaf BM, Verhagen JM, et al. Mutations in SMAD3 cause a syndromic form of aortic aneurysms and dissections with early-onset osteoarthritis. Nat Genet. 2011;43(2):121–126. doi: 10.1038/ng.744. [DOI] [PubMed] [Google Scholar]
- 36.Tardif G, Pelletier JP, Dupuis M, Geng C, Cloutier JM, Martel-Pelletier J. Collagenase 3 production by human osteoarthritic chondrocytes in response to growth factors and cytokines is a function of the physiologic state of the cells. Arthritis Rheum. 1999;42(6):1147–1158. doi: 10.1002/1529-0131(199906)42:6<1147::AID-ANR11>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 37.Furumatsu T, Tsuda M, Taniguchi N, Tajima Y, Asahara H. Smad3 induces chondrogenesis through the activation of SOX9 via CREB-binding protein/p300 recruitment. J Biol Chem. 2005;280(9):8343–8350. doi: 10.1074/jbc.M413913200. [DOI] [PubMed] [Google Scholar]
- 38.Kang JS, Alliston T, Delston R, Derynck R. Repression of Runx2 function by TGF-beta through recruitment of class II histone deacetylases by Smad3. EMBO J. 2005;24(14):2543–2555. doi: 10.1038/sj.emboj.7600729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shimizu E, Selvamurugan N, Westendorf JJ, Olson EN, Partridge NC. HDAC4 represses matrix metalloproteinase-13 transcription in osteoblastic cells, and parathyroid hormone controls this repression. J Biol Chem. 2010;285(13):9616–9626. doi: 10.1074/jbc.M109.094862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vega RB, Matsuda K, Oh J, Barbosa AC, Yang X, Meadows E, et al. Histone deacetylase 4 controls chondrocyte hypertrophy during skeletogenesis. Cell. 2004;119(4):555–566. doi: 10.1016/j.cell.2004.10.024. [DOI] [PubMed] [Google Scholar]
- 41.Takeda S, Bonnamy JP, Owen MJ, Ducy P, Karsenty G. Continuous expression of Cbfa1 in nonhypertrophic chondrocytes uncovers its ability to induce hypertrophic chondrocyte differentiation and partially rescues Cbfa1-deficient mice. Genes Dev. 2001;15(4):467–481. doi: 10.1101/gad.845101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li F, Lu Y, Ding M, Napierala D, Abbassi S, Chen Y, et al. RUNX2 contributes to murine COL10A1 gene regulation through direct interaction with its cis-enhancer. J Bone Miner Res. 2011 doi: 10.1002/jbmr.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zheng Q, Zhou G, Morello R, Chen Y, Garcia-Rojas X, Lee B. Type X collagen gene regulation by Runx2 contributes directly to its hypertrophic chondrocyte-specific expression in vivo. J Cell Biol. 2003;162(5):833–842. doi: 10.1083/jcb.200211089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dong YF, Soung do Y, Schwarz EM, O'Keefe RJ, Drissi H. Wnt induction of chondrocyte hypertrophy through the Runx2 transcription factor. J Cell Physiol. 2006;208(1):77–86. doi: 10.1002/jcp.20656. [DOI] [PubMed] [Google Scholar]
- 45.Li TF, Darowish M, Zuscik MJ, Chen D, Schwarz EM, Rosier RN, et al. Smad3-deficient chondrocytes have enhanced BMP signaling and accelerated differentiation. J Bone Miner Res. 2006;21(1):4–16. doi: 10.1359/JBMR.050911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Blaney Davidson EN, Remst DF, Vitters EL, van Beuningen HM, Blom AB, Goumans MJ, et al. Increase in ALK1/ALK5 ratio as a cause for elevated MMP-13 expression in osteoarthritis in humans and mice. J Immunol. 2009;182(12):7937–7945. doi: 10.4049/jimmunol.0803991. [DOI] [PubMed] [Google Scholar]
- 47.Finnson KW, Parker WL, Chi Y, Hoemann CD, Goldring MB, Antoniou J, et al. Endoglin differentially regulates TGF-beta-induced Smad2/3 and Smad1/5 signalling and its expression correlates with extracellular matrix production and cellular differentiation state in human chondrocytes. Osteoarthritis Cartilage. 2010;18(11):1518–1527. doi: 10.1016/j.joca.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 48.Ijiri K, Zerbini LF, Peng H, Correa RG, Lu B, Walsh N, et al. A novel role for GADD45beta as a mediator of MMP-13 gene expression during chondrocyte terminal differentiation. J Biol Chem. 2005;280(46):38544–38555. doi: 10.1074/jbc.M504202200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Correa D, Hesse E, Seriwatanachai D, Kiviranta R, Saito H, Yamana K, et al. Zfp521 is a target gene and key effector of parathyroid hormone-related peptide signaling in growth plate chondrocytes. Dev Cell. 2010;19(4):533–546. doi: 10.1016/j.devcel.2010.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chang JL, Brauer DS, Johnson J, Chen CG, Akil O, Balooch G, et al. Tissue-specific calibration of extracellular matrix material properties by transforming growth factor-beta and Runx2 in bone is required for hearing. EMBO Rep. 2010;11(10):765–771. doi: 10.1038/embor.2010.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.