Abstract
Background: An epidermoid cyst is a common epithelial-lined cyst. There have been many studies on epidermoid cysts, but few focused on ruptured epidermoid cyst and its histopathologic characteristics. Objective: We evaluated the histopathologic differences between ruptured and unruptured epidermoid cysts, and their relationships. Methods: We retrospectively examined 359 excision biopsy specimen diagnosed as epidermoid cyst from 1991 to 2011 at Department of dermatology at Daegu Catholic University Hospital. Results: The mean cyst area was 38.89 mm2 and the mean cyst area of the unruptured group was larger than that of the ruptured group. The mean wall thickness was 90.15 μm and was thicker in ruptured group than in unruptured group. The correlation between cyst diameter and wall thickness had statistically negative correlation in unruptured and in ruptured group. In ruptured group, the cystic size of the cases with rete ridge was smaller than that of without rete ridge. The cyst wall thickness of the cases with rete ridge was thicker than that of the cases without rete ridge. Limitations: For comparative evaluation of sizes, randomly shaped cysts are assumed to be perfectly elliptic. And only those with more than 3/4 cystic wall remaining were included in the subject. Conclusion: When comparing the ruptured and the unruptured cyst, the rupture of cyst had significant relationship with increased cyst diameter and area, increased wall thickness, more cyst contents, and more wall changes. Moreover, the presence of rete ridge in ruptured cystic wall is a valuable variable to recognize the duration of the rupture.
Keywords: Epidermal cyst, epidermoid cyst, histopathologic comparison, rete rigde, ruptued epidermoid cyst, unruptued epidermoid cyst
Introduction
An epidermoid cyst is a common keratin-filled epithelial-lined cyst and often occurring in face, scalp, and trunk. Clinically, epidermoid cyst occurs in dermis or subcutaneous tissue as a movable nodule with central punctum. If the epidermoid cyst ruptures and causes foreign body reaction or inflammation, it is difficult to treat with a simple complete resection due to the wider extent of adherence or damage to the surrounding tissues. The mainstay of the treatment of ruptured epidermoid cysts is the use of antibiotics or anti-inflammatory agents to reduce the size of the lesion combined with surgical scraping of the damaged tissue, instead of removing by total excision. However, this method has high recurrence rate and is costly [1].
There have been many studies on epidermoid cysts, but few focused on ruptured epidermoid cyst and its histopathologic characteristics. Identifying its histopathologic features would help its treatment and be used as a reference of further epidermoid cyst study. Therefore, we studied histostructural differences of ruptured and unruptured epidermoid cysts for 21 years, from 1991 to 2011 in the department of pathology at the Catholic University of Daegu, Daegu, South Korea.
Materials and methods
The histopathology of 359 cases diagnosed as epidermoid cyst with excision biopsy at the department of dermatology, Daegu Catholic Medical Center from 1991 to 2011 was evaluated retrospectively. Rupture of cyst was defined as loss of continuity of cyst wall accompanied by inflammatory cell infiltration, keratin granuloma, or giant cell. Preliminary study was performed on the samples of all subjects using existing Hematoxylin & Eosin (H&E) stained tissue samples. Based on the results of the preliminary study, subjects with loss of more than 1/4 of the epidermoid cystic wall due to severe extent of rupture or inflammation and thus were unable to be used in the comparative study were excluded. And further exclusions were cases with uncertain diagnosis and insufficient data.
The institutional review board of Daegu Catholic University medical center approved this study.
Histopathologic analysis
Microscopic examinations of the serial sections at 1 mm interval were performed on all the remaining 359 cases of epidermoid cysts using an optical microscope (Olympus Bh-2). A ×10 ocular lens (Olympus whk 10x/201) was used with the microscope for the measurements of the walls and diameters of the cysts. The cyst diameter and the cystic wall thickness were determined based on the measurements from the slice of the largest cyst among the serial sections. The cystic wall thickness was measured from the base of the cystic wall up to the granular layer and the final value was determined by taking four measurements at right angle at the measurable locations and calculating the mean value of the two measurements excluding the maximum and the minimum values. The cyst diameter was measured by taking the measurement of the major axis and of the minor axes at right angle to the major axis and calculating the mean value of the two measurements. Cyst area was calculated from the elliptical area of the cyst from one end of the cystic wall granular layer to the granular layer on the opposite end (Figure 1).
Figure 1.
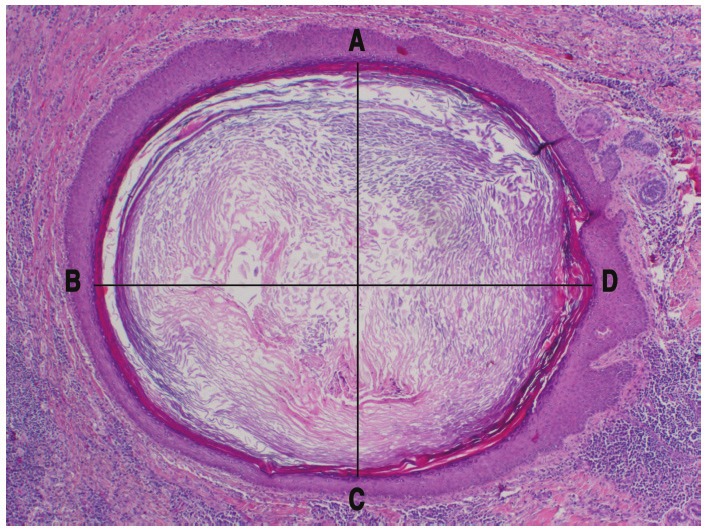
Cyst’s diameter was measured at the mean value between line AC and line BD (H&E, ×20).
Statistical analysis
Data analyses were performed using statistical software program: SPSS 13.0 (SPSS Inc, Chicago, IL). The significance level of the statistical difference was verified with Chi-square test and t-test. A P value less than 0.05 were considered statistically significant in all cases (rounded up to second decimal place). Positive or negative correlation was determined using Pearson’s correlation analysis.
Results
Of the 359 biopsy specimen investigated, 256 cases were unruptured and 103 cases were ruptured. The mean diameter of the investigated epidermoid cysts was 5.50 mm for all groups, 5.84 mm for unruptured cyst group, and 4.64 mm for ruptured cyst group showing significantly greater cysts in diameter in unruptured cyst group. Comparison of two-dimensional area of the subject histological cyst samples calculated based on the maximum diameter of the sample and the diameter perpendicular to it revealed that the overall mean value was 38.89 mm2. The mean value of the unruptured cyst group was 42.70 mm2 and the ruptured cyst group was 29.42 mm2. The area of unruptured cyst group was significantly greater than the ruptured one. The overall mean value of cystic wall thickness was 90.15 μm, with the mean value of the unruptured cyst group being 71.21 μm and the mean value of the ruptured cyst group being 137.23 μm, showing significantly thicker wall in the ruptured cyst group (Table 1). Correlation between the diameter and the thickness of the cysts in the ruptured and unruptured cyst groups was analyzed. As the results, the diameter and the thickness of the cysts had negative correlation in both ruptured and unruptured cyst groups, indicating that the larger the size of the cyst, the thinner the wall thickness. The correlation coefficient was -0.125 for unruptured cyst group and -0.198 for ruptured cyst group showing no significant inter-group difference (Figure 3).
Table 1.
Comparison of ruptured group and unruptured group by cyst diameter, cyst area, and thickness of wall
| Unruptured | Ruptured | Total | Significance (p-value) | |
|---|---|---|---|---|
| Cyst diameter (mm) | 5.84±3.24 | 4.64±3.14 | 5.50±3.25 | 0.002 |
| Cyst area (mm2) | 42.70±48.79 | 29.42±38.96 | 38.89±46.52* | 0.014 |
| Thickness of wall (μm) | 71.21±64.17 | 137.23±104.72 | 90.15±83.38† | 0.000 |
The mean cyst area was 38.89 mm2 and the mean cyst area of the unruptured group was wider than it of the ruptured group (P<0.05);
The mean wall thickness was 0.09mm and the mean wall thickness of ruptured group was thicker than it of the unruptured group(P<0.05).
Figure 3.
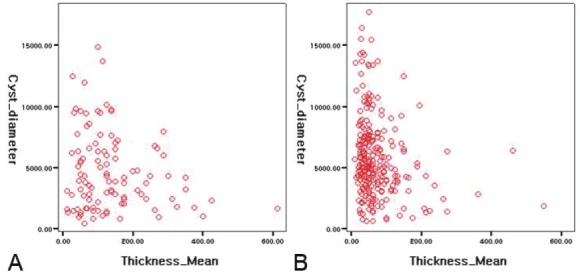
Scatter diagram of cyst diameter and wall thickness of ruptured cysts (A) and unruptured cysts (B).
The ruptured cyst group was further divided into sub-groups with or without rete ridge (Figure 4) and the diameter and the area of the cyst and the cystic wall thickness were compared with those of unruptured cyst group, and results showed that the cyst diameter was 5.23 mm in the ruptured cyst without rete ridge subgroup and 3.40 mm in the ruptured cyst with rete ridge sub-group, showing significant intergroup difference. The result of the comparison between the unruptured cyst group and the ruptured cyst with rete ridge sub-group also showed significant difference. However, the result of comparison between the unruptured cyst group and the ruptured cyst without rete ridge sub-group did not show significant difference. The cyst area was 36.34 mm2 in the ruptured cyst without rete ridge sub-group and 14.75 mm2 in the ruptured cyst with rete ridge sub-group and only the results of comparison between the unruptured cyst group and the ruptured cyst with rete ridge did not show significant difference. The cystic wall thickness was 102.60 μm in the ruptured cyst without rete ridge sub-group and 210.68 μm in the ruptured cyst with rete ridge sub-group and both of the ruptured cyst sub-groups with and without rete ridge showed significantly thicker cystic wall thickness (P<0.05). When the same was compared between the ruptured cyst with rete ridge sub-group and the ruptured cyst without rete ridge sub-group, the ruptured cyst with rete ridge sub-group showed significantly thicker cystic wall (P<0.05) (Table 2).
Figure 4.
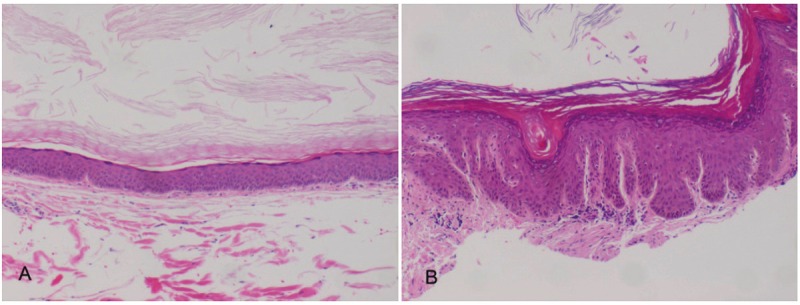
Two types of ruptured cystic wall. A. Without rete ridge type (H&E, ×40). B. With rete ridge type (H&E, ×40).
Table 2.
Comparison among unruptured cyst group, ruptured group without rete ridge, and ruptured group with rete ridge by cyst diameter, cyst area, and thickness of wall
| Parameters | Unruptured (n=256) | Ruptured | Significance (p-value) | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Rete ridge(-) (n=70) | Rete ridge(+) (n=33) | a | b | c | ||
| Cyst diameter (mm) | 5.84±3.24 | 5.23±3.37 | 3.40±2.15 | 0.168 | 0.000 | 0.001 |
| Cyst area (mm2) | 42.70±48.79 | 36.34±43.63 | 14.75±20.18 | 0.323 | 0.000 | 0.001 |
| Thickness of wall (μm) | 71.21±64.17 | 102.60±67.05 | 210.68±130.68 | 0.000 | 0.000 | 0.000 |
a: Unruptured group vs rete ridge(-) ruptured group, b: Unruptured group vs rete ridge(+) ruptured group, c: Rete ridge(-) ruptured group vs rete ridge(+) ruptured group. The mean cyst area of ruptured group with rete ridge showed difference with unruptured group (P<0.05), whereas the ruptured group without rete ridge did not show difference (P>0.05).
Cystic contents such as abscess, parakeratotic cells, red blood cells, pilomatricoma-like change, giant cells, cholesterol clefts, bacterial colonies as well as keratinous materials were observed (Table 3). Microscopic observation showed that, compared with the unruptured cyst group, the ruptured cyst group had statistically more cases of containing abscess, parakeratotic cells and red blood cells giant cells (Figure 2A) or pilomatricoma-like cells in the cyst (Figure 2B). Other observed changes were not statistically significant due to insufficiency of the number of case. Histopathologic changes of cystic walls were hyperplasia, hypergranulosis, microabscess, parakeratosis, necrotic change, verrucous change, exocytosis, atrophy, dyskeratosis, eosinophilic inclusion cyst and vacuolation (Table 4). Compared with the unruptured cyst group, the ruptured cyst group showed statistically larger number of the manifestations of hyperplasia, hypergranulosis, microabscess, parakeratosis (Figure 2B), necrotic change, verrucous change and exocytosis, but did not show significant difference in other changes.
Table 3.
Contents of cyst in unruptured and ruptured cyst
| Content of cyst | Unruptured (n=256) | Ruptured (n=103) | Total (%) | Significance p-value/OR* |
|---|---|---|---|---|
| Abscess | 4 | 29 | 33 (34.7) | 0.000/25.127 |
| Parakeratotic cell | 10 | 15 | 25 (26.3) | 0.000/4.259 |
| RBC | 1 | 10 | 11 (11.6) | 0.000/27.826 |
| Pilomatricomal like change‡ | 4 | 7 | 11 (11.6) | 0.009/4.661 |
| Multinucleated giant cell | 1 | 7 | 8 (8.4) | 0.000/18.863 |
| Cholesterol cleft | 1 | 2 | 3 (3.2) | - |
| Bacterial colonies | 0 | 1 | 1 (1.1) | - |
| Others† | 2 | 1 | 3 (3.2) | - |
OR: odd ratio;
Uniform basaloid cells with shallow cells that exhibit an imprint of a nucleus that has been lost;
Others: other pathologic remarks (include spores, ghost cells, dyskeratotic cells).
Figure 2.
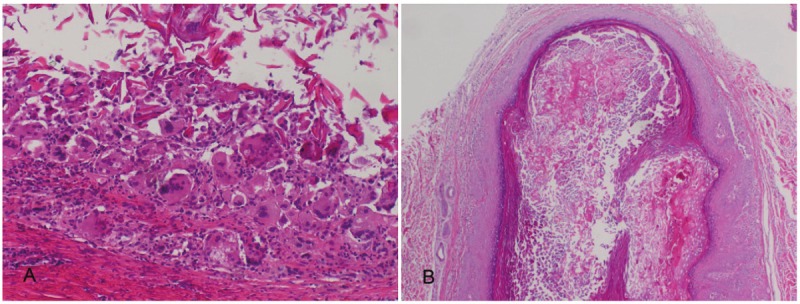
A. Giant cells in the cyst (H&E, ×100). B. A pilomatricoma-like changes (H&E, ×40).
Table 4.
Comparison of unruptured group and ruptured group by wall changes
| Wall change | Unruptured (n=256) | Ruptured (n=103) | Total (%) | p-value |
|---|---|---|---|---|
| Hyperplasia | 26 | 49 | 75 (29.5) | 0.000 |
| Hypergranulosis | 25 | 19 | 44 (17.3) | 0.020 |
| Microabscess | 6 | 21 | 27 (10.6) | 0.000 |
| Parakeratosis | 7 | 11 | 18 (7.1) | 0.002 |
| Necrotic change | 2 | 14 | 16 (6.3) | 0.000 |
| Verrucous change | 12 | 2 | 14 (5.5) | 0.232 |
| Exocytosis | 1 | 13 | 14 (5.5) | 0.000 |
| Atrophy | 6 | 6 | 12 (4.7) | 0.092 |
| Dyskeratosis | 7 | 3 | 10 (3.9) | 0.910 |
| Eosinophilic inclusion cyst | 2 | 6 | 8 (3.1) | 0.003 |
| Vacuolation | 3 | 3 | 6 (2.4) | 0.237 |
| Others* | 7 | 3 | 10 (3.9) | 0.910 |
Others: other pathologic remarks (include keratin cleft, small cystic change, koilocyte like change, giant cell granuloma, bowen like change).
Discussion
Epidermoid cysts are the most common of the cysts. They are formed by several proposed mechanisms such as proliferation of ectodermal remnant during embryogenesis, plugging of pilosebaceous units, or traumatic implantation of epithelial cells [1]. Histopathologically, they are lined by stratified epithelium, which is identical in structure to the epidermis and expresses the same cytokeratin profiles as the follicular infundibulum [1,2]. Some authors suggest that it originates from follicular infundibulum, and thus also called infundibular cyst [3].
Epidermoid cysts are usually asymptomatic. But if they rupture, several findings such as suppuration, foreign body granulomatous reaction, and granulation tissue [2] can be observed. Comparison of manifestations in each group revealed observations of more various histopathologic findings including inflammation in the ruptured cyst group than in the unruptured cyst group. The contents of the cysts in the ruptured cyst group included more abscess, parakeratotic cells, red blood cells, giant cells and pilomatricoma-like cells than in the unruptured cyst group. The pilomatricoma in association with epidermoid cyst was reported several times. Some authors thought that pilomatricoma-like change in epidermoid cyst is related to Gardner’s syndrome [4-6] In this case 11 cases with pilomatricoma like cell were observed but none of them were related to Gardner’s syndrome. Observation of the cystic wall also revealed more various manifestations of changes including hyperplasia, hypergranulosis, microabscess, parakeratosis, necrotic change, verrucous change and exocytosis, which were observed more in the ruptured cyst group than in the unruptured cyst group. The findings about previous reported proliferation of epidermoid cyst wall were also observed in this study [2]. Most of these manifestations were inflammation-related and observed more in ruptured group. Previous radiologic studies showed similar findings [7-9] but it is not clear whether the cause of inflammation such as bacterial infection was involved in the rupture or they were the secondary inflammatory reaction after the rupture. Therefore, further studies on inflammation in epidermoid cysts are necessary.
The thickness and the size of epidermoid cysts were measured for ruptured and unruptured cysts. Only few attempts have been made using this approach perhaps because structural elements of the epidermoid cysts are difficult to reconstruct into 3-dimensional structure from 2-dimensional microscopic images. In order to address these problems, we attempted microscopic observations of serial sections and performed measurements based on the values from the largest diameter section. Microscopic measurements showed significantly greater diameter and area of the cysts in unruptured cyst group than in ruptured cyst group. The mean cystic wall thickness was 71.21 μm in the unruptured cyst group and 137.23 μm in the ruptured cyst group, which means, compared with average epidermal thickness 100 μm, the cystic wall thickness in the unruptured cyst group was smaller than the average epidermal thickness whereas that in the ruptured cyst group was greater than the average epidermal thickness [10,11], the cystic wall thickness in the ruptured cyst group being thicker than that in the unruptured cyst group with statistical significance (Table 1). The diameter and the average area of cysts are relatively smaller in the ruptured cyst group than in the unruptured cyst group, perhaps because the overall size of the cyst is reduced as the result of internal cystic rupture. However, the fact that the cystic wall thickness in the ruptured cyst group is greater than that in the unruptured cyst group conflicts with the natural assumption that rupture can more easily occur when the cystic wall is thinner [12]. We believe that the reason for the observed results is because, in the ruptured cyst group, cystic rupture causes inflammation due to foreign-body reaction to the cystic contents and released many transmitters including growth factors then affect the proliferation of the cystic wall cells [13].
Correlation between the diameter and the thickness of the cysts was investigated and results showed negative correlation in both ruptured and unruptured cyst groups, indicating that the larger the size of the cyst, the thinner the wall thickness, which is considered because increased contents of the epidermoid cyst caused its size and internal pressure to increase which, in turn, cased the cystic wall to become thinner influencing the occurrence of rupture [12] (Figure 3).
From these results, it can be deduced that, in order for the epidermoid cyst to rupture it should grow bigger and its wall thinner. However, we interpreted the fact that the ruptured cyst group had thicker cystic wall than unruptured group in this study seems to be considered as a secondary result. In other words, the cystic wall thickness in the ruptured cyst group should be similar to that of the unruptured cyst group in the early post-rupture stage and if so, it can hypothesized that the cystic wall thickness of both group may be similar in early period of the rupture, but as time passes, it may show different feature between each group. However, some authors suggest that the rete ridge formation in epidermoid cyst wall is due to repeated inflammation. Therefore in this study, we divided the ruptured cyst group into those showed rete ridges in its wall and others without (Figure 4). The cysts with rete ridges had shorter diameter and smaller area and greater wall thickness than those without. The ruptured cyst without rete ridge sub-group did not show statistically significant differences in the diameter and the area of the cysts compared with the unruptured cyst group and the cystic wall thickness was greater in the subgroup with rete ridges than the one without. Difference could also be observed between the ruptured cyst sub-groups with and without rete ridges. In the cases without rete ridges, no significant difference could be observed between the ruptured and unruptured cyst groups, suggesting that, during the early post-rupture stage, the structure of ruptured epidermoid cyst is similar to that of unruptured epidermoid cysts. Also the finding of rete ridge in the ruptured epidermoid cystic wall could reliably suggest that some time has passed after the rupture.
As described above, histostructural approach to various factors that influence epidermoid cystic rupture were found to have problems in that; all samples must be prepared into sequential sections to overcome the limitation of 2-dimensional microscopic examinations; 3-dimensional size of cysts have to be evaluated by comparing the cystic diameter and area of cysts, instead of cystic volume; for comparative evaluation of sizes, randomly shaped cysts are assumed to be perfectly elliptic; and only those with more than 3/4 cystic wall remaining were included in the subject. However, we endeavored to find statistic standards by using increased number of cases and we believe we succeeded to compensate the limitation to some extent.
In conclusion, according to the results of investigation on various causes of epidermoid cyst and the difference between ruptured and unruptured cysts, the ruptured epidermoid cysts showed differences in their thickness and area, contents, and changes in cystic wall, compared with unruptured cysts. The manifestation of rete ridge in the cystic wall is an indicator of the duration of the existence of epidermoid cystic rupture.
Furthermore, the histostructural approach and the results of this study could be used as a reference of other epidermoid cyst study. Further prospective studies on various topics about epidermoid cystic rupture and structure based on this study will be necessary.
Acknowledgement
We are grateful to Hyun Chung, MD, PhD, Dong Hoon Shin, MD, PhD, and Jae Bok Park, MD, PhD for critical pathologic review. We appreciate In Soo Chae, MD and In Yong Kim, MD for statistically analysis.
References
- 1.Thomas VD, Swanson NA, Lee KK. Benign epithelial tumors, harmatomas, and hyperplasias. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick’s dermatology in general medicine. 7th ed. New York, NY: McGraw-Hill; 2008. pp. 1054–1067. [Google Scholar]
- 2.Vicente J, Vázquez-Doval FJ. Proliferations of the epidermoid cyst wall. Int J Dermatol. 1998;37:181–185. doi: 10.1046/j.1365-4362.1998.00361.x. [DOI] [PubMed] [Google Scholar]
- 3.Ackerman BA, Reddy VB, Soyer HP. Neoplasms with follicular differentiation. 2nd ed. New York, NY: Ardor Scribendi; 2001. [Google Scholar]
- 4.Cooper PH, Fechner RE. Pilomatricoma-like changes in the epidermal cysts of Gardner’s syndrome. J Am Acad Dermatol. 1983;8:639–644. doi: 10.1016/s0190-9622(83)70071-x. [DOI] [PubMed] [Google Scholar]
- 5.Benharroch D, Sacks MI. Pilomatricoma associated with epidermal cyst. J Cutan Pathol. 1989;16:40–43. doi: 10.1111/j.1600-0560.1989.tb00006.x. [DOI] [PubMed] [Google Scholar]
- 6.Pujani M, Agarwal S, Goyal RK, Jyotsna PL, Tejwani N, Rautela A. Pilomatricoma coexistent with epidermal cyst. Int J Dermatol. 2012;51:624–625. doi: 10.1111/j.1365-4632.2010.04618.x. [DOI] [PubMed] [Google Scholar]
- 7.Yuan WH, Hsu HC, Lai YC, Chou YH, Li AF. Differences in sonographic features of ruptured and unruptured epidermal cyst. J Ultrasound Med. 2012;31:265–272. doi: 10.7863/jum.2012.31.2.265. [DOI] [PubMed] [Google Scholar]
- 8.Jin W, Ryu KN, Kim GY, Kim HC, Lee JH, Park JS. Sonographic findings of ruptured epidermal inclusion cysts in superficial soft tissue: emphasis on shapes, pericystic changes, and pericystic vascularity. J Ultrasound Med. 2008;27:171–176. doi: 10.7863/jum.2008.27.2.171. quiz 177-178. [DOI] [PubMed] [Google Scholar]
- 9.Hong SH, Chung HW, Choi JY, Koh YH, Choi JA, Kang HS. MRI findings of subcutaneous epidermal cysts: emphasis on the presence of rupture. Am J Roentgenol. 2006;186:961–966. doi: 10.2214/AJR.05.0044. [DOI] [PubMed] [Google Scholar]
- 10.Sandby-Møller J, Poulsen T, Wulf HC. Epidermal Thickness at Different Body Sites: Relationship to Age, Gender, Pigmentation, Blood Content, Skin Type and Smoking, Habits. Acta Derm Venereol. 2003;83:410–413. doi: 10.1080/00015550310015419. [DOI] [PubMed] [Google Scholar]
- 11.McGrath JA, Uitto J. Anatomy and organization of human skin. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook’s textbook of dermatology. 8th ed. Singapore: Wiley-Blackwell; 2010. pp. 3.1–3.5. [Google Scholar]
- 12.Woo MJ, Park JS, Chung H, Kim SW, Park JB. Pigmentation degree and thickness of the epidermal cyst in Korean. Korean Journal of Investigative Dermatology. 2003;10:27–33. [Google Scholar]
- 13.Takematsu H, Terui T, Torinuki W, Tagami H. Leukocyte chemotactic properties of soluble horny contents in epidermal cysts. Arch Dermatol Res. 1987;279:449–453. doi: 10.1007/BF00412590. [DOI] [PubMed] [Google Scholar]


