Abstract
Introduction:
acute respiratory failure is manifested clinically as patient with variable degrees of respiratory distress, but characteristically an abnormal arterial blood partial pressure of oxygen or carbon dioxide. The application of mechanical ventilation in this setting can be life saving.
Goals:
The aim of this study is to evaluate the effects of two recruitment maneuvers not only on oxygenation, but on aeration of the lung as well. For that purpose chest x ray and thoracic computed tomography scan (CT) of the lung were used as safe and objective methods for evaluation the impact of recruitment maneuvers on aeration of the lung. CT scan and chest x ray were performed before recruitment maneuvers as confirmation of diagnose and one day after the last recruitment maneuvers.
Material and methods:
Sixty patients who met ar DS criteria of the american european consensus conference were included in this study. This study was conducted in iCU in our hospital between november 2009 and December 2011. Patients were orally intubated, sedated with 0, 2-0, 4 μg/kg /min and midazolam 4 mg/h, and ventilated with evita 2 Dura ventilator (Dragger germany). According to the recom-mendation of the Consensus Conference of the american College of Chest physician all patients had an arterial catheter and cen-tral venous catheter. Hemodynamic data were collected from Data Ohmeda monitors. Gas analyses were mesured from blood samples taken from arteria radialis. Partial pressure of oxygen of mixed blood was messured from blood sample taken from v jugularis interior. We used arterial blood colection syringe Bd preset, and blood samples were analyzed with aVl 995HB blood gas analiser.
Results:
Hemodynamic changes: there wasn’t any differences in heart rate, and mean arterial blood pressure before the recruitment five minutes and sixty minutes after the recruitment in both groups. respiratory mechanics: Highest values of the compliance are achived during the recruitment manouver in both groups. There was better improvment in compliance during the e sigh recruitment maneouver, then in Cpap recruitment maneouver. There was improvement in chest X ray in both groups. 93,4% of patients in the Cpap group and 96,7% in e sigh group. CT scan: in Cpap group there were 8 patients with focal changes and 22 patients with diffusse changes. in e sigh group 29 patients had diffuse changes of the lung and one patient had focal changes. We noticed that there was better improvment in aeration in patients with diffuse changes of the lung 96.7% in e sigh group and 73,3% in Cpapgroup. In patient with focal changes there was improvment in 26,7% in e sigh group and 3,3% in Cpap group. We noticed that there was better improvmnet in aeration in patients with diffuse changes than in patients with focal changes. E sigh maneuver had better impact on aeration of the lung then Cpap recruitment maneuver.
Conclusion:
In our study we proved that e sigh recruitment maneuvers better improved oxygenation in arterial blood than Cpap recruitment maneuver. Repetative e sigh manouvers proved to be essential for arDS patients. They reopened collapsed alveolli and improved aeration of the lung which was confirmed by X ray and CT scan as an objective methods for verification of lung condition.
Key words: acute respiratory failure, respiratory distress, repetitive recruitment maneuvers.
1. INTRODUCTION
Acute respiratory failure is manifested clinically as patient with variable degrees of respiratory distress, but characteristically an abnormal arterial blood partial pressure of oxygen or carbon dioxide. The application of mechanical ventilation in this setting can be life saving (1). Acute respiratory distress syndrome is characterized with acute lung inflammation, with increased vascular permeability. There are bilateral widespread infiltrates on X-ray, PaO2/FiO2ratio is < 40 k Pa, and pulmonary arterial wedge pressure is less than 2,5kPa (PAWP < 2,5kPa) (2). By definition ARDS is lung permeability edema, which means that alveolar are not collapsed but liquid filled (3). Reduction of tidal volume and plateau pressure (Pplat) < 35 cm H2O and adequate positive end expiratory pressure to improve oxygenation , FiO2< 0,5 is recommended for the ventilatory management of ARDS (4, 5). It is well known that reduction in tidal volume promotes a decrease in lung aeration (6, 7). Several studies recommend the adjunction of recruitment maneuvers to mechanical ventilation to limit alveolar derecruitment induced by low tidal volume (8, 9, 10, 11). During ongoing management of ALI/ARDS, a lung recruitment maneuvers requires briefly increasing of the alveolar pressure to a level above that recommended, in order to aerate lung units filled with edema or inflammatory cells. Recruitment is a physiological process that reopens previously gas less lung units exposed to positive pressure ventilation (12)..Until now there are lot of studies that evaluated effects of extended sigh (e sigh) and continuous positive airway pressure (CPAP) recruitment maneuvers not only on gas exchanges but on respiratory mechanics as well (13, 14. 15, 16, 17, 18).
2. GOAL OF STUDY
The aim of this study is to evaluate the effects of two recruitment maneuvers not only on oxygenation, but on aeration of the lung as well. For that purpose chest x ray and thoracic computed tomography scan (CT) of the lung were used as safe and objective methods for evaluation the impact of recruitment maneuvers on aeration of the lung. CT scan and chest x ray were performed before recruitment maneuvers as confirmation of diagnose and one day after the last recruitment maneuvers. We established that the last recruitment maneuver would be considered the maneuver after which two consecutive gas analysis (the first one will be taken at 7 h , and the last one at 19h) would fulfill these criteria : PaO2> 12,9 k Pa and PaO2/FiO2 > 40 k Pa.
3. MATERIALS AND METHODS
Sixty patients who met ARDS criteria of the American European consensus conference (2) were included in this study. This study was conducted in ICU in our hospital between November 2009 and December 2011. Exclusion criteria were age under eighteen years, chronic respiratory insufficiency, chronic obstructive pulmonary disease, asthma, restrictive respiratory insufficiency, bronchoplaeural fistula, intracranial hypertension, and hemodynamic instability despite support therapy. Patients were orally intubated, sedated with 0, 2-0, 4 μg/kg /min and midazolam 4 mg/h, and ventilated with Evita 2 Dura ventilator (Dragger Germany)according to the recommendation of the Consensus Conference of the American College of Chest Physician (19). All patients had an arterial catheter and central venous catheter. Hemodynamic data were collected from Data Ohmeda monitors.
Gas analyses were mesured from blood samples taken from arteria radialis. Partial pressure of oxygen of mixed blood was messured from blood sample taken from v jugularis interior. We used arterial blood colection syringe Bd preset, and blood samples were analyzed with AVL 995HB blood gas analiser. Patients were ventilated in volume control ventilation with tidel volume (Vt) 6ml/kg and respiratory rate was 12 respiration per minute. Positive end expiratory pressure (PEEP) and fraction of inspired oxygen (FiO2) were set to obtain partial pressure of carbon dioxid (PaCO2) equal or less then 6,13kPa. We continously monitored compliance, tidel volume,respiratory rate, plateau pressure,paek airway pressure on the display of Evita 2 Dura ventilators (Drager Germany). The image of pressure volume curves were obtained under quasi static conditions during mechanical ventilation (20).
An invastigator who was responsable for the collection of the data and statistical analyses was blinded in respect of the protocol.
Before the RM, hemodynamic status of the patient was checked. Noninvasive blood pressure, puls and electrocardiogram (EKG) were monitored on Data Ohmeda monitors. If fluid adminstartion or vasopresors were not enough for hemodynamic stabilty, we didn’t start recruitment manouver. Patients were ventilated in zero end expiratory pressure (ZEEP) for five minutes. Compliance of the lung was recorded and lower inflaction point (LIP and uper inflaction point (UIP) were established on the pressure–volume curve of the ventilator. Then we proceeded with recruitment maneuvers.
3.1. Recruitment manouvers
Group 1. The continous positive airway pressure (CPAP) recruitment maneuver: The ventilator was set to CPAP mode with pressure of 35 cm H2O applied for 35 seconds. After that patients were ventilated in baseline values.
Group 2. Extended sigh manouver: Positive end expiratory pressure (PEEP) was 10 cm H2O above LIP was applied for 15 minutes. Patients were on volume control ventilation. If plato pressure was higher then upper inflaction point or higher then 35 cm H2O, we decreased tidel volume. During the recruitment manouver maximum peak pressure was limited to 50 cm H2O. In case of severe hemodynamic instabilti (systolic pressure <70mmHg, heart rate < 50 breaths per minute, hypoxemia SpO2<80%) recruitment maneuver was immediately stopped.
Before recruitment maneuvers (time 1) five minutes (time 2); and one hour (time3) after the recruitment maneuvers we colected data from: a) hemodynamic parametars: heart rate, mean arterial pressure (MAP), EKG; b) gas analyzes taken from blood samples from a. radialis partial pressureof oxygen (PaO2), partial pressure of carbon dioksid (PaCO2), saturation of oxygen (sat O2) and partial pressure of oxygen in intern jugular vein (SjVO2). PaO2/FiO2ratio was mathematically established; c) respiratory mechanics were read from the display of the ventilator: compliance, platau pressure (p plat), peak airway pressure (p peak), positive end expiratory pressure (PEEP). Lower inflaction point (LIP) and upper inflaction point (UIP) were read on pressure – volume curve (21, 22, 23, 24).
Two chest x ray films were taken during this study. The first one was before we started with recruitment maneuvers. We were looking for presence of intense parenchimal opafication (focal or homogeneous increase in density). The extent of these changes were scored 0 none, 1- focal, 2-diffuse. We were looking for signs of pneumothorax, pneumo-mediastinum, as a assessment of saftly perfomed reccruitment manover. Thesecond chest x ray was taken one day after the last recruitment maneuver. Thoracic computed tomography scan was taken before recruitment maneuvers and one day after the last recruitment maneuver.
Thoracic computed tomography scan procedure (CT): Lung scaning was performed in supine position from apex to the diaphragm by Ge Bright Speed Elite General Elektrik (Ge) USA. All images were observed at a window width of 1600 Hounsfield units(HU) and a window level of 600 HU .The exposures were taken without contrast materials. By protocol CT was performed before RM at zero PEEP and one day after the last RM when gas analysis of the patients fulfilled this criteria: PaO2> 12,9 k Pa and PaO2/FiO2 > 40 k Pa. During the CT scan we monitored: puls oxymetry, electrokardiogram and blood pressure.If there was hemodinamic instability or periferal saturation (SpO2), was ≤85% we stopped the procedure. Qualitative assessment of lung were performed by a applying CT scan ARDS criteria: focal loss of aeration, diffuse loss of aeration and patchy loss of aeration (25).
3.2. Statistical analysis
All data are expressed as mean and standard deviation. Baseline clinical and ventilator data are compared by student t-test for parametric data and Mann-Whitney U test for nonparametric data. Kolmogorov Smirnov test was used for verification of normal distribution of quantative data. The statistical significance level eas fixed at 0.05.
4. RESULTS
The mean values of PaO2, SpO2, PaO2/FiO2 ratio, SjVO2, O2 sat heart rate and mean arterial pressure are shown at Table 1. The highest value PaO2, SpO2, PaO2/FiO2 ratio, SjVO2, O2 sat was achieved five minutes after the recruitment maneuvers in both groups. There is significant difference in PaO2 PaO2/FiO2 ratio, O2 saturation before the recruitment maneuvers and after recruitment maneuvers (p=0.0000) (Table 3). The lowest mean value of PaCO2 in e sigh group was achieved one hour after the RM .In CPAP group, the lowest value was achieved 5 minutes after the RM. Acording to the post hoc Turkey HSD, both recruitment maneuvers had positive impact on PaO2, PaO2/FiO2,O2 saturation SpO2, not only five minutes afer the recruitment maneuvers, but also sixty minutes after the recruitment maneuvers (p=0.000). We used Mann-Whitney U test (Table 3) to compare the imapact of two recruitment manouvers on gas exchage in three measuring points. For partial presure of oxygen (PaO2) five minutes after the recruitment manouvers there wasn’t any differences bteween two groups. One hour after the recruitments, extended sigh had better impact on PaO2 comparing to values in CPAP group p=0.007. Extended sigh also had better impact on PaO2/FiO2 ratio (p=o. ooooo) peripheral saturation of oxygen (SpO2) and saturation of oxygen in mixed blood (sjVO2) five minutes and one hour after the recruitment maneuver. There wasn’t significant differences for oxygen saturation in arterial blood sample (O2 sat) and partial pressure of oxygen taken from blood sample of jugulair vein (SjVO2) between two groups.
Table 1.
Mean minimum,and maximum values and standard deviation for gas analyses in three time points. t1 before recruitment maneuver t2 five minutes after the recruitment maneuver, t3 one hour after the recruitment maneuver
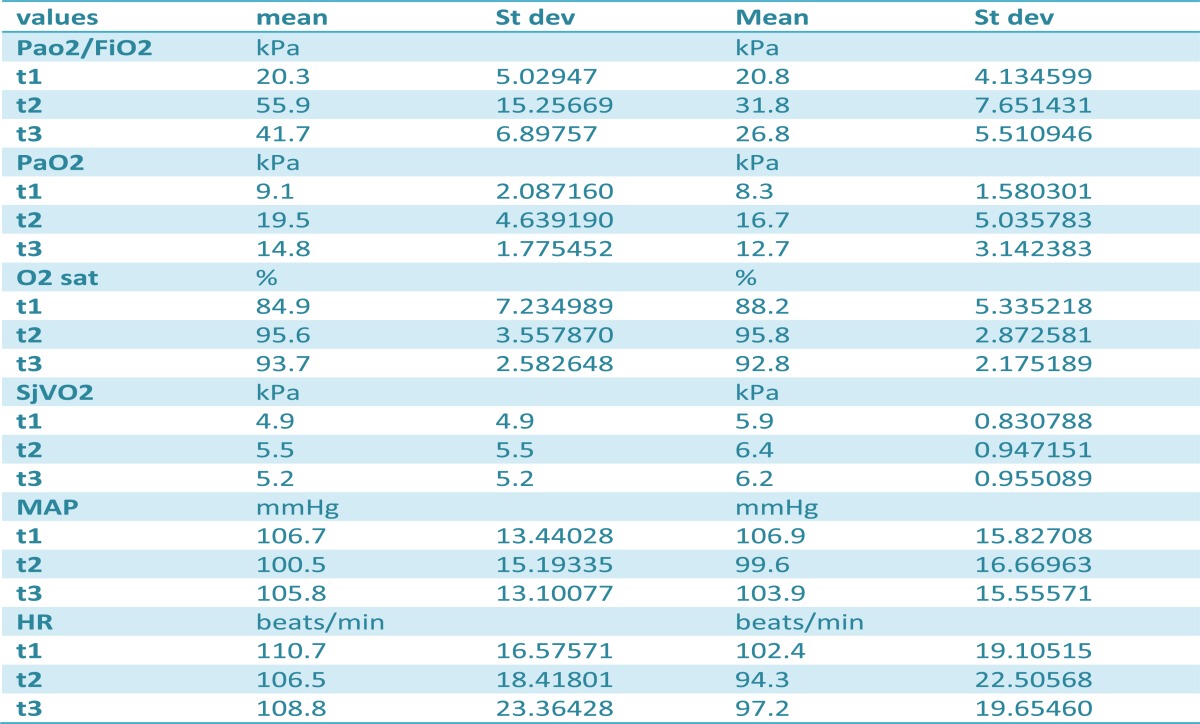 |
Table 3.
Analysis of variance ANOVA test
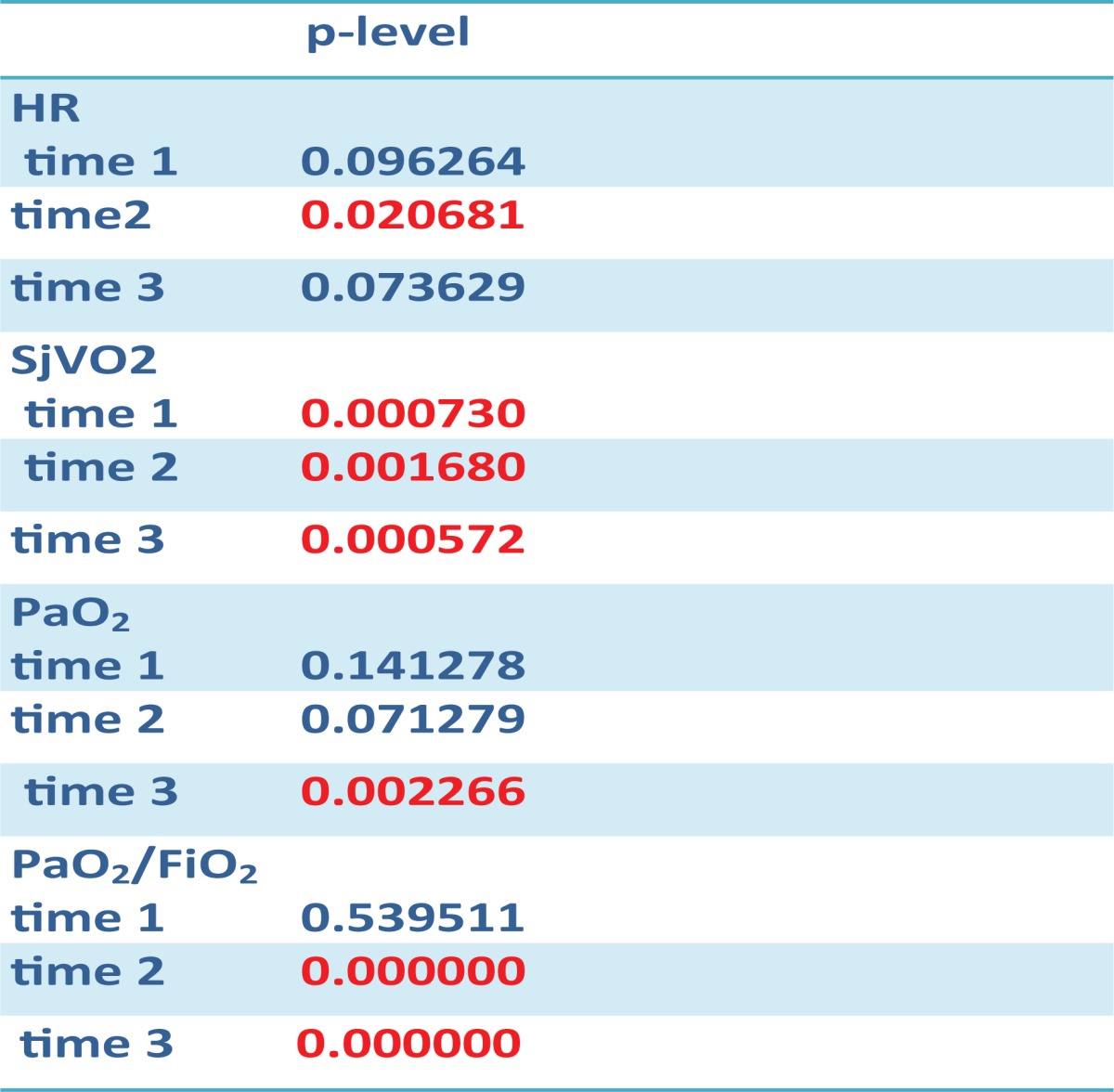 |
Hemodynamic changes: There wasn’t any differences in heart rate, and mean arterial blood pressure before the recruitment five minutes and sixty minutes after the recruitment in both groups.
Respiratory mechanics: Highest values of the compliance are achived during the recruitment manouver in both groups. There was better improvment in compliance during the e sigh recruitment maneouver,then in CPAP recruitment maneouver (Table 2).
Table 2.
Mean, minimum maximum values of Tidel volume, Peak Pressure, Positive endexpiratory pressure(PEEP), plato pressure, compliance, before and during recruitment manouver (mean, minimum, maximum values and standard deviation). t1 before recruitment, t2 during the recruitment
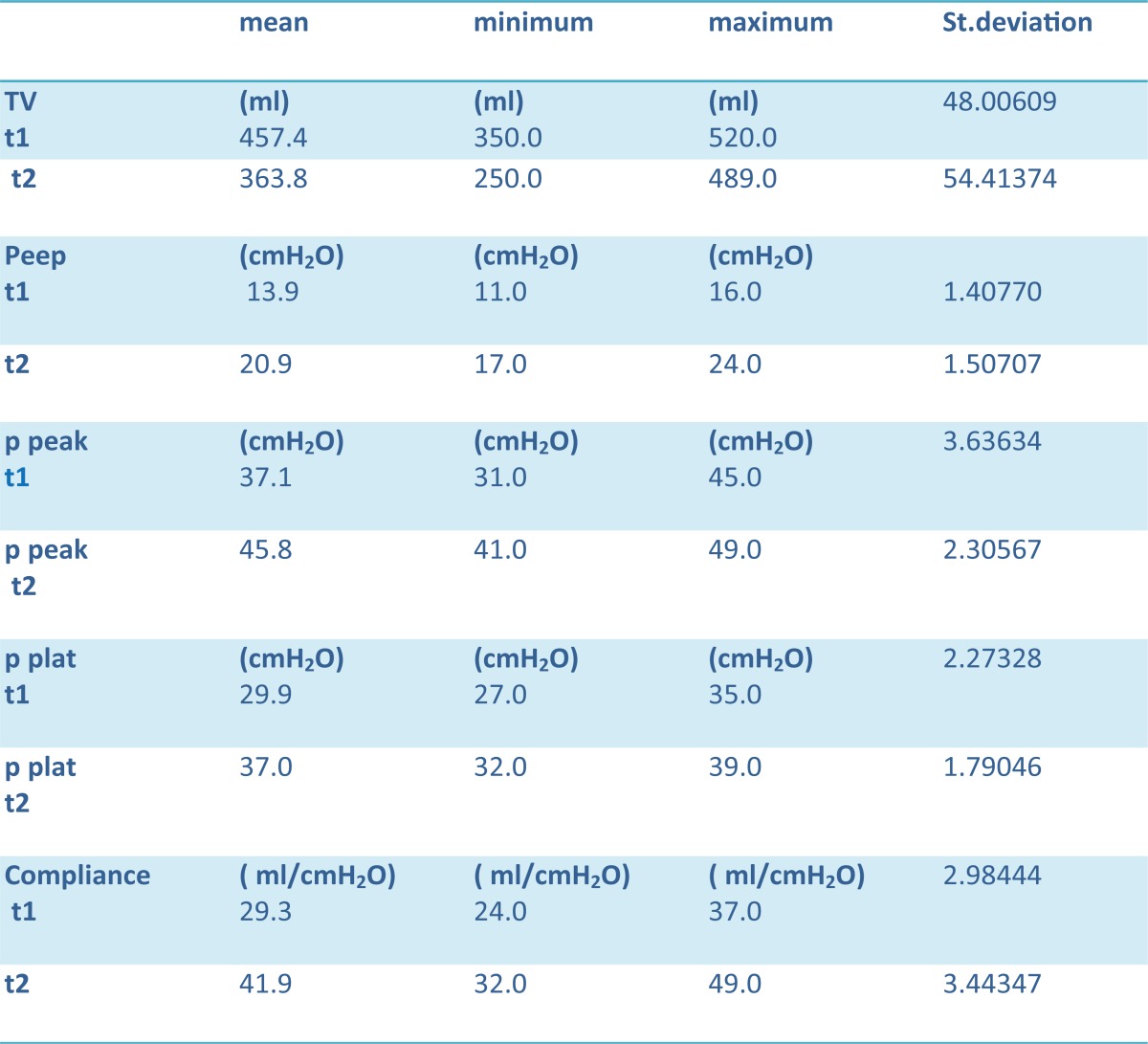 |
There was improvement in chest x ray in both groups. 93,4% of patients in the CPAP group and 96,7% in e sigh group. CT scan: In CPAP group there were 8 patients with focal changes and 22 patients with diffusse changes. In e sigh group 29 patients had diffuse changes of the lung and one patient had focal changes. We noticed that there was better improvment in aeration in patients with diffuse changes of the lung 96.7% in e sigh group and 73,3% in CPAP group. In patient with focal changes there was improvment in 26,7% in e sigh group and 3,3% in CPAP group. We noticed that there was better improvmnet in aeration in patients with diffuse changes than in patients with focal changes. E sigh maneuver had better impact on aeration of the lung then CPAP recruitment maneuver.
5. DISCUSSION
In our study we proved that e sigh recruitment maneuver improved arterial oxygenatin. Partial pressure of oxygen(PaO2) and oxygen saturation (O2 sat) in arterial blood showed better results in e sigh recruitment maneuvers. Partial pressure of oxygen in vena jugularis interna (SjVO2) was also improved but there was not statistical differences in SjVO2 before and after the recruitment maneuvers. Compliance of lung was also better improved during the e sigh recruitment maneuvers RM.
Lim and al. (27) used e sigh as recruitment maneuvers. He gradualy reduced tidal volumes from 8 to 2 ml/kg and increased PEEP from 10 to 25 cmH2O. When PEEP of 25 cm H2O was reached, CPAP of 30 cm-H2O was applied for 30 seconds. This was a succssessful manouver, oxigenation was incresed and patients were hemidinamically stabile. Lots of authors (11, 17, 19) showed that e sigh was safe and efficiant method for improvment in oxygenation. Constantin et al. (28) compared two recruitment maneuvers, e sigh with PEEP 10 cm H2O above LIP for 15 minutes and CPAP 40 cmH2O for 40 seconds.
Both manouvers approved oxygenation but CPAP was assossiated with hemodynamic instability. Khaled M Mahmoud and Amany S Ammar (28) also proved that extended sigh was more effective in oxygenation of the patients then CPAP. In study of Pellosi (29) was shown that conventional e sigh improved oxygenatian but the effect of improvment was limited untill the discoutinuation. Lapinsky et al. (30) applied inflation manouver using 45 cm H2O or the peak pressure at he tidel volume at the tidel volume of 12ml/kg which was lower.
The manouver was applied for 20 seconds. Improvment in oxygenation occured in 10 minutes. No barotrauma nor nor complications were recoreded. Five patient developed hypotension and mild oxygen desaturation.
6. CONCLUSION
In our study we proved that e sigh recruitment maneuvers better improved oxygenation in arterial blood than CPAP recruitment maneuver. Repetative e sigh manouvers proved to be essential for ARDS patients. They reopened collapsed alveolli and improved aeration of the lung which was confirmed by x ray and CT scan as an objective methods for verification of lung condition.
Conflict of interest
None declared.
REFERENCES
- 1.Donahoe M. Basic ventilator management: Lung protective Strategies. Surg Clin N Am. 2006;86:1389–1408. doi: 10.1016/j.suc.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 2.Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994 Mar;149(3 Pt 1):818–824. doi: 10.1164/ajrccm.149.3.7509706. [DOI] [PubMed] [Google Scholar]
- 3.Guerin C, Debord S, Leray V, Delannoy B, Bayle F, Bourdin G, Jean-Cristophe Richard. Efficacy and safety of recruitment maneuvers in acute respiratory distress syndrome. Annals of Intensive care. 2011;1:9. doi: 10.1186/2110-5820-1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wolthuis EK, Veelo DP, Choi G, Determann RM, Korevaar JC, Spronk PE, Kuiper MA, Schultz MJ. Mechanical ventilation with-lower tidal volumes does not influence the prescription of opioids or sedatives. Crit Care. 2007;11:R77. doi: 10.1186/cc5969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Villar J, Kacmarek RM, Perez-Mendez L, Aguirre-Jaime A. A highpositive end-expiratory pressure, low tidal volume ventilatorystrategy improves outcome in persistent acute respiratory distress syndrome: a randomized, controlled trial. Crit Care Med. 2006;34:1311–1331. doi: 10.1097/01.CCM.0000215598.84885.01. [DOI] [PubMed] [Google Scholar]
- 6.Richard JC, Maggiore SM, Jonson B, Mancebo J, Lemaire F, Brochard L. Influence of tidal volume on alveolar recruitment. Respective role of PEEP and a recruitment maneuver. Am J Respir Crit Care Med. 2001;163:1609–1613. doi: 10.1164/ajrccm.163.7.2004215. [DOI] [PubMed] [Google Scholar]
- 7.Lapinsky SE, Mehta S. Bench-to-bedside review: Recruitment and recruiting maneuvers. Crit Care. 2005;9:60–65. doi: 10.1186/cc2934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rouby JJ, Lu Q. Bench-to-bedside review: Adjuncts to mechanical ventilation in patients with acute lung injury. Crit Care. 2005;9:465–471. doi: 10.1186/cc3763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barbas CS, de Mattos GF, Borges Eda R. Recruitment maneuvers and positive end-expiratory pressure/tidal ventilation titration in acute lung injury/acute respiratory distress syndrome: translating experimental results to clinical practice. Crit Care. 2005;9:424–426. doi: 10.1186/cc3800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gaver DP, Samsel RW, Solway J. Effects of mechIcal ventilation in patients with acute lung injury. Crit Care. 2005;9:465–471. doi: 10.1186/cc3763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barbas CS, de Mattos GF, Borges Eda R. Recruitment maneuversand positive end-expiratory pressure/tidal ventilation titration in acute lung injury/acute respiratory distress syndrome: translating experimental results to clinical practice. Crit Care. 2005;9:424–426. doi: 10.1186/cc3800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Medoff BD, Harris RS, Kesselman H, Venegas J, Amato MB, Hess D. Use of recruitment maneuvers and high-positive end-expiratory pressure in a patient with acute respiratory distress syndrome. Crit Care Med. 2000;28:1210–1216. doi: 10.1097/00003246-200004000-00051. [DOI] [PubMed] [Google Scholar]
- 13.Riva DR, Contador RS, Baez-Garcia CS, Xisto DG, Cagido VR, Martini SV, et al. Recruitment maneuver: RAMP versus CPAP pressure profile in a model of acute lung injury. Respir Physiol Neurobiol. 2009;169:62–68. doi: 10.1016/j.resp.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 14.Rothen HU, Neumann P, Berglund JE, Valtysson J, Magnusson A, Hedenstierna G. Dynamics of re-expansion of atelectasis during general anaesthesia. Br J Anaesth. 1999;82:551–556. doi: 10.1093/bja/82.4.551. [DOI] [PubMed] [Google Scholar]
- 15.Pelosi P, Bottino N, Chiumello D, Caironi P, Panigada M, Gamberoni C, et al. Sigh in supine and prone position during acute respiratory distress syndrome. Am J Respir Crit Care Med. 2003;167:521–527. doi: 10.1164/rccm.200203-198OC. [DOI] [PubMed] [Google Scholar]
- 16.Lapinsky SE, Aubin M, Mehta S, Boiteau P, Slutsky AS. Safety and efficacy of a sustained inflation for alveolar recruitment in adults with respiratory failure. Intensive Care Med. 1999;25:1297–1301. doi: 10.1007/s001340051061. [DOI] [PubMed] [Google Scholar]
- 17.Lim CM, Koh Y, Park W, Chin JY, Shim TS, Lee SD, et al. Mechanistic scheme and effect of “extended sigh” as a recruitment maneuver in patients with acute respiratory distress syndrome: A preliminary study. Crit Care Med. 2001;29:1255–1260. doi: 10.1097/00003246-200106000-00037. [DOI] [PubMed] [Google Scholar]
- 18.Rodriguez L, Marquer B, Mardrus P, Molenat F, Le Grand JL, Reboul M, et al. A new simple method to perform pressure-volume curves obtained under quasi-static conditions during mechanical ventilation. Intensive Care Med. 1999;25:173–179. doi: 10.1007/s001340050812. [DOI] [PubMed] [Google Scholar]
- 19.Ware LB, Matthay MA. The acute respiratory distress syndrome. N Engl J Med. 2000 May 4;342(18):1334–1349. doi: 10.1056/NEJM200005043421806. [DOI] [PubMed] [Google Scholar]
- 20.Rodriguez L, Marquer B, Mardrus P, Molenat F, Le Grand JL, Reboul M, et al. A new simple method to perform pressure-volume curves obtained under quasi-static conditions during mechanical ventilation. Intensive Care Med. 1999;25:173–179. doi: 10.1007/s001340050812. [DOI] [PubMed] [Google Scholar]
- 21.Constantin JM, Cayot-Constantin S, Roszyk L, Futier E, Sapin V, Dastugue B, Bazin JE, Rouby JJ. Response to recruitment maneuver influences net alveolar fluid clearance in acute respiratory distress syndrome. Anesthesiology. 2007;106:944–951. doi: 10.1097/01.anes.0000265153.17062.64. [DOI] [PubMed] [Google Scholar]
- 22.Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149:818–824. doi: 10.1164/ajrccm.149.3.7509706. [DOI] [PubMed] [Google Scholar]
- 23.Lu Q, Vieira S, Richecoeur J, Puybasset L, Kalfon P, Coriat P, Rouby JJ. A simple automated method for measuring pressure-volume curve during mechanical ventilation. Am J Resp Crit Care Med. 1999;159:257–282. doi: 10.1164/ajrccm.159.1.9802082. [DOI] [PubMed] [Google Scholar]
- 24.Lu Q, Constantin JM, Nieszkowska A, Elman M, Vieira S, Rouby JJ. Measurement of alveolar derecruitment in patients with acute lung injury: computerized tomography versus pressure-volume curve. Crit Care. 2006;10:R95. doi: 10.1186/cc4956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koutsoukou A, Bekos B, Sotiropoulou C, Koulouris NG, Roussos C, Milic-Emili J. Effects of positive end-expiratory pressure ongas exchange and expiratory flow limitation in adult respiratorydistress syndrome. Crit Care Med. 2002;30:1941–1949. doi: 10.1097/00003246-200209000-00001. [DOI] [PubMed] [Google Scholar]
- 26.Thille AW, Richard JC, Maggiore SM, Ranieri VM, Brochard L. Alveolar recruitment in pulmonary and extrapulmonary acute respiratory distress syndrome: comparison using pressurevolumecurve or static compliance. Anesthesiology. 2007;106:212–217. doi: 10.1097/00000542-200702000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Malbouisson LM, Muller JC, Constantin JM, Lu Q, Puybasset L, Rouby JJ. Computed tomography assessment of positive endexpiratory pressure-induced alveolar recruitment in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2001;163:1444–1450. doi: 10.1164/ajrccm.163.6.2005001. [DOI] [PubMed] [Google Scholar]
- 28.Lim CM, Koh Y, Park W, Chin JY, Shim TS, Lee SD, et al. Mechanistic scheme and effect of “extended sigh” as a recruitment maneuver in patients with acute respiratory distress syndrome: A preliminary study. Crit Care Med. 2001;29:1255–1260. doi: 10.1097/00003246-200106000-00037. [DOI] [PubMed] [Google Scholar]
- 29.Constantin JM, Jaber S, Futier E, Cayot-Constantin S, Verny-Pic M, Jung B, et al. Respiratory effects of different recruitment maneuvers in acute respiratory distress syndrome. Crit Care. 2008;12:R50. doi: 10.1186/cc6869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mahmoud KM, Ammar AS. A comparison between two different alveolar recruitment maneuvers in patients with acute respiratory distress syndrome. Int J Crit Illn J Sci. 2011;1:114–120. doi: 10.4103/2229-5151.84795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pelosi P, et al. Sigh in acute respiratory distress syndrome. Am J Respir Crit Care Med. 1999;159:1081–1085. doi: 10.1164/ajrccm.159.3.9802090. [DOI] [PubMed] [Google Scholar]
- 32.Lapinsky SE, Aubin M, Mehta S, Boiteau P, Slutsky AS. Safety and efficacy of a sustained inflatation for alveolar recruitment in adults with respiratory failure. Intensive care medicine. 1999;25:1297–1301. doi: 10.1007/s001340051061. [DOI] [PubMed] [Google Scholar]


