Abstract
Study Objectives:
To investigate the surgical outcomes and efficacy of modified uvulopalatopharyngoplasty (mod UPPP) and Coblation channelling of the tongue (CCT) as a treatment for obstructive sleep apnea (OSA).
Methods:
Adult patients with simple snoring or obstructive sleep apnea were treated with combined modified UPPP, bilateral tonsillectomy, and CCT (N = 48). Full polysomnography was performed preoperatively and 3 months postoperatively. Postoperative clinical assessment, sleep questionnaires, and patient demographics including body mass index were compared to preoperative data. All polysomnograms were re-scored to AASM recommended criteria by 2 sleep professionals.
Results:
The preoperative AHI (median and interquartile range) of 23.1 (10.4 to 36.6) was lowered to a postoperative AHI of 5.6 (1.9 to 10.4) (p < 0.05). The Epworth Sleepiness Scale score fell from 10.5 (5.5 to 13.5) to 5.0 (3.09 to 9.5) (p < 0.05). Morbidity of the surgery was low, with no long-term complications recorded.
Conclusions:
Modified UPPP combined with CCT is a highly efficacious intervention for OSA with minimal morbidity. It should be considered for individuals who fail or are intolerant of CPAP or other medical devices.
Citation:
MacKay SG; Carney AS; Woods C; Antic N; McEvoy RD; Chia M; Sands T; Jones A; Hobson J; Robinson S. Modified uvulopalatopharyngoplasty and coblation channeling of the tongue for obstructive sleep apnea: a multi-centre australian trial. J Clin Sleep Med 2013;9(2):117–124.
Keywords: Uvulopalatopharyngoplasty, snoring, obstructive sleep apnea, tongue, palate, surgery
Obstructive sleep apnea (OSA) is a common condition.1 It is associated with impaired quality of life, increased cardiovascular risk, excessive daytime sleepiness, increased risk of motor vehicle accidents, neuropsychological impairment and increased health service use.2 Currently, adult OSA may be treated with continuous positive airway pressure (CPAP) therapy, mandibular advancement splints (MAS), loss of weight, avoidance of the supine body position, contemporary airway reconstruction surgery, or with other conservative/adjunctive management strategies. While CPAP has been regarded as the “gold standard” therapeutic option for many years, it is only accepted by a proportion of sufferers, and adherence is highly variable (32% to 90%).3 There is thus a pressing need for effective alternative therapies for OSA beyond CPAP, particularly for those who fail CPAP therapy. There is now increasing evidence for the efficacy of multilevel airway surgery, although some authors have contested the use of contemporary surgical paradigms in this patient group.4 A recent American Academy of Sleep Medicine paper, “Practice Parameters for the Surgical Modifications of the Upper Airway for Obstructive Sleep Apnea in Adults” highlighted the significant progress in surgical techniques for the treatment of OSA but referred to the “lack of rigorous data evaluating surgical modifications of the upper airway.”5 Further, the paper recommended “systematic and methodical investigations” in order to “determine which populations are most likely to benefit from a particular procedure or procedures, and optimize perioperative care.”
BRIEF SUMMARY
Current Knowledge/Study Rationale: This study was undertaken to evaluate the effectiveness of a new, reconstructive modified UPPP technique combined with a potentially low morbidity tongue reduction for sleep disordered breathing. It was designed to assess the role that such an intervention has in contemporary airway reconstruction protocols.
Study Impact: Paradigms for adult sleep disordered breathing treatment are in constant evolution. This new multi-level surgical technique is effective in significantly improving physiological and subjective markers of obstructive sleep apnea, whilst avoiding long term complications.
Traditionally, surgeons have treated selected OSA patients with uvulopalatopharyngoplasty, plus or minus bilateral tonsillectomy, where applicable. The efficacy of the procedure was reasonable, but complications were not uncommon and late failures occurred as scar tissue formed. Many surgeons then modified their UPPP techniques to address the lateral velopharyngeal ports, while leaving a neo-uvula to prevent globus pharyngeus. These UPPP modifications resulted in much higher rates of success with a lower morbidity. However, despite adequate palatal surgery, a significant number of patients still have failed to achieve satisfactory results, presumably as a result of untreated collapse at other levels. For a variety of reasons, including a scarcity of trained surgeons and concerns about complications (including airway obstruction and hemorrhage), extensive tongue surgeries have traditionally been performed in only a small number of centers worldwide. A simpler method of tongue reduction involves Coblation (radiofrequency + saline resulting in a localized plasma field that ablates a column of tissue) technology, to produce multiple channels of ablated tissue through anatomically safe areas of the tongue. Whilst excellent results, largely from China, have been presented at numerous international conferences, there is yet to be formal outcome data published in the Chinese or English speaking literature, combining this technique with modified UPPP.
In this two-center prospective trial, we considered the hypothesis that modified UPPP + CCT would provide satisfactory outcomes for patients with snoring/OSA.
METHODS
Study Design
The study was a prospective, 2-center cohort study (Adelaide and Wollongong). Ethical approval for the study was obtained from The Flinders University Clinical Human Research Ethics Committee.
Patient Recruitment and Surgical Protocol
Consecutive patients with complete datasets were recruited from the practices of the participating primary surgeons.
The following preoperative data was collected for all patients:
Formal in-laboratory polysomnography (PSG)
Epworth Sleepiness Scale (ESS) score
Age and sex
Body mass index (BMI)
Friedman tonsil and palate/tongue grade
The two surgeons in this trial previously worked together in an Australian teaching hospital with expertise in contemporary airway reconstruction techniques for snoring and OSA.
Inclusion Criteria
Patients with all degrees of snoring and OSA were entered into the trial, although the vast majority (94%) of the 48 patients analyzed had mild, moderate, or severe OSA according to apnea-hypopnea index (AHI) recommended criteria. Patients with Friedman Stage 1 or 2 anatomy were included, where tonsillar and/or retropalatal generated collapse was demonstrated using a modified Mueller maneuver and Woodson's hypotonic method6 and any degree of retrolingual collapse was observed. Patients with Friedman Stage 3 were entered into the trial when these patients declined device use or more extensive tongue or palatal surgery.
Exclusion criteria: Patients with BMI > 35 were initially not accepted for surgery, and weight loss surgery or device use was recommended. However, one patient with BMI > 40 and tonsillar enlargement declined other treatment options and was included. We excluded patients with obvious micrognathia or other bony anatomical deficiencies and patients with cardiopulmonary conditions that rendered them an unacceptable anaesthetic or operative risk.
Modified uvulopalatopharyngoplasty (mod UPPP) with bilateral tonsillectomy and Coblation channelling of the tongue (CCT) was performed under general anaesthesia in all patients. All patients subsequently underwent repeat PSG at approximately 3 months postoperatively. ESS, BMI, and a further clinical assessment were repeated at that time.
As PSG data were derived from a variety of referral laboratories, all sleep studies were then transferred electronically and formally scored by 2 sleep experts, using AASM 2007 Recommended Criteria, to ensure congruity of sleep study data.
Surgical Technique
Each patient was operated on under general anesthesia, with either nasal or oral intubation. All underwent a Robinson-type modified uvulopalatopharyngoplasty, which involves the following steps:
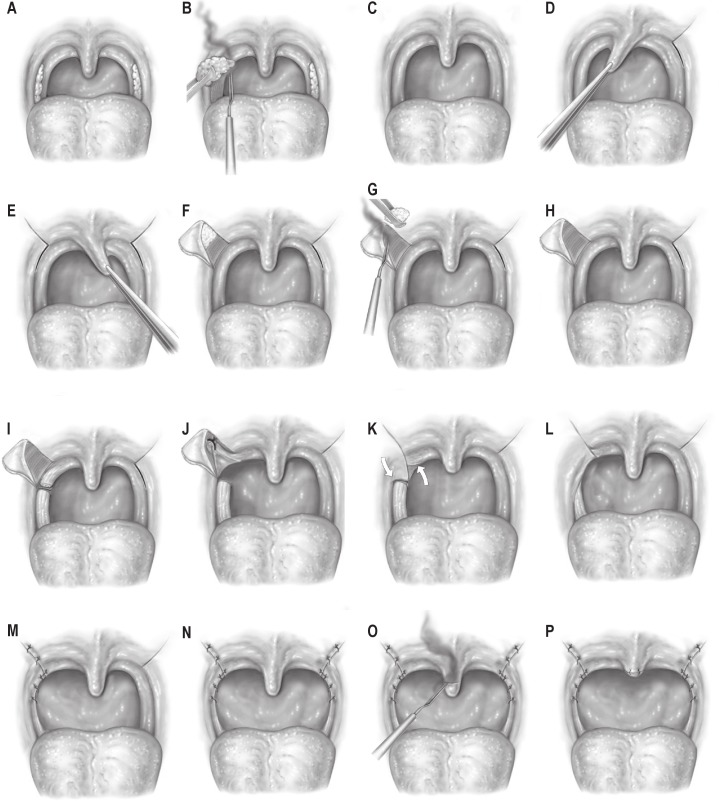
Resection of the tonsils, with preservation of pillar mucosa (Diagram 1A-C)
Traction on the uvula caudally while elevating a triangular flap of mucosa on each side as shown diagrammatically (Diagram 1D-F)
Resection of supratonsillar fat bilaterally (Diagram 1G)
Division of posterior pillar mucosa and musculature at the junction of upper third/lower two-thirds (Diagram 1I)
Suture advancement of the upper part of the posterior pillar musculature into the superolateral velopharyngeal port created in steps 2 and 3 using 2/0 Vicryl (Diagram 1J)
Closure of the overlying mucosa using 3/0 Vicryl (Diagram 1K-N)
Resection of approximately 50% to 75% of the uvula in a bevelled fashion to create a neo-uvula (Diagram 1O, P)
Diagram 1.
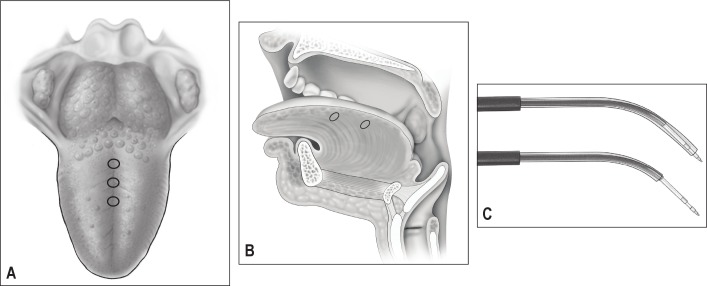
Seven-port Coblation channelling of the tongue was then performed, using a Reflex 55 or SP plasma wand (Arthrocare Corp, Austin, TX, USA) at a power setting of 6, for 15 sec per channel (Diagram 2C). The 7 channels include 3 midline channels with 2 lateral channels on each side (Diagram 2A, B). The 3 midline channels start from 1 cm in front of the apex of the circumvallate papillae, moving forward by 1–2 cm, but no further forward than 2.5 cm from the tip of the tongue. The lateral channels are produced in the axial plane, with entry points at the junction of the dorsal and lateral tongue mucosa with the probe directed and angled toward the posterior tongue just behind the circumvallate papillae.
Diagram 2.
All patients remained in hospital overnight and were discharged the following day on oral analgesia and a 5–7 day course of oral broad-spectrum antibiotic.
Polysomnography
Attended PSG was performed on all patients preoperatively and postoperatively. Standard techniques of monitoring were used including EEG, electroculographic derivations, electromyographic derivations, nasal pressure transducer, chest and abdominal effort monitors, body position monitor, leg EMG derivations, and single ECG channels, as well as dedicated pulse oximetry. The polysomnographic data were then analyzed by 2 independent sleep experts (one in Wollongong, one in Adelaide), rescoring all results to AHI recommended criteria, as per the American Academy of Sleep Medicine Scoring Criteria.7 Epochs were reviewed in 30-sec frames.
Data Analysis and Statistics
Friedman Stage is an important indicator of palate (relative to tongue) position, tonsil size, and BMI.8 The group data were stratified for each Friedman stage to determine patient characteristics best suited for this operation. Data were analyzed using the statistical package PASW Statistics 18. Dependent variables were generally skewed, and with a comparatively small sample size, nonparametric statistical tests (related-samples Wilcoxon signed ranks test) were used to assess the differences between preoperative and postoperative variables (AHI; ESS; lowest oxygen saturation, LSaO2; and BMI). Data are presented as median (interquartile range) or median difference (median of postoperative minus preoperative value). P-value < 0.05 was considered statistically significant.
RESULTS
Sample size for the group was 48 patients (n = 27 in Adelaide – Surgeon 2; n = 21 in Wollongong – Surgeon 1). There were 7 females and 41 males, with average age 41.1 ± 13.0 years (range 16–76 years).
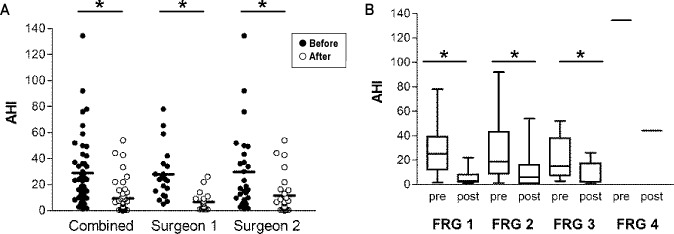
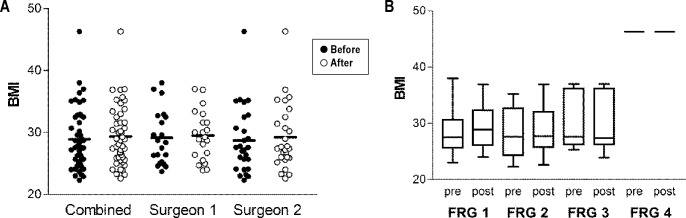
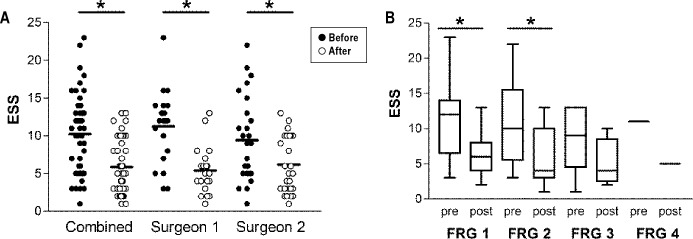
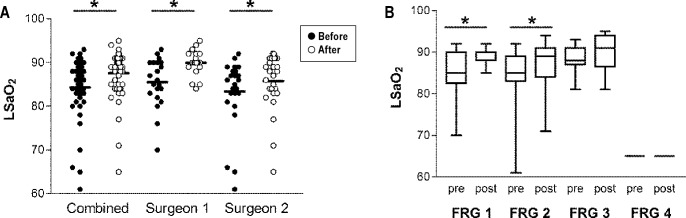
Preoperative and postoperative group data are summarized in Tables 1A and 1B, with significant improvements observed for AHI (median difference of −12.5; p < 0.05), ESS (median difference of −3.0; p < 0.05), and LSaO2 (median difference of 2.0; p < 0.05). Importantly, 39 of the 48 (81%) patients had a preoperative LSaO2 < 90%; of these, 16 (41%) improved clinically to a postoperative LSaO2 > 90%. Note, 1 of 9 (11%) patients with preoperative LSaO2 > 90% also had postoperative LSaO2 < 90%. No change in BMI was observed (p > 0.05). Similar improvements in AHI (p < 0.05), ESS (p < 0.05), and LSaO2 (p < 0.05) measurements were observed for each surgeon (Table 1B, Figures 1A, 2A, and 3A). BMI remained unchanged between preoperative and postoperative assessments for each surgeon (Figure 4; p > 0.05).
Table 1A.
Comparison of preoperative and postoperative variables
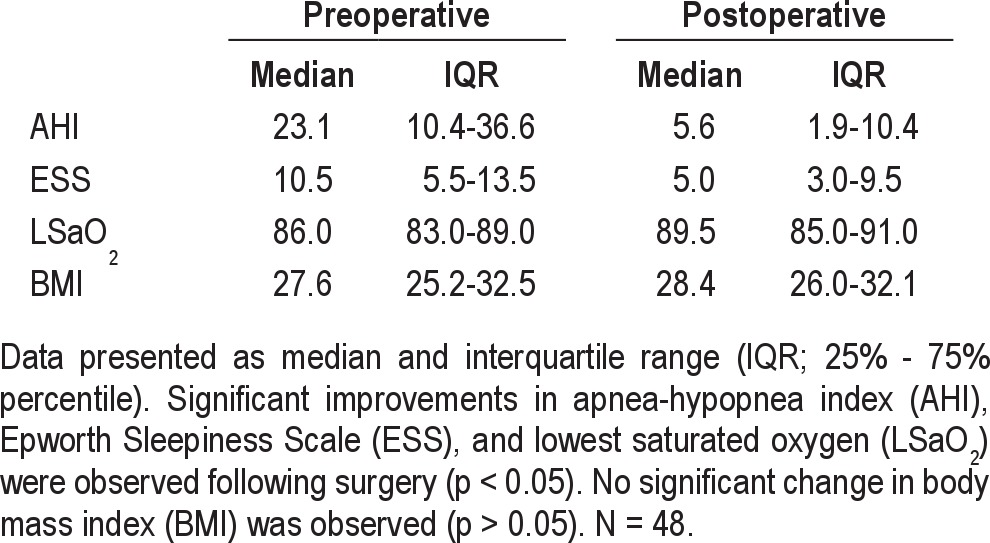
Table 1B.
Summary of median difference for each variable
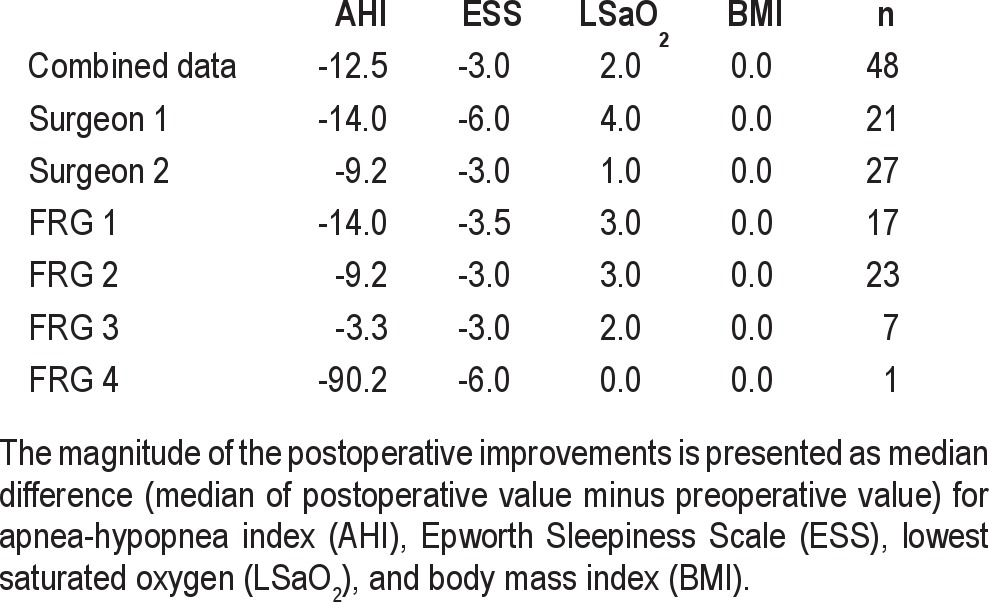
Figure 1. Comparison of preoperative and postoperative apnea hypopnea index (AHI).
Significant improvements in the AHI were observed following surgery. (A) Dot plots representing individual patient AHI result before and after surgery. Data presented for each surgeon and for both surgeons together (combined). (B) Box plot representing median, interquartile range, minimum, and maximum of AHI measurements for the combined data set, with patients tonsil size and palate (relative to tongue) position categorized according to Friedman (FRG) stage. *p < 0.05 related-samples Wilcoxon signed ranks test. N = 21 Surgeon 1, N = 27 Surgeon 2, N = 48 combined. N = 17, 23, 7, 1 for FRG class 1, 2, 3, 4, respectively.
Figure 4. Comparison of preoperative and postoperative body mass index (BMI).
No significant changes in BMI were observed following surgery. (A) Dot plots representing individual patient BMI score before and after surgery. Data presented for each surgeon, and for both surgeons together (combined). (B) Box plot representing median, interquartile range, minimum, and maximum of BMI measurements for the combined data set, with patients tonsil size and palate (relative to tongue) position categorized according to the Friedman (FRG) stage. N = 21 Surgeon 1, N = 27 Surgeon 2, N = 48 combined. N = 17, 23, 7, 1 for FRG class 1, 2, 3, and 4, respectively.
Figure 2. Comparison of preoperative and postoperative Epworth Sleepiness Scale (ESS).
Significant improvements in ESS were observed following surgery. (A) Dot plots representing individual patient ESS result before and after surgery. Data presented for each surgeon and for both surgeons together (combined). (B) Box plot representing median, interquartile range, minimum, and maximum of ESS measurements for the combined data set, with patients tonsil size and palate (relative to tongue) position categorized according to the Friedman (FRG) stage. *p < 0.05 related-samples Wilcoxon signed ranks test. N = 21 Surgeon 1, N = 27 Surgeon 2, N = 48 combined. N = 17, 23, 7, 1 for FRG class 1, 2, 3, 4, respectively.
Figure 3. Comparison of preoperative and postoperative lowest saturated oxygen (LSaO2).
Significant improvements in LSaO2 were observed following surgery. (A) Dot plots representing individual patient LSaO2 result before and after surgery. Data presented for each surgeon and for both surgeons together (combined). (B) Box plot representing median, interquartile range, minimum and maximum of LSaO2 measurements for the combined data set, with patients tonsil size and palate (relative to tongue) position categorized according to the Friedman (FRG) stage. *p < 0.05 related-samples Wilcoxon signed ranks test. N = 21 Surgeon 1, N = 27 Surgeon 2, N = 48 combined. N = 17, 23, 7, 1 for FRG class 1, 2, 3, 4, respectively.
Data were analyzed according to Friedman staging and showed significant improvement in median AHI for stages 1–3 (p < 0.05), with the single patient who was morbidly obese (Friedman stage 4) also showing a marked reduction in AHI (Figure 1B). Using the classical means of reporting surgical success (i.e. > 50% decrease in AHI plus post-surgical AHI < 20 events/h of sleep), the response rates in Friedman stages 1, 2, and 3 were 13/17 (76%), 14/23 (61%), and 5/7 (71%), respectively. There were significant improvements in ESS and LSaO2 for Friedman stage 1 (p < 0.05) and 2 (p < 0.05; Table 1B, Figures 2B and 3B).
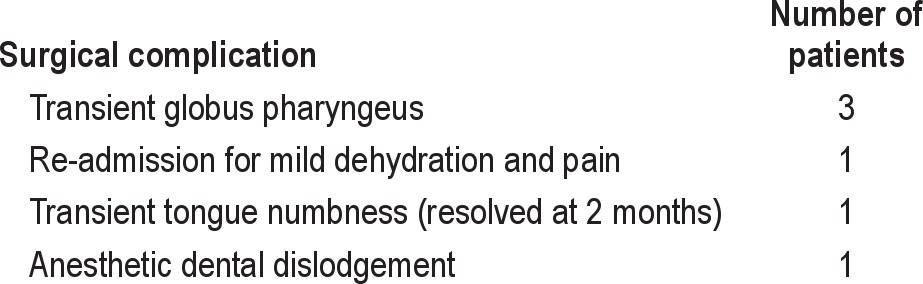
Minor surgical or anesthetic complications occurred in 6 patients (12.5%), and are summarized in Table 2. One patient was shown to have persistent sleep apnea postoperatively and went on to have further tongue reduction surgery. Two patients demonstrated postoperative mild sleep apnea and then re-tried CPAP with success.
Table 2.
Surgical complications
All patients in this series have been followed up for up to 4 years. There have been no late surgical failures detected clinically, although PSG studies have not been repeated since the 3-month postoperative study.
DISCUSSION
Airway surgery for sleep disordered breathing, particularly the use of UPPP in isolation, is controversial.9 There is a genuine need for good quality research to establish the exact role and clinical importance of sleep surgery.10
This study has demonstrated significant improvements in physiological parameters and clinical well-being in a group of patients who have failed or declined device treatment options. Using a modified lateral velopharyngeal port opening Robinson type UPPP with minimally invasive tongue reduction in the form of CCT, we have achieved significant improvements in AHI and other markers. Mean AHI fell 68% (from 28.9 to 9.3 events/h of sleep), which compares favorably with the 33% reduction in mean AHI (40.3 to 29.8 events/h of sleep) reported for UPPP alone in a recent meta-analysis.9
Although Friedman stage I patients are considered to have the most favorable anatomy for, and treatment response to, UPPP we included them in this study of multilevel surgery since one in five such patients are still found to fail UPPP.11 While our results in this group were very favorable (reduction in median AHI from 23 to 5; responders 76%), they are similar to the results reported by Friedman et al. for UPPP alone (reduction in mean AHI from approximately 25 to 6, responders 80%).11 Thus, we may not have achieved any additional benefit from adding tongue base Coblation in this group, although this is worthy of further study using a randomized controlled study design. Our results among Freidman stage 2 patients are better than reported for UPPP alone9 and comparable to those reported previously for UPPP + radiofrequency tongue base ablation.11 We would argue, however, that Coblation channelling carries with it less morbidity than radiofrequency ablation. While the numbers of patients in our study with Friedman stages 3 and 4 were small, the results with combined UPPP and Coblation tongue channelling among these patients are perhaps the most encouraging. A significant fall in AHI was demonstrated in our patients who were Friedman stage 3. Expressing response as the median of change in AHI in this group of only 7 patients with a very wide range of disease severity tended to obscure what were, in fact, very positive results. All but one patient had a reduction in AHI post-surgery, and 5 of 7 (71%) were responders using the traditional definition of > 50% decrease in AHI, with AHI < 20. This compares very favorably with response rates reported by Friedman et al.11 in stage 3 patients of 8% with UPPP alone and 33% with UPPP + tongue base radiofrequency ablation. Despite the fact that Friedman stage 3 may include patients with no tonsils, it is interesting to note that all stage 3 patients in this study were noted to have some tonsillar tissue.
Recent published literature5 has highlighted the difference between a classical UPPP and the newer variations (lateral velopharyngeal port opening procedures). There is an increasing amount of evidence5,12,13 to support the latter over the former. We would suggest that a traditional UPPP now has little, if any, role in current sleep surgical practice. We believe a modified UPPP is superior, not only because of better PSG outcomes but also in terms of reducing any potential complications related to dysfunction of the velopharynx. It stands to reason that preservation of most of the structures of the free edge of the palate without significant resection (i.e., a reconstructive intervention rather than an ablative procedure) is likely to reduce the risk of long term adverse events.
The technique used in this paper is also unique in its ease of performance, reproducibility, and low complication profile. It also importantly permits return to CPAP for failures without air leak or complication.
Coblation channelling is unique in its use of saline enhanced radiofrequency to create a plasma field. Tissue reduction is achieved by creating tissue ablation (into low-molecular weight gases) rather than coagulation. Animal modelling and MRI studies have clarified the effect of this technique on the tongue tissue.14,15
The modified Robinson uvulopalatopharyngoplasty technique is unique in its simplicity. It focuses on opening the lateral velopharyngeal ports without resection of tissue other than tonsils and submucosal fat. It is therefore reconstructive, not ablative, decreasing the subsequent risk of unpredictable scar. It achieves a similar result to expansion sphincteroplasty but is more reproducible and easier to learn for the general ENT surgeon, as it does not require the separating out of the posterior pillar musculature from mucosa, or the rotation of muscle. It is distinguished from the extended uvulopalatal flap technique in its maintenance of a neo-uvula, although it can be converted to a conservative uvulopalatal flap if there is forward projection of the neo-uvula. No resection of mucosa or significant “trenching” is required, as with some lateral pharyngoplasty type surgeries.
Traditional temperature controlled radiofrequency tongue ablation has been proven to be effective in a number of studies, including a randomized control trial.16 It is important to realize that there are now several technologies available for lingual surgery that utilize monopolar and bipolar radiofrequency devices. However, when radiofrequency is applied through an ionic fluid (e.g., saline), a powerful ablative localized plasma field is produced. This is the technology utilized in Coblation which allows maximal tissue ablation with minimal thermal injury and therefore a reduction in subsequent postoperative pain, which has been demonstrated in randomized controlled trials.17 The effectiveness of Coblation tongue channelling has been demonstrated in an animal model and retrospective case series in man.14,15 The seven-channel technique is unique in improving outcomes as demonstrated in this paper as well as reducing the risk of globus pharyngeus. We postulate the reduction in globus is achieved by separating the posterior third tongue from the free edge of the palate. The seven-channel Coblation technique treats the middle third and posterior third of the tongue, rather than the tongue base alone.
The patients in this study had significant improvement in a number of sleep related outcome measures. The mean fall in ESS pre- and post-treatment was 4.36, which compares favorably with reductions of approximately 4 in other studies investigating patients with moderate-to-severe OSA treated with CPAP.5,18
As paradigm development for treatment of obstructive sleep apnea in adults develops and broadens, the multidisciplinary team now has many options. In addition to CPAP treatment, there is mandibular advancement splint, contemporary airway reconstruction, bariatric surgery, weight loss expertise, dietary advice, and other treatment modalities.19
The dilemma of what procedure (or combination of procedures) to perform on which patient remains highly controversial. Should we proceed straight to extensive palatal surgery (e.g., transpalatal advancement plus modified UPPP) and aggressive tongue surgery in patients with unfavorable anatomy or severe sleep apnea? One approach is to start with more minimally invasive procedures with lower morbidity and progress to more extensive surgeries if needed. When palatal surgery alone is performed for sleep disordered breathing, a proportion of patients will not achieve an adequate result. With the availability of a minimally invasive option for treatment of any retrolingual segment collapse, we have the option of performing a modified UPPP along with CCT without any apparent extra risk to our patients. This study has demonstrated such intervention delivers extremely good surgical outcomes with minimal morbidity. This two-level combination procedure should be considered a potential first-line surgical option for all patients with snoring or OSA. More extensive staged surgery can always be performed if required. In this cohort, further surgery has rarely been necessary.
The strength of this multicenter case series demonstrates significantly improved outcomes, not merely in physiological parameters but also in daytime sleepiness (ESS). This is in the context of an unchanged body mass index, confirming there has been no treatment effect from weight loss following surgery.
In addition, our study demonstrates that a contemporary multilevel surgical approach for patients with sleep disordered breathing can be effective without creating significant risk of complications in the long term. The use of two centers also demonstrates a degree of generalizability and reproducibility for the achievement of a successful outcome from the intervention. The rescoring of all pre- and post-polysomnographic data confirms efficacious outcome while ensuring congruency in reporting.
There are several weaknesses in this study. There was a short time frame of postoperative PSG assessment, although all patients are subsequently being followed on an annual and 3-yearly basis and will be referred for further PSG analysis if there is return of any snoring or gain in weight. Secondly, as with all studies of this nature, a proportion of the patients (approximately 15%) operated on did not return for follow-up assessment within the trial period. The possibility of bias due to patient withdrawal must therefore be borne in mind when interpreting the results. It is reasonable to concede that the two surgeons involved in the study were trained in a hospital with a major interest in sleep treatments. It will be important to analyze data from surgeons with more general training to confirm that similar results can be obtained by most otolaryngologists. Furthermore, cardiovascular outcomes were not assessed in this study, nor were more general quality of life outcomes measured. Such outcomes should be the subject of further research. Finally, we have not analyzed polysomnographic parameters related to percentage of deep sleep or positional data, but regardless, the overall outcomes are significant.
In conclusion, this study has demonstrated that modified lateral port uvulopalatopharyngoplasty combined with Coblation channelling of the tongue provides significant reductions in AHI and ESS, and improvement in lowest oxygen saturations measured post-surgery, even in patients with unfavorable anatomy. It is a well-tolerated procedure with no long-term complications recorded in this series. We believe our data help to establish the role of modified UPPP and CCT within the construct of contemporary upper airway surgical protocols.
DISCLOSURE STATEMENT
The authors did not receive financial support for the work contributing to this paper. A. Simon Carney is a member of the International Medical Advisory Board of Arthrocare, PLC. All monies from this activity are donated to charity.
ACKNOWLEDGMENTS
The authors acknowledge the hard work of two senior sleep technologists, Jeremy Mercer and Amanda McKenna, for their sizeable contribution in rescoring polysomnographic data. We are grateful also for the statistical advice provided by Dr. Susan Kim, Statistical Consultant with Flinders Prevention, Promotion and Primary Health Care, Dept. of General Practice, Flinders University. Finally, the authors also acknowledge the tremendous contribution to sleep surgery made by our co-author Dr. Sam Robinson who sadly passed away prior to the submission of this paper. Dr. Robinson was a major contributor to this paper, not only in its conception and design, but also as a major contributor of patients. He was collecting data for use in this study at the time of his death. Work for this study was performed at University of Wollongong and Illawarra ENT Head and Neck Clinic, Wollongong, NSW and Flinders Medical Centre and Memorial Hospital, Adelaide, South Australia.
REFERENCES
- 1.Young T, Peppard PE, et al. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165:1217–39. doi: 10.1164/rccm.2109080. [DOI] [PubMed] [Google Scholar]
- 2.Jennum P, Riha RL. Epidemiology of sleep apnoea/hypopnoea syndrome and sleep-disordered breathing. Eur Respir J. 2009;33:907–14. doi: 10.1183/09031936.00180108. [DOI] [PubMed] [Google Scholar]
- 3.Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5:173–8. doi: 10.1513/pats.200708-119MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elshaugh AG, Moss JR, Southcott A, et al. An analysis of the evidence-practice continuum: is surgery for obstructive sleep apnoea contra-indicated? J Eval Clin Pract. 2007;13:3–9. doi: 10.1111/j.1365-2753.2006.00793.x. [DOI] [PubMed] [Google Scholar]
- 5.Aurora RN, Casey KR, Kristo D, et al. Practice parameters for the surgical modifications of the upper airway for obstructive sleep apnea in adults. Sleep. 2010;33:1408–13. doi: 10.1093/sleep/33.10.1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fairbanks DNF, Mickelson SA, Woodson BT. 3rd ed. Lippincott Williams – Williams; 2003. Snoring and obstructive sleep apnea; pp. 62–4. [Google Scholar]
- 7.Iber C, Ancoli-Isreal S, Chesson AL, Quan SF. 1st Ed. Westchester, IL: American Academy of Sleep Medicine; 2007. The AASN manual for the scoring of sleep and associated events: Rules, terminology and technical specifications. [Google Scholar]
- 8.Friedman M, Ibrahim H, Joseph MJ. Staging of obstructive sleep apnoea/hypopnea syndrome: A guide to appropriate treatment. Laryngoscope. 2004;114:454–9. doi: 10.1097/00005537-200403000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Caples MS, Rowley JA, Prinsell JR, et al. Surgical modifications of the upper airway for obstructive sleep apnoea in adults: A systemic review and meta-analysis. Sleep. 2010;33:1396–1407. doi: 10.1093/sleep/33.10.1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Field CJ, Robinson S, MacKay S, Harrison JD, Marshall NS. Clinical equipoise in sleep surgery: investigating clinical targets. Otolaryngol Head Neck Surg. 2011;145:347–53. doi: 10.1177/0194599811406053. [DOI] [PubMed] [Google Scholar]
- 11.Friedman M, Ibrahim H, Lee G, Joseph NJ. Combined uvulopalatopharyngoplasty and radiofrequency tongue base reduction for treatment of obstructive sleep apnea/hypopnea syndrome otolarynogology. Head Neck Surg. 2003;129:611–21. doi: 10.1016/j.otohns.2003.07.004. [DOI] [PubMed] [Google Scholar]
- 12.Pang KP, Woodson BT. Expansion sphincter pharyngoplasty: a new technique in the treatment of obstructive sleep apnea. Otolaryngol Head Neck Surg. 2007;137:110–4. doi: 10.1016/j.otohns.2007.03.014. [DOI] [PubMed] [Google Scholar]
- 13.Marshall NS, MacKay S, Gallagher R, Robinson S. Uvulopalatopharyngoplasty funded by the Australian Government's Medicare Scheme (1995–2007) Otolaryngol Head Neck Surg. 2010;142:3S1. doi: 10.1016/j.otohns.2009.06.011. [DOI] [PubMed] [Google Scholar]
- 14.Salinas NL, Barrera JE. Coblation Lesion Formation in a porcine tongue model. Otolaryngol Head Neck Surg. 2010;143:448–53. doi: 10.1016/j.otohns.2010.04.016. [DOI] [PubMed] [Google Scholar]
- 15.Zhang Q, Song W, She C, et al. Coblation-assisting uvulopalatopharyngoplasty combining Coblation-channeling of the tongue for patients with severe OSAHS. J Clin Otorhinolaryngol Head Neck Surg. 2012;26:114–7. doi: 10.13201/j.issn.1001-1781.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 16.Woodson BT, Steward DL, Weaver EM, et al. A randomised control trial of temperature-controlled radiofrequency, continuous positive airway pressure and placebo for obstructive sleep apnoea syndrome. Otolaryngol Head Neck Surg. 2003;128:848–61. doi: 10.1016/S0194-59980300461-3. [DOI] [PubMed] [Google Scholar]
- 17.Joshi H, Carney AS. Use of Coblation in Otolaryngology, Head and Neck Surgery. Br J Hosp Med (Lond) 2011;72:565–9. doi: 10.12968/hmed.2011.72.10.565. [DOI] [PubMed] [Google Scholar]
- 18.Antic NA, Eckerman S, Esterman A, et al. Clinical effectiveness of CPAP in normalising daytime sleepiness, quality of life and neurocognitive function in moderate-severe OSA. Sleep. 2011;34:111–19. doi: 10.1093/sleep/34.1.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Epstein LJ, Kristo D, Strollo PJ, et al. Clinical guideline for the evaluation, management and long term care of obstructive sleep apnoea in adults. J Clin Sleep Med. 2009;5:263–76. [PMC free article] [PubMed] [Google Scholar]