Abstract
Study Objectives:
Many studies have reported a positive association between sleep problems and suicidal ideation. Some prospective studies in the elderly have shown that insomnia is a risk factor for suicide death after controlling for other depressive symptoms. However, hypotheses to explain how this risk is mediated have not previously been assessed. We tested the hypothesis that insomnia symptoms are related to suicidal ideation through mediation by dysfunctional beliefs and attitudes about sleep and/or nightmares.
Methods:
We measured symptoms of depression, hopelessness, insomnia severity, dysfunctional beliefs and attitudes about sleep, nightmares, and suicidal ideation intensity on a convenience sample of 50 patients with depressive disorders, including 23 outpatients, 16 inpatients, and 11 suicidal ED patients. Mediation analysis was used to assess the indirect effects of insomnia symptoms on suicidal ideation through dysfunctional beliefs about sleep and through nightmares.
Results:
Our findings again confirmed a positive association between insomnia symptoms and the intensity of suicidal ideas in depressed patients (b = 0.64, 95% CI = [0.14, 1.15]). However, we extended and clarified our earlier findings by now showing that dysfunctional beliefs and attitudes about sleep as well as nightmares may mediate the association between insomnia symptoms and suicidal ideation. The indirect effects of insomnia symptoms through dysfunctional beliefs about sleep and through nightmares were 0.38 (-0.03, 0.97) and 0.35 (0.05, 0.75), respectively.
Conclusions:
Nightmares as well as dysfunctional beliefs and attitudes about sleep each are positively and independently related to the intensity of suicidal ideation, and the effect of insomnia symptoms appears to be mediated through these two variables.
Citation:
McCall WV; Batson N; Webster M; Case LD; Joshi I; Derreberry T; McDonough A; Farris SR. Nightmares and dysfunctional beliefs about sleep mediate the effect of insomnia symptoms on suicidal ideation. J Clin Sleep Med 2013;9(2):135–140.
Keywords: Insomnia, suicidal ideation, depression, nightmares, dysfunctional beliefs and attitudes about sleep, inpatients, outpatients, emergency department, electronic health record
Suicide is a leading cause of death across all ages and occurs at a rate of 10–11 cases per 100,000 persons per year in the Unites States.1 It is the third leading cause of death in those younger than 30 years of age.1 The majority of suicides occur in the context of an active psychiatric disorder, the most common of which is major depressive disorder (MDD).1
The risk factors for suicide have been described and include both unmodifiable and some potentially modifiable factors.2–4 Examples of unmodifiable factors include advancing age, male gender, and Caucasian ethnicity; potentially modifiable risk factors include symptoms of depression, hopelessness, social isolation, active alcohol/substance use, insomnia, and nightmares. Insomnia symptoms are significant predictors of near-lethal suicide attempts,5 yet insomnia is often overlooked in review papers about risk factors for suicide and suicide prevention.6 The need to broaden the search for modifiable risk factors is epitomized by this statement from a recent review of suicide prevention research: “nowhere is the lack of proven therapeutic methods greater than in the prevention of suicidal behavior.”7
As reviewed elsewhere, many studies have linked insomnia symptoms and/or nightmares to either suicidal ideation or completed suicide in adults.8 While most of the studies were cross-sectional and/or focused on suicidal ideation, four studies prospectively reported statistically significant relative risks of suicide death up to 2.4 in those with insomnia.9 Insomnia was the most common sleep disturbance associated with suicide, but nightmares also conferred risk. These associations generally remained even after adjusting for severity of depression.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Many independent reports have a shown that insomnia is a risk factor for suicidal ideation. However, prior studies have not tested a hypothesis for identifying specific mediators of this association between insomnia and suicidal ideation.
Study Impact: This study examined patients with a wide range of severity in depressive and suicidal symptoms and suicidal ideation, finding that the relationship between insomnia and suicidal ideation is mediated through nightmares and through dysfunctional beliefs and attitudes about sleep. These findings suggest new targets in the reduction of suicidal ideation.
We recently reported a relationship between the intensity of suicidal ideation and the intensity of insomnia symptoms.10 Our report was the first to show this relationship holds true in the context of a clinical trial for insomnia and depression,11 raising the question whether more aggressive treatment of insomnia might be justified as a way to prevent worsening suicidal ideation.
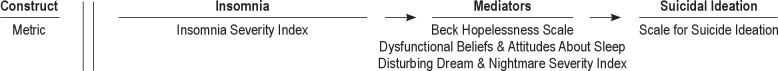
The finding that insomnia is a risk factor for suicide begs the question of the mediating variables that confer this risk.8 One candidate mediator is the sleep-specific cognitive distortion that frequently occurs in insomnia. These cognitive distortions, like those associated with hopelessness, are potentially modifiable with treatment.3 Interestingly, many of the cognitive distortions seen in chronic insomnia have a “hopelessness flavor” to them, as reflected in the content of the Dysfunctional Beliefs and Attitudes about Sleep Scale, which includes items such as “When I sleep poorly one night, I know it will disturb my sleep schedule for the whole week.”12–14 These dysfunctional beliefs regarding sleep have been identified in depressed insomniacs.15 Treating insomnia with cognitive behavior therapy for insomnia (CBT-I) reduces hopeless cognitions as the insomnia syndrome resolves.14 Another possible mediating factor is nightmares, as nightmares have been repeatedly cited as associated with suicidal ideation.8,10 Our hypothesis and theoretical model is that the intensity of insomnia symptoms is positively correlated with nightmares as well as dysfunctional beliefs and attitudes about sleep, which in turn mediate the intensity of suicidal ideation (Figure 1). In this paper, we assess the indirect effect of insomnia symptoms on suicidal ideation through nightmares plus dysfunctional beliefs and attitudes about sleep.
Figure 1. Theoretical model of mediation of the effect of insomnia on suicidal ideation.
METHODS
The current cross-sectional study utilized a convenience sample of patients with depressive disorders being seen at Wake Forest Baptist Medical Center (WFBMC), including patients being managed in the outpatient clinic, the inpatient adult psychiatry unit, and the emergency department (ED). We chose this broad demographic to yield a sample with a wide range of depressive symptoms, insomnia symptoms, and suicidal ideation.
Participants
Inclusion Criteria
Participants were literate, English-speaking adults ≥ 18 years old who had a chart diagnosis of one of the following depressive illnesses with nil, mild, moderate, or severe degree of overall symptoms: MDD without psychotic features, MDD with psychotic features, Depressive Disorder Not Otherwise Specified, Bipolar Disorder Type I-Most Recent Episode Depressive, or Bipolar Disorder Type II-Most Recent Episode Depressive. Patients with chronic pain were not excluded. All ED patients selected for inclusion were being held in the ED for admission for suicidal ideation. Written, informed consent was obtained from participants after they were given a complete description of the study. The study was approved by the local IRB.
Exclusion Criteria
Patients with laboratory-confirmed or clinically suspected sleep apnea or restless leg syndrome (RLS) were excluded. The presence or absence of sleep apnea and/or RLS was made on the basis of inspection of the electronic health record (EHR) for the results of prior polysomnography (PSG), or for a presumptive prior clinical diagnosis in the absence of PSG, or positive response to both questions: “Do you snore?” and “Does your bed partner state that you stop breathing periodically in your sleep?” Patients endorsing all the symptoms of the International Restless Leg Syndrome questionnaire were excluded.16 Patients with a chart diagnosis of Schizophrenia, Schizoaffective Disorder, Cognitive Disorder (Dementia), or Borderline Personality Disorder were excluded. All patients with frequent nocturia (out of bed ≥ 2 times per night every night), electroconvulsive therapy in the last 30 days, or substance abuse or dependence in the last 30 days were excluded. All included inpatients and all ED patients had a negative blood alcohol and negative urine drug screen at the time of presentation.
Clinical Assessment
Psychiatric physicians, including both residents and faculty, conducted all patient assessments. Physicians collected demographic and clinical information on all participants, including age, gender, education level, race, marital status, presence or absence of chronic pain, and number of prior clinical encounters (both inpatient and outpatient) within the WFBMC Department of Psychiatry and Behavioral Medicine. In the absence of a structured diagnostic interview, we recorded the number of clinical encounters (cataloged in ranges: 1–5, 6–10, 11–15, 16+) to reflect the sum of our prior clinical experience with the patients, as a corollary of our confidence in the diagnosis. Psychiatric diagnoses were therefore ascertained by a review of the entire EHR.
Physicians reviewed the EHR for all current medications and verified them with the participant. All psychotropic medications were permitted and were catalogued according to the following general categories, irrespective of dose:
Non-sedating antidepressants: selective serotonin reuptake inhibitors, selective serotonin-norepinephrine reuptake inhibitors, and bupropion
Sedating antidepressants: trazodone, mirtazapine, tricyclic antidepressants
Antipsychotics: typicals (e.g., haloperidol, fluphenazine, thiothixene) and atypicals (e.g., aripiprazole, zisprasidone, asenapine, quetiapine, olanzapine, risperidone)
Mood stabilizers: lithium, lamotrigine, valproate
Hypnotic/anxiolytics: benzodiazepines, hydroxyzine, zolpidem, eszopiclone, zaleplon
Over-the-counter sleep aids: melatonin, diphenhydramine, doxylamine
Psychometrics
Physicians collected the following psychometrics on each patient.
Depression severity was measured with the Patient Health Questionnaire-9 (PHQ-9). The PHQ-9 tracks the 9 symptoms found in the Diagnostic and Statistical Manual (DSM)-IV criteria for MDE, with each symptom scored between 0 (not at all) and 3 (nearly every day). A PHQ score ≥ 10 has 88% sensitivity and specificity for MDD.17 Syndromal depression was defined as a total score ≥ 10, with mood or anhedonia items scored ≥ 1. The total PHQ score minus the sleep and suicide item was used in the mediation analyses.
The Beck Hopelessness Scale is a 20-item scale that assesses pessimism and negative expectancies for the future with demonstrated validity across a wide age range.18,19 It has been found to predict future suicidal behavior.20
The Insomnia Severity Index (ISI) is a 7-item questionnaire, with each item scored 0–4, for a maximum of 28 points.21 The items are scaled according to the degree of dissatisfaction with sleep, in contrast to a sleep diary which measures the dimension of time spent awake or asleep. Higher scores on the ISI represent greater degrees of insomnia, and scores > 7 indicate a clinically relevant degree of insomnia.
The Dysfunctional Beliefs and Attitudes Scale (DBAS-16) captures the most common distorted cognitions about sleep that are reported by insomniacs. The DBAS-16 is a set of 16 items and uses a 0–10, Likert-type scale response format (0-strongly disagree to 10-strongly agree).22 There are 4 factors within the DBAS-16: (a) perceived consequences of insomnia, (b) worry/helplessness about insomnia, (c) sleep expectations, and (d) medication. The DBAS-16 was found to have adequate internal consistency and temporal stability, to show acceptable convergent validity with conceptually related measures, and to present adequate construct validity as evidenced by a factor structure consistent with current psychological conceptualizations of insomnia.23
The frequency and intensity of disturbing dreams and nightmares was measured with the Disturbing Dream and Nightmare Severity Index (DDNSI). This scale is derivative of the Nightmare Frequency Questionnaire that had a test-retest weighted kappa > 0.85.24 The revised DDNSI has good internal consistency with a Cronbach's alpha > 0.80.25,26 DDNSI has 5 items which measure the dimensions of frequency, intensity, and severity of nightmares. Scores can range from 0–37, with higher scores indicating a greater degree of difficulty with nightmares.
The Beck Scale for Suicide Ideation (SSI) is a well validated instrument consisting of 19 items that evaluate 3 dimensions of suicide ideation: active suicidal desire, specific plans for suicide, and passive suicidal desire.27,28 Each item is rated on a 3-point scale from 0 to 2 for a maximum score of 38, with a lower score indicating less severe suicidal ideation. Other investigators have found that an SSI score ≥ 3 predicts greater risk of suicide death over a time period of years.4 The ascertainment of the SSI included a review of the patient's suicide attempt history.
Analytical Plan
The sample size of 50 persons was chosen to provide ≥ 80% power for detecting correlations ≥ 0.4 among insomnia symptoms, dysfunctional beliefs about sleep, nightmares, and suicidal ideation at the 5% two-sided level of significance. Means and standard deviations were used to summarize continuous variables, while frequencies and percentages were used to summarize categorical variables. The degree of linear association between continuous variables was quantified using Pearson linear correlation coefficient. Mediation analyses were used to determine the mediation effects of dysfunctional sleep beliefs as well as nightmares in the relationship between insomnia symptoms and suicidal ideation, unadjusted and adjusted for covariates.29 In these analyses, the total effect (denoted by c) of insomnia symptoms on suicidal ideation is estimated using a simple linear regression model predicting suicidal ideation from insomnia symptoms. Additional linear models are run to predict dysfunctional sleep beliefs and attitudes about sleep from insomnia symptoms and nightmares from insomnia symptoms, and the betas from those models are denoted by a1 and a2. Finally a multiple linear model is fit to predict suicidal ideation from dysfunctional sleep beliefs, nightmares, and insomnia symptoms, and the betas are denoted by b1, b2, and c', respectively. The 2 indirect effects of interest, insomnia symptoms on suicidal ideation through dysfunctional sleep beliefs and insomnia symptoms on suicidal ideation through nightmares are estimated as a1b1 and a2b2, respectively. The total indirect effect is the sum of the 2 indirect effects, and c' is an estimate of the direct effect of insomnia symptoms on suicidal ideation. The total effect of insomnia symptoms (c) is the sum of the indirect (a1b1 and a2b2) and direct (c') effects. Bootstrapping (with 5,000 samples) was used to obtain biased corrected 95% confidence intervals for the indirect effects. Usual normal theory was used to obtain 95% confidence intervals for the total and direct effects. Given our relatively small sample size, we assessed the effect of each patient characteristic (see Table 1), depressive symptoms, and hopelessness separately and only adjusted for those that were statistically significant in separate mediation analyses. SAS 9.3 was used for all analyses. The mediation analyses were done using the SAS Macro INDIRECT.30
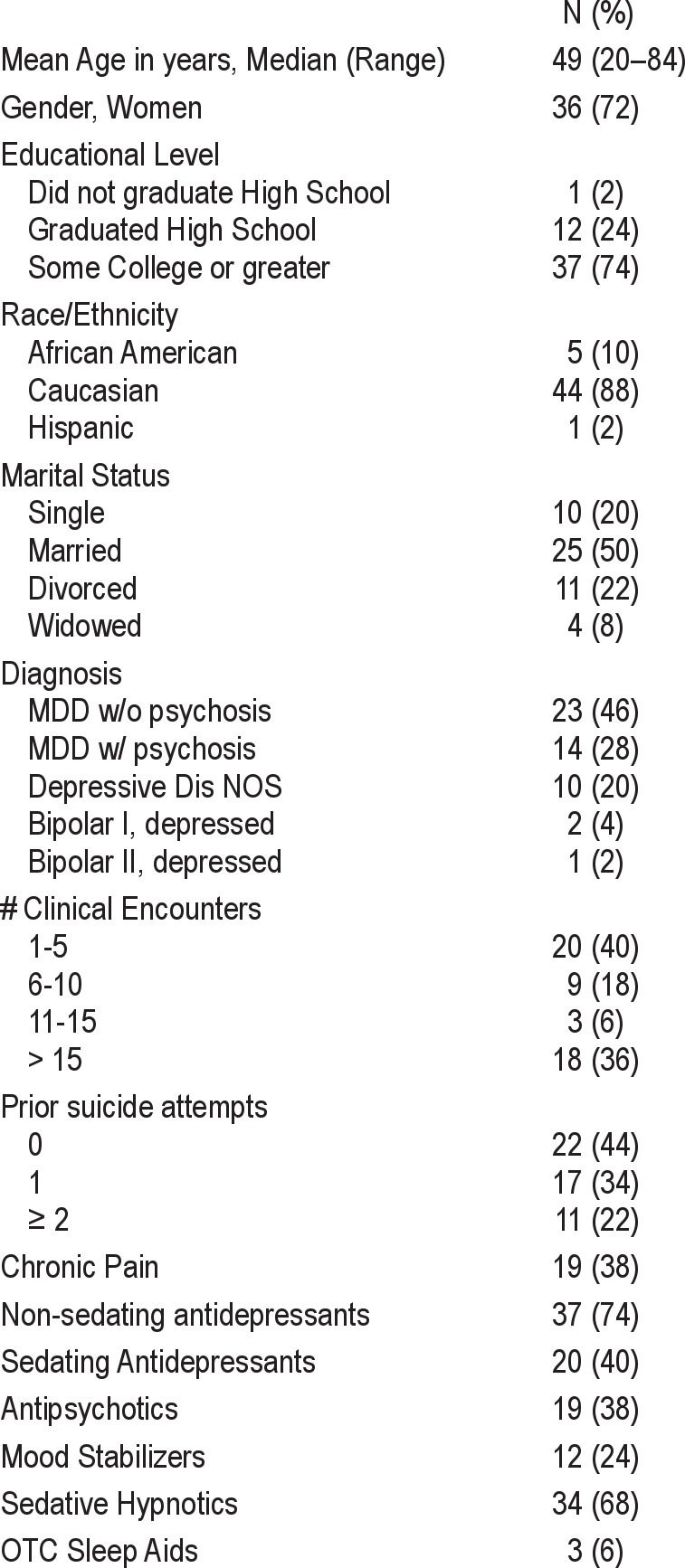
Table 1.
Demographic and clinical characteristics (N = 50)
RESULTS
The final sample of 50 patients included 23 outpatients, 16 inpatients, and 11 ED patients. Patient characteristics are summarized in Table 1. Age ranged from 20 to 80 years, with a median of 48. The majority were female (72%), Caucasian (88%), and had at least some college education (74%); half were married. Diagnoses included MDD without psychosis (46%), MDD with psychosis (28%), Depression NOS (20%), and Bipolar I or II with depression (6%). Slightly over half the patients had attempted to commit suicide, and 36% had > 15 clinical encounters. All but 4 of the 50 patients were taking a non-sedating antidepressant, sedating antidepressant, antipsychotic, mood stabilizer, or sedative hypnotic, as would be expected for patients in various phases of treatment for depression.
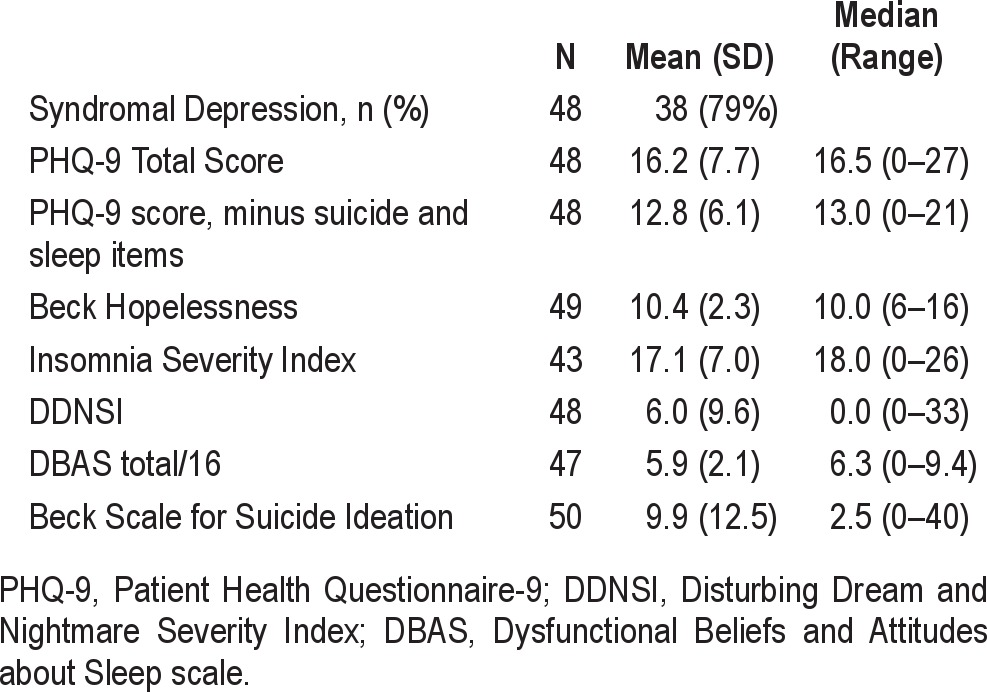
The psychometric test scores are summarized in Table 2. Seventy-nine percent of the patients met our definition of “syndromal depression.” The median total PHQ score was 16.5 and ranged from 0 to 27, indicating a moderate degree of depression. Similarly, the ISI mean score of 17. 1 indicates a moderate degree of insomnia symptoms.
Table 2.
Psychometrics
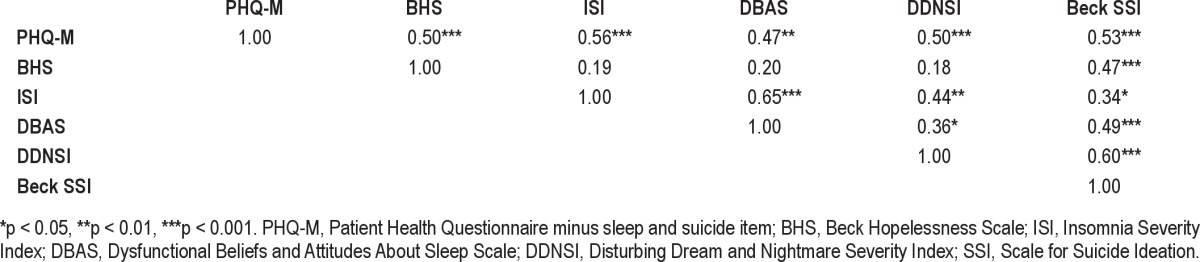
Correlations among the psychometric measures are shown in Table 3. Depression severity, minus the sleep and the suicide items, was significantly related to all other psychometric variables. While Hopelessness was related, as expected, to the Scale for Suicide Ideation, it was not significantly related to any of the 3 sleep variables—ISI, DBAS, or DDNSI. However, all 3 of these sleep variables were intercorrelated, and all 3 were correlated with the Scale for Suicide Ideation.
Table 3.
Pearson r correlations among depressive symptoms, hopelessness, insomnia symptoms, dysfunctional sleep beliefs, nightmares, and suicidal ideation
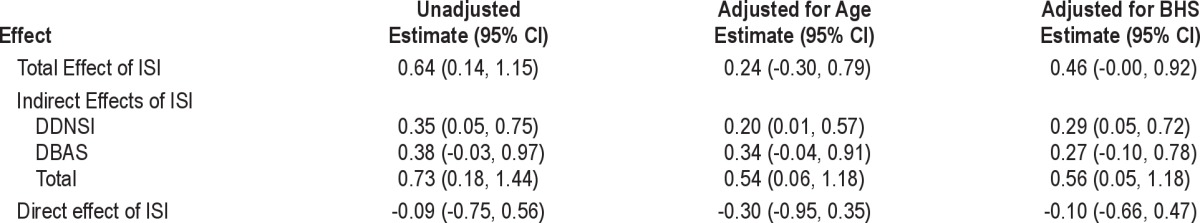
Results of the mediation analysis for the relation between insomnia symptoms and suicidal ideation are summarized in Table 4. Unadjusted for covariates, the total effect of ISI on suicidal ideation was 0.64 (95% CI: 0.14, 1.15), meaning for every unit increase in ISI suicidal ideation was expected to increase by 0.64. As seen in the first column of Table 4, that effect was mediated by DDNSI and DBAS. The indirect effect of ISI through DDNSI was 0.35 (0.05, 0.75), while the indirect effect of ISI through DBAS was 0.38 (-0.03, 0.97). That is, suicidal ideation was expected to increase by 0.35 for every unit increase in ISI through ISI's effect on DDNSI. The total indirect effect is 0.73 (0.18, 1.44). The direct effect of ISI (the effect of ISI on suicidal ideation after adjusting for DDNSI and DBAS) is −0.09 (-0.75, 0.56). We then assessed the relationship between patient covariates and suicidal ideation. Of the patient characteristics in Table 1, only age was significantly associated with suicidal ideation univariately (and also using forward and backward stepwise algorithms). Both PHQ and BHS were univariately associated with suicidal ideation. However, in a joint model including age, PHQ, and BHS, only BHS remained statistically significant. Results of separate mediation models adjusting for age and BHS are also shown in Table 4 and are similar to the unadjusted results. In all models, the direct effect of ISI after adjusting for DDNSI and DBAS was nonsignificant. The indirect effect of ISI through DDNSI remained statistically significant, while the mediation effect of DBAS remained borderline significant.
Table 4.
Mediation results of the effect of ISI on Suicidal Ideation through DDNSI and DBAS
DISCUSSION
The primary goal of this study was to define the mediation of the effect of insomnia on suicidal ideation. Our prior research, and that of others, has reported that overall insomnia severity is related to suicidal ideation. While all of the psychometric predictor variables, including depression severity, hopelessness, and the three sleep variables (ISI, DBAS, and DDNSI) were related to Scale for Suicide Ideation scores in univariate analyses, remarkably, none of the sleep variables were related to hopelessness. This suggests that the three measures of sleep distress represent a different construct than what is included in the classic conceptualization of hopelessness.
We found that the effect of insomnia symptoms is mediated by dysfunctional beliefs and attitudes about sleep and by nightmares. That is, insomnia symptoms appear indirectly related to suicidal ideation through their effect on DDNSI and DBAS. Insomnia symptoms per se were not a significant predictor when dysfunctional beliefs and attitudes about sleep plus nightmares were included in the model. If true, our findings present novel targets for suicide prevention, including targeted treatments for nightmares and dysfunctional beliefs and attitudes about sleep.
Treatment approaches for these targets might include either pharmacological or psychological approaches. Dysfunctional beliefs and attitudes about sleep have been shown to be modified by cognitive behavior therapy for insomnia (CBT-I). While hypnotic medications have not been convincingly shown to modify dysfunctional beliefs and attitudes about sleep, it is plausible that hypnotic medications might modify beliefs about sleep indirectly by sustained relief of insomnia symptoms. Because of overdose risk, any use of hypnotics in depressed, suicidal insomniacs would require great caution, and some authors have reported an increased association of suicidal ideation with hypnotic use.31
This study has several limitations. The first is the use of a convenience sample, which, while providing us with a range of suicidal ideation score, is not representative of any one group, nor is it a random sample of the general population. A second limitation is the cross-sectional measurement, which prevents statements of causality between the sleep variables and suicidal ideation. A third limitation is the wide but uneven use of psychotropic medications, which have unpredictable effects on sleep and suicidal ideation. While it is conceivable that data could have been collected on medication free outpatients, it seems unlikely that medication-free status could be achieved for inpatients or ED patients. A fourth limitation is the ascertainment of diagnosis by chart review and PHQ-9 definitions. A structured interview for diagnosis would be preferred.
In summary, we have again confirmed a positive association between insomnia symptoms and suicidal ideation in depressed patients. We have extended and clarified our earlier findings in two ways, by showing that: (1) the relationship between insomnia and suicidal ideation extends to patients who are experiencing emergent suicidal risk, and (2) nightmares as well as dysfunctional beliefs and attitudes about sleep may each mediate part of the previously observed association between insomnia and suicidal ideation.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. McCall has consulted for Sunovion and Astra Zeneca. The other authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: a systematic review. JAMA. 2005;294:2064–74. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 2.Maris R. Suicide. Lancet. 2002;360:319–26. doi: 10.1016/S0140-6736(02)09556-9. [DOI] [PubMed] [Google Scholar]
- 3.Coryell W, Young EA. Clinical predictors of suicide in primary major depressive disorder. J Clin Psychiatry. 2005;66:412–417. doi: 10.4088/jcp.v66n0401. [DOI] [PubMed] [Google Scholar]
- 4.Brown GK, Beck AT, Steer RA, Grisham JR. Risk factors for suicide in psychiatric outpatients: a 20-year prospective study. J Consult Clin Psychol. 2000;68:371–7. [PubMed] [Google Scholar]
- 5.Hall R, Platt D, Hall R. Suicide risk assessment: a review of risk factors for suicide in 100 patients who made severe suicide attempts. Psychosomatics. 1999;40:18–27. doi: 10.1016/S0033-3182(99)71267-3. [DOI] [PubMed] [Google Scholar]
- 6.Oquendo M, Malone K, Mann JJ. Suicide: risk factors and prevention in refractory major depression. Depress Anxiety. 1997;5:202–11. [PubMed] [Google Scholar]
- 7.Oquendo M, Mann JJ. Intervention research for suicidal behavior. Lancet. 2003;362:844–5. doi: 10.1016/S0140-6736(03)14347-4. [DOI] [PubMed] [Google Scholar]
- 8.McCall WV. Insomnia is a risk factor for suicide - what are the next steps? Sleep. 2011;34:1149–50. doi: 10.5665/SLEEP.1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fujino Y, Mizoue T, Tokui N, Yoshimura T. Prospective cohort study of stress, life satisfaction, self-rated health, insomnia, and suicide death in Japan. Suicide Life Threat Behav. 2005;35:227–37. doi: 10.1521/suli.35.2.227.62876. [DOI] [PubMed] [Google Scholar]
- 10.McCall WV, Blocker JN, D'Agostino R, Jr, et al. Insomnia severity is an indicator of suicidal ideation during a depression clinical trial. Sleep Med. 2010;11:822–27. doi: 10.1016/j.sleep.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McCall WV, Blocker JN, D'Agostino RB, Jr, et al. Treatment of insomnia in depressed insomniacs: effects on health-related quality of life, objective and self-reported sleep, and depression. J Clini Sleep Med. 2010;6:322–9. [PMC free article] [PubMed] [Google Scholar]
- 12.Espie C, Inglis S, Harvey L, Tessier S. Insomniacs' attributions: psychometric properties of the dysfunctional beliefs and attitudes about sleep scale and the sleep disturbance questionnaire. J Psychosom Res. 2000;48:141–8. doi: 10.1016/s0022-3999(99)00090-2. [DOI] [PubMed] [Google Scholar]
- 13.Morin C, Stone J, Trinkle D, Mercer J, Remsberg S. Dysfunctional beliefs and attitudes about sleep among older adults with and without insomnia complaints. Psychol Aging. 1993;8:463–7. doi: 10.1037//0882-7974.8.3.463. [DOI] [PubMed] [Google Scholar]
- 14.Carney CE, Edinger Jack D. Identifying critical beliefs about sleep in primary insomnia. Sleep. 2006;29:444–53. [PubMed] [Google Scholar]
- 15.Carney C, Edinger J, Manber R, Garson C, Segal Z. Beliefs about sleep in disorders characterized by sleep and mood disturbance. J Psychosom Res. 2007;62:179–88. doi: 10.1016/j.jpsychores.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 16.Allen R, Picchietti D, Hening WA, Trenkwalder C, Walters A, Montplaisir J. Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology: a report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med. 2003;4:101–19. doi: 10.1016/s1389-9457(03)00010-8. [DOI] [PubMed] [Google Scholar]
- 17.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beck A, Steer R. Beck Hopeless Scale Manual. New York: Psychological Corporation; 1988. [Google Scholar]
- 19.Steer R, Beck A. Use of the Beck Depression Inventory, Hopelessness Scale, Scale for Suicidal Ideation, and Suicidal Intent Scale with Adolescents. Adv Adolesc Mental Health. 1988;3:219–31. [Google Scholar]
- 20.Beck A, Brown G, Berchick R, Stewart B, Steer R. Relationship between hopelessness and ultimate suicide: A replication with psychiatric outpatients. Am J Psychiatry. 1990;147:190–5. doi: 10.1176/ajp.147.2.190. [DOI] [PubMed] [Google Scholar]
- 21.Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 22.Morin C, Vallieres A, Ivers H. Dysfunctional beliefs and attitudes about sleep (DBAS): validation of a brief version (DBAS-16) Sleep. 2007;30:1547–54. doi: 10.1093/sleep/30.11.1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Belanger L, Vallieres A, Ivers H, Moreau V, Lavigne G, Morin CM. Meta-analysis of sleep changes in control groups of insomnia treatment trials. J Sleep Res. 2007;16:77–84. doi: 10.1111/j.1365-2869.2007.00566.x. [DOI] [PubMed] [Google Scholar]
- 24.Krakow B, Schrader R, Tandberg D, et al. Nightmare frequency in sexual assault survivors with PTSD. J Anxiety Disord. 2002;16:175–90. doi: 10.1016/s0887-6185(02)00093-2. [DOI] [PubMed] [Google Scholar]
- 25.Bernert R, Joiner T, Cukrowicz K, Schmidt N, Krakow B. Suicidality and sleep disturbances. Sleep. 2005;28:1135–41. doi: 10.1093/sleep/28.9.1135. [DOI] [PubMed] [Google Scholar]
- 26.Bernert R, Reeve J, Perlis M, Joiner T. Insomnia and nightmares as predictors of elevated suicide risk among patients seeking admission to emergency mental health facility. Sleep. 2009;32:A365–6. [Google Scholar]
- 27.Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. 1979;47:343–52. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- 28.Beck AT, Brown GK, Steer RA. Psychometric characteristics of the Scale for Suicide Ideation with psychiatric outpatients. Behav Res Ther. 1997;35:1039–46. doi: 10.1016/s0005-7967(97)00073-9. [DOI] [PubMed] [Google Scholar]
- 29.Hayes AF. Beyond Baron and Kenny: statistical mediation analysis in the new millennium. Commun Monogr. 2009;76:408–20. [Google Scholar]
- 30.Preacher K, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Beh Res Methods. 2008;40:879–91. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 31.Perlis R, Purcell S, Fava M, et al. Association between treatment-emergent suicidal ideation with citalopram and polymorphisms near cyclic adenosine monophosphate response element binding protein in the STAR*D study. Arch Gen Psychiatry. 2007;64:689–97. doi: 10.1001/archpsyc.64.6.689. [DOI] [PubMed] [Google Scholar]