Abstract

The purpose of this literature review is to determine the current state of the science for the effectiveness of patient navigation on improving outcomes of cancer care across the continuum among Native Americans. The research will help healthcare professionals ascertain potential evidence-based practice guidelines and gaps in knowledge, which may provide direction for future research. Data synthesis included the use of Native navigation for cancer care, which has been demonstrated in limited, nonrandomized studies to improve cancer knowledge, access to care, and quality of life for Native Americans. Those studies had limitations, including small sample size, self-report of outcome measures, and lack of randomization. Evidence is insufficient to conclude that the use of Native navigation is superior to usual cancer care for Native American patients. Oncology nurses have a role in training personnel to serve as cancer navigators. Nurses need to be supportive of culturally appropriate navigation programs and know about services provided by navigators. In addition, nurse educators need to encourage Native Americans in their communities to consider choosing nursing as a profession. If an oncology nurse has an interest in research, opportunities exist to assist with or conduct research projects regarding Native cancer navigation. A particular need exists for addressing the gaps in research identified in this article.
Cancer burden continues to escalate among Native Americans (NAs) (Cobb, Wingo, & Edwards, 2008). Burden includes multiple ways cancer affects the family, such as loss of income from the patient, when family members move home to serve as caregivers, and increased time and money needed for transportation to and from healthcare facilities that provide cancer care. Disparities in cancer incidence and mortality, as well as increasing cancer burden, necessitate interventions to improve access of American Indian/Alaska Native (AIAN) patients to prevention and treatment services to decrease cancer burden.
Patient navigation programs offer one avenue for delivery of cancer screening and other services, but their success among specific cultural groups often hinges on innovative and culturally appropriate approaches (Edwards et al., 2010). Examining the literature about patient navigation programs successfully implemented within AIAN communities may provide the basis for future culturally relevant evidence-based models. Therefore, the purpose of this review is to determine the current state of the science for the effectiveness of patient navigation on improving outcomes of cancer care across the continuum among NAs. The search strategy included a review of cancer-related patient navigation programs published in peer-reviewed journals or online to ascertain potential evidence-based practice guidelines and gaps in knowledge that may provide direction for future research.
Background and Significance
NA refers to both American Indians and Alaska Natives (see Figure 1). Disparities in health care began when NAs relinquished their lands to the federal government in the past for the promise of health care (Dixon & Roubideaux, 2001). Health care for NAs has never been funded at a level comparable to that of other Americans (Dixon & Roubideaux, 2001). Limited access to health care has had serious consequences in the health status of NAs, including the high cancer incidence and mortality rates.
FIGURE 1.

Terminology
American Indian and Alaska Native Cancer Disparities
Cancer incidence rates vary among AIAN populations and often differ from rates among non-Hispanic Whites (NHWs) (Wiggins et al., 2008). For all cancer sites combined, AIAN incidence rates are higher than NHW rates among men and women in the Northern and Southern Plains and in Alaska. AIANs are more likely to be diagnosed in more advanced disease stages and less likely to take part in early detection programs. Such data differences are probably not explained by race misclassification (Wiggins et al., 2008). Cancer incidence among some sites, such as colorectal cancer, is increasing most rapidly among AIAN compared to all other racial and ethnic groups (Edwards et al., 2010). AIAN colorectal cancer incidence rates varied almost five-fold regionally, from 21 per 100,000 in the Southwest to 102.6 in Alaska (Perdue et al., 2008). Among staged cancers, 67% of AIANs were diagnosed at late-stage colorectal cancer compared with 60% of NHWs; AIAN men and women were more likely to have late-stage colorectal cancer at diagnosis in each region (Perdue et al., 2008). AIAN women had higher rates of cervical cancer than NHW women and were more likely to be diagnosed with later-stage disease (Becker et al., 2008). AIAN women had lower rates of breast cancer than NHW women, but the highest rates for AIANs were in Alaska (134.8 per 100,000), the Northern Plains (115.9), and the Southern Plains (115.7) (Wingo et al., 2008). AIAN women were more likely to be diagnosed with late-stage disease. AIAN men from the Northern Plains region and AIAN women from Alaska and the Northern and Southern Plains regions had higher cancer incidence rates than NHWs in the same areas (Espey et al., 2007; National Cancer Institute [NCI], 2007). Thus, in specific regions of the country, Natives are not experiencing the decreases in cancer incidence that are occurring among other racial groups (Jemal et al., 2004; U.S. Department of Health and Human Services, 2000) (see Table 1).
TABLE 1.
AIAN Age-Adjusted Cancer Incidence, 1999–2003
| Variable | All Cancer Sites
|
Breast
|
Cervix
|
Colorectal
|
Lung
|
Prostate
|
|||
|---|---|---|---|---|---|---|---|---|---|
| Female | Male | Female | Female | Female | Male | Female | Male | Male | |
| CHSDA AIAN | 334.8 | 406.9 | 84.7 | 9.4 | 41.6 | 51.5 | 48 | 68 | 104 |
|
| |||||||||
| NHW | 425.8 | 553.5 | 134.8 | 7.5 | 43.8 | 60.4 | 59.2 | 87.6 | 154.7 |
|
| |||||||||
| AN | 511 | 543.3 | 139.5 | 9.2 | 106.2 | 98.5 | 78.9 | 116.5 | 82.1 |
|
| |||||||||
| NHW | 415.3 | 569 | 135.6 | 6 | 40.6 | 61.4 | 59.9 | 84.8 | 179.9 |
|
| |||||||||
| Northern Plains AI | 468.1 | 611.4 | 112.2 | 11.3 | 60.4 | 79.8 | 97.4 | 115.5 | 164.6 |
|
| |||||||||
| NHW | 413.3 | 542.5 | 130.5 | 7.5 | 45.3 | 62 | 52 | 86.7 | 160 |
|
| |||||||||
| Southern Plains AI | 439.2 | 568.2 | 115.2 | 14.1 | 54.4 | 68.9 | 68.8 | 108.7 | 156.9 |
|
| |||||||||
| NHW | 403.7 | 549.3 | 130 | 9.2 | 43.4 | 63.5 | 62.9 | 109.1 | 146.6 |
|
| |||||||||
| Pacific Coast AI | 292.7 | 333 | 74.5 | 6.9 | 34.8 | 44 | 47 | 56.5 | 83.1 |
|
| |||||||||
| NHW | 437.5 | 556.8 | 142.5 | 7 | 42 | 56.4 | 60.9 | 82.4 | 160.4 |
|
| |||||||||
| East AI | 258.3 | 286.3 | 69.1 | 8.2 | 34.6 | 35.5 | 45.2 | 45.4 | 82.9 |
|
| |||||||||
| NHW | 435.1 | 578.4 | 132.8 | 7.7 | 46.9 | 65.9 | 61.3 | 94.5 | 156.3 |
|
| |||||||||
| Southwest AI | 219.3 | 261.5 | 50.4 | 7.9 | 17.6 | 26.7 | 10.3 | 22.1 | 67 |
|
| |||||||||
| NHW | 404.3 | 513.1 | 127.2 | 7.5 | 40.3 | 56.1 | 56.9 | 78.1 | 136.7 |
AI—American Indian; AN—Alaska Native; CHSDA—Contract Health Service delivery area; NHW—Non-Hispanic White
Note. Based on information from Espey et al., 2007.
Similar patterns of disparity are seen in the mortality data. From 1997–2006, short-term trends in death rates for all cancers combined decreased for all racial or ethnic groups for men and women, except for AIAN women (Edwards et al., 2010). According to the 2008 Indian Health Service (IHS) data (Edwards et al., 2010), regional differences exist for most cancer sites, with Alaska and the Northern and Southern Plains having elevated mortality compared to other AIs living in the 48 contiguous states (see Figure 2).
FIGURE 2.
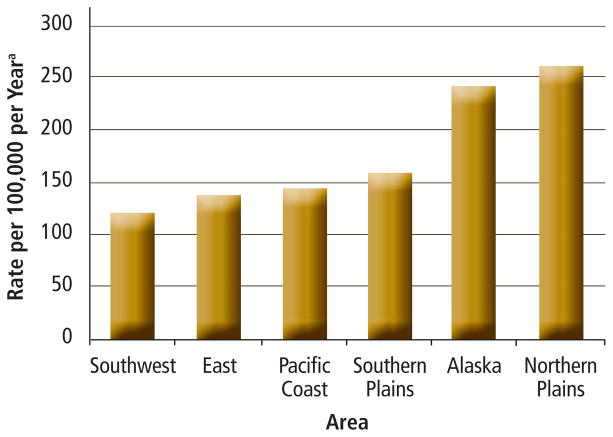
All Site Cancer Mortality Rates, Both Genders, 1999–2003
Note. From Cancer Mortality Among American Indians and Alaska Natives: Regional Differences, 1999–2003 (p. 19), by D. Haverkamp, D. Espey, R. Paisano, and N. Cobb, 2008, Rockville, MD: Indian Health Service.
a Adjusted to 2000 U.S. population
Note. The rate for the entire Indian Health Service is 169.9, which is significantly lower than the all-U.S. rate of 195.7.
Late-stage cancer at diagnosis is associated with limited survival. Causes of disparity in late-stage cancer diagnosis vary by site, but may include factors related to low socioeconomic status (e.g., health insurance, income, education) or related demographic attributes (e.g., age, gender, racial or ethnic minority). That association supports the need for continued development of early detection and stage-appropriate treatment strategies, as well as expanded efforts to ensure that all Americans have equal access to these life-saving interventions (Edwards et al., 2010). AIAN populations are more likely to live in poverty and less likely to have a high school education and health insurance compared to NHW, all indicators of less access to cancer prevention and control services (Edwards et al., 2010).
Provision of Health for Native Americans
Discussing provision of health for Native Americans is important for two primary reasons. First, such a discussion can be helpful in illustrating how limited access to and resources for care may negatively impact the cancer health status of AIANs. Second, it shows how complex the healthcare system is for AIAN patients; cancer care can be complex and confusing for any patient, but AIAN patients who need to deal with multiple systems can get lost easily.
IHS provides variable support for direct healthcare services through IHS/Tribal/Urban Indian clinics in the United States. Per capita expenditures in the 2003 federal budget for AIAN in the IHS were $1,914 compared to $3,879 for Medicare recipients and $3,803 for federal inmates (U.S. Commission on Civil Rights, 2004). The funding disparity continued. In 2009, AIAN patients in the IHS system received 55% of the per capita healthcare funding needed (IHS, 2009). In the same year, the Indian Health Care Improvement Fund (IHCIF) was allocated to raise all IHS and tribal sites to 40%, as directed by Congress. IHCIF allocation is based on the Federal Employees Health Plan Disparity Index (FDI), an index to compare IHS funding to the cost of providing medical insurance for AIAN users in mainstream health insurance plans, such as the Federal Employees Health Benefits program. In 2009, the FDI ranged from 43% in Bemidji Area, MN to 64% in Nashville, TN. In addition, NAs face a lack of funding provided by Congress to support IHS Contract Health Service (CHS). Several articles described the underfunding of IHS CHS and cancer care (Burhansstipanov, 2000, 2001, 2006; Burhansstipanov, Gilbert, LaMarca, & Krebs, 2001; Burhansstipanov & Olsen, 2001; Edwards et al., 2010; Espey et al., 2007).
Cancer Patient Navigation
The cancer continuum is the medical and non-medical trajectory of the experience of cancer, including cancer prevention, detection, diagnosis, treatment, and survivorship (NCI, n.d.a). Patients with cancer may experience a variety of barriers during each phase of the cancer continuum (Burg et al., 2010; Freeman & Chu, 2005; Strzelczyk & Dignan, 2002). Patient navigation is a strategy of employing trained individuals to assist others in navigating the healthcare system to receive needed education and services, a process by which an individual (i.e., patient navigator) provides outreach and education, ensures access to screening examinations, and guides patients with a suspicious finding (e.g., test shows they may have cancer) through and around barriers in the complex cancer care system to help ensure timely diagnosis and treatment (Freeman, 2004). Patient navigation began in the 1980s in Harlem, NY, mainly with African American women with breast cancer (Freeman & Chu, 2005). Navigation has been successful in assisting patients, survivors, families, and caregivers in overcoming barriers to cancer care (Battaglia, Roloff, Posner, & Freund, 2007; Dohan & Schrag, 2005; Ell, Vourlekis, Lee, & Xie, 2007; Freeman & Chu, 2005; Percac-Lima et al., 2009).
A key for successful navigation is cultural competency (Banner et al., 1995; Freeman, 2004; Matsunaga et al., 1996; Petereit et al., 2008). Because those who are part of the community served know the cultures of the community best, it has been a successful strategy to train community members to become navigators (Banner et al., 1995; Burhansstipanov, Christopher, & Schumacher, 2005; Burhansstipanov, Dignan, Bad Wound, Tenney, & Vigil, 2000; Freeman, 2004; Gotay et al., 2000; Matsunaga et al., 1996). Navigators may or may not have nursing backgrounds or education. Trained lay health workers are less costly than professional healthcare workers, and often are viewed as more approachable to community members (Freeman, 2006). Clinical navigators may have easier access to clinical settings. Advantages and disadvantages exist for navigators who are hired or work from a clinical setting compared to those who are hired or work from community-based organizations (see Table 2).
TABLE 2.
Examples of Advantages and Disadvantages of Where Navigators Work
| Factor | Clinical Setting
|
Community-Based Setting
|
||
|---|---|---|---|---|
| Advantages | Disadvantages | Advantages | Disadvantages | |
| Cultural skills and language | Typically some cultural awareness and skills | Although required by law, clinical settings are unable to address the multitude of languages used by patients. | Tailored, appropriate cultural interventions, interactions, and communication patterns acceptable to the patients | Cannot provide 24/7 cultural or Native language speaker services |
|
| ||||
| Access to screening and follow-up services | Usually has a long-term or established relationship with the clinics that provide screening, diagnosis, or follow-up care. | Internal politics of other healthcare providers who feel they have already been implementing the navigator duties | Flexibility to work with patients and help them attain help regardless of the service provider | Need formal agreements with healthcare facilities to be able to access services |
|
| ||||
| Protocols | Protocols usually clearly specified (i.e., who, what, when, where, how, and how often) | Protocols may not be adaptable to meet the needs of patients or families | May or may not include protocols for how the Native navigator is to interact with patients and families | Intermittent funding likely to interfere with training and continuity of navigation services |
|
| ||||
| Health benefits for navigators | Usually access to higher-quality benefits for the navigator (e.g., insurance) | Many of the navigators are expected to work for no salary or benefits. | Native navigators are paid and some may receive benefits, depending on number of hours worked. | Some community-based organizations are unable to provide benefits. |
|
| ||||
| Transportation | Drivers (Community Health Representative if Indian Health Service/Tribal/Urban program) or access to a free clinical transportation system | Intermittent schedules and may not go to the communities where American Indians and Alaska Natives live | Some Native navigators have coverage to protect them in case of accidents when they pick up and transport patients and family members. | Many community-based organizations cannot provide supplemental automobile coverage. |
|
| ||||
| Child care | Some clinics have a children’s play area with toys or videos. | Play area may be located away from patients; no super vision unless a family member watches the children | Children typically welcome in any Native setting | May not be a play area or supervision if family member or staff member is not available to watch children |
|
| ||||
| Mobile van versus mammogram from clinic | If the van is from the clinic, films are delivered directly to the radiologist for reading. | Back-log of films for the radiologist to read; mobile films frequently put at the bottom of the pile | Van goes to Indian Health Service/Urban/Tribal clinics where patients feel the most comfortable; Native navigator can accompany them up until the mammogram is done; Native women blessing the equipment and women before and after screening | Vans must do about 18 mammograms a day to break even on their costs. Fewer vans exist because of cost; when a van does more than 20 screenings a day, later ones frequently have more errors and women have to come back for follow-up |
Note. From Native Sister/Patient Navigation: American Indian/Alaska Native (p. 2), by B. Seals and L. Burhansstipanov, 2008, Lakewood, CO: Native American Cancer Research. Copyright 2008 by Native American Cancer Research. Reprinted with permission.
Successful patient navigation programs combine community and culturally sensitive care, often employing community members of the same ethnicity and culture as those they serve to become trained as navigators (Freeman & Chu, 2005; Vargas, Ryan, Jackson, Rodriguez, & Freeman, 2008). In NA communities, this is a particularly critical consideration because of a history of devastation from conquest and forced assimilation at the hands of outsiders (Shelton, 2001). The term Native navigator in this article refers to an NA who assists a person in an NA community in navigating the healthcare system across the cancer continuum (i.e., “Native navigation”). This is a particularly appropriate strategy for NAs, who have a historical mistrust of outsiders (Christopher, Watts, McCormick, & Young, 2008; Deloria, 1974; Dixon & Roubideaux, 2001).
Methods
The authors performed a systematic review to synthesize the published research literature to determine the current state of the science for use of patient navigations among NAs. Ovid MEDLINE® and Nursing databases, as well as EBSCOhost Health Source: Nursing/Academic Edition were searched with no limit on a start date (earliest records for MEDLINE start in 1950) through November 2010 using the following keywords: Native American, American Indian, Alaska Native, navigator, community health worker, lay health worker, minority, and cancer. The authors focused on studies that examined outcomes of navigation for NA patients with cancer. Patients of all ages were included. In addition, studies on navigation for all phases of the cancer continuum of care were included. Criteria for inclusion of literature in the current analysis were (a) based in an NA community, (b) focused on any type of cancer, (c) along any portion of the cancer continuum, (d) had some type of comparison (could include evaluation studies and descriptive studies), (e) included any age group, (f) included any gender, (g) contained navigation within the intervention, and (h) published in a peer-reviewed journal or online. Commentaries, letters to the editor, and program descriptions without mentioning of evaluation of navigation outcomes were excluded. In addition, articles not written in English were excluded.
A total of 98 articles were found using relevant combinations of the keywords. However, most of those related to patient navigation with other populations. The first published article relating to Native cancer navigation appeared in 1998 (Burhansstipanov et al., 1998). Each eligible article was reviewed by the first author. The reviewer abstracted data on study design, participant characteristics, study setting, continuum of care phase addressed, outcome measures, and findings, including navigation type. Studies were categorized into experimental and observational studies.
During the review, the following information about participants were noted: age, gender, and other demographic characteristics; cancer type; and other comorbidity. The setting referred to geographic area and urban or rural status. Navigators were categorized into lay health workers, nurse navigators, and other. In addition, the phase of continuum of care and type of navigation services provided were noted. Finally, for outcome measures and findings, data collection and measurement methods and major findings related to effectiveness of navigation were examined. That information was used to assess the strengths and limitations of each study examined.
Relevant Literature
Nine documents were retrieved regarding Native navigation, including one that referred to a navigation project in Washington, D.C. (Robinson-White, Conroy, Slavish, & Rosenzweig, 2010). Information about that project was located in a final project report on the research project’s Web site (Warren-Mears & Ramsey, 2007). Thus, only eight peer-reviewed articles from the literature search contained information regarding the use of cancer navigation for NAs (see Table 3).
TABLE 3.
Summary of Published Articles Pertaining to Native Cancer Navigation
| Study | Design, Sample, and Setting | Cancer Continuum Phase | Outcome Measure | Findings | Study Authors’ Comments |
|---|---|---|---|---|---|
| Burhansstipanov et al., 1998 | Descriptive, comparative survey; described role and duties of Native Sisters N not specified; Native American women in Los Angeles, CA and Denver, CO |
Education, screening, and follow-up for diagnosis | Participants completed a one-page inventory assessing strategies or factors improving screening | Role of Native Sisters listed by patients as most effective factor in improving screening mammography 90% of patients were being rescreened as recommended by providers. |
Encouraged providers to create culturally appropriate navigator protocols for their communities |
| Burhansstipanov et al., 2000 | Descriptive, comparative 71 American Indian women in Denver, CO |
Education, screening, and follow-up for diagnosis | Recruitment of women to mammography screening Questionnaire completed on screening day asssessing demographic information, cancer history, and factors related to decision to obtain mammography |
Native Women’s Wellness Through Aware ness project increased recruitment of American Indian women (p < 0.05) compared to time period prior to implementation of the program. | Future efforts to increase participation of American Indian people in cancer screening need to include recognition of American Indian values and lifestyle. |
| Burhansstipanov et al., 2010 | Descriptive, comparative survey; tested use of face-to-face and telephone navigation by trained navigators 313 Caucasian, African American, Latina, and Native American women from Denver, CO; 113 received navigator intervention and follow-up survey |
Education, screening, follow-up for diagnosis, treatment, follow-up care, and support | Self-report survey of rescreening mammogram | 55% of those receiving intervention had rescreening mammogram (p < 0.000). Associations between receiving intervention and reporting rescreening mammogram for all racial or ethnic groups (p < 0.05) Those who received the intervention obtained mammograms even without provider recommendation. |
Noted that because Native Americans and Latinos rarely have the same provider each year, they are less influenced by provider recommendation for mammograms |
| Christopher et al., 2008 |
Quantitative: One group pretest and post-test interviews of random sample of Apsáalooke (Crow) women Qualitative: Community and university partner experiences, field notes, and meeting minutes 83 American Indian women from the Apsáalooke reservation in Montana |
Education | Interviews and qualitative observations and analysis regarding knowledge, comfort discussing cancer issues, and cervical cancer awareness | No significant increase in Papanicolaou (Pap) test knowledge until those with high pretest scores were eliminated (p < 0.05) Increase in cervical cancer knowledge (p < 0.05) Increase in comfort discussing cancer issues (p < 0.01) Increase in those that had heard of test for cervical cancer (p < 0.01) Increase in those that had heard about cervical health in the past year (p < 0.001) Increase in those that had heard about Messengers for Health (p < 0.001) Program widely accepted, women saying “Pap test” and “cervix” more now, and women asking for Pap tests |
Emphasizes value of quantitative and qualitative data to enhance rigor of study Noted limitation of nonexperimental, one-group pretest and post-test design was that it was unable to conclude intervention was successful in achieving outcomes |
| Dignan et al., 2005 | Pretest and post-test survey with random assignment to face-to-face or telephone navigation by Native Sisters; compared to Colorado Mammography Program 157 Native American women from Denver, CO received navigator intervention and follow-up survey. |
Screening | Self-report survey including demographics, history of breast cancer and mammograms, and adherence with recommendations | 29% of sample lost to follow-up. Difference in pretest versus post-test for navigator intervention (p = 0.013) No difference in effectiveness of face-to-face versus telephone navigator intervention (p = 0.83) No significant difference between the intervention and comparison groups (p = 0.1) |
A need exists for improved ability to track participants, as within the 18-month period of study, half the telephone numbers were no longer valid. Attrition may have contributed to the lack of intervention effect. |
| English et al., 2008 | Descriptive pilot project; described building a partnership between tribal community, academic institution, and intertribal organization and the results of intervention (Ramah Navajo Mammography Days) to facilitate mammography 89 women of the Ramah Band of Navajo Indians from West Central, NM, split into (a) focus groups (n = 50) and (b) survey (n = 39) |
Screening |
|
Major themes included awareness, fatalism and fear, taboos, barriers to care, and facilitators to care All participants indicated they would participate in mammography events the next year. Majority cited lunch as the component of the intervention they liked most, followed by transportation, social support, health education, and friendly staff. |
Pointed out that using tribal community health representatives as navigators was so effective that a waiting list developed for the home-visit recruitment effort. Indicated that key intervention aspects incorporated cultural traditions. |
| Petereit et al., 2005 | Prospective, clinical trials; described collaborative between Rapid City Regional Hospital, the University of Wisconsin, the Mayo Clinic, and the American Indian community N not specified; American Indian men and women from Rapid City, SD |
Screening, follow-up for diagnosis, treatment, and follow-up care | Analysis of process, clinical trials participation, treatment outcome, and assessment of access to cancer care at early stage of disease | Patient navigator program developed with use of trained community research representatives Culturally appropriate survey developed to examine barriers to accessing cancer care Educational modules developed for breast and prostate cancer in partnership with Native American Cancer Research Clinical trial protocols have been developed to shorten course of radiation treatment from 6–8 to 1–4 weeks. |
Explained that the long distances Native Americans have to drive for traditional radiotherapy trials makes participation unlikely |
| Petereit et al., 2008 | Retrospective, comparative analysis that measured whether navigated patients undergoing curative radiotherapy had fewer treatment interruptions compared to those who were not navigated 116 American Indian men and women from Rapid City, SD |
Screening, follow-up for diagnosis, treatment, and follow-up care | Missed days of radiotherapy treatment | Those who received navigation had an average of three fewer days of treatment interruptions compared to those who did not (p = 0.002). | Reported positive word-of-mouth communication about navigation as patients returned to their community Emphasized that having fewer missed radiotherapy treatments may lead to increased cure rates |
| Warren-Mears & Ramsey, 2007 | Descriptive, mixed methods; described development, implementation, and evaluation of patient navigation program with a focus on screenable cancers (e.g., breast, cervical, prostate, colorectal) 501 American Indian patients from Idaho, Oregon, and Washington who were navigated |
Screening, follow-up for diagnosis, treatment, and follow-up care | Success of navigator model evaluated via surveys, interviews, and data linkage to clinics and cancer registry | High level of patient and provider satisfaction with navigator program | More extensive studies are need ed to determine whether clinical outcomes can be improved with this navigation model. |
Published studies regarding the use of navigation for cancer care for NAs included Native Sisters (California and Colorado) (Burhansstipanov, 2000; Burhansstipanov et al., 1998, 2010; Burhansstipanov, Krebs, Grass, Wanliss, & Saslow, 2005; Dignan et al., 2005); community health workers as “outreach workers” (New Mexico) (English et al., 2008); Walking Forward (South Dakota) (Petereit et al., 2005, 2008; Rogers & Petereit, 2005); lay health advisors (Montana) (Christopher et al., 2008); and the Northwest Tribal Cancer Navigation Program (Washington state) (Warren-Mears & Ramsey, 2007), which was funded by the Patient Navigation Research Program (NCI, n.d.b).
Data Synthesis
Study Design
The use of Native navigation for cancer care has been demonstrated in limited, nonrandomized studies to improve cancer knowledge, access to care, and quality of life for NAs. One study used a random sample (Christopher et al., 2008). Most of the studies were descriptive or comparative. None of the studies had an experimental design. The existing science is limited because of the lack of rigorous studies.
Minimal financial, equipment, transportation, and personnel resources are available for cancer services, including navigation. To make cancer navigation services available to Native people was an accomplishment in and of itself. Going from the provision of basic cancer navigation services to conducting a randomized, controlled trial is quite a leap. Therefore, descriptive, comparative studies compose the majority of research designs to date.
Grant and Wall (2009) listed five benefits of quasiexperimental research: (a) strengthening causal inference when random assignment and controlled manipulation are not possible or ethical; (b) building better theories of time and temporal progression; (c) minimizing ethical dilemmas of harm, inequity, paternalism, and deception; (d) facilitating collaboration with practitioners; and (e) using context to explain conflicting findings.
When working with AI communities, cultural issues arise with randomization. For instance, many Native communities are close-knit, and a danger exists of those in the intervention group interacting with and influencing those in the control group. Thus, multisite trials are necessary so that contamination and threats to internal validity are minimized.
In addition, because many AI communities lack adequate access to cancer care, it usually would be unethical to withhold a navigation intervention for the entire length of a study. Thus, a quasiexperimental design, such as a controlled, delayed intervention trial, would offer the most internal and external validity.
Sample and Setting
Only two of the studies had relatively large sample sizes: 313 in Burhansstipanov et al. (2010) and 501 in Warren-Mears and Ramsey (2007). The samples included are from only eight states in the United States. Because of differences in Native cultures and health practices, findings may exist that vary depending on tribal location. In addition, of interest from examination of the completed studies are the limited sample characteristics. All of the studies included women; in fact, many of the samples included women only. None of the research conducted included children. None of the studies focused on caregivers or the family of cancer survivors and how navigation might assist them.
Location on Cancer Continuum
Gaps exist as to where the focus of the study lies on the cancer continuum. The focus of most published studies regarding Native navigation centers on cancers that include screening, which leaves a large research gap for the navigation of cancers for which screening does not exist. No studies included end-of-life care. Only two of the studies included supportive care (Burhansstipanov et al., 2010; Warren-Mears & Ramsey, 2007).
Outcome Measures
The outcome measures for the studies included information related mainly to breast cancer and mammography. That information included recruitment (Burhansstipanov et al., 2000); screening (Burhansstipanov et al., 2000; Dignan et al., 2005; English et al., 2008); rescreening (Burhansstipanov et al., 2010); and knowledge, beliefs, and attitudes toward screening (English et al., 2008); as well as perceived barriers and facilitators to screening (Burhansstipanov et al., 1998).
Petereit et al. (2005) reported fewer days of radiation treatment interruption for those receiving navigation, and described the development of a collaborative navigator program with educational modules developed for prostate and breast cancer (Petereit et al., 2008). Burhansstipanov et al. (2010) compared mammography rates for women receiving telephone versus in-person navigation, as well as rescreening for those receiving the navigator intervention compared to those who were not.
One study investigated cervical cancer and Papanicolaou (Pap) test knowledge, comfort talking about cancer issues, and cervical cancer awareness (Christopher et al., 2008). Warren-Mears and Ramsey (2007) described patient and provider satisfaction with patient navigation for screening, follow-up for diagnosis, treatment, and follow-up care for breast, prostate, colorectal, and cervical cancer, and included patients with lung cancer as well as “other” or “unknown” cancers.
Outcome measures were ascertained largely through self-report surveys, as well as interviews. Only one study used data linkage with local clinics and a cancer registry (Warren-Mears & Ramsey, 2007).
Findings
Native navigation has been shown to increase recruitment (Burhansstipanov et al., 2000) screening (Burhansstipanov et al., 2000; Dignan et al., 2005; English et al., 2008), rescreening (Burhansstipanov et al., 2010), and perceived barriers and facilitators to screening (Burhansstipanov et al., 1998) regarding breast cancer. Increases in knowledge were observed regarding Pap tests and cervical cancer, in addition to comfort talking about cancer issues and awareness of cervical cancer issues (Christopher et al., 2008). Burhansstipanov et al. (2010) found no difference in mammography for women receiving telephone versus in-person navigation. However, 55% of those receiving the navigator intervention had a statistically significant difference in receiving rescreening compared to those who were not navigated.
Native navigation was shown to lead to three fewer days of treatment interruption for radiotherapy (Petereit et al., 2008). Warren-Mears and Ramsey (2007) reported high levels of patient and provider satisfaction with patient navigation. However, those studies had limitations, including small sample size, self-report of outcome measures, and lack of randomization.
Implications for Oncology Nursing
Oncology nurses have a role in training personnel to serve as cancer navigators. Those personnel can have a variety of backgrounds; they may be licensed nurses, nursing assistants, community health representatives, ancillary healthcare personnel, and even lay people who want to enter the healthcare field as navigators. Training can include anatomy and physiology; cancer screening, diagnosis, treatment, and supportive care; major types of cancers; palliative care; nutrition; and exercise. Thus, even if a nurse is not a navigator, the opportunity exists to provide education in areas with which the nurse is familiar. The content of the current article could be rewritten for a PowerPoint© presentation format to be used in recruitment sessions to attract motivated NA lay people to become trained as navigators. Including examples of how the navigator model works in other ethnic communities also may encourage NA communities to develop such a care delivery model.
Oncology nurses need to be supportive of culturally appropriate navigation programs. Oncology nurses who serve NAs need to be familiar with the cultural practices and beliefs of the Native people of the area. When a nurse interacts with Native navigators, questions about culture may be asked of the navigators, who often live the culture. Respect for local cultures by nurses will serve to strengthen the relationship with navigators, as well as Native patients who are served.
Nurses also need to be knowledgeable about services provided by navigators. The services offered may differ, depending on whether navigators work in hospitals or community settings. In some large medical centers, multiple navigators of differing educational backgrounds may be serving in specialty cancer clinics. Contact information for the navigators should be made available to share with patients as needed.
Oncology nurse educators need to encourage NAs in their communities to consider choosing nursing as a profession. They may provide support and share resources with them, including scholarship opportunities, and offer mentoring. In addition, if an oncology nurse has an interest in research, opportunities exist to assist with or conduct research projects regarding Native cancer navigation. A particular need exists for addressing the gaps in research identified in the current article.
Conclusions
The majority of research designs have been descriptive, comparative studies. A need exists for a more robust study design. Because of ethical considerations, as well as those pertaining to internal and external validity, a multisite delayed-intervention trial is proposed, rather than a randomized, controlled clinical trial.
Limited examination exists of Native people from various geographic areas of the United States. A need exists to test Native navigation in areas other than California, Colorado, Idaho, Montana, New Mexico, Oregon, South Dakota, and Washington state. For instance, none of the interventions reviewed in the current article took place in the Southern Plains, an area that has cancer incidence rates almost as high as those of the Northern Plains. Unique characteristics may exist that facilitate or impede successful implementation of Native navigation in the Southern Plains, and tailoring culturally relevant interventions for this community may be necessary.
Few outcome measures have been examined, which indicates a need to examine other vital outcome measures of Native navigation, such as cost effectiveness, time from screening to diagnosis, and time from diagnosis to treatment. Because other cancers affect AIAN people besides those for which screening is available, examination of the use of Native navigation for other cancers is needed.
Most data was collected from self-report surveys. Limitations exist with self-report surveys, as participants may respond in a way they feel the investigator wishes them to. Therefore, a need exists to use more robust tools to measure outcomes, including medical records data and data linkage with cancer registries.
Insufficient evidence exists to conclude that use of Native navigation is superior to usual cancer care for NA patients. Because of study limitations, evidence-based practice guidelines cannot be provided. In particular, quasiexperimental studies using robust measures need to be conducted in various geographic areas of the United States with patients who have a variety of cancer types across the continuum to compare Native navigation to usual cancer care among NA patients.
Implications for Practice.
Culturally appropriate Native navigation programs need to be supported.
Oncology nurses need to be knowledgeable about services provided by Native navigators in their communities.
Native American community members should be encouraged to consider nursing as a profession to address cancer disparities.
Footnotes
The authors take full responsibility for the content of the article. No financial relationships to disclose. The content of this article has been reviewed by independent peer reviewers to ensure that it is balanced, objective, and free from commercial bias. No financial relationships relevant to this article have been disclosed by the authors, planners, independent peer reviewers, or editorial staff.
Contributor Information
Valerie Eschiti, College of Nursing at the University of Oklahoma Health Sciences Center in Oklahoma City.
Linda Burhansstipanov, Native American Cancer Research in Pine, CO.
Shinobu Watanabe-Galloway, College of Public Health in the Department of Epidemiology at the University of Nebraska Medical Center in Omaha.
References
- Banner RO, DeCambra H, Enos R, Gotay C, Hammond OW, Hedlung N, Tsark JA. A breast and cervical cancer project in a native Hawaiian community: Wai’anae cancer research project. Preventive Medicine. 1995;24:447–453. doi: 10.1006/pmed.1995.1072. [DOI] [PubMed] [Google Scholar]
- Battaglia TA, Roloff K, Posner MA, Freund KM. Improving follow-up to abnormal breast cancer screening in an urban population. A patient navigation intervention. Cancer. 2007;109(2, Suppl):359–367. doi: 10.1002/cncr.22354. [DOI] [PubMed] [Google Scholar]
- Becker TM, Espey DK, Lawson HW, Saraiya M, Jim MA, Waxman AG. Regional differences in cervical cancer incidence among American Indians and Alaka Natives, 1999–2004. Cancer. 2008;113(5, Suppl):1234–1243. doi: 10.1002/cncr.23736. [DOI] [PubMed] [Google Scholar]
- Burg MA, Zebrack B, Walsh K, Maramaldi P, Lim JW, Smolinski KM, Lawson K. Barriers to accessing quality health care for cancer patients: A survey of members of the association of oncology social work. Social Work in Health Care. 2010;49(1):38–52. doi: 10.1080/00981380903018470. [DOI] [PubMed] [Google Scholar]
- Burhansstipanov L. Urban Native American health issues. Cancer. 2000;88(5, Suppl):1207–1213. doi: 10.1002/(SICI)1097-0142 (20000301). [DOI] [PubMed] [Google Scholar]
- Burhansstipanov L. Cancer: A growing problem. In: Dixon M, Roubideaux Y, editors. Promises to keep: Public health policy for American Indians and Alaska Natives in the 21st century. Washington, DC: American Public Health Association; 2001. pp. 223–251. [Google Scholar]
- Burhansstipanov L. American Indian and Alaska Native women and cancer. In: Dow KH, editor. Nursing care of women and cancer. St. Louis, MO: Mosby Elsevier; 2006. pp. 459–471. [Google Scholar]
- Burhansstipanov L, Bad Wound D, Capelouto N, Goldfarb F, Harjo L, Hatathlie L, White M. Culturally relevant “Navigator” patient support. The Native Sisters. Cancer Practice. 1998;6:191–194. doi: 10.1046/j.1523-5394.1998.006003191.x. [DOI] [PubMed] [Google Scholar]
- Burhansstipanov L, Christopher S, Schumacher SA. Lessons learned from community-based participatory research in Indian Country. Cancer Control. 2005;12(Suppl 2):70–76. doi: 10.1177/1073274805012004s10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burhansstipanov L, Dignan MB, Bad Wound D, Tenney M, Vigil G. Native American recruitment into breast cancer screening: The NAWWA project. Journal of Cancer Education. 2000;15(1):28–32. doi: 10.1080/08858190009528649. [DOI] [PubMed] [Google Scholar]
- Burhansstipanov L, Dignan MB, Schumaker A, Krebs LU, Alfonsi G, Apodaca CC. Breast screening navigator programs within three settings that assist underserved women. Journal of Cancer Education. 2010;25:247–252. doi: 10.1007/s13187-010-0071-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burhansstipanov L, Gilbert A, LaMarca K, Krebs LU. An innovative path to improving cancer care in Indian country. Public Health Reports. 2001;116:424–433. doi: 10.1016/S0033-3549(04)50071-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burhansstipanov L, Krebs LU, Grass R, Wanliss EJ, Saslow D. A review of effective strategies for native women’s breast health outreach and education. Journal of Cancer Education. 2005;20(Suppl):71–79. doi: 10.1207/s15430154jce2001s_15. [DOI] [PubMed] [Google Scholar]
- Burhansstipanov L, Olsen SJ. Cancer prevention and early detection in American Indian and Alaska Native populations. In: Frank-Stromborg M, Olsen SJ, editors. Cancer prevention in diverse populations: Cultural implications for the multidisciplinary team. Pittsburgh, PA: Oncology Nursing Society; 2001. pp. 3–52. [Google Scholar]
- Christopher S, Watts V, McCormick AK, Young S. Building and maintaining trust in a community-based participatory research partnership. American Journal of Public Health. 2008;98:1398–1406. doi: 10.2105/ajph.2007.125757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobb N, Wingo PA, Edwards BK. Introduction to the supplement on cancer in the American Indian and Alaska Native populations in the United States. Cancer. 2008;113(5, Suppl):1113–1116. doi: 10.1002/cncr.23729. [DOI] [PubMed] [Google Scholar]
- Deloria V., Jr . Behind the trail of broken treaties: An Indian declaration of independence. Houston, TX: University of Austin Press; 1974. [Google Scholar]
- Dignan MB, Burhansstipanov L, Hariton J, Harjo L, Rattler T, Lee R, Mason M. A comparison of two Native American Navigator formats: Face-to-face and telephone. Cancer Control. 2005;12(Suppl 2):28–33. doi: 10.1177/1073274805012004S05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon M, Roubideaux Y. Introduction. In: Dixon M, Roubideaux Y, editors. Promises to keep: Public health policy for American Indians and Alaska Natives in the 21st century. Washington, DC: American Public Health Association; 2001. pp. xix–xxi. [Google Scholar]
- Dohan D, Schrag D. Using navigators to improve care of underserved patients: Current practices and approaches. Cancer. 2005;104:848–855. doi: 10.1002/cncr.21214. [DOI] [PubMed] [Google Scholar]
- Edwards BK, Ward E, Kohler BA, Eheman C, Zauber AG, Anderson RN, Ries LA. Annual report to the nation on the status of cancer, 1975–2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer. 2010;116:544–573. doi: 10.1002/cncr.24760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ell K, Vourlekis B, Lee PJ, Xie B. Patient navigation and case management following an abnormal mammogram: A randomized clinical trial. Preventive Medicine. 2007;44(1):26–33. doi: 10.1016/j.ypmed.2006.08.001. [DOI] [PubMed] [Google Scholar]
- English KC, Fairbanks J, Finster CE, Rafelito A, Luna J, Kennedy M. A socioecological approach to improving mammography rates in a tribal community. Health Education and Behavior. 2008;35:396–409. doi: 10.1177/1090198106290396. [DOI] [PubMed] [Google Scholar]
- Espey DK, Wu XC, Swan J, Wiggins C, Jim MA, Ward E, Edwards BK. Annual report to the nation on the status of cancer, 1975–2004, featuring cancer in American Indians and Alaska Natives. Cancer. 2007;110:2119–2152. doi: 10.1002/cncr.23044. [DOI] [PubMed] [Google Scholar]
- Freeman HP. A model patient navigation program. Oncology Issues. 2004;19:44–46. [Google Scholar]
- Freeman HP. Patient navigation: A community centered approach to reducing cancer mortality. Journal of Cancer Education. 2006;21(1, Suppl):S11–S14. doi: 10.1007/s11524-006-9030-0. [DOI] [PubMed] [Google Scholar]
- Freeman HP, Chu KC. Determinants of cancer disparities: Barriers to cancer screening, diagnosis, and treatment. Surgical Oncology Clinics of North America. 2005;14:655–669. doi: 10.1016/j.soc.2005.06.002. [DOI] [PubMed] [Google Scholar]
- Gotay CC, Banner RO, Matsunaga DS, Hedlund N, Enos R, Issell BF, DeCambra H. Impact of a culturally appropriate intervention on breast and cervical screening among native Hawaiian women. Preventive Medicine. 2000;31:529–537. doi: 10.1006/pmed.2000.0732. [DOI] [PubMed] [Google Scholar]
- Grant AM, Wall TD. The neglected science and art of quasi-experimentation: Why-to, when-to, and how-to advice for organizational researchers. Organizational Research Methods. 2009;12:653–686. doi: 10.1177/1094428108320737. [DOI] [Google Scholar]
- Indian Health Service. Federal disparity index. 2009 Retrieved from http://www.ihs.gov/nonmedicalprograms/lnf/2008/IHCIFAllAreaAllSites5-8-08.pdf.
- Jemal A, Clegg LX, Ward E, Ries LA, Wu X, Jamison PM, Edwards BK. Annual report to the nation on the status of cancer, 1975–2001, with a special feature regarding survival. Cancer. 2004;101:3–27. doi: 10.1002/cncr.20288. [DOI] [PubMed] [Google Scholar]
- Matsunaga DS, Enos R, Gotay CC, Banner RO, DeCambra H, Hammond OW, Tsark JA. Participatory research in a Native Hawaiian community. The Wai’anae Cancer Research Project. Cancer. 1996;78(7, Suppl):1582–1586. doi: 10.1002/(SICI)1097-0142(19961001)78:7<1582::AID-CNCR37>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute. Continuum of care. n.d.a Retrieved from http://www.cancer.gov/dictionary/?CdrID=561395.
- National Cancer Institute. Patient Navigation Research Program. n.d.b Retrieved from http://crchd.cancer.gov/pnp/pnrp-index.html.
- National Cancer Institute. Annual report to the nation finds cancer death rate decline doubling: Special feature examines cancer in American Indians and Alaska Natives. 2007 Retrieved from http://www.cancer.gov/newscenter/pressreleases/2007/reportnation2007release.
- Percac-Lima S, Grant RW, Green AR, Ashburner JM, Gamba G, Oo S, Atlas SJ. A culturally tailored navigator program for colorectal cancer screening in a community health center: A randomized, controlled trial. Journal of General Internal Medicine. 2009;24:211–217. doi: 10.1007/s11606-008-0864-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perdue DG, Perkins C, Jackson-Thompson J, Coughlin SS, Ahmed F, Haverkamp DS, Jim MA. Regional differences in CRC incidence, state, and subsite among American Indians and Alaska Natives, 1999–2004. Cancer. 2008;113(5, Suppl):1179–1190. doi: 10.1002/cncr.23726. [DOI] [PubMed] [Google Scholar]
- Petereit DG, Molloy K, Reiner ML, Helbig P, Cina K, Miner R, Roberts CR. Establishing a patient navigator program to reduce cancer disparities in the American Indian communities of Western South Dakota: Initial observations and results. Cancer Control. 2008;15:254–259. doi: 10.1177/107327480801500309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petereit DG, Rogers D, Burhansstipanov L, Kaur J, Govern F, Howard SP, Mehta MP. Walking forward: The South Dakota Native American project. Journal of Cancer Education. 2005;20(1, Suppl):65–70. doi: 10.1207/s15430154jce2001s_14. [DOI] [PubMed] [Google Scholar]
- Robinson-White S, Conroy B, Slavish KH, Rosenzweig M. Patient navigation in breast cancer: A systematic review. Cancer Nursing. 2010;33:127–140. doi: 10.1097/NCC.0b013e3181c40401. [DOI] [PubMed] [Google Scholar]
- Rogers D, Petereit DG. Cancer disparities research partnership in Lakota Country: Clinical trials, patient services, and community education for the Oglala, Rosebud, and Cheyenne River Sioux tribes. American Journal of Public Health. 2005;95:2129–2132. doi: 10.2105/AJPH.2004.053645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelton BL. Legal and historical basis of Indian health care. In: Dixon M, Roubideaux Y, editors. Promises to keep: Public health policy for American Indians and Alaska Natives in the 21st century. Washington, DC: American Public Health Association; 2001. pp. 1–28. [Google Scholar]
- Strzelczyk JJ, Dignan MB. Disparities in adherence to recommended followup on screening mammography: Interaction of sociodemographic factors. Ethnicity and Disease. 2002;12(1):77–86. [PubMed] [Google Scholar]
- U.S. Commission on Civil Rights. Broken promises: Federal funding and unmet needs in Indian country. Washington, DC: Author; 2004. [Google Scholar]
- U.S. Department of Health and Human Services. Healthy people 2010: Understanding and improving health. 2. Washington, DC: U.S. Government Printing Office; 2000. [Google Scholar]
- Vargas RB, Ryan GW, Jackson CA, Rodriguez R, Freeman HP. Characteristics of the original patient navigation programs to reduce disparities in the diagnosis and treatment of breast cancer. Cancer. 2008;113:426–433. doi: 10.1002/cncr.23547. [DOI] [PubMed] [Google Scholar]
- Warren-Mears V, Ramsey K. Northwest Tribal Cancer Navigator Program: Pilot project final report. 2007 Retrieved from http://www.npaihb.org/images/epicenter_docs/navigator/2008/NavPilotFinalDsgn.pdf.
- Wiggins CL, Espey DK, Wingo PA, Kaur JS, Wilson RT, Swan J, Lanier AP. Cancer among American Indians and Alaska Natives in the United States, 1999–2004. Cancer. 2008;113(5, Suppl):1142–1152. doi: 10.1002/cncr.23734. [DOI] [PubMed] [Google Scholar]
- Wingo PA, King J, Swan J, Coughlin SS, Kaur S, Erb-Alvarez JA, Arambula Solomon TG. Breast cancer incidence among American Indian and Alaska Native Women: US, 1999–2004. Cancer. 2008;113(5, Suppl):1191–1202. doi: 10.1002/cncr.23725. [DOI] [PubMed] [Google Scholar]


