Abstract
Background and objective
Appropriate triage of patients with severe community-acquired pneumonia (CAP) may improve morbidity, mortality, and use of hospital resources. Worse outcomes from delayed intensive care unit (ICU) admission have long been suspected but have not been verified.
Methods
In a retrospective study of consecutive patients with CAP admitted from 1996–2006 to the ICUs of a tertiary care hospital, we measured serial severity scores, intensive therapies received, ICU-free days, and 30-day all-cause mortality. Primary outcome was mortality. We developed a regression model of mortality with ward triage (and subsequent ICU transfer within 72 hours) as the predictor, controlled by propensity for ward triage and radiographic progression.
Results
Of 1,059 hospital-admitted patients, 269 (25%) were admitted to the ICU during hospitalization. Of those, 167 were directly admitted to the ICU without current requirement for life support, while 61 (23%) were initially admitted to the hospital ward, 50 of those undergoing ICU transfer within 72 hours. Ward triage was associated with increased mortality (OR 2.6, p=0.056) after propensity adjustment. The effect was less (OR 2.2, p=0.12) after controlling for radiographic progression. The effect probably increased (OR 4.0, p=0.08) among patients with ≥ 3 severity predictors at admission.
Conclusions
Initial ward triage among patients subsequently transferred to the ICU is associated with twofold higher 30-day mortality. This effect is most apparent among patients with ≥ 3 severity predictors at admission and is partially attenuated by controlling for radiographic progression. Intensive monitoring of ward-admitted patients with CAP seems warranted. Further research is needed to optimize triage in CAP.
Keywords: Intensive Care, Outcome Assessment, Pneumonia, Respiratory Tract Infections, Triage
Introduction
Community-acquired pneumonia (CAP) is an important clinical and public health problem. When combined with influenza, CAP is the eighth-leading cause of death in the United States and the most common cause of death from infection in the developed world.1–3 Approximately 500,000 adults are admitted to the hospital in the US annually for CAP.4 Since appropriate site of care presumably improves outcome and is the major determinant of cost, optimal triage of these patients is considered important.5, 6 While patients requiring mechanical ventilation or vasopressor infusion require immediate ICU admission, how best to triage patients with some markers of severity but no current need for mechanical ventilation or vasopressor infusion is not clear. Delayed triage to the intensive care unit (ICU) may place patients at risk for worse outcomes, including prolonged ICU or hospital stay and premature mortality, while unnecessary ICU admission is costly and may expose patients to other risks, e.g. hospital-acquired infection or delirium. Previous studies have yielded conflicting conclusions about the risks of delayed ICU triage.7–13
Regardless of ICU triage, radiographically progressive pneumonia is more lethal than pneumonia associated with stable radiographic infiltrates.14, 15 Radiographic progression of CAP accords with the common clinical understanding that a subset of patients has progressive disease regardless of therapy, due to predisposition for ARDS or unmeasured microbe-specific factors. Recent studies of delayed ICU admission did not control for radiographically progressive pneumonia, which may have confounded their finding of worse outcome with delayed ICU admission.16–18
Worse outcomes from delayed intensive care unit (ICU) admission have long been suspected but not certain. To evaluate the effect of initial ward triage on mortality and length of stay, after controlling for radiographic progression and propensity for initial ward triage, we studied a cohort of patients with severe CAP (SCAP) whose triage was not dictated by a current requirement for mechanical ventilation or vasopressor infusion.
Methods
Setting
We have reported our general methods previously.19 Briefly, the study was performed at LDS Hospital, a tertiary care, university-affiliated teaching hospital, with 520 total and 68 ICU beds. There are approximately 26,500 Emergency Department (ED) visits per year, resulting in approximately 7,000 hospital admissions. In 1995, the LDS Hospital ED initiated a standardized pneumonia therapy protocol; severity assessment and triage guidelines based on the 1993 ATS guidelines were available on a paper form that was rarely utilized by ED staff.20–22 Hospital policy required ICU admission for any patient requiring ≥ 60% inspired oxygen unless advanced directives limiting care were in place.
Patients
In a retrospective analysis of prospectively acquired electronic data using a validated algorithm,23 we identified all patients admitted to LDS Hospital with ICD-9 codes for primary diagnosis of pneumonia (480–487.x) or respiratory failure or organism-specific sepsis (518.x, 038.x) with a secondary diagnosis of pneumonia (480–487.x) from 1996 to 2006. A chest radiograph compatible with pneumonia was required within 48 hours of admission, as extracted manually from radiologist-dictated reports.
We included patients admitted to the ICU either directly or within 72 hours of hospital admission who were not undergoing mechanical ventilation or vasopressor support (the IDSA/ATS 2007 major criteria5) at the time of transfer from the ED to the ICU. We thus studied patients who did not have an obvious, immediate indication for ICU admission.
We excluded a) patients with aspiration pneumonia or immune suppression (AIDS, solid organ or bone marrow transplantation, metastatic solid tumors, or present or past hematologic malignancies as defined by ICD-9 codes); b) patients residing in a skilled nursing facility; c) patients discharged from a hospital within the prior 90 days; d) patients receiving chronic hemodialysis;5 e) patients with admission do-not-resuscitate/do-not-intubate (DNR/DNI) orders24; and f) patients who expired in the ED. Patients were included only once in any 12-month period.
We calculated admission IDSA/ATS 20075 and SMART-COP25 pneumonia severity prediction scores as well as the admission SAPS-2 score.26 We also calculated daily IDSA/ATS 2007 scores for the first 72 hours following admission and the IDSA/ATS 2007 score at the time of transfer to the ICU among ward-triage patients. Thirty-day all-cause mortality, the primary mortality endpoint based on consensus that it best reflects pneumonia-associated mortality27–30, was determined from the Utah Population Database.31 We defined intensive therapies per our published methodology.19 We defined radiographic progression as an extension of infiltrates or development of new pleural effusion on the basis of radiologist reports.
Triage Definitions
We defined ward triage a priori as initial admission to the hospital ward followed by ICU transfer within 72 hours. We chose 72 hours as a compromise meant to capture progressive SCAP while excluding late complications and to follow other reports.16, 17 We also evaluated patients who died within 72 hours of being admitted to the ward but were never transferred to the ICU. Patients in this group whose death was unrelated to decisions to limit use of intensive therapies were considered to have undergone initial ward triage.
Because we were interested in the triage decision itself, we defined ICU triage as admission directly from ED to ICU, without any intervening stay on the hospital ward. We considered patients transferred from the ward to the ICU within 24 hours to have undergone ward triage, contrary to other studies.16, 18 Because we were interested in whether observation in the ICU setting is beneficial, we included all patients admitted to the ICU, regardless of receipt of intensive therapies.
Primary analysis
Primary outcome was 30-day mortality. Our primary analysis was to determine whether initial ward triage (as opposed to initial ICU triage) was associated with increased mortality among patients who did not have an immediate need for ICU admission at the time they left the ED. To this end, we developed a logistic regression model of the association between ward triage and 30-day all-cause mortality in patients evaluated in the ED, adjusted for propensity32–34 of ward triage and radiographic progression. We built the propensity model on the basis of IDSA/ATS 2007 severity score, SAPS-2 score, age, and other relevant predictors. We incorporated the propensity score into a final backward stepwise logistic regression, excluding predictors with p>0.1. The ultimate outcome of interest was all-cause 30-day mortality; the defined predictor of interest was ward triage. A linear regression model of ICU-free days at 30 days was built in the same manner. Missing predictors were assumed to be normal if dichotomous. Statistical significance was defined as a two-tailed p < 0.05. Analyses were performed with Stata 10 (College Park, TX) and R 2.10.2 (Vienna, Austria).35
Sensitivity Analyses
We performed three sensitivity analyses. First, we stratified the cohort based on an initial IDSA/ATS 2007 severity score ≥ 3, a consensus threshold for defining SCAP.19, 36, 37 This first sensitivity analysis sought to define the association between ward triage and mortality among patients who appear to have been mis-triaged on the basis of high admission severity scores. Second, we replicated the methodology of Renaud et al16 by including patients transferred from the ward to the ICU within 24 hours of hospital admission with patients directly admitted to the ICU to assess the effect of this methodology on the estimate of the association between ward triage and mortality. Third, we stratified the cohort into two time periods to evaluate for secular trends in the association.
Finally, we performed an exploratory matching procedure based on serial IDSA/ATS 2007 scores, intended to assess whether the effect of ward triage was mediated by clinical deterioration. Clinical deterioration was defined as an increase in the IDSA/ATS 2007 score over time. Ward-triage patients were matched to ICU-triage patients based on admission IDSA/ATS 2007 score as well as IDSA/ATS 2007 score at the time of transfer to the ICU. Because ICU-triage patients did not have a corresponding time of transfer, we used the IDSA/ATS 2007 score for the hospital day that matched the transfer time of the matched ward-triage patient. For example, if the ward-triage patient was transferred to the ICU 36 hours after admission, the ICU-triage patient’s day 2 IDSA/ATS 2007 score was used for matching.
Ethical considerations
This study was approved by the Intermountain Healthcare Institutional Review Board (#1008505); individual patient consent was not required.
Results
Clinical and Demographic Findings
Two-hundred seventeen patients met inclusion criteria (Figure 1). Table 1 presents admission data on this cohort. Overall 30-day mortality was 5.8% (61 of 1,059) for admitted, ED-evaluated patients. Among patients in the study cohort, 15% (32 of 217) died; of ward-triage patients, 22% (11 of 50) died, while of ICU-triage patients, 12.6% (21 of 167) died. Ward-triage patients (N=50) had a mean IDSA/ATS 2007 score of 1.9 (median 2, IQR 1–3) at the time of admission. At the time of transfer from the ward to the ICU, the mean IDSA/ATS 2007 score was 3.9 (median 4, IQR 3–5), a significant increase (p<0.001). ICU-triage patients (N=167) had a mean IDSA/ATS 2007 score of 2.3(median 2, IQR 2–3) at time of admission, which was stable through the second hospital day. An admission IDSA/ATS 2007 score ≥ 3 was associated with significantly higher odds of death across all patient strata—mortality was highest (43%) among ward-triage patients with an admission score ≥ 3.
Figure 1.
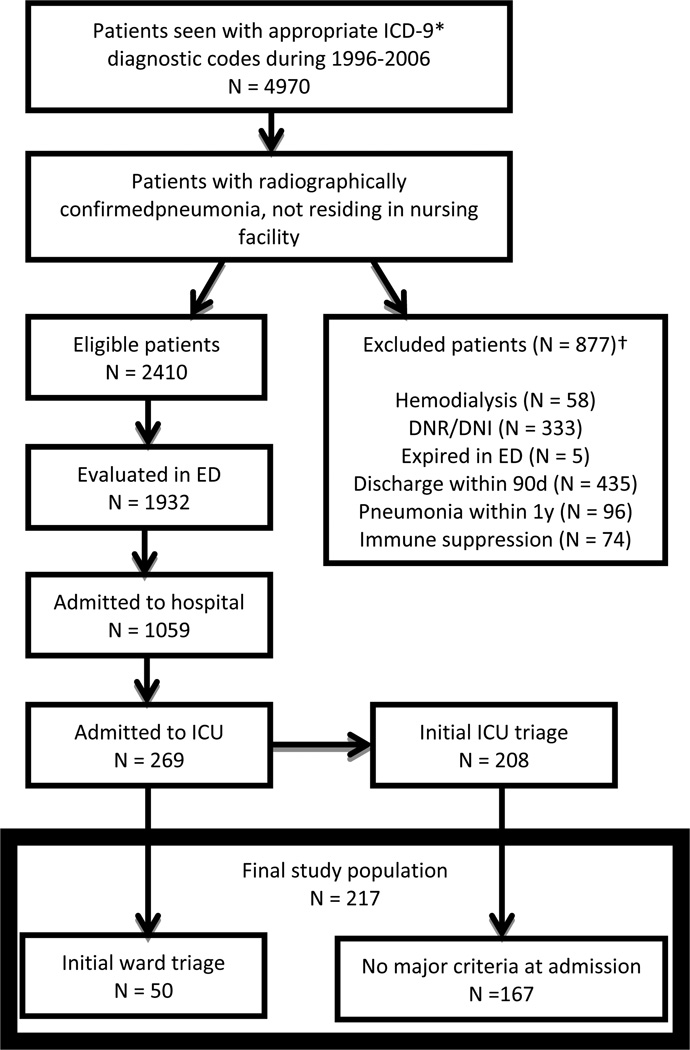
Flow chart illustrating patient selection for the final study population.
*Primary ICD-9 code for pneumonia (480–487.x) or respiratory failure (518.x), organism-specific sepsis (0.38.x) with pneumonia (480–487.x) as secondary diagnosis.
†Some patients had >1 exclusion; 11 (excluded) patients were transferred to ICU after >72 h
Table 1.
Comparison of Admission Characteristics
| Parameter | Ward triage N=50 |
ICU triage N=167 |
p-value for comparison |
|---|---|---|---|
| Age (years) | 62 | 58 | 0.3 |
| Sex (% female) | 46 | 46 | 0.95 |
| CURB-65 (points) | 1.9 | 1.9 | 0.8 |
| SMART-COP (points) | 2.9 | 3.5 | 0.02 |
| IDSA/ATS 2007 minor criteria (points) | 1.9 | 2.4 | 0.01 |
| SAPS-2 score (points) | 25 | 26.4 | 0.4 |
| Appropriate initial antibiotics (%) | 72 | 71 | 0.9 |
| Bacteremia (%) | 8 | 8 | 0.96 |
| Microbial etiology identified (%) | 18 | 16 | 0.7 |
| Confusion (%) | 4 | 10 | 0.2 |
| Multilobar disease (%) | 50 | 58 | 0.3 |
| Blood Urea Nitrogen > 20mg/dl (%) | 64 | 54 | 0.2 |
| Respiratory rate >= 30/min (%) | 14 | 37 | <0.01 |
| Mean Arterial Pressure < 65mmHg (%) | 16 | 23 | 0.3 |
| P/F ratio<250 (%)* | 30 | 44 | 0.07 |
| Hypothermia—Temp<36C (%) | 10 | 8 | 0.6 |
| White Blood Cells < 4,000/mm3 (%) | 6 | 3 | 0.3 |
| Platelets<100,000/mm3 (%) | 0 | 5 | 0.1 |
| Hospital mortality (%) | 20 | 12 | 0.1 |
| 30-day mortality (%) | 22 | 13 | 0.1 |
Adjusted for altitude of LDS Hospital (1400m, average barometric pressure 650 mmHg) CURB-65: Confusion, Urea, Respiratory Rate, Blood Pressure, Age>65 Score; SMART-COP: Systolic blood pressure, Multilobar pneumonia, low Albumin, Respiratory rate, Tachycardia, Confusion, low Oxygen, low PH Score; IDSA/ATS 2007: Infectious Diseases Society of America/American Thoracic Society 2007 Pneumonia Guidelines; SAPS-2: Simplified Acute Physiology Score.
The distribution of intensive therapies among patients based on their initial triage is displayed in Table 2. Ward-triage patients were much more likely to receive intensive therapies following ICU transfer than ICU-triage patients. The total volume of crystalloid infused in the first 12 or 24 hours, a marker of the adequacy of resuscitation, did not differ significantly between ICU-triage and ward-triage patients.
Table 2.
Intensive therapies received by initial triage decision
| Intensive therapy | Ward triage % (95% CI) (N=50) |
ICU triage % (95% CI) (N=167) |
p value for comparison |
|---|---|---|---|
| Any intensive therapy | 84 (74–94) | 68 (61–75) | 0.02 |
| NIPPV | 12 (3–21) | 11 (6–15) | 0.8 |
| FiO2>=0.6 | 62 (49–75) | 52 (45–60) | 0.2 |
| Mechanical ventilation | 52 (38–66) | 23 (17–30) | <0.01 |
| Vasopressor support | 34 (21–47) | 19 (13–24) | 0.02 |
| Ventilation and vasopressors | 30 (17–43) | 14 (9–20) | 0.01 |
| Ventilation or vasopressors | 56 (42–70) | 28 (21–34) | <0.01 |
| Central venous catheter | 38 (25–51) | 23 (17–29) | 0.03 |
| Arterial catheter | 50 (36–64) | 41 (33–48) | 0.2 |
| Aggressive fluid resuscitation* | 22 (11–33) | 12 (7–17) | 0.08 |
NIPPV: Non-invasive positive pressure ventilation
>=4L of crystalloid within 2 hours
Death on the ward within 72 hours of admission but without transfer to the ICU affected four patients (median age 87 years), all of whom were excluded for newly instituted limitations of care that prohibited ICU transfer. By comparison, all patients directly admitted to the ICU who died within 72 hours of admission received aggressive support, including vasopressors and mechanical ventilation.
Primary Analysis
The results of the final regression model for the primary analysis are displayed in Table 3, controlling for admission severity scores. In the propensity-adjusted model, initial ward triage had an OR of 2.6 (p= 0.056). When this effect was controlled for radiographic progression, OR was 2.2 (p=0.1). The linear regression model of ICU-free days at 30 days associated initial ward triage with approximately 3.3 fewer ICU-free days after controlling for propensity (p=0.02). Controlling for radiographic progression (the model displayed in Table 4) reduced the estimate to 2.3days (p=0.1).
Table 3.
Regression models for 30-day mortality
| Predictor | OR (95% CI; p value) unadjusted |
OR (95% CI; p value) propensity- adjusted |
OR (95% CI; p value) adjusted for radiographic progression |
|---|---|---|---|
| Initial Ward Triage (vs. Initial ICU Triage) | 2.4 (0.95–5.9; 0.06) | 2.6 (0.98–7.0; 0.056) | 2.2 (0.8–6.0; 0.12) |
| Age (per year) | 1.04 (1.01– 1.07; <0.01) | 1.04 (1.01– 1.08; <0.01) | 1.05 (1.02– 1.08; <0.01) |
| Minor Criteria Score (per point) | 1.8 (1.3–2.5; <0.01) | 1.8 (1.2–2.8; 0.01) | 1.7 (1.1–2.7; 0.02) |
| Propensity Score | NA | 1.6 (0.04–62; 0.8) | 1.5 (0.04–60; 0.8) |
| Radiographic Progression (vs. no radiographic progression) | NA | NA | 2.4 (0.92–6.3; 0.07) |
95% CI: Ninety-five percent confidence interval for Odds Ratio
Table 4.
Linear Regression of ICU-free days at 30 days (N=209)*
| Predictor | Coefficient | 95%CI | p value |
|---|---|---|---|
| Ward Triage | −2.3 | −5.1-0.5 | 0.1 |
| Age | −0.06 | −0.13-0.001 | 0.06 |
| Minor Criteria Score | −1.5 | −2.6 -−0.4 | < 0.01 |
| Propensity Score | 0.3 | −9.1-9.1 | 0.9 |
| Radiographic Progression | −3.8 | −6.1-−1.5 | <0.01 |
| Intercept | 34 | 29–39 | <0.01 |
The 8 patients with low platelet count were all admitted directly to the ICU so were excluded from the model.
Sensitivity Analyses
Stratifying the cohort based on admission IDSA/ATS 2007 score suggested a difference in the effect of initial ward triage on 30-day mortality. When restricted to patients with an admission score ≥ 3, the odds ratio was 4.1 (p=0.07), while among patients with an admission score < 3, the odds ratio was 1.6 (p=0.5). The sensitivity analysis applying the methodology of Renaud et al to our cohort yielded an OR of 3.7(p=0.04) for initial ward triage. Controlling for radiographic progression yielded an OR of 2.9 (p=0.1).
Discussion
Initial ward triage of patients subsequently transferred to the ICU within 72 hours was associated with higher 30-day mortality after controlling for propensity for ward triage. The significance of this association was attenuated by controlling for radiographic progression, though the effect estimate was reasonably stable. This association depends strongly on baseline severity: patients who met IDSA/ATS 2007 criteria for severe pneumonia (≥ 3 predictors) in the ED had a fourfold increased risk of death if triaged to the ward, an effect that almost reached statistical significance (p=0.07) despite the low size of this predefined subgroup.
Our study expands prior observations16–18 in several ways. First, we estimated the influence of progressive pneumonia, a distinct clinical entity that likely confounded prior studies.14, 15 Second, we studied actual triage rather than merging patients transferred from the ward to the ICU within 24 hours.16, 18 (Merging patients transferred within 24 hours inflates the risk of ward triage, as demonstrated by a sensitivity analysis in our cohort.) Third, we evaluated the effect of ward triage in a hospital with respiratory protocols, low thresholds for ICU transfer, and low overall mortality from CAP, a setting in which ward triage should be relatively safe. Fourth, we explicitly investigated patients who died before ICU transfer but within 72 hours. Our study thus increases the confidence of inferences about worse outcomes among patients initially triaged to the hospital ward.
The issue of confounding by progressive pneumonia is important to consider in assessing the risk of ward triage of patients with CAP. The development of ARDS or a systemic cytokine response to bacteriolysis in patients with a high titer of genomic bacterial DNA38 could cause rapid progression of CAP in a patient who initially appears well. Similarly, late-appearing shock is generally more lethal than early-appearing shock in infected patients.15, 39, 40 This study helps address the concern that the association between ward triage and poor outcome is confounded by the entity of progressive CAP. First, the association between ward triage and mortality persisted as a trend (p=0.1) after control for radiographic progression. Second, the association between ward triage and mortality is large (OR 4.0, p=0.08) among patients with severe pneumonia at admission. Though the small number of such patients limits certainty about this conclusion, our patient cohort suggests that progressive CAP only partially accounts for the association between ward triage and mortality.
Mortality associated with ward triage may be related to physiological deterioration. Patients who deteriorate die more frequently; our primary analysis suggests that this clinical deterioration may be related to initial ward triage. That deteriorating patients have higher mortality is not surprising, but our study suggests that ward triage may contribute to this deterioration.
There are limits to the generalizability of our findings. Progressive respiratory failure is monitored closely on the wards of the study hospital, often with continuous pulse oximetry, and ICU transfer is usually undertaken before mechanical ventilation is immediately required. In institutions where the clinical course of CAP patients cannot be monitored frequently, the deleterious effect of initial ward triage may be substantially worse. In addition, the use of a treatment guideline for CAP might alter results compared to a setting where care is more variable. Our study was retrospective, though clinical data were recorded prospectively throughout the duration of the study, and the retrospective design avoided the risk of a Hawthorne effect (clinicians behaving differently when they believe they are being observed). Our mortality is consistent with other studies. Our ICU admission rate is somewhat higher and our ED stays shorter than at some other US hospitals.28, 41, 42 We were unable to gather data on how often bed availability affected triage decisions. Relatively few patients in eleven years underwent discordant triage; the modest sample size may limit generalizability of the present study.
We propose that healthcare systems provide careful scrutiny of moderately ill patients (≥ 2 IDSA/ATS severity criteria, with special emphasis on patients with ≥ 3 criteria) with CAP, a group whose triage is not straightforward. Data from multiple centers now provide evidence to justify prospective evaluation of explicit triage strategies. Such triage strategies should include objective assessment of CAP severity in the ED. A triage protocol might recommend ICU admission for patients with ≥ 3 minor criteria, particularly those with hypoxemia, and careful monitoring on a hospital ward for patients with ≥ 2 minor criteria. We also propose development of models for predicting deterioration on the hospital ward among patients with pneumonia. Better models should improve the efficiency and generalizability of the prospective studies that should be performed to confirm our findings. Until results from rigorous, prospective studies become available, we believe that early ICU admission or better-than-usual monitoring on the floor should be implemented for moderately ill patients admitted with CAP.
Summary at a Glance.
It is unclear whether admitting a patient with severe pneumonia to the hospital ward has a negative effect on outcome. Attempts to answer this question have been confounded by the entity of progressive pneumonia. In this study we suggest that some of the association of initial ward triage with mortality is accounted for by progressive pneumonia.
Acknowledgements
We are grateful to Ted Liou, MD and James Orme, MD for close readings of the manuscript, to Susan Crapo and Joe Dalto for data extraction, and to Marc-Aurel Martial for data quality assurance. Financial Support was received from the Intermountain Research and Medical Foundation, National Institute of General Medical Sciences (K23GM094465), National Center for Research Resources (Public Health Services research grant UL1-RR025764).
References
- 1.Heron M, Hoyert DL, Murphy SL, Xu J, Kochanek KD, et al. Deaths: final data for 2006. Natl Vital Stat Rep. 2009;57:1–134. [PubMed] [Google Scholar]
- 2.Armstrong GL, Conn LA, Pinner RW. Trends in infectious disease mortality in the United States during the 20th century. Jama. 1999;281:61–66. doi: 10.1001/jama.281.1.61. [DOI] [PubMed] [Google Scholar]
- 3.Singanayagam A, Chalmers JD, Hill AT. Severity assessment in community-acquired pneumonia: a review. QJM. 2009 doi: 10.1093/qjmed/hcp027. [DOI] [PubMed] [Google Scholar]
- 4.Marston BJ, Plouffe JF, File TM, Jr, Hackman BA, Salstrom SJ, et al. Incidence of community-acquired pneumonia requiring hospitalization. Results of a population-based active surveillance Study in Ohio. The Community-Based Pneumonia Incidence Study Group. Arch Intern Med. 1997;157:1709–1718. [PubMed] [Google Scholar]
- 5.Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(Suppl 2):S27–S72. doi: 10.1086/511159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bartolome M, Almirall J, Morera J, Pera G, Ortun V, et al. A population-based study of the costs of care for community-acquired pneumonia. Eur Respir J. 2004;23:610–616. doi: 10.1183/09031936.04.00076704. [DOI] [PubMed] [Google Scholar]
- 7.Hook EW, 3rd, Horton CA, Schaberg DR. Failure of intensive care unit support to influence mortality from pneumococcal bacteremia. Jama. 1983;249:1055–1077. [PubMed] [Google Scholar]
- 8.Ewig S, Bauer T, Hasper E, Pizzulli L, Kubini R, et al. Prognostic analysis and predictive rule for outcome of hospital-treated community-acquired pneumonia. Eur Respir J. 1995;8:392–397. doi: 10.1183/09031936.95.08030392. [DOI] [PubMed] [Google Scholar]
- 9.Woodhead M, Welch CA, Harrison DA, Bellingan G, Ayres JG. Community-acquired pneumonia on the intensive care unit: secondary analysis of 17,869 cases in the ICNARC Case Mix Programme Database. Crit Care. 2006;10(Suppl 2):S1. doi: 10.1186/cc4927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leroy O, Santre C, Beuscart C, Georges H, Guery B, et al. A five-year study of severe community-acquired pneumonia with emphasis on prognosis in patients admitted to an intensive care unit. Intensive Care Med. 1995;21:24–31. doi: 10.1007/BF02425150. [DOI] [PubMed] [Google Scholar]
- 11.Shmueli A, Sprung CL. Assessing the in-hospital survival benefits of intensive care. Int J Technol Assess Health Care. 2005;21:66–72. doi: 10.1017/s0266462305050087. [DOI] [PubMed] [Google Scholar]
- 12.Sprung CL, Geber D, Eidelman LA, Baras M, Pizov R, et al. Evaluation of triage decisions for intensive care admission. Crit Care Med. 1999;27:1073–1079. doi: 10.1097/00003246-199906000-00021. [DOI] [PubMed] [Google Scholar]
- 13.Simchen E, Sprung CL, Galai N, Zitser-Gurevich Y, Bar-Lavi Y, et al. Survival of critically ill patients hospitalized in and out of intensive care. Crit Care Med. 2007;35:449–457. doi: 10.1097/01.CCM.0000253407.89594.15. [DOI] [PubMed] [Google Scholar]
- 14.Lisboa T, Blot S, Waterer GW, Canalis E, de Mendoza D, et al. Radiologic progression of pulmonary infiltrates predicts a worse prognosis in severe community-acquired pneumonia than bacteremia. Chest. 2009;135:165–172. doi: 10.1378/chest.08-1216. [DOI] [PubMed] [Google Scholar]
- 15.Roson B, Carratala J, Fernandez-Sabe N, Tubau F, Manresa F, et al. Causes and factors associated with early failure in hospitalized patients with community-acquired pneumonia. Arch Intern Med. 2004;164:502–508. doi: 10.1001/archinte.164.5.502. [DOI] [PubMed] [Google Scholar]
- 16.Renaud B, Santin A, Coma E, Camus N, Van Pelt D, et al. Association between timing of intensive care unit admission and outcomes for emergency department patients with community-acquired pneumonia. Crit Care Med. 2009;37:2867–2874. doi: 10.1097/CCM.0b013e3181b02dbb. [DOI] [PubMed] [Google Scholar]
- 17.Phua J, Ngerng WJ, Lim TK. The impact of a delay in intensive care unit admission for community-acquired pneumonia. Eur Respir J. 2010 doi: 10.1183/09031936.00154209. [DOI] [PubMed] [Google Scholar]
- 18.Restrepo MI, Mortensen EM, Rello J, Brody J, Anzueto A. Late admission to the ICU in patients with community-acquired pneumonia is associated with higher mortality. Chest. 2010;137:552–557. doi: 10.1378/chest.09-1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brown SM, Jones BE, Jephson AR, Dean NC. Validation of the Infectious Disease Society of America/American Thoracic Society 2007 guidelines for severe community-acquired pneumonia. Crit Care Med. 2009;37:3010–3016. doi: 10.1097/CCM.0b013e3181b030d9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dean NC, Bateman KA. Local guidelines for community-acquired pneumonia: development, implementation, and outcome studies. Infect Dis Clin North Am. 2004;18:975–991. doi: 10.1016/j.idc.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 21.Dean NC, Silver MP, Bateman KA, James B, Hadlock CJ, et al. Decreased mortality after implementation of a treatment guideline for community-acquired pneumonia. Am J Med. 2001;110:451–457. doi: 10.1016/s0002-9343(00)00744-0. [DOI] [PubMed] [Google Scholar]
- 22.Dean NC, Jones JP, Aronsky D, Brown S, Vines CG, et al. Hospital admission decision for patients with community-acquired pneumonia: variability among physicians in an emergency department. Ann Emerg Med. 2012;59:35–41. doi: 10.1016/j.annemergmed.2011.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aronsky D, Haug PJ, Lagor C, Dean NC. Accuracy of administrative data for identifying patients with pneumonia. Am J Med Qual. 2005;20:319–328. doi: 10.1177/1062860605280358. [DOI] [PubMed] [Google Scholar]
- 24.Aronsky D, Kasworm E, Jacobson JA, Haug PJ, Dean NC. Electronic screening of dictated reports to identify patients with do-not-resuscitate status. J Am Med Inform Assoc. 2004;11:403–409. doi: 10.1197/jamia.M1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Charles PG, Wolfe R, Whitby M, Fine MJ, Fuller AJ, et al. SMART-COP: a tool for predicting the need for intensive respiratory or vasopressor support in community-acquired pneumonia. Clin Infect Dis. 2008;47:375–384. doi: 10.1086/589754. [DOI] [PubMed] [Google Scholar]
- 26.Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. Jama. 1993;270:2957–2963. doi: 10.1001/jama.270.24.2957. [DOI] [PubMed] [Google Scholar]
- 27.Jencks SF, Williams DK, Kay TL. Assessing hospital-associated deaths from discharge data. The role of length of stay and comorbidities. Jama. 1988;260:2240–2246. [PubMed] [Google Scholar]
- 28.Fine MJ, Auble TE, Yealy DM, Hanusa BH, Weissfeld LA, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997;336:243–250. doi: 10.1056/NEJM199701233360402. [DOI] [PubMed] [Google Scholar]
- 29.Jencks SF, Daley J, Draper D, Thomas N, Lenhart G, et al. Interpreting hospital mortality data. The role of clinical risk adjustment. Jama. 1988;260:3611–3616. [PubMed] [Google Scholar]
- 30.Mortensen EM, Coley CM, Singer DE, Marrie TJ, Obrosky DS, et al. Causes of death for patients with community-acquired pneumonia: results from the Pneumonia Patient Outcomes Research Team cohort study. Arch Intern Med. 2002;162:1059–1064. doi: 10.1001/archinte.162.9.1059. [DOI] [PubMed] [Google Scholar]
- 31.Skolnick M. The Utah genealogical database: a resource for genetic epidemiology. In: Cairns JL,JL, Skolnick M, editors. Banbury Report No 4; Cancer Incidence in Defined Populations. New York: Cold Spring Harbor Laboratory; 1980. pp. 285–297. [Google Scholar]
- 32.Kurth T, Walker AM, Glynn RJ, Chan KA, Gaziano JM, et al. Results of multivariable logistic regression, propensity matching, propensity adjustment, and propensity-based weighting under conditions of nonuniform effect. Am J Epidemiol. 2006;163:262–270. doi: 10.1093/aje/kwj047. [DOI] [PubMed] [Google Scholar]
- 33.D'Agostino RB., Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17:2265–2281. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 34.Stone RA, Obrosky DS, Singer DE, Kapoor WN, Fine MJ. Propensity score adjustment for pretreatment differences between hospitalized and ambulatory patients with community-acquired pneumonia. Pneumonia Patient Outcomes Research Team (PORT) Investigators. Med Care. 1995;33:AS56–AS66. [PubMed] [Google Scholar]
- 35.Team RDC. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. Austria: Vienna; 2009. [Google Scholar]
- 36.Liapikou A, Ferrer M, Polverino E, Balasso V, Esperatti M, et al. Severe community-acquired pneumonia: validation of the Infectious Diseases Society of America/American Thoracic Society guidelines to predict an intensive care unit admission. Clin Infect Dis. 2009;48:377–385. doi: 10.1086/596307. [DOI] [PubMed] [Google Scholar]
- 37.Phua J, See KC, Chan YH, Widjaja LS, Aung NW, et al. Validation and clinical implications of the IDSA/ATS minor criteria for severe community-acquired pneumonia. Thorax. 2009;64:598–603. doi: 10.1136/thx.2009.113795. [DOI] [PubMed] [Google Scholar]
- 38.Rello J, Lisboa T, Lujan M, Gallego M, Kee C, et al. Severity of pneumococcal pneumonia associated with genomic bacterial load. Chest. 2009;136:832–840. doi: 10.1378/chest.09-0258. [DOI] [PubMed] [Google Scholar]
- 39.Sakr Y, Vincent JL, Schuerholz T, Filipescu D, Romain A, et al. Early- versus late-onset shock in European intensive care units. Shock. 2007;28:636–643. [PubMed] [Google Scholar]
- 40.Roman-Marchant O, Orellana-Jimenez CE, De Backer D, Melot C, Vincent JL. Septic shock of early or late onset: does it matter? Chest. 2004;126:173–178. doi: 10.1378/chest.126.1.173. [DOI] [PubMed] [Google Scholar]
- 41.Angus DC, Marrie TJ, Obrosky DS, Clermont G, Dremsizov TT, et al. Severe community-acquired pneumonia: use of intensive care services and evaluation of American and British Thoracic Society Diagnostic criteria. Am J Respir Crit Care Med. 2002;166:717–723. doi: 10.1164/rccm.2102084. [DOI] [PubMed] [Google Scholar]
- 42.Roson B, Carratala J, Dorca J, Casanova A, Manresa F, et al. Etiology, reasons for hospitalization, risk classes, and outcomes of community-acquired pneumonia in patients hospitalized on the basis of conventional admission criteria. Clin Infect Dis. 2001;33:158–165. doi: 10.1086/321808. [DOI] [PubMed] [Google Scholar]


