Abstract
Introduction
Diabetes self-management education is a cornerstone of diabetes care. However, many diabetics in the United Arab Emirates (UAE) lack sufficient knowledge about their disease due to illiteracy. Thus, before considering any possible intervention it was imperative to assess present knowledge, attitudes, and practices of patients towards the management of diabetes.
Methods
A random sample of 575 DM patients was selected from diabetes outpatient's clinics of Tawam and Al-Ain hospitals in Al-Ain city (UAE) during 2006–2007, and their knowledge attitude and practice assessed using a questionnaire modified from the Michigan Diabetes Research Training Center instrument.
Results
Thirty-one percent of patients had poor knowledge of diabetes. Seventy-two had negative attitudes towards having the disease and 57% had HbA1c levels reflecting poor glycemic control. Only seventeen percent reported having adequate blood sugar control, while 10% admitted non-compliance with their medications. Knowledge, practice and attitude scores were all statistically significantly positively, but rather weakly, associated, but none of these scores was significantly correlated with HbA1c.
Conclusions
The study showed low levels of diabetes awareness but positive attitudes towards the importance of DM care and satisfactory diabetes practices in the UAE. Programs to increase patients' awareness about DM are essential for all diabetics in the UAE in order to improve their understanding, compliance and management and, thereby, their ability to cope with the disease.
Introduction
The management of diabetes mellitus (DM) largely depends on patients' ability to self-care in their daily lives, and therefore, patient education is always considered an essential element of DM management. Studies have consistently shown that improved glycemic control reduces the rate of complications and evidence suggests that patients, who are knowledgeable about DM self-care, have better long term glycemic control [1], [2], [3]. Thus it is indispensable to ensure that patients' knowledge, attitudes and practices are adequate.
Although the prevalence of DM is high among populations in the Middle East and Gulf countries, patients often lack the knowledge and skills to self-manage their condition [4]–[7] and although the International Diabetes Federation (IDF) in 2011 ranked the UAE's prevalence for type 2 DM as the tenth highest in the world (19.2%) [8], little is known about the knowledge, attitudes and practices of DM patients in the UAE. In 2006, a study demonstrated poor levels of compliance and knowledge among DM patients in the UAE. Twenty-five percent only of the patients reported an increase in their physical activity levels following diagnosis with a mere 3% meeting the recommended guidelines and 76% could not distinguish between low and high carbohydrate glycemic index food items [9], [10]. To date, only one study assessed DM knowledge among patients in a primary health care setting in the UAE, and identified significant knowledge shortfalls in this population [11]. Since its publication in 2001 there has been considerable media coverage of DM and the level of general education of the population has also increased substantially. A new survey on DM patients' knowledge, attitudes and practice about DM is therefore badly needed.
Materials and Methods
Ethics Statement
This study was approved by Al-Ain Medical District Human Research Ethics Committee (MDREC). Informed written consent was obtained from all literate participants while verbal consent was obtained from illiterate participants, for which we obtained approval from Al Ain MDREC. The researchers ensured that the verbal consent contained all the elements of the written consent. The research nurses, in the presence of a witness, explained verbally all the pertinent information of the study and allowed the subjects the opportunity to ask questions and verified that this was understood. Both the research nurse and the witness signed the consent forms when the participants verbally agreed to participate.
Setting
The study was carried out at the outpatient departments of two major government hospitals, Tawam and Al-Ain hospitals, which serve approximately three quarters of the patients' population in the Eastern District of Abu Dhabi Emirate (Al-Ain region). The health care system in the region is organized along the lines of conventional health care systems, i.e. primary health care (provided by 18 healthcare centres), including basic health care to DM patients, with referral to secondary and tertiary care where needed, provided by the above (only) two referral government hospitals. For logistical reasons (data completeness and accessibility) only referred patients, i.e. those attending the diabetes centres at Al-Ain and Tawam hospitals, were included in the study.
Study design and selection of participants
The study was a cross-sectional survey to assess the knowledge, attitude and practice (KAP) of diabetic patients in Al-Ain District, UAE using a modified instrument, adopted, with permission, from the Diabetes Research Training Center of Michigan [12]. In addition to KAP, we collected socio-demographic data that include gender, age, occupation, marital status, educational level, income, family history of diabetes, duration of diabetes and medications. The questionnaire was translated into Arabic separately by two bilingual translators. The two versions were combined and revised and then back translated into English by another bilingual translator. The translation was refined after back translation until agreement was obtained among the four people involved in the translations. Two diabetologists examined and approved the Arabic version of the questionnaire for content and construct validity. The questionnaire was then piloted among 10 outpatient DM patients, which gave rise to minor rewordings of the questionnaire. The sampling frame comprised all UAE and non-UAE diabetic patients of all ages and both genders attending the diabetes centres of Al-Ain or Tawam hospitals. In the absence of any diabetes registries, patients were randomly selected from the lists of clinic appointments. We decided that a sample size of 572 would be adequate. This number would provide 90% power, at the 5% significance level, to detect an association between two dichotomous (1/0; y/n) variables, one that splits the sample into two approximately equal halves (e.g. male and female, or the two participating clinics) and another that is 10% and 20% positive for each of the levels of the first variable. To reach this target 620 patients were approached, out of whom 575 (92%) agreed to participate.
Data collection and definitions
Informed consent was obtained from each patient at the time of their visit to the hospital. Literate patients filled out the questionnaires themselves while illiterate participants were interviewed by trained nurses. Clinical data, including diabetes complications and HbA1c (within six months prior to the survey) of participants were retrieved from medical records (HbA1c available for 208 patients only). Since, it was not always possible to distinguish clearly between types 1 and 2 DM from these records, patients were classified as either “insulin treated”, or “non-insulin treated”. Glycemic control was considered good, acceptable or poor when HbA1c levels were less than 7%, 7 to 8% and greater than 8, respectively, according to the American Diabetes Association's recommended guidelines [13].
The instrument
In the questionnaire patients' knowledge of diabetes was assessed using 23 questions relating to definitions, symptoms, causes and complications of DM. Attitudes were assessed using a series of questions on positive and/or negative attitudes towards having the disease, the ability to self-manage diabetes and awareness of the importance of adherence to DM (self) care. Patients' practices were assessed using questions on self-care, dietary modification, compliance with medications, weight control, self-monitoring of blood sugar, and regular follow up. DM knowledge was then scored by assigning one point for each correct response. We considered a score of 19–23 ‘Good Knowledge’; a score of 15–18 ‘Moderate Knowledge’ and 0–14 ‘Poor Knowledge’. Attitudes were elicited using Likert scales with 0 = strongly disagree, 1 = disagree, 2 = neutral, 3 = agreement and 4 = strong agreement. Patients' responses were summarized and a score of 1–32 was considered ‘Negative Attitude’ and a score of 33–44 a ‘Positive Attitude’. Similar Likert scales were used to assess patients' practice where a score of 1–8 was considered ‘Negative Practice’ while a score of 9–12 was considered ‘Positive Practice’.
Statistical analysis
Data were analyzed using SPSS version 19. All statistical tests were performed using 0.05 as the level of significance. One-way ANOVA and Student t- test were used to compare groups. Correlation between variables was assessed using Pearson correlation coefficients. Scale properties of the knowledge and attitude scores were assessed using Cronbach's Alpha (as the practice score essentially asked about all essential elements of good practice this was considered inappropriate for this score). Stepwise linear regression analysis was used to examine the simultaneous effect of various patient characteristics on patient knowledge, practice, attitude, and HbA1c levels.
Results
Of the 575 participants 55% were females, 65% were UAE citizens and 46% were illiterate. Twelve percent were current smokers. The mean (SD) age of the sample was 50 (15) years and the mean duration of diabetes was 9 (7) years. Mean HbA1c was 7.7±(3.3)%. Other patients' socio-demographic and clinical characteristics are shown in Tables 1 and 2 respectively.
Table 1. Socio-Demographic Characteristics of the Study Participants (n = 575).
| Variable | N (%) |
| Sex | |
| Female | 316 (55.1) |
| Level of Education | |
| illiterate | 265 (46.3) |
| elementary | 143 (25) |
| secondary | 105 (18.4) |
| college | 59 (10.3) |
| Age group (Years) | |
| ≤39 | 114 (19.9) |
| 40–49 | 138 (24) |
| 50–59 | 153 (26.7) |
| 60 or above | 169 (29.4) |
| Nationality group | |
| UAE | 374 (65.2) |
| Other Gulf Council countries (GCC) citizens | 85 (14.8) |
| Arabs from other countries | 115 (20) |
| Marital status | |
| Single | 59 (10.3) |
| Married | 417 (73) |
| Divorced | 20 (3.5) |
| Widowed | 75 (13.1) |
| Monthly family income | |
| <5000 Dhs. | 208 (36.9) |
| 5000–9000 Dhs. | 219 (38.9) |
| 10,000–15,000 Dhs. | 101 (17.9) |
| >15,000 Dhs. | 35 (6.2) |
| Occupation | |
| Government employees | 106 (18.6) |
| Private employees | 24 (4.2) |
| Private business | 4 (0.7) |
| Retired | 120 (21.1) |
| Housewives | 279 (49) |
| Students | 36 (6.3) |
| Place of interview | |
| Tawam Hospital | 299 (52) |
| Al-Ain Hospital | 276 (48) |
Table 2. Clinical Characteristics of the Study Participants (n = 575).
| Variable | Proportion of all Diabetics | |
| N | Percent (95% CI) | |
| Type of DM | ||
| Insulin treated diabetes | 198 | 34.9 (30.98–38.82) |
| Non-insulin treated diabetes | 370 | 65.1 (61.18–69.02) |
| Mode of diagnosis | ||
| Incidental | 189 | 34.5 (30.52–38.48) |
| Symptomatic | 359 | 65.5 (61.52–69.48) |
| Family history of DM | ||
| Present | 360 | 64.4 (60.43–68.37) |
| Duration of DM | ||
| <1 year | 47 | 8.5 (6.18–10.82) |
| 1.1–5 years | 143 | 25.8 (22.16–29.44) |
| 5.1–10 years | 151 | 27.2 (23.50–30.90) |
| 10.1–20 years | 183 | 33 (29.09–36.91) |
| >20 years | 31 | 5.6 (3.69–7.51) |
| Other chronic conditions | ||
| Present | 317 | 61.2(57.00–65.40) |
| Glycemic control | ||
| Good (HbA1c <7%) | 74 | 26.9 (21.7–32.1) |
| Acceptable (HbA1c 7–8%) | 45 | 16.4 (12.0–20.8) |
| Poor (HbA1c >8%) | 156 | 56.7 (50.8–62.6) |
Knowledge Assessment
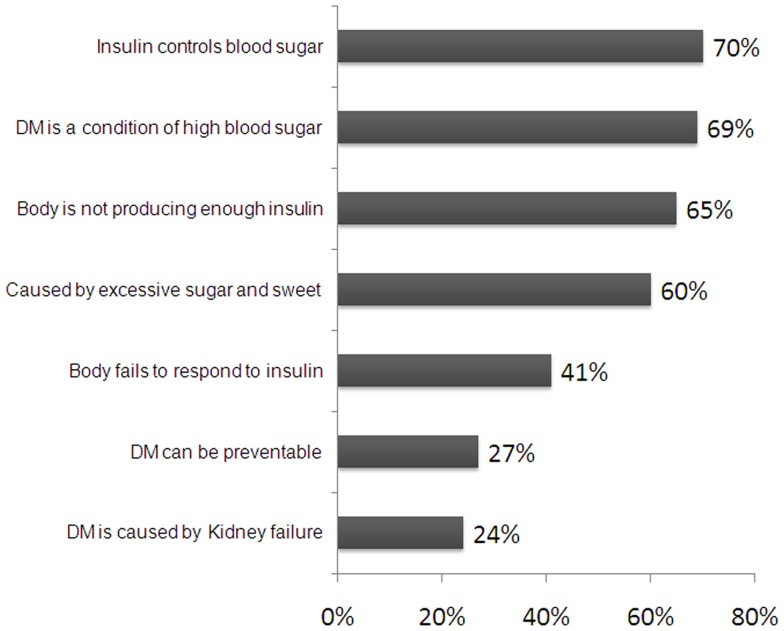
The mean knowledge score was 15.7 (4.4), which fall within our definition of ‘Poor Knowledge’. Cronbach's alpha for the knowledge score was 0.674 and all items, except knowledge about impotence, were positively correlated with total score. In fact, 33% had ‘good knowledge’, 36% had ‘fair knowledge’, and 31% had ‘poor knowledge’. Percentages of correct answers to questions on general DM knowledge and on DM symptoms and complications are shown in Figures 1 and 2 respectively.
Figure 1. Diabetes General Knowledge (n = 575).
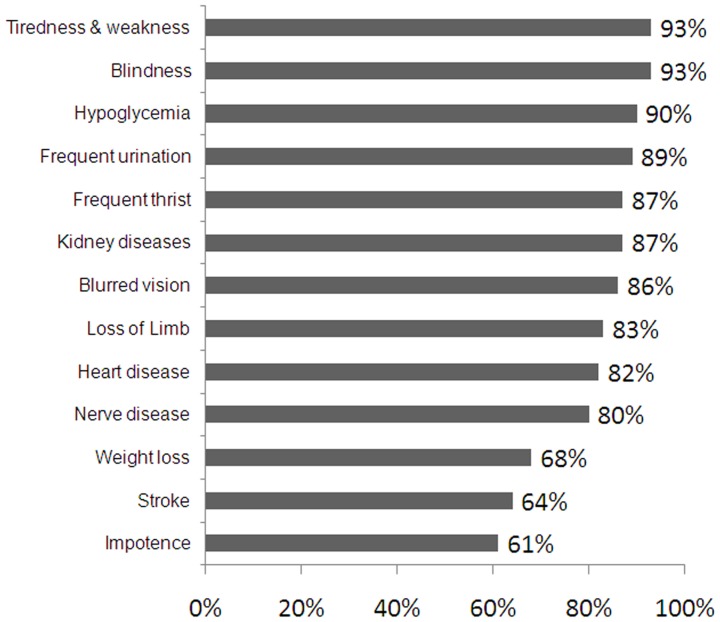
Figure 2. Knowledge of Diabetes Symptoms and Complications(n = 575).
Most (89%) of the surveyed patients had seen a diabetic educator since their diagnosis, but many only a few times. Most patients (87%) cited doctors as the primary source of DM knowledge, but other sources were also frequently mentioned (Table 3).
Table 3. Sources of DM Knowledge among the Study Participants (n = 575).
| Source of DM Health Information (can choose more than one) | N | % (95% C.I.) |
| Doctors | 494 | 87.4 (84.7–90.1) |
| Nurses | 167 | 31.0 (27.1–34.9) |
| Pharmacists | 11 | 2.1(0.9–3.3) |
| Electronic media | 218 | 41.0 (36.8–45.2) |
| Health educator | 161 | 30.5 (26.6–34.4) |
| Dieticians | 106 | 20.1 (16.7–23.5) |
| Friends and family | 179 | 33.3 (29.3–37.3) |
| Published media | 142 | 26.7 (22.9–30.5) |
| Frequency of seeing diabetes educator | ||
| None | 30 | 11.5 (7.6–15.4) |
| Once | 68 | 26 (20.7–31.3) |
| Twice | 50 | 19 (14.2–23.8) |
| More | 114 | 44 (38.0–50.0) |
Knowledge of diabetes varied significantly among nationalities, with Asians (mostly Indians and Pakistanis) having a higher mean knowledge score than UAE citizens, other Arab nationalities, and patients from the Gulf Council Countries. Other factors affecting diabetes knowledge were sex, age, level of education, marital status, profession, income, insulin treatment, mode of diagnosis and duration of diabetes (Table 4). Interestingly, analysis showed a positive correlation between patients' knowledge and the number of contacts with a diabetic education in the last two years.
Table 4. Mean Diabetes Knowledge, Attitudes and Practice Scores for Different Characteristics of the Participants (n = 575).
| Variable | Total know Score | Total Practice Score | Total Attitude score | HbA1c | |
| Mean | Mean | Mean | Mean | ||
| Sex | Male | 17.08 | 24.16 | 27.32 | 7.62 |
| Female | 15.26 | 23.55 | 27.81 | 7.68 | |
| p. value | 0.000 | 0.273 | 0.441 | 0.891 | |
| Age group | < = 39 years | 16.79 | 23.97 | 27.30 | 8.04 |
| 40–49 years | 16.52 | 23.85 | 28.32 | 7.70 | |
| 50–59 years | 16.37 | 24.46 | 27.75 | 7.36 | |
| 60> = | 14.98 | 23.20 | 27.04 | 7.84 | |
| p. value | 0.001 | 0.386 | 0.501 | 0.769 | |
| Marital status | Single | 16.81 | 25.17 | 28.85 | 8.00 |
| Married | 16.43 | 24.08 | 27.66 | 7.71 | |
| Divorced | 14.80 | 21.15 | 27.80 | 7.72 | |
| Widowed | 14.13 | 22.19 | 26.39 | 7.24 | |
| p. value | 0.000 | 0.011 | 0.322 | 0.883 | |
| Nationality | UAE | 15.70 | 23.87 | 27.81 | 7.84 |
| GCC | 15.48 | 22.95 | 26.75 | 7.45 | |
| Other Arabs | 17.73 | 24.23 | 27.62 | 7.54 | |
| Asians | 19.50 | 29.00 | 21.00 | . | |
| p. value | 0.000 | 0.342 | 0.515 | 0.759 | |
| Occupation | Gov. employed | 18.17 | 24.83 | 27.87 | 7.03 |
| Private employee | 18.42 | 24.29 | 30.08 | 7.79 | |
| Retired | 16.46 | 23.94 | 26.74 | 7.12 | |
| Housewife | 14.97 | 23.34 | 27.88 | 7.98 | |
| Private business | 19.25 | 23.75 | 32.25 | 11.00 | |
| Others | 16.11 | 25.81 | 27.42 | 8.54 | |
| Level of education | p. value | 0.000 | 0.181 | 0.293 | 0.448 |
| Illiterate | 14.74 | 23.31 | 27.65 | 7.92 | |
| Primary school | 16.59 | 24.34 | 27.44 | 7.93 | |
| Secondary school | 17.27 | 23.78 | 28.40 | 7.38 | |
| University | 19.48 | 26.05 | 27.16 | 6.31 | |
| Post graduate | 19.67 | 25.00 | 30.67 | 5.30 | |
| p. value | 0.000 | 0.053 | 0.762 | 0.285 | |
| Monthly family income | Less than 5000 | 15.84 | 23.36 | 26.75 | 7.44 |
| 5000–9999 | 16.27 | 24.24 | 28.38 | 7.77 | |
| 10000–15000 | 15.77 | 23.73 | 27.75 | 8.26 | |
| More than 15000 | 18.26 | 25.94 | 28.66 | 6.62 | |
| p. value | 0.008 | 0.133 | 0.127 | 0.570 | |
| Mode of DM diagnosis | Incidental | 17.08 | 24.91 | 28.44 | 7.14 |
| Symptomatic | 15.76 | 23.43 | 27.38 | 7.97 | |
| p. value | 0.000 | 0.009 | 0.111 | 0.124 | |
| Insulin treatment | Yes | 16.20 | 24.27 | 27.32 | 7.47 |
| No | 15.00 | 21.64 | 30.18 | 7.65 | |
| p. value | 0.000 | 0.189 | 0.003 | 0.752 | |
| Frequency of seeing diabetes educator in the past 2 years | None | 15.74 | 23.29 | 28.31 | 7.98 |
| Once | 14.65 | 24.47 | 28.41 | 7.45 | |
| Twice | 18.00 | 24.92 | 27.62 | 7.38 | |
| More than twice | 17.50 | 25.79 | 26.70 | 5.71 | |
| p. value | 0.000 | 0.001 | 0.187 | 0.020 | |
| Duration of diabetes | One year or less | 14.70 | 21.40 | 27.32 | 8.71 |
| 1.1–5 years | 15.93 | 24.00 | 28.22 | 7.82 | |
| 5.1–10 years | 16.10 | 23.83 | 27.62 | 7.17 | |
| 10.1–20 years | 16.46 | 24.60 | 27.57 | 7.93 | |
| p. value (trend) | 0.003 | 0.007 | 0.399 | 0.740 | |
Assessment of Attitudes
Cronbach's alpha of the attitude score was 0.845 and all items were positively correlated with the overall score. Analysis showed that the majority of patients (72%) had a negative attitude towards having diabetes. However, only 6% expressed a ‘negative attitude’ towards the importance of DM care (Table 5), notably of controlling blood sugar levels and body weight, as well as compliance with medications. Bivariate analysis showed that the only factor that is associated with attitude is the type of DM (Table 4).
Table 5. Attitudes towards DM and DM Care among the Study Participants (n = 575).
| Attitudes towards having DM | N (%) |
| Positive attitude | 157 (28) |
| Negative attitude | 410 (72) |
| Attitudes towards the importance of DM care | |
| Positive attitude | 559 (94) |
| Negative attitude | 36 (6) |
Assessment of Patients Practice towards DM Control
Analysis showed that most patients had satisfactory practice, and that the majority had reported regular routine follow up (Table 6). A large minority however, did not follow a diet, or control their weight. Also a substantial proportion was not exercising and admitted lack of compliance to medications Reported blood sugar control and monitoring were generally poor (Table 6). Only 27% of patients had good glycemic control.
Table 6. Diabetes Practices of the Study Participants (n = 575).
| Variable | N | % (95% C.I.) |
| DM practice scores levels | ||
| Good practice | 217 | 37.7 (33.7–41.7) |
| Satisfactory practice | 270 | 47.0 (42.9–51.1) |
| Poor practice | 88 | 15.3 (12.1–17.9) |
| Patients' control of DM | ||
| Always attending DM clinic for follow-up | 452 | 80.4 (77.2–83.6) |
| Never controlling weight | 93 | 17 (13.9–20.1) |
| Not undertaking any physical exercise | 95 | 16.6 (13.6–19.6) |
| Not following any special DM diet | 158 | 27.7 (24.0–31.6) |
| Not complying with medication | 55 | 9.8 (7.4–12.2) |
| Never checked or cared for toes and feet | 103 | 18.1 (15.0–21.2) |
| Never taken care when cutting toe nails | 65 | 11.5 (8.9–14.1) |
| Patients' self control of blood sugar | ||
| Always in good control | 97 | 17.1 (14.0–20.2) |
| Often in good control | 223 | 39.3 (35.3–43.3) |
| Sometimes in good control | 195 | 34.4 (30.5–38.3) |
| Never in good control | 52 | 9.2 (6.8–11.6) |
| Patients' self test of blood sugar | ||
| Always test for blood sugar | 235 | 41.7 (37.7–45.7) |
| Often check for blood sugar | 126 | 22.4 (19.0–25.8) |
| Sometimes take blood sugar test | 67 | 11.9 (9.3–14.5) |
| Never took blood sugar test | 135 | 24 (20.5–27.5) |
| Barriers of self testing among DM patients | ||
| Too expensive | 52 | 10.2 (7.7–12.7) |
| Too painful | 7 | 1.4 (0.4–2.9) |
| Not really needed | 43 | 8.4 (6.1–10.7) |
| Don't know how to read results | 24 | 4.7 (3.0–6.4) |
Bivariate analysis showed (marginally) significant associations between the practice score and level of education, marital status, mode of diagnosis, duration of disease, insulin use and frequency of seeing diabetes educator (Table 4). There were no statistically significant association between patients' practice score and family history of DM, sex, age, nationality, monthly income or occupation (Table 4).
There was a weak, but statistically significant, correlation between the level of knowledge and practice and also between attitudes and practice (r = 0.320, p<0.001 and r = 0.270, p<0.001, respectively). Similarly there was a weak, but statistically significant association between knowledge and attitude scores (r = 0.115, p = 0.006). HbA1c was not statistically significantly correlated with any of the three scores.
Multivariate Analysis
Stepwise linear regression for the total knowledge scores, total practice scores, and total attitudes scores on covariates identified in bivariate analysis showed several significant (adjusted) associations. Table 7 shows the results for the knowledge score and Table 8 for the practice score. No variables were identified as significantly predictive of the attitude score in this regression analysis. Regression analysis, using HbA1c as a dependent variable and the covariates of age, sex, level of education, nationality (UAE or not) , type of DM, and marital status (married or not) as independent variables showed that only the level of education (as continuous variable) and type of DM were (negatively with level of education) independently associated with HbA1c levels (Table 9).
Table 7. Patients Characteristics associated with Diabetes Knowledge Score in stepwise linear regression (n = 575).
| Model | Un -standardized Coefficients | Sig. | |
| B | Std. Error | ||
| (Constant) | 14.996 | .905 | .000 |
| Level of education | 1.210 | .164 | .000 |
| Gender (Male) | 1.026 | .325 | .002 |
| Type of DM | −1.014 | .340 | .003 |
| Married | 1.260 | .354 | .000 |
| Family history of DM | −.828 | .331 | .011 |
| UAE nationality | .716 | .328 | .029 |
| Duration of DM | .061 | .022 | .007 |
| Freq. of seeing diabetes educator | .256 | .098 | .009 |
Dependent variable: Total Knowledge Score. Co variables entered were: level of education, gender, age, type of DM (insulin treated/not on insulin), married, frequency of seeing a DM educator in the past 2 years, duration of DM, UAE nationality, family income, mode of diagnosis, family history of DM, being employed.
Table 8. Patients characteristics associated with Practice Score in stepwise linear regression (n = 575).
| Model | Un -standardized Coefficients | Sig. | |
| B | Std. Error | ||
| (Constant) | 20.081 | .865 | .000 |
| Married | 1.250 | .617 | .043 |
| DM duration | 0.096 | .039 | .014 |
| Level of education | 0.732 | .280 | .009 |
| Freq. of seeing diabetes educator | 0.541 | .173 | .002 |
Dependent Variable: Total Practice Scores. Co variables entered were: level of education, sex, age, type of DM (insulin treated/not on insulin), married, frequency of seeing a DM educator in the past 2 years, duration of DM, UAE nationality, family income, mode of diagnosis, family history of DM, being employed.
Table 9. Patients Characteristics associated with Glycemic Control in stepwise linear regression (n = 575).
| Model | Un -standardized Coefficients | Sig. | |
| B | Std. Error | ||
| (Constant) | 10.484 | .966 | .000 |
| Type of DM | −1.169 | . 494 | .019 |
| Level of education | −.448 | .219 | .042 |
Dependent Variable: HbA 1C. .Co variables entered: age, sex, level of education, UAE nationality, type of DM (insulin treated/not on insulin), married (0/1).
Discussion
Studies from both developed and developing countries have reported that diabetes knowledge is generally poor among diabetic patients [4]–[7], [14]–[17]. However, it is difficult to compare our results with others, as most of the studies used different instruments and/or are carried out among different ethnic or age groups. This study shows that the levels of knowledge seemed particularly low in the UAE. For example, two thirds of our patients cited excessive sugar consumption as the primary cause of the disease, while less than one third was aware that type 2 diabetes can be prevented or delayed. However, patients' general awareness of diabetes symptoms and complications was relatively high, perhaps because they had experienced these symptoms themselves or observed them in fellow-patients. We observed several correlates of knowledge, attitudes and practice. Some of our findings, e.g. that men had higher mean knowledge score than women appear to conflict with other studies [17], [18], [19]. Other correlates, such as the effects of education, are predictable. Of all significant correlates of knowledge and practice, education is the only modifiable risk factor. Fortunately, education is now practically universal in the UAE, and illiteracy is expected to disappear gradually.
Our study also shows that a history of diabetes in first degree relatives has a positive impact on diabetes knowledge. Having a close relative with chronic disease may be a good source of health information [20], [21], but such informal sources cannot be relied upon.
A major point to address therefore is regular access to/contact with diabetic educators which currently is severely substandard. However, while improved knowledge would definitely facilitate patient management, it would not necessarily guarantee improvement in the overall outcomes. This study showed no correlation between the level of knowledge and glycemic control, while other studies reported conflicting findings [22], [23], [24]. It is therefore essential to direct more resources to improving both the knowledge of diabetic patients, and the development of innovative tools and educational models that improve patient's compliance and practices. Such efforts would require further in-depth research on diabetic patients' knowledge, attitudes and practices and how they interrelate.
As our study was outpatient hospital based, the results may not be truly representative of all DM patients in the UAE. In particular, the fact that the study was conducted in university teaching hospitals, where diabetes education may be more readily accessible to patients, raises concerns that diabetic patients attending primary health care centers in the region with less access to diabetes education may have even poorer diabetes awareness and practices. The results suggest that special attention and increased care are required for the elderly diabetic patients in the UAE who are mostly illiterate. Also, patients on insulin should receive special attention as knowledge of DM management for them is a key.
Acknowledgments
Our special thanks are extended to the staff, doctors and nurses working in Tawam and Al-Ain hospitals where the survey was conducted, for their invaluable support. Our special thanks go to Mr. Hussain Al-Ajab from the Institute of Public Health, College of Medicine & Health Sciences, UAE University, for his help in the data analysis and the tabulation of study results.
Funding Statement
UAE University funded this research. However, the funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. McPherson ML, Smith SW, Powers A, Zuckerman IH (2008) Association between diabetes patients' knowledge about medications and their blood glucose control. Res Social Adm Pharm Mar; 4 (1) 37–45. [DOI] [PubMed] [Google Scholar]
- 2. Norris SL, Engelgau MM, Narayan KM (2001) Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care 24: 561–87. [DOI] [PubMed] [Google Scholar]
- 3. Duke SA, Colagiuri S, Colagiuri R (2009) Individual patient education for people with type 2 diabetes mellitus. Cochrane Database Syst Rev Jan 21 (1) CD005268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ben Abdelaziz A, Thabet H, Soltane I, Gaha K, Gaha R, et al. (2007) Knowledge of patients with type 2 diabetes about their condition in Sousse, Tunisia. East Mediterr Health J May–Jun; 13 (3) 505–14. [PubMed] [Google Scholar]
- 5. Kamel NM, Badawy YA, el-Zeiny NA, Merdan IA (1999) Sociodemographic determinants of management behavior of diabetic patients Part 2. Diabetics' knowledge of the disease and their management behavior. EMHJ 5: 5, 974–983. [PubMed] [Google Scholar]
- 6. Khan LA, Khan SA (2000) Level of Knowledge and Self-Care in Diabetics in a Community Hospital in Najran. Annals of Saudi Medicine Vol 20 (Nos 3–4). [DOI] [PubMed] [Google Scholar]
- 7. Al-Adsani AM, Moussa MA, Al-Jasem LI, Abdella NA, Al-Hamad NM (2009) The level and determinants of diabetes knowledge in Kuwaiti adults with type 2 diabetes. Diabetes Metab Apr; 35 (2) 121–8. [DOI] [PubMed] [Google Scholar]
- 8.International Diabetes Federation (IDF) Atlas: Available: http://www.idf.org/diabetesatlas/5e/the-global-burden. Accessed 2012 Jun 18.
- 9. Al-Kaabi J, Al-Maskari F, Saadi H, Afandi B, Parkar H, et al. (2009) Physical activity and reported barriers to activity among type 2 diabetic patients in the United Arab Emirates. Rev Diabet Stud Winter 6 (4) 271–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Al-Kaabi J, Al-Maskari F, Saadi H, Afandi B, Parkar H, et al. (2008) Assessment of dietary practice among diabetic patients in the United Arab Emirates. Rev Diabet Stud Summer 5 (2) 110–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Abdullah L, Margolis S, Townsend T (2001) Primary health care patients' knowledge about diabetes in the United Arab Emirates. East Mediterr Health J Jul–Sep;7 (4–5) 662–70. [PubMed] [Google Scholar]
- 12.The Michigan Diabetes Research and Training Center (MDRTC), University of Michigan Health System website. Available: http://www.med.umich.edu/mdrtc/profs/survey.html. Accessed 2012 Jun 4.
- 13. American Diabetes Association (2002) Standards of medical care for patients with diabetes mellitus (position statement). Diabetes care 25: S33–49. [DOI] [PubMed] [Google Scholar]
- 14. He X, Wharrad HJ (2007) Diabetes knowledge and glycemic control among Chinese people with type 2 diabetes. Int Nurs Rev Sep; 54 (3) 280–7. [DOI] [PubMed] [Google Scholar]
- 15. Speight J, Bradley C (2001) The ADKnowl: identifying knowledge deficits in diabetes care. Diabet Med 2001 Aug;18 (8) 626–33. [DOI] [PubMed] [Google Scholar]
- 16.Ardeňa GJ, Paz-Pacheco E, Jimeno CA, Lantion-Ang FL, Paterno E, et al. (2010) Knowledge, attitudes and practices of persons with type 2 diabetes in a rural community: Phase I of the community-based Diabetes Self-Management Education (DSME) Program in San Juan, Batangas, Philippines. Diabetes Res Clin Pract Nov; 90 ((2) ):160–6. Epub 2010 Sep 9. [DOI] [PubMed] [Google Scholar]
- 17. Murata GH, Shah JH, Adam KD, Wendel CS, Bokhari SU, et al. (2003) Factors affecting diabetes knowledge in Type 2 diabetic veterans. Diabetologia 46: 1170–8. [DOI] [PubMed] [Google Scholar]
- 18. Rhee MK, Cook CB, El-Kebbi I, Lyles RH, Dunbar VG, et al. (2005) Barriers to diabetes education in urban patients: perceptions, patterns, and associated factors. Diabetes Educ May–Jun; 31 (3) 410–7. [DOI] [PubMed] [Google Scholar]
- 19. Hawthorne K, Tomlinson S (1999) Pakistani moslems with Type 2 diabetes mellitus: effect of sex, literacy skills, known diabetic complications and place of care on diabetic knowledge, reported self-monitoring management and glycaemic control. Diabet Med Jul; 16 (7) 591–7. [DOI] [PubMed] [Google Scholar]
- 20. Harrison TA, Hindorff LA, Kim H, Wines RC, Bowen DJ, et al. (2003) Family history of diabetes as a potential public health tool. Am J Prev Med Feb; 24 (2) 152–9. [DOI] [PubMed] [Google Scholar]
- 21. Ezenwaka CE, Offiah NV (2003) Patients' health education and diabetes control in a developing country. Acta Diabetol Dec; 40 (4) 173–5. [DOI] [PubMed] [Google Scholar]
- 22. Al-Qazaz HKh, Sulaiman SA, Hassali MA, Shafie AA, Sundram S, et al. (2011) Diabetes knowledge, medication adherence and glycemic control among patients with type 2 diabetes. Int J Clin Pharm Dec;33 (6) 1028–35. [DOI] [PubMed] [Google Scholar]
- 23. Panja S, Starr B, Colleran KM (2005) Patient knowledge improves glycemic control: is it time to go back to the classroom? J Investig Med Jul; 53 (5) 264–6. [DOI] [PubMed] [Google Scholar]
- 24. Ozcelik F, Yiginer O, Arslan E, Serdar MA, Uz O, et al. (2010) Association between glycemic control and the level of knowledge and disease awareness in type 2 diabetic patients. Pol Arch Med Wewn Oct; 120 (10) 399–406. [PubMed] [Google Scholar]


