Abstract
Objective
Rapid cycling (RC) affects 13–30% of bipolar patients. Most of the data regarding RC have been obtained in tertiary care research centers. Generalizability of these findings to primary care populations is thus questionable. We examined clinical and demographic factors associated with RC in both primary and tertiary care treated populations.
Method
Clinical data were obtained by interview from 240 bipolar I disorder (BDI) or bipolar II disorder (BDII) community-treated patients and by chart reviews from 119 bipolar patients treated at an outpatient clinic of a teaching hospital.
Results
Lifetime history of rapid cycling was present in 33.3% and 26.9% of patients from the primary and tertiary care samples, respectively. Among community-treated patients, lifetime history of RC was significantly associated with history of suicidal behavior and higher body mass index. There was a trend for association between RC and BDII, psychiatric comorbidity, diabetes mellitus, as well as lower age of onset of mania/hypomania. In the tertiary care treated sample there was a trend for association between lifetime history of RC and suicidal behavior. Tertiary versus primary care treated subjects with lifetime history of RC demonstrated markedly lower response to mood stabilizers.
Conclusions
Lifetime history of RC is highly prevalent in both primary and tertiary settings. Even primary care treated subjects with lifetime history of RC seem to suffer from a more complicated and less treatment-responsive variant of bipolar disorder. Our findings further suggest relatively good generalizability of data from tertiary to primary care settings.
Keywords: bipolar disorders, diabetes, primary care, rapid cycling, suicide, tertiary care
Rapid cycling (RC) is included in the DSM-IV as a course specifier of bipolar I disorder (BDI) or bipolar II disorder (BDII). It affects 13–30% of bipolar patients, depending on diagnostic criteria and inclusion of BDII subjects (1–3). Since the original introduction of the term by Dunner and Fieve (4), studies have examined RC in the context of demographic, clinical factors, illness course, and response to treatment. The majority of studies have identified RC as a marker for risk of recurrence, suicidal behavior, comorbidity, poor outcome, decreased functioning, and relative treatment resistance not only to lithium, but also valproate (5–8). In light of these findings, the importance of continuing to study the phenomenology of RC bipolar disorder in the hope of improving the mental health, social burden, and quality of life of patients is clear.
Most of the data pertaining to RC have been obtained in research centers. Hence, they may be biased by the selection of patients with particular clinical and treatment characteristics and their generalizability to the primary care population is questionable. Although there is no study in bipolar disorder (BD) comparing primary versus secondary or tertiary care treated patients, such data are available for major depression and suggest marked differences between primary and tertiary care treated subjects. Depression in primary care patients is less severe (9), and may present with a different subset of depressive symptoms (10, 11), different rates of suicidality (11), preceding life events (12), and different demographic characteristics including sex, age, and comorbidity (9). In fields of medicine outside of psychiatry, generalizability from the secondary to the primary setting has also been questioned (13).
Despite the fact that almost three-quarters of bipolar patients in some countries are treated in primary care settings (14), primary care treated subjects remain the least studied population. To the best of our knowledge, there has not yet been a study examining the clinical and demographic factors associated with RC in a purely community-treated population. In the absence of more specific data, findings from tertiary care centers with possibly limited generalizability to primary care settings are used.
The principal aim of this study was to characterize clinical and demographic variables associated with lifetime history of RC in community-treated BDI and BDII patients. In the absence of data from primary care, we expected to replicate the findings from tertiary care settings, e.g., association between RC and comorbidity, BDII, suicidal behavior, female sex, hypothyroidism, and relative treatment resistance to lithium and also valproate. We then compared these data with findings obtained from patients treated at a university-aflliated outpatient department, expecting to find greater severity of illness among tertiary care treated subjects, manifesting as a higher proportion of RC and lower response to treatment.
Patients and methods
Primary care treated subjects
Subjects were recruited through the Maritime Bipolar Registry, a community-based project in the Maritime Provinces of Canada encompassing both metropolitan and rural areas in Nova Scotia, New Brunswick, and Prince Edward Island (7). The registry is voluntary. Patients who are treated by a family physician or community psychiatrist are informed about the opportunity to participate in the study. Patients who had given consent to participate in the project were interviewed by a psychiatrist or research nurse with experience with diagnostic interviewing from previous studies of affective disorders. Prior to conducting the assessments, all interviewers underwent extensive training consisting of participation on interviews and interviews under supervision. High inter-rater reliability was established among these researchers based on diagnostic reviews of eight detailed cases with a variety of major psychiatric disorders (weighted κ of 0.84). The diagnostic interviews followed the Schedule for Affective Disorders and Schizophrenia–Lifetime version (SADS-L) format (15). The diagnostic interview was expanded for the section of mood disorders to allow for diagnoses based on both Research Diagnostic Criteria (16) and DSM-IV criteria. We used DSM-IV diagnoses throughout the text. We also obtained further details about the illness. These included details about clinical course (i.e., single episode, completely episodic, episodic with residual symptoms, chronic fluctuating, chronic) using the lifetime charting approach, history of treatments and treatment responses, family history, history of suicidal behavior, and physical comorbidities. Medical comorbidity was ascertained based on previous diagnosis and treatment for each selected medical condition. Clinical notes and progress and treatment reports were also reviewed to clarify the clinical information. All subjects were receiving maintenance treatment at the time of interviews. None were assessed during acute episodes of the illness. Patients continued to be treated by their family physician or community psychiatrist. Ethnically, most participants were of Irish, Scottish, or French Acadian origin. The study was approved by the ethics committee of the Capital District Health Authority, Halifax, Nova Scotia, and all included subjects signed the informed consent after a complete description of the study.
Tertiary care treated subjects
We reviewed clinical records of a consecutive series of patients selected from a general mental health outpatient clinic located in a tertiary care teaching facility. The case reviews followed a structured procedure. In particular, we documented the clinical course of BD, including the number, duration, and treatment of mood episodes, history of treatment, compliance, drug levels where applicable, and use of concomitant medication.
Clinical assessments common for both groups
Lifetime treatment response to lithium, carbamazepine, valproate, lamotrigine, and olanzapine was determined in both the primary and tertiary care treated subjects, using the previously described scale (17). The scale was developed specifically for retrospective evaluation of prophylactic treatment response in patients not treated according to a research protocol. The scale weights the degree of improvement in the course of treatment (subscale A) by five factors (subscale B) which assist in determining the probability that the observed improvement is a result of the treatment rather than a spontaneous improvement or an effect from additional medication. Inter-rater reliability scores were calculated based on reviews of 10 randomly selected charts by three independent clinical reviewers (concordance of ratings 90%, weighted κ of 0.8). For each patient, treatment response was evaluated only to those mood stabilizers received for a minimum of six months at adequate doses. The lithium, valproate, or carbamazepine dosage was considered adequate if it produced levels in the therapeutic range. For lamotrigine, the daily dose had to be at least 100 mg; for olanzapine, at least 5 mg.
The RC course specifier was diagnosed in both study groups using the DSM-IV criteria. The DSM-IV definition of RC has been shown to have good inter-rater reliability and specificity (18). This study focused on correlates of lifetime, not current RC.
Statistical analyses
To analyze the association between RC and categorical variables [sex, comorbidity, bipolar subtype, history of suicidal behavior, electro-convulsive treatment (ECT), treatment with anti-depressants, presence of psychosis with episodes, hypothyroidism, diabetes mellitus, high blood pressure, response to medications], we performed Pearson χ2 tests. Differences in body mass index (BMI) between patients with and without RC were compared using the t-test. In order to decrease the risk of Type I error, we used a more stringent p = 0.01 as a threshold for statistical significance. In order not to overly inflate the risk of Type II error we report results with 0.01 < p < 0.05 as trend associations. Variables with a trend or significant associations were entered into a stepwise multiple logistic regression to control for intercorrelations. All analyses were performed using BMDP software.
Results
Primary care treated sample
At the time of the analyses, data from 252 patients were included in the registry. Information about RC was missing in 12 patients. There were 164 BDI and 76 BDII patients, 91 men and 149 women, in the age range of 15–82 years (mean age 44.1 ± 12.2). A total of 234 patients (92.9%) were treated with mood stabilizers (lithium or anticonvulsants), 182 (75.8%) with antidepressants, and 134 (55.8%) with antipsychotics. Only 12 patients (5%) were treated with monotherapy, 101 patients (42.1%) received a combination of two, and 91 (37.9%) patients a combination of three psychotropic drug classes. In 36 patients information about at least one drug class was missing.
Lifetime history of RC was present in 33.3% (80/240) of the community-treated patients. RC was associated with a history of suicidal behavior and higher BMI. There was a trend association (0.01 < p < 0.05) between RC and diagnosis of BDII, psychiatric non-affective comorbidity, diabetes mellitus, an earlier age of onset of mania/hypomania, and lower treatment response to valproate among primary care treated subjects. No association was observed between lifetime history of RC and sex, hypothyroidism, hypertension, history of psychotic episodes, family history of psychiatric disorders, history of antidepressant or antipsychotic treatment, age of onset of depression, treatment response to lithium, and a history of ECT among primary care treated subjects. For details, see Table 1. There were no significant differences between proportions of RC patients with partial/complete response to valproate versus lithium.
Table 1.
Variables associated with lifetime history of rapid cycling in the primary care treated sample
| Characteristic | Lifetime history of rapid cycling
|
(χ2)a or t | p | |
|---|---|---|---|---|
| Yes n= 80 |
No n = 160 |
|||
| History of suicidal behavior | 34 (44.2) | 33 (20.6) | 14.2 | 0.0002 |
| Body mass index (kg/m2), mean ± SD | 28.9 ± 11.6 | 24.3 ± 11.4 | 2.9 | 0.004 |
| Diabetes mellitus | 14 (17.9) | 14 (8.8) | 4.3 | 0.04 |
| Age of onset of mania/hypomania (years), mean ± SD | 27.7 ± 11.5 | 30.9 ± 11.0 | 2.1 | 0.04 |
| Bipolar I disorder | 48 (60) | 116 (72.5) | 3.9 | 0.05 |
| Comorbidity | 41 (63.1) | 67 (48.2) | 3.9 | 0.05 |
| Valproate efficacy complete/partial | 27 (62.8) | 52 (80.0) | 3.9 | 0.05 |
| Lithium efficacy complete/partial | 36 (64.3) | 84 (77.8) | 3.4 | 0.06 |
| History of electroconvulsive therapy | 18 (22.8) | 21 (13.1) | 3.6 | 0.06 |
| Age of onset of depression (years), mean ± SD | 23.4 ± 10.6 | 26.3 ± 12.0 | 1.8 | 0.08 |
| Treatment response to at least one mood stabilizer | 62 (80.5) | 122 (88.4) | 2.49 | 0.11 |
| Hypothyroidism | 24 (38.7) | 55 (31.3) | 1.2 | 0.28 |
| Psychotic episodes | 36 (50.0) | 88 (58.3) | 1.35 | 0.24 |
| Lifetime history of antidepressant treatment | 63 (87.5) | 119 (82.1) | 1.05 | 0.31 |
| Family history of psychiatric disorders | 62 (77.5) | 134 (83.8) | 1.39 | 0.24 |
| Hypertension | 13 (16.7) | 20 (12.5) | 0.73 | 0.39 |
| Lamotrigine efficacy | 16 (66.7) | 14 (56.0) | 0.59 | 0.44 |
| Lifetime history of antipsychotic treatment | 47 (62.7) | 87 (57.6) | 0.53 | 0.47 |
| Female | 50 (62.5) | 99 (61.5) | 0.02 | 0.88 |
| Combination of 2 versus 3 medications | 35 (52.2) | 67 (53.2) | 0.006 | 0.94 |
Values are presented as n (%) except where indicated.
df = 1 for all χ2 analyses.
Multivariate analyses
We included all differences with p < 0.05 from bivariate analyses into a stepwise logistic regression model. After controlling for other variables, only history of diabetes mellitus, suicidal behavior, diagnosis of BDII, and an earlier age of onset of mania/hypomania remained significantly associated with lifetime history of RC in this model. History of ECT, psychiatric comorbidity, age of onset of depression, and BMI dropped out of the regression model; for details, see Table 2.
Table 2.
Variables associated with lifetime history of rapid cycling in logistic regression model
| Variable | β | SE β | β/SE β | p |
|---|---|---|---|---|
| History of suicidal behavior | 1.10 | 0.36 | 3.05 | 0.001 |
| Diabetes mellitus | 1.12 | 0.5 | 2.27 | 0.01 |
| Age of onset of mania/hypomania | 0.04 | 0.02 | 2.17 | 0.02 |
| Diagnosis (bipolar I disorder versus bipolar II disorder) | −0.66 | 0.359 | −1.85 | 0.03 |
Psychiatric comorbidity, age of onset of depression, body mass index = ns.
Tertiary care treated sample
At the time of data analysis, records of 120 subjects were reviewed. Data concerning RC were missing in one subject. There were 82 BDI and 37 BDII patients, 37 men and 82 women, in the age range of 20–81 years (mean age 44.5 ± 14.1). A total of 77 (64.7%) subjects were treated with lithium, 108 (90.8%) with anticonvulsants (valproate, carbamazepine, lamotrigine) and seven (5.9%) with olanzapine.
Lifetime history of RC was present in 26.9% (32/119) of the tertiary care treated subjects. It was associated with a history of suicidal behavior. There was a trend association (0.01 < p < 0.05) between RC and a poor treatment response to first medication prescribed among tertiary care treated subjects. Lifetime history of RC was present in similar proportions among BDI and BDII patients, with no difference in prevalence between men and women. There was no association between lifetime history of RC and psychiatric comorbidity or family history of psychiatric disorders. The percentage of lifetime responders to long-term treatment with at least one mood stabilizer (lithium, olanzapine, lamotrigine, carbamazepine, valproate) was not significantly different between patients with versus patients without history of RC (26.7% versus 35.3%, respectively) in the tertiary care setting. There were too few lithium or valproate responders in this dataset to allow for separate analyses. For details, see Table 3.
Table 3.
Variables associated with lifetime history of rapid cycling in the tertiary care treated sample
| Characteristic | Lifetime history of rapid cycling
|
(χ2)a or t | p | |
|---|---|---|---|---|
| Yes (n = 32) n (%) |
No (n = 87) n (%) |
|||
| History of suicidal behavior | 17 (53.1) | 26 (30.6) | 5.1 | 0.02 |
| Response to first medication | 3 (9.4) | 23 (26.4) | 4.0 | 0.05 |
| Psychosis with episode | 9 (28.1) | 39 (47.0) | 3.4 | 0.07 |
| Comorbidity | 26 (81.2) | 56 (66.7) | 2.4 | 0.12 |
| Lithium response | 3 (15.8) | 20 (34.5) | 2.4 | 0.12 |
| Bipolar I disorder | 19 (59.4) | 63 (72.4) | 1.86 | 0.17 |
| Treatment response to at least one mood stabilizer | 8 (26.7) | 30 (35.3) | 0.75 | 0.39 |
| Family history of psychiatric disorders | 14 (46.7) | 43 (53.1) | 0.36 | 0.55 |
| Female | 23 (71.9) | 59 (67.8) | 0.18 | 0.67 |
df = 1 for all χ2 analyses.
Primary versus tertiary care treated patients
The primary and tertiary care samples were comparable with regard to mean age and proportion of women. The proportion of patients with lifetime history of RC did not significantly differ between primary and tertiary care treated patients [80/240 (33.2%) versus 32/119 (26.9%); χ2 = 1.54; df = 1; p = 0.21]. Whereas 50% (36/72) of primary care treated patients with a history of RC suffered from psychosis during episodes, only 28.1% (9/32) among tertiary care treated subjects did (χ2 = 4.32; df = 1; p = 0.04). In comparison with their primary care treated counterparts, tertiary care treated patients with a history of RC had a significantly lower lifetime treatment response to medications [8/30 (26.7%) versus 62/77 (80.5%); χ2 = 27.68, df = 1, p < 0.0001].
There were no differences in proportion of BDI [19/32 (59.4%) versus 48/80 (60%), χ2 = 0.004; df = 1; p = 0.95], women [50/80 (62.5%) versus 23/32 (71.9%); χ2 = 0.89; df = 1; p = 0.35], and patients with history of suicidal behavior [17/32 (53.1%) versus 34/77 (44.2%); χ2 = 0.73; df = 1; p = 0.39] between tertiary and primary care treated subjects with a history of RC. For details, see Fig. 1.
Fig. 1.
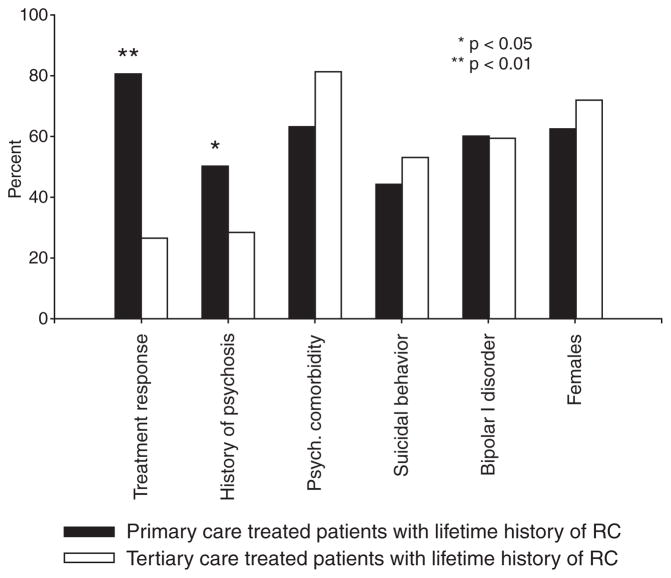
Differences between patients with lifetime history of rapid cycling (RC) treated in the primary and tertiary care setting.
Discussion
In keeping with a priori hypotheses, RC among primary care treated subjects was associated with history of suicidal behavior and there was a trend association between RC and psychiatric comorbidity, lower treatment response to valproate, and BDII.
Contrary to a priori hypotheses, we observed a similar treatment response to lithium among primary care treated patients with a history versus without a history of RC. This may be due to different methods for measuring lithium response. Initial studies described failure of lithium to fully prevent illness recurrences (4, 19). But a recent meta-analysis considering a partial response as well showed that 59% of patients with RC demonstrated at least 50% reduction in symptoms (6). This is in keeping with our data, where 64% of RC treated in the community showed at least partial lithium response. Lithium has a variety of biological effects, including interactions with ion channels, neurotransmitters, second messengers, and transcription factors (20). It is conceivable that the partial response seen in RC patients is based on different mechanisms than the full response in more typical bipolar disorder.
It is widely held that women are more likely than men to manifest RC. Indeed, women comprised 62.5% and 71.9% of subjects with lifetime history of RC in the primary and tertiary care samples, respectively. However, the proportion of women among RC patients in both the primary and tertiary care treated samples was not significantly different from the proportion of women among non-rapid cycling (NRC) subjects. This is in keeping with recent analyses of data which suggest that the preponderance of female patients with RC may be overstated and related to overrepresentation of women in research samples (6, 21) and to definitions of RC, which suspend the criteria for duration of affective episodes (18).
Sex distribution favoring women is thought to explain the association between BDII and RC (22). Our findings do not support this hypothesis, as we observed a trend for significantly more BDII among primary care treated RC patients in absence of difference in proportion of sex between RC and NRC patients. The association between RC and BDII may be due to the preponderance of depressive episodes among RC patients (22), which may make these patients more susceptible to antidepressant-induced rapid mood fluctuations (23). The lack of differences in proportion of subjects with history of antidepressant treatment between RC and NRC subjects, however, does not support this explanation. Alternatively, within the framework of phenotypic spectra of BD, mood lability is a hallmark of characterological phenotype with a higher preponderance of BDII (24).
In addition to a priori hypotheses, we observed a lower age of onset of mania/hypomania in RC patients. The literature regarding age of onset in patients with RC is inconsistent. Some reports showed earlier age of onset among RC patients (25, 26), congruent with our findings. Others reported either later age of onset (27) or no difference in age of onset between RC and NRC patients (22, 28). These discrepancies may be due to the existence of several distinct mechanisms, which may play disproportionate roles in the pathophysiology of RC in early- versus late-onset mood disorders. Rapid cycling has been associated with diffuse brain pathology, which is more likely to occur later in life (29). On the other hand, pediatric BD seems to be characterized by labile, overly responsive mood, resulting in rapid or even continuous cycling (30). This instability of mood in pediatric patients may be related to differential development of subcortical and cortical brain areas (31) and appears to be a transient phenomenon in the majority of cases (25).
From the exploratory analyses regarding Axis III comorbidities, it appears that subjects with a lifetime history of RC are especially likely to suffer from diabetes mellitus and high BMI, which were intercorrelated. High BMI among RC patients does not seem to be related to polypharmacy and side effects of medications (6), since we did not observe increased rates of treatment with antipsychotics or with combinations of more than two medications among patients with RC in the community-treated sample. We can speculate that the association between RC and high BMI/diabetes mellitus may be due to lifestyle issues or presence of atypical depressive symptoms (hypersomnia, hyperphagia, carbohydrate craving). It is also possible that both mood disorders and diabetes mellitus share some pathophysiological mechanisms such as hypothalamo-pituitary-adrenal axis abnormalities, dysregulation in glycogen synthase kinase 3β, or brain-derived neurotrophic factor signaling (32, 33).
We did not find increased prevalence of hypothyroidism among patients with a lifetime history of RC. Hypothyroidism is frequently described as a hallmark of RC (28, 34, 35). On the other hand, some studies refute this association (36–40). A recent meta-analysis showed that the association between RC and hypothyroidism may be more pronounced when current as opposed to lifetime definition of RC is used (6). Furthermore, data from three studies conducted purely with inpatient samples (28, 39, 40) found high rates of hypothyroidism in both RC and NRC patients. Rather than being specific to RC, thyroid dysfunction may be associated with various forms of refractory bipolar disease.
As for the comparisons between primary and tertiary care treated subjects, in keeping with a priori expectations, tertiary care treated subjects with history of RC demonstrated markedly lower lifetime treatment response to mood stabilizers than their primary care treated counterparts. On the other hand, we found similar prevalence of RC among primary and tertiary care treated subjects. One potential explanation is that frequency of cycling does not have to correlate with severity of episodes, as evidenced by the association between RC and BDII in this and other studies [for review see Kupka et al. (6)]. It is possible that RC patients represent an extreme on the continuum of frequency, but not severity of episodes and thus continue to be treated in primary care settings, even though their treatment response is low (8, 41).
The hypothesis that RC does not necessarily have to be a marker for severity of episodes is also supported by the trend for lower rates of psychotic symptoms among RC patients, especially in the tertiary care setting. Psychosis may be an independent risk factor for disease severity, which does not necessarily concur with RC. Serreti et al. (3), for example, also reported that patients with RC showed less severe lifetime psychotic symptomatology than did NRC patients. These findings also fit well with the conceptual framework of phenotypic spectra of bipolar disorders (psychotic, characterological, and classic forms of bipolar disorders). Psychosis, severe manic episodes, and extreme mood lability in this model are characteristics of different phenotypic clusters (24).
We were unable to replicate the association between RC and BDII and RC and comorbidity in the tertiary care treated subjects. The fact that there were over twice as many patients in the primary care group as in the tertiary care group could have accounted for the larger number of significant findings in the primary than the tertiary care groups (i.e., greater power to detect differences in the larger sample).
Our findings in patients with lifetime history of RC are congruent with results of previous studies in patients with current rapid cycling. This is in keeping with a recent meta-analysis, where, aside from hypothyroidism, there were no significant differences between studies using current versus lifetime definitions of RC in the prevalence of females, BDII, history of suicidal behavior, and family history of mood disorders (6).
There are several limitations of this study. These include retrospective assessment, naturalistic design of data collection, differences in data collection in primary versus tertiary care settings and potential for selection bias. A retrospective design hinders the possibility to assess causality and makes the evaluation of number and polarity of mood episodes less accurate than prospective evaluation. This limitation, however, applies to a number of other studies in this field, including recent large-scale endeavors, such as the Systematic Treatment Enhancement Program (26). When considering the findings regarding treatment response, a naturalistic design of data collection in both groups should be taken into account. Furthermore, we evaluated a lifetime history of treatment response, not treatment response during periods of rapid cycling. Information about patients treated in the tertiary care setting was obtained from chart reviews, whereas primary care treated subjects were assessed in an interview. The tertiary care treated subjects were a part of a separate study. They were not selected with the goal of comparing them to the primary care treated subjects. Thus, there is only a partial overlap in studied variables between the groups. However, the two groups were comparable with respect to age and sex. Selection bias is inherent to every clinical study, as the willingness of patients to participate in research studies varies and some will always refuse to participate. Despite that, the primary care treated population likely reflects the general psychiatric population better than the tertiary care treated subjects.
Conclusions
Lifetime history of RC is highly prevalent in both primary (33%) and tertiary (27%) care treated patients, without significant differences in prevalence between these two groups. Our findings can be divided into two parts. The first cluster of results suggests that even primary care treated patients with a lifetime history of RC may suffer from a more complicated form of BD which is characterized not only by high prevalence of psychiatric but also Axis III comorbidity (e.g., diabetes mellitus, high BMI), a high rate of suicidal behavior, and lower age of onset of mania/hypomania. The second cluster of findings indicates that patients with a lifetime history of RC are more difficult to treat, with a higher proportion of refractoriness to treatment with lithium, as well as valproate.
The differences in our study between primary and tertiary care samples were relatively minor (e.g., differences in rate of psychosis, rate of response to treatment). Furthermore, our findings from primary care samples closely resemble the literature regarding RC in tertiary care treated samples. Overall, the generalizability of data from tertiary care centers, where most of the research is conducted, to primary care settings, where most of the patients are treated, thus seems to be good.
Acknowledgments
This study was supported by Canadian Institutes of Health Research Grant No. 64410 and by an unrestricted grant from Neuroscience Research Foundation, Eli Lilly & Co.
Footnotes
Parts of this paper were presented at the XIII World Congress of Psychiatry, Cairo, Egypt, 2005, and at the 3rd International Society for Affective Disorders Meeting, Lisbon, Portugal, 2006.
The authors of this paper do not have any commercial associations that might pose a conflict of interest in connection with this manuscript.
References
- 1.Dunner DL, Patrick V, Fieve RR. Rapid cycling manic depressive patients. Compr Psychiatry. 1977;18:561–566. doi: 10.1016/s0010-440x(97)90006-7. [DOI] [PubMed] [Google Scholar]
- 2.Kirov G, Murphy KC, Arranz MJ, et al. Low activity allele of catechol-O-methyltransferase gene associated with rapid cycling bipolar disorder. Mol Psychiatry. 1998;3:342–345. doi: 10.1038/sj.mp.4000385. [DOI] [PubMed] [Google Scholar]
- 3.Serretti A, Mandelli L, Lattuada E, Smeraldi E. Rapid cycling mood disorder: clinical and demographic features. Compr Psychiatry. 2002;43:336–343. doi: 10.1053/comp.2002.34630. [DOI] [PubMed] [Google Scholar]
- 4.Dunner DL, Fieve RR. Clinical factors in lithium carbonate prophylaxis failure. Arch Gen Psychiatry. 1974;30:229–233. doi: 10.1001/archpsyc.1974.01760080077013. [DOI] [PubMed] [Google Scholar]
- 5.Kupka RW, Luckenbaugh DA, Post RM, et al. Comparison of rapid-cycling and non-rapid-cycling bipolar disorder based on prospective mood ratings in 539 outpatients. Am J Psychiatry. 2005;162:1273–1280. doi: 10.1176/appi.ajp.162.7.1273. [DOI] [PubMed] [Google Scholar]
- 6.Kupka RW, Luckenbaugh DA, Post RM, Leverich GS, Nolen WA. Rapid and non-rapid cycling bipolar disorder: a meta-analysis of clinical studies. J Clin Psychiatry. 2003;64:1483–1494. doi: 10.4088/jcp.v64n1213. [DOI] [PubMed] [Google Scholar]
- 7.Hajek T, Slaney C, Garnham J, Ruzickova M, Passmore M, Alda M. Clinical correlates of current level of functioning in primary care-treated bipolar patients. Bipolar Disord. 2005;7:286–291. doi: 10.1111/j.1399-5618.2005.00182.x. [DOI] [PubMed] [Google Scholar]
- 8.Calabrese JR, Shelton MD, Rapport DJ, et al. A 20-month, double-blind, maintenance trial of lithium versus divalproex in rapid-cycling bipolar disorder. Am J Psychiatry. 2005;162:2152–2161. doi: 10.1176/appi.ajp.162.11.2152. [DOI] [PubMed] [Google Scholar]
- 9.Schwenk TL, Coyne JC, Fechner-Bates S. Differences between detected and undetected patients in primary care and depressed psychiatric patients. Gen Hosp Psychiatry. 1996;18:407–415. doi: 10.1016/s0163-8343(96)00062-x. [DOI] [PubMed] [Google Scholar]
- 10.Williamson PS, Yates WR. The initial presentation of depression in family practice and psychiatric outpatients. Gen Hosp Psychiatry. 1989;11:188–193. doi: 10.1016/0163-8343(89)90040-6. [DOI] [PubMed] [Google Scholar]
- 11.Gaynes BN, Rush AJ, Trivedi M, et al. A direct comparison of presenting characteristics of depressed outpatients from primary vs. specialty care settings: preliminary findings from the STAR*D clinical trial. Gen Hosp Psychiatry. 2005;27:87–96. doi: 10.1016/j.genhosppsych.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 12.Coyne JC, Thompson R, Pepper CM. The role of life events in depression in primary medical care versus psychiatric settings. J Affect Disord. 2004;82:353–361. doi: 10.1016/j.jad.2004.02.008. [DOI] [PubMed] [Google Scholar]
- 13.Oudega R, Moons KG, Hoes AW. Limited value of patient history and physical examination in diagnosing deep vein thrombosis in primary care. Fam Pract. 2005;22:86–91. doi: 10.1093/fampra/cmh718. [DOI] [PubMed] [Google Scholar]
- 14.ten Have M, Vollebergh W, Bijl R, Nolen WA. Bipolar disorder in the general population in The Netherlands (prevalence, consequences and care utilisation): results from The Netherlands Mental Health Survey and Incidence Study (NEMESIS) J Affect Disord. 2002;68:203–213. doi: 10.1016/s0165-0327(00)00310-4. [DOI] [PubMed] [Google Scholar]
- 15.Endicott J, Spitzer RL. A diagnostic interview: the schedule for affective disorders and schizophrenia. Arch Gen Psychiatry. 1978;35:837–844. doi: 10.1001/archpsyc.1978.01770310043002. [DOI] [PubMed] [Google Scholar]
- 16.Spitzer RL, Endicott J, Robins E. Research diagnostic criteria: rationale and reliability. Arch Gen Psychiatry. 1978;35:773–782. doi: 10.1001/archpsyc.1978.01770300115013. [DOI] [PubMed] [Google Scholar]
- 17.Grof P, Duffy A, Cavazzoni P, et al. Is response to prophylactic lithium a familial trait? J Clin Psychiatry. 2002;63:942–947. doi: 10.4088/jcp.v63n1013. [DOI] [PubMed] [Google Scholar]
- 18.Maj M, Pirozzi R, Formicola AM, Tortorella A. Reliability and validity of four alternative definitions of rapid-cycling bipolar disorder. Am J Psychiatry. 1999;156:1421–1424. doi: 10.1176/ajp.156.9.1421. [DOI] [PubMed] [Google Scholar]
- 19.Wehr TA, Goodwin FK. Rapid cycling in manic-depressives induced by tricyclic antidepressants. Arch Gen Psychiatry. 1979;36:555–559. doi: 10.1001/archpsyc.1979.01780050065007. [DOI] [PubMed] [Google Scholar]
- 20.Manji HK, Zarate CA. Molecular and cellular mechanisms underlying mood stabilization in bipolar disorder: implications for the development of improved therapeutics. Mol Psychiatry. 2002;7 (Suppl 1):S1–S7. doi: 10.1038/sj.mp.4001068. [DOI] [PubMed] [Google Scholar]
- 21.Tondo L, Baldessarini RJ. Rapid cycling in women and men with bipolar manic-depressive disorders. Am J Psychiatry. 1998;155:1434–1436. doi: 10.1176/ajp.155.10.1434. [DOI] [PubMed] [Google Scholar]
- 22.Bauer MS, Calabrese J, Dunner DL, et al. Multisite data reanalysis of the validity of rapid cycling as a course modifier for bipolar disorder in DSM-IV. Am J Psychiatry. 1994;151:506–515. doi: 10.1176/ajp.151.4.506. [DOI] [PubMed] [Google Scholar]
- 23.Perugi G, Micheli C, Akiskal HS, et al. Polarity of the first episode, clinical characteristics, and course of manic depressive illness: a systematic retrospective investigation of 320 bipolar I patients. Compr Psychiatry. 2000;41:13–18. doi: 10.1016/s0010-440x(00)90125-1. [DOI] [PubMed] [Google Scholar]
- 24.Alda M. The phenotypic spectra of bipolar disorder. Eur Neuropsychopharmacol. 2004;14 (Suppl 2):S94–S99. doi: 10.1016/j.euroneuro.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 25.Coryell W, Solomon D, Turvey C, et al. The long-term course of rapid-cycling bipolar disorder. Arch Gen Psychiatry. 2003;60:914–920. doi: 10.1001/archpsyc.60.9.914. [DOI] [PubMed] [Google Scholar]
- 26.Schneck CD, Miklowitz DJ, Calabrese JR, et al. Phenomenology of rapid-cycling bipolar disorder: data from the first 500 participants in the Systematic Treatment Enhancement Program. Am J Psychiatry. 2004;161:1902–1908. doi: 10.1176/ajp.161.10.1902. [DOI] [PubMed] [Google Scholar]
- 27.Baldessarini RJ, Tondo L, Floris G, Hennen J. Effects of rapid cycling on response to lithium maintenance treatment in 360 bipolar I and II disorder patients. J Affect Disord. 2000;61:13–22. doi: 10.1016/s0165-0327(99)00196-2. [DOI] [PubMed] [Google Scholar]
- 28.Cowdry RW, Wehr TA, Zis AP, Goodwin FK. Thyroid abnormalities associated with rapid-cycling bipolar illness. Arch Gen Psychiatry. 1983;40:414–420. doi: 10.1001/archpsyc.1983.01790040068010. [DOI] [PubMed] [Google Scholar]
- 29.Schneider U, Malmadier A, Dengler R, Sollmann WP, Emrich HM. Mood cycles associated with normal pressure hydrocephalus. Am J Psychiatry. 1996;153:1366–1367. doi: 10.1176/ajp.153.10.1366. [DOI] [PubMed] [Google Scholar]
- 30.Birmaher B, Axelson D, Strober M, et al. Clinical course of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry. 2006;63:175–183. doi: 10.1001/archpsyc.63.2.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Blumberg HP, Martin A, Kaufman J, et al. Frontostriatal abnormalities in adolescents with bipolar disorder: preliminary observations from functional MRI. Am J Psychiatry. 2003;160:1345–1347. doi: 10.1176/appi.ajp.160.7.1345. [DOI] [PubMed] [Google Scholar]
- 32.Gould TD, Zarate CA, Manji HK. Glycogen synthase kinase-3: a target for novel bipolar disorder treatments. J Clin Psychiatry. 2004;65:10–21. [PubMed] [Google Scholar]
- 33.Krabbe KS, Nielsen AR, Krogh-Madsen R, et al. Brain-derived neurotrophic factor (BDNF) and type 2 diabetes. Diabetologia. 2007;50:431–438. doi: 10.1007/s00125-006-0537-4. [DOI] [PubMed] [Google Scholar]
- 34.Bauer MS, Whybrow PC, Winokur A. Rapid cycling bipolar affective disorder. I. Association with grade I hypothyroidism. Arch Gen Psychiatry. 1990;47:427–432. doi: 10.1001/archpsyc.1990.01810170027005. [DOI] [PubMed] [Google Scholar]
- 35.Bartalena L, Pellegrini L, Meschi M, et al. Evaluation of thyroid function in patients with rapid-cycling and non-rapid-cycling bipolar disorder. Psychiatry Res. 1990;34:13–17. doi: 10.1016/0165-1781(90)90054-9. [DOI] [PubMed] [Google Scholar]
- 36.Coryell W, Endicott J, Keller M. Rapidly cycling affective disorder. Demographics, diagnosis, family history, and course. Arch Gen Psychiatry. 1992;49:126–131. doi: 10.1001/archpsyc.1992.01820020046006. [DOI] [PubMed] [Google Scholar]
- 37.Kupka RW, Nolen WA, Post RM, et al. High rate of autoimmune thyroiditis in bipolar disorder: lack of association with lithium exposure. Biol Psychiatry. 2002;51:305–311. doi: 10.1016/s0006-3223(01)01217-3. [DOI] [PubMed] [Google Scholar]
- 38.Maj M, Magliano L, Pirozzi R, Marasco C, Guarneri M. Validity of rapid cycling as a course specifier for bipolar disorder. Am J Psychiatry. 1994;151:1015–1019. doi: 10.1176/ajp.151.7.1015. [DOI] [PubMed] [Google Scholar]
- 39.Post RM, Kramlinger KG, Joffe RT, et al. Rapid cycling bipolar affective disorder: lack of relation to hypothyroidism. Psychiatry Res. 1997;72:1–7. doi: 10.1016/s0165-1781(97)00076-0. [DOI] [PubMed] [Google Scholar]
- 40.Wehr TA, Sack DA, Rosenthal NE, Cowdry RW. Rapid cycling affective disorder: contributing factors and treatment responses in 51 patients. Am J Psychiatry. 1988;145:179–184. doi: 10.1176/ajp.145.2.179. [DOI] [PubMed] [Google Scholar]
- 41.Maj M, Pirozzi R, Magliano L, Bartoli L. Long-term outcome of lithium prophylaxis in bipolar disorder: a 5-year prospective study of 402 patients at a lithium clinic. Am J Psychiatry. 1998;155:30–35. doi: 10.1176/ajp.155.1.30. [DOI] [PubMed] [Google Scholar]


