Abstract
Background/Objectives
Chronic kidney disease (CKD) is diagnosed by serum creatinine, which is biased by muscle mass, age and race. We evaluated whether cystatin C, an alternative measure of kidney function, can detect high risk CKD among elderly Mexican-Americans.
Design
Longitudinal
Setting
Sacramento Area Study of Latinos (SALSA)
Participants
1,435 Mexican-Americans ages 60–101 with mean follow-up 6.8 years
Measurements
We estimated glomerular filtration rate (eGFR, ml/min/1.73m2)by creatinine and cystatin C, and classified persons into four mutually exclusive categories: (1) CKD neither (eGFRcreat ≥60 and eGFRcys ≥60); (2) CKD creatinine only (eGFRcreat <60 but eGFRcys ≥60); (3) CKD cystatin only (eGFRcreat ≥60 but eGFRcys <60); and (4) CKD both (eGFRcreat <60 and eGFRcys <60). We studied the association of each CKD classification with all-cause death and cardiovascular (CVD) death using Cox regression.
Results
At baseline, mean was age 71±7; 34% (N=481) were diabetic and 68% (N=980) hypertensive. Compared with persons with no CKD by either marker, persons with CKD both had the highest risks for death (HR 2.30, 1.78–2.98) and CVD death (HR 2.75, 1.96–3.86) after full adjustment. Persons with CKD by cystatin C only were also at increased risk for death, HR 1.91 (1.37–2.67) and for CVD death, HR 2.56 (1.64–3.99)) compared to no CKD. In contrast, persons with CKD by creatinine only were not at increased risk for CVD death (HR 1.39, 0.71–2.72), but remained at higher risk for all-cause death (HR 1.95, 1.27–2.98).
Conclusions
Cystatin C may be a useful alternative in addition to creatinine to detect high risk CKD in elderly Mexican Americans.
Keywords: chronic kidney disease, Mexican-Americans, elderly, creatinine, cystatin C, cardiovascular disease
INTRODUCTION
Chronic kidney disease (CKD), defined as an estimated glomerular filtration rate (eGFR) <60 ml/min/1.73m2, affects over 8% of the U.S. population, and its prevalence sharply increases with age.1 The presence of CKD is associated with higher risk for death, heart failure, cardiovascular events, and progression to end stage renal disease (ESRD).2, 3 In the elderly, CKD is also associated with increased frailty4 and unsuccessful aging.5 Hispanics have been shown to have higher rates of ESRD,6 with paradoxical reports of lower CKD prevalence.1, 7 Hispanics have also been shown to have faster rates of progression from CKD to ESRD compared with Whites.8 Since Hispanics are the largest growing segment of the U.S. population, CKD in elderly Hispanics is a growing public health concern. An accurate diagnosis of CKD is imperative for risk assessment and appropriate treatment in this high risk group.
However, CKD misclassification remains an important barrier in clinical care. Current practice standards rely on serum creatinine to assess kidney function. 9 Since the eGFR estimated from creatinine is now automatically reported by most laboratories, many providers rely on this measure to detect CKD. However, serum creatinine is highly affected by muscle mass, and the existing equations to estimate GFR from creatinine have not been adequately validated in the elderly or in Hispanics.10 An alternative measure of kidney function, cystatin C, has been approved for clinical use by the FDA. Cystatin C is less affected by muscle mass, it is not biased by race, and it has stronger and more linear associations with adverse events compared with creatinine.3 Recently, our group showed that adding cystatin C measurements to creatinine improves detection and risk stratification of CKD.11, 12 Whether measuring cystatin C can improve detection and risk stratification of CKD in elderly Mexican-Americans has not been studied.
Therefore, we designed this study to examine the prevalence of CKD by creatinine and/or cystatin C in a cohort of elderly Mexican-Americans participating in the Sacramento Area Study of Latinos (SALSA). We then studied the association of each CKD classification with all cause death, cardiovascular death and incident cardiovascular disease.
METHODS
Study population
We included participants from the Sacramento Area Study of Latinos (SALSA). SALSA is an NIH-sponsored longitudinal cohort study of 1,789 community-dwelling Mexican-Americans residing in California’s Sacramento Valley who were aged 60–101 years at recruitment (1998–1999). Details on the study population, recruitment and follow up have been previously published.13 Briefly, participants were followed every 12–15 months with home visits that included clinical, cognitive, and functional assessments up to 2008. Mortality surveillance continues to be accrued. In addition to the follow-up visit, a semi-annual phone call updated information on medications, health events, and socio-demographic risk factors. For these analyses, participants were eligible if they had both cystatin C and creatinine measured at baseline (N=1,435). SALSA has been approved by the Institutional Review Boards (IRB) at the University of Michigan, and the University of California at San Francisco and Davis.
Kidney Function Measures
Kidney function was assessed by serum creatinine and serum cystatin C. Serum creatinine was analyzed by using a standard spectrophotometric assay. Cystatin C was measured from previously frozen samples stored at −70° C at the University of Michigan, using a particle enhanced immnoassay by Gentian (Gentian) at the University of California, Los Angeles.14 We estimated the GFR with the use of the CKD-EPI creatinine equation and the CKD-EPI cystatin C equation without demographic coefficients: eGFRcys=76.7 × cys C −1.19. These formulae were developed from the pooling of several cohorts with GFR measured from iothalamate clearance. We defined CKD as an eGFR <60 ml/min/1.73m2.15
Ascertainment of Outcomes
Mortality has been ascertained through May, 2010, using online obituary surveillance, review of the Social Security death index and the National Death Index, review of vital statistics data files from California, and interviews with family members.13 Among persons known to be deceased, cause of death was abstracted from death certificates for 84% of participants (n = 375). For these analyses, cardiovascular death was defined as a death for which anywhere on the death certificate mentioned any of the following codes from the Tenth Revision of the International Statistical Classification of Diseases and Related Health Problems: codes I20–125, heart failure code 150 and stroke codes I63 or 164. If a death certificate was not located, the death was classified as all-cause mortality, with the cause unspecified. Persons were censored at date of last contact.
In a secondary analysis, we ascertained incident cardiovascular disease. For these analyses, we excluded 351 persons with prevalent CVD. Incident CVD was defined as a fatal or non-fatal CV event. Non-fatal CVD events were ascertained by asking participants whether they were told by a physician that they had any of the following events: myocardial infarction, angina, catheterization or coronary artery bypass grafting, stroke, heart failure, or atrial fibrillation. This approach has been validated in SALSA by chart review of a subsample of events.
Covariates
Information on age, gender, income, education, and smoking were ascertained by questionnaire at the baseline visit. Height and weight were measured with participants wearing light clothing and no shoes. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Fasting blood was collected and stored until needed for the appropriate assays, including HDL cholesterol, glucose, and C-reactive protein. Low-density lipoprotein (LDL) cholesterol was calculated using the Friedewald equation. Hypertension was defined as the use of antihypertensive medications, a self report of hypertension, or a sitting blood pressure of >140/90 mmHg at baseline visit. Diabetes was defined as a participant report of physician-diagnosed diabetes, the use of insulin or oral hypoglycemic agents or a baseline fasting glucose ≥ 126 mg/dL. Hypertension and diabetes medication use was assessed by medicine cabinet inventory at each annual visit where prescription medications were collected at all home visits using a manual review by the technicians.16 These were updated at the semi-annual phone call. Prevalent cardiovascular disease was defined as having a self reported history of coronary heart disease, heart failure, stroke or atrial fibrillation.
Statistical Analysis
We first categorized individuals into four mutually exclusive groups defined by presence or absence of CKD based on cystatin C and creatinine: 1) those with eGFRcreat ≥60ml/min/1.73m2 and eGFRcys ≥60 ml/min/1.73m2, herein described as CKD Neither; 2) those with eGFRcreat <60ml/min/1.73m2, but eGFRcys ≥60 ml/min/1.73m2, herein described as CKD creatinine only; 3) those with eGFRcreat ≥60ml/min/1.73m2 but eGFRcys <60 ml/min/1.73m2, herein described as CKD cystatin only; and 4) those with eGFRcreat <60 ml/min/1.73m2, and eGFRcys <60 ml/min/1.73m2 herein described as CKD both. We first described baseline characteristics by CKD group and compared these using ANOVA or Chi-square tests as appropriate.
For each of the above four groups, we estimated all-cause and cardiovascular mortality rates, and incident CVD rates, and present these as rates per 1,000 person years. Then, using Cox proportional hazard models, we evaluated the association of the CKD classification with the risks for death, CVD death, and incident CVD with study time as the time scale. We used a global test of proportional hazards assumption and this was not violated. We adjusted for the above-mentioned covariates chosen a priori from the literature as potential confounders of the association of eGFR <60 ml/min/1.73m2 with adverse outcomes. Finally, in a sensitivity analysis, we included both eGFRcreat and eGFRcys as continuous variables in a fully adjusted model to ascertain the association of each estimate of GFR with CVD death. Analyses were conducted in SAS v9.2 (SAS Institute Inc., Cary, NC).
RESULTS
Cohort Characteristics
Among 1,435 SALSA participants, the mean age was 71 (SD 7) years. Approximately 34% (N=481) had diabetes and 68% (N=980) had hypertension. Prevalent cardiovascular disease was present in 24% (N=351) of the SALSA participants. Characteristics of the 354 excluded participants were not significantly different from the remaining cohort (mean age 71 ± 7 years, 30 % diabetics, and 58% hypertensives).
Overall, 21% (N=300) of SALSA participants had CKD by either creatinine and/or cystatin C. Among persons with CKD by either marker, 52% had CKD by both markers, whereas 16% had CKD by creatinine only, and 32% had CKD by cystatin C only. Elderly Mexican Americans with CKD by both markers were older, they had higher prevalence of diabetes and hypertension, and they had the lowest eGFR by both creatinine and cystatin C (Table 1). During an average follow-up period of 6.8 years, there were 430 deaths, 227 of which were CVD deaths.
Table 1.
Baseline Demographics and Prevalence of Each Group
| CKD Neither | CKD Creatinine Only | CKD Cystatin C Only | CKD Both | P Value | |
|---|---|---|---|---|---|
| N | 1,135 | 49 | 95 | 156 | |
| Age | 69.4 (6.3) | 74.0 (7.9) | 74.5 (7.9) | 75.5 (8.3) | <0.001 |
| Female (%) | 689 (61) | 24 (49) | 47 (49) | 105 (67) | 0.01 |
| Education | 7.6 (5.4) | 8.3 (4.9) | 6.7 (5.2) | 6.4 (5.2) | 0.02 |
| Income (%) | |||||
| <$1,000 | 472 (42) | 18 (37) | 44 (48) | 83 (53) | 0.07 |
| $1,000–$1,499 | 207 (19) | 8 (16) | 20 (22) | 32 (21) | |
| $1,500–$1,999 | 135 (12) | 6 (12) | 9 (10) | 16 (10) | |
| $2,000–$2,499 | 113 (10) | 10 (20) | 9 (10) | 12 (8) | |
| ≥$2,500 | 186 (17) | 7 (14) | 10 (11) | 13 (8) | |
| Diabetes (%) | 358 (32) | 14 (29) | 31 (33) | 78 (50) | <0.001 |
| Fasting Glucose | 116.5 (47.8) | 115.9 (50.5) | 105.1 (33.0) | 114.1 (46.4) | 0.15 |
| Hypertension (%) | 720 (63) | 41 (84) | 74 (78) | 145 (93) | <0.001 |
| Systolic Blood Pressure | 137.8 (18.6) | 143.2 (22.7) | 141.2 (19.3) | 144.3 (21.8) | 0.0005 |
| Diastolic Blood Pressure | 76.2 (10.0) | 75.8 (11.1) | 75.3 (12.2) | 73.9 (11.5) | 0.09 |
| HTN Medication (%) | 457 (40) | 33 (67) | 53 (56) | 123 (79) | <0.001 |
| Smoking (%) | |||||
| Never Smoked | 537 (47) | 24 (49) | 39 (41) | 71 (46) | 0.59 |
| Former Smoker | 477 (42) | 21 (43) | 40 (42) | 69 (44) | |
| Current Smoker | 119 (11) | 4 (8) | 16 (17) | 16 (10) | |
| Prevalent CVD (%) | 225 (20) | 15 (31) | 37 (39) | 74 (47) | <0.001 |
| Total Cholesterol | 213.4 (38.7) | 216.9 (35.1) | 202.9 (38.2) | 210.1 (43.7) | 0.06 |
| LDL | 123.5 (34.4) | 125.5 (32.0) | 120.4 (30.7) | 116.3 (35.4) | 0.08 |
| HDL | 52.6 (13.9) | 54.7 (13.2) | 47.6 (11.3) | 49.7 (12.1) | 0.0003 |
| Body Mass Index | 29.6 (5.7) | 29.1 (5.0) | 30.3 (6.0) | 30.6 (7.8) | 0.15 |
| eGFRcys | 85.6 (17.1) | 67.7 (7.0) | 52.1 (5.6) | 40.1 (13.2) | <0.001 |
| eGFRcr | 85.8 (10.8) | 54.0 (5.9) | 74.9 (9.0) | 42.0 (14.7) | <0.001 |
| C-Reactive Protein | 5.6 (12.8) | 3.3 (4.0) | 9.8 (14.8) | 9.7 (17.6) | <0.001 |
Note: N (%) or Mean (SD).
Abbreviations: Chronic Kidney Disease (CKD); Hypertension (HTN); Cardiovascular Disease (CVD); Low Density Lipoprotein (LDL); High Density Lipoprotein (HDL); Cystatin C-based Estimated Glomerular Filtration Rate (eGFRcys); Creatinine-based Estimated Glomerular Filtration Rate (eGFRcr); Interleukin-6 (IL-6).
Association of CKD Definition with Outcomes
Participants with CKD by both cystatin C and creatinine had the highest rates of death and cardiovascular death and incident CVD. Persons with CKD detected by cystatin C only, (i.e those in whom CKD would otherwise be missed by creatinine), had the second highest risk for all outcomes. Interestingly, persons with CKD by creatinine only had comparable rates of CVD death and incident CVD to persons with no CKD by either marker, but they were still at increased risk for all cause death (Figure 1).
Figure 1.
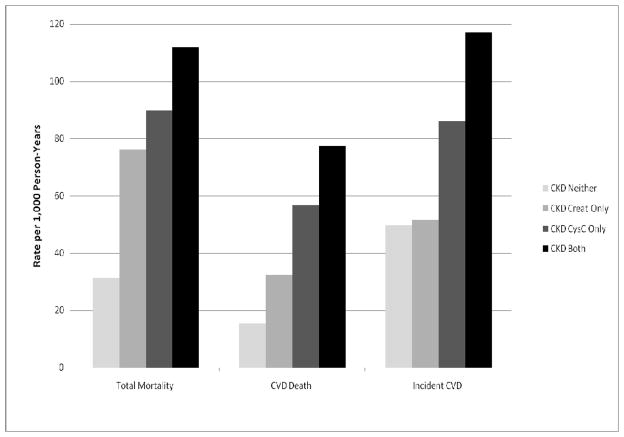
Rate per 1,000 Person-Years for Each Outcome
In multivariable models, the risk of all-cause death was almost 2-fold for participants who had CKD by creatinine only or cystatin C only compared to participants with CKD neither. Persons with CKD by both markers had the highest risk of death compared to persons with CKD by neither after full adjustment (Table 2).
Table 2.
The Association of All-Cause Mortality and Cardiovascular Death by CKD Group in SALSA
| N | N Events | Hazard Ratio (95% Confidence Interval)
|
|||
|---|---|---|---|---|---|
| Unadjusted Model | Demographic- Adjusted Modela | Multivariate- Adjusted Modelb | |||
| All-Cause Mortality | |||||
| CKD Neither | 1,135 | 252 | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| CKD Creatinine Only | 49 | 25 | 2.71 (1.79–4.09) | 2.08 (1.36–3.16) | 1.95 (1.27–2.98) |
| CKD Cystatin C Only | 95 | 52 | 2.48 (1.83–3.35) | 1.91 (1.39–2.61) | 1.91 (1.37–2.67) |
| CKD Both | 156 | 101 | 3.70 (2.93–4.67) | 2.68 (2.10–3.41) | 2.30 (1.78–2.98) |
| Cardiovascular Death | |||||
| CKD Neither | 1,135 | 120 | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| CKD Creatinine Only | 49 | 10 | 2.25 (1.18–4.28) | 1.69 (0.88–3.25) | 1.39 (0.71–2.72) |
| CKD Cystatin C Only | 95 | 31 | 3.79 (2.55–5.64) | 2.66 (1.76–4.01) | 2.56 (1.64–3.99) |
| CKD Both | 156 | 66 | 5.24 (3.86–7.12) | 3.50 (2.53–4.85) | 2.75 (1.96–3.86) |
Demographic Model adjusted for: age, gender, income, and education.
Multivariate-Adjusted Model further adjusted for: LDL, HDL, hypertension, diabetes mellitus, smoking, body mass index, prevalent cardiovascular disease, and CRP.
Findings were somewhat different for the outcome CVD death. Participants with CKD by creatinine only had risks of CVD death similar to those with no CKD by either marker. However, the risk of CVD death was highest for those with CKD by cystatin C only and those with CKD both (Table 2).
Similarly, in secondary analyses, persons with CKD by creatinine only were not at increased risk for incident CVD compared with persons with CKD neither, HR 1.03 (0.55–1.93) in unadjusted models. Persons with CKD by cystatin C only and CKD both were at higher risk for incident CVD, HR 1.76 (1.17–2.66) and 2.47 (1.80–3.39), respectively. Though estimates were attenuated after full adjustment, the HR for persons with CKD by cys C only remained similar to that of persons with CKD by both markers, HR 1.24 (0.80–1.93) and HR 1.46 (1.03–2.08), respectively.
In a sensitivity analysis including both eGFRcys and eGFRcreat in a fully adjusted model, only eGFR by cystatin C was independently associated with CVD death. Each 10 ml/min/1.73m2 increase in eGFRcys was associated with a HR 0.78 (0.69 to 0.87, p <0.001) for CVD death. The HR for eGFRcreat was 1.02, 95%CI 0.91 to 1.13).
DISCUSSION
In this cohort of elderly Mexican-Americans, we found that persons who have CKD detected by cystatin C but are otherwise missed by creatinine are at increased risk for death, CVD death, and incident CVD. Moreover, we showed that persons with CKD confirmed by both markers were at highest risk for adverse events. In contrast, persons with CKD by creatinine only but not confirmed by cystatin C were at increased risk for all cause death, but had risks for CVD death and incident CVD comparable to persons with no CKD by either marker. These findings suggest that cystatin C may be a useful additional marker of kidney function in this population.
Our findings extend prior reports of the importance of CKD misclassification in the elderly.17, 18 We also expand on prior studies from our group which have shown that cystatin C can improve detection and risk stratification in Black and White adults by identifying persons at high risk who would have otherwise been missed by creatinine.11, 12 Our finding that cystatin C alone detected over 30% of the CKD in elderly Mexican-Americans, and that these persons comprised the second highest risk group in the cohort is of importance. For example, these may be elderly with unpredictable muscle mass who may still need adjustment for drug dosing, assessment of risk for contrast, and other adverse outcomes associated with CKD. Future studies are needed to understand the cost-utility of measuring cystatin C among elderly persons in clinical practice.
In addition, our findings may also shed light on the paradoxical reports of lower prevalence of eGFR <60 ml/min/1.73m2 among Mexican Americans7 but higher incidence of ESRD compared with whites. The high prevalence of CKD detected by cystatin C only suggests that CKD misclassification may explain some of these observations. This is also supported by prior reports of similar prevalence of CKD in Hispanics compared with whites when using cystatin C.19 Given the very high comorbidity burden among elderly Mexican Americans, cystatin C may be an important tool in improving future studies aimed to understand CKD complications in this high risk group.
On the other hand, 16% of persons in SALSA had CKD by creatinine only. Although these persons were still at increased risk for all-cause death, they had risks for CVD death and incident CVD comparable to persons with no CKD. In the Cardiovascular Health Study, we also previously reported that elderly persons with CKD by creatinine only had similar risk of death and CVD compared with persons with no CKD.12 Taken together, our findings support the notion that, among the elderly, some persons classified as CKD by creatinine only may not be at increased cardiovascular risk. Future studies are necessary to identify persons in which a multiple panel of creatinine and cystatin C may be cost-efficient to accurately risk stratify persons with CKD.
Our study is the first to investigate the use of cystatin C in a large cohort of elderly Mexican Americans. We must note several limitations. First, we do not have gold standard measured GFR. Therefore, whether each filtration marker may be associated with factors other than kidney function which may explain some of the observed associations cannot be ascertained. While creatinine is biased by muscle mass, age, sex and race,10 cystatin C has been associated with inflammation and obesity.20 However, direct GFR measurement is impractical in large epidemiological studies. Moreover, our findings remained robust after adjustment for BMI, lipids and CRP. We are also limited by the lack of measured albumin in the urine. Albuminuria has been shown to be an independent predictor of adverse events.21 In addition, our outcome of incident CVD was self-reported, though SALSA has previously validated this approach.
In summary, we found that cystatin C, an alternative marker of kidney function, could identify elderly Mexican Americans at increased risk for death and CVD that are not detected by creatinine based measures. These persons with CKD detected by cystatin C only were at high risk for death and CVD. In addition, persons who had CKD by creatinine and confirmed by cystatin C had the highest risk for death and CVD. Future studies are needed to understand the most cost-efficient way to implement the use of cystatin C in clinical practice.
Acknowledgments
The authors thank the other investigators, the staff, and the participants of the SALSA study for their valuable contributions. CP had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The authors would like to acknowledge Dr. Allison Aiello, PhD, and her laboratory at the University of Michigan for handling and measurement of cystatin C samples for this study.
Sponsor’s Role:
CP is funded by the National Institutes of Diabetes and Digestive and Kidney Diseases 1K23SK082793 and a Robert Wood Johnson Harold Amos award. SALSA and Dr. Haan are funded by National Institute of Aging R01012975 and National Institutes of Diabetes and Digestive and Kidney Diseases R01DK60753. These funding sources had no involvement in the design or execution of this study.
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Author Contributions
CP: study concept and design, analysis and interpretation of data, drafting of the manuscript, manuscript revision; MNH: study concept and design, analysis and interpretation of data, drafting of the manuscript, manuscript revision, cohort development, measurement of data; AL: analysis and interpretation of data, drafting of the manuscript, manuscript revision; MO: analysis and interpretation of data, manuscript revision; LL: analysis and interpretation of data, manuscript revision; JN: analysis and interpretation of data, manuscript revision; AZH: analysis and interpretation of data, manuscript revision;
References
- 1.Coresh J, Selvin E, Stevens LA, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298:2038–2047. doi: 10.1001/jama.298.17.2038. [DOI] [PubMed] [Google Scholar]
- 2.Go AS, Chertow GM, Fan D, et al. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–1305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 3.Shlipak MG, Sarnak MJ, Katz R, et al. Cystatin C and the risk of death and cardiovascular events among elderly persons. N Engl J Med. 2005;352:2049–2060. doi: 10.1056/NEJMoa043161. [DOI] [PubMed] [Google Scholar]
- 4.Odden MC, Chertow GM, Fried LF, et al. Cystatin C and measures of physical function in elderly adults: The Health, Aging, and Body Composition (HABC) Study. Am J Epidemiol. 2006;164:1180–1189. doi: 10.1093/aje/kwj333. [DOI] [PubMed] [Google Scholar]
- 5.Sarnak MJ, Katz R, Fried LF, et al. Cystatin C and aging success. Arch Intern Med. 2008;168:147–153. doi: 10.1001/archinternmed.2007.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.United States Renal Data System. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2009. [Google Scholar]
- 7.Coresh J, Astor BC, Greene T, et al. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination Survey. Am J Kidney Dis. 2003;41:1–12. doi: 10.1053/ajkd.2003.50007. [DOI] [PubMed] [Google Scholar]
- 8.Peralta CA, Katz R, Deboer I, et al. Racial and ethnic differences in kidney function decline among persons without chronic kidney disease. J Am Soc Nephrol. 2011;22:1327–1334. doi: 10.1681/ASN.2010090960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.KDOQI Clinical Practice Guidelines and Clinical Practice Recommendations for Diabetes and Chronic Kidney Disease. Am J Kidney Dis. 2007;49:S12–154. doi: 10.1053/j.ajkd.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 10.Stevens LA, Coresh J, Greene T, et al. Assessing kidney function--measured and estimated glomerular filtration rate. N Engl J Med. 2006;354:2473–2483. doi: 10.1056/NEJMra054415. [DOI] [PubMed] [Google Scholar]
- 11.Peralta CA, Shlipak MG, Judd S, et al. Detection of chronic kidney disease with creatinine, cystatin C, and urine albumin-to-creatinine ratio and association with progression to end-stage renal disease and mortality. JAMA. 2011;305:1545–1552. doi: 10.1001/jama.2011.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peralta CA, Katz R, Sarnak MJ, et al. Cystatin C identifies chronic kidney disease patients at higher risk for complications. J Am Soc Nephrol. 2011;22:147–155. doi: 10.1681/ASN.2010050483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Colon-Lopez V, Haan MN, Aiello AE, et al. The effect of age at migration on cardiovascular mortality among elderly Mexican immigrants. Ann Epidemiol. 2009;19:8–14. doi: 10.1016/j.annepidem.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shlipak MG, Weekley CC, Li Y, et al. Comparison of cardiovascular prognosis by 3 serum cystatin C methods in the Heart and Soul Study. Clin Chem. 2011;57:737–745. doi: 10.1373/clinchem.2010.158915. [DOI] [PubMed] [Google Scholar]
- 15.Stevens LA, Coresh J, Schmid CH, et al. Estimating GFR using serum cystatin C alone and in combination with serum creatinine: A pooled analysis of 3,418 individuals with CKD. Am J Kidney Dis. 2008;51:395–406. doi: 10.1053/j.ajkd.2007.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haan MN, Mungas DM, Gonzalez HM, et al. Prevalence of dementia in older latinos: The influence of type 2 diabetes mellitus, stroke and genetic factors. J Am Geriatr Soc. 2003;51:169–177. doi: 10.1046/j.1532-5415.2003.51054.x. [DOI] [PubMed] [Google Scholar]
- 17.Giannelli SV, Patel KV, Windham BG, et al. Magnitude of underascertainment of impaired kidney function in older adults with normal serum creatinine. J Am Geriatr Soc. 2007;55:816–823. doi: 10.1111/j.1532-5415.2007.01196.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maaravi Y, Burzstyn M, Stessman J. Underdiagnosis of impaired kidney function in older adults with normal serum creatinine. J Am Geriatr Soc. 2008;56:382. doi: 10.1111/j.1532-5415.2007.01525.x. [DOI] [PubMed] [Google Scholar]
- 19.Kramer H, Palmas W, Kestenbaum B, et al. Chronic kidney disease prevalence estimates among racial/ethnic groups: The Multi-Ethnic Study of Atherosclerosis. Clin J Am Soc Nephrol. 2008;3:1391–1397. doi: 10.2215/CJN.04160907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Knight EL, Verhave JC, Spiegelman D, et al. Factors influencing serum cystatin C levels other than renal function and the impact on renal function measurement. Kidney Int. 2004;65:1416–1421. doi: 10.1111/j.1523-1755.2004.00517.x. [DOI] [PubMed] [Google Scholar]
- 21.Matsushita K, van der Velde M, Astor BC, et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: A collaborative meta-analysis. Lancet. 2010;375:2073–2081. doi: 10.1016/S0140-6736(10)60674-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


