Abstract
Aims:
To create a normative data for lea grating (LG) in the Indian population and to compare LG with Cardiff Acuity Card (CAC).
Settings and Design:
Normative Data was acquired from normal children between 6 months-3 years coming to the ‘Immunisation Clinic’ and ‘Well-Baby Clinic’ at a Civil Hospital. To compare LG with CAC, normal and amblyopic children between 6 months-3 years were evaluated,
Materials and Methods:
Monocular and binocular visual acuity (VA) was measured using LG and then CAC. VA and time taken to perform the test were compared.
Statistical Analysis Used:
Pearson's Correlation Coefficient to compare VA and Student paired t-test (significance P<0.005) to compare time.
Results:
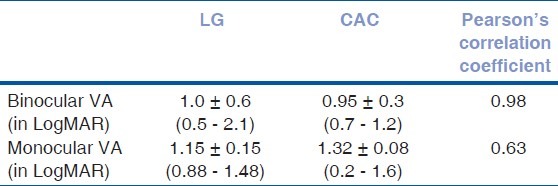
Two standard deviations of VA of 100 normal children overlapped with that published by Lea. Of the 30 amblyopic children aged 18.32 ± 10.5 months (2-36), 18 were females. VA was 0.95 ± 0.3 logMAR (0.7–1.2) and 1.0 ± 0.6 logMAR (0.5–2.1) binocularly and 1.32 ± 0.08 logMAR (0.2-0.6) and 1.15 ± 0.15 logMAR (0.88-1.48) monocularly on CAC and LG respectively. Pearson's correlation coefficient was 0.98 and 0.63 for binocular and monocular assessment respectively. Time taken to perform LG monocularly and binocularly was significantly less (P<0.001) than CAC.
Conclusion:
Normative data acquired in Indian pre-verbal children is similar to that published by Lea. Though VA by CAC is better than LG, the two tests are comparable.
Keywords: Cardiff acuity cards, lea grating, visual acuity in pre-verbal children
Measuring visual acuity (VA) in preverbal children has always been difficult. Forced preferential looking (FPL) tests like grating acuity (GA) test [Teller Acuity Card (TAC)] and vanishing optotype test [Cardiff Acuity Card (CAC)] are well-established for the purpose.[1] A study comparing the two has been done.[2] Lea grating (LG) test is a new grating-based acuity test. It is in the form of 2 paddles, making the test more convenient. Also, it is relatively cost-effective, which is a major concern when it comes to tests like TAC. In this study, we have compared CAC to LG. One would also like to compare TAC to LG. Normative data for LG is available for the western population only. Thus, there is a need for an Indian database for the same.
In this study, we have created a normative data for children aged between 6 months to 3 years using LG. We have also compared various parameters of visual acuity testing in normal and amblyopic children using CAC and LG.
Materials and Methods
This was a prospective, observational study. The procedures followed were in accordance with the ethical standards as stated in the Helsinki Declaration of 1975 and revised in 2000. Our cohort comprised of children aged between 6 months and 3 years. Children coming to an ‘immunization clinic’ and ‘well baby clinic’ at a civil hospital were evaluated by a well-trained pediatric ophthalmologist, to rule out any ocular abnormalities. These children were included in the Normative Data group (N). In addition to these, children with unilateral strabismic or anisometropic amblyopia that were referred for further evaluation to a pediatric ophthalmologist (MK) were included in the Comparison group (C). All these children were undergoing an ophthalmological evaluation for the first time, and none were familiar with either of the tests. Uncooperative children, giving unreliable results (as judged by the examiner) or children with any ocular, neurological or systemic co-morbidity were excluded from the study.
Monocular and binocular VA in all was recorded first using LG and then using CAC by the same examiner. LG were used from a distance of 57 cm. The test was performed first with both eyes open, followed by right eye open and then left eye. The opposite eye of the child was closed either by a micropore tape or by the mother's hand while the child sat the mother's lap. Three presentations of LG paddles were presented, and 2 correct responses were taken as positive. If the child's visual acuity was better than that detected at the required distance, testing distance was not increased. This was done to avoid loss of attention with an increased distance. A break of 5 - 15 minutes was given before checking VA with CAC to maintain the child's alertness during the test. The same procedure was repeated with the CAC, which was performed from a distance of 50 cm.
Data collected from group N with LG was used to form a normative data. This was then compared to that got by Dr. Lea. Data from group N and C was used to compare LG with CAC. Person's Correlation Coefficient was used to compare the VA, and students paired t-test was used to compare the time taken.
Results
2 standard deviations of our normative data overlapped that acquired by Lea [Fig. 1]. We had 400 eyes of 200 normal children in the N group and 60 eyes of 30 children in group C [Table 1].
Figure 1.
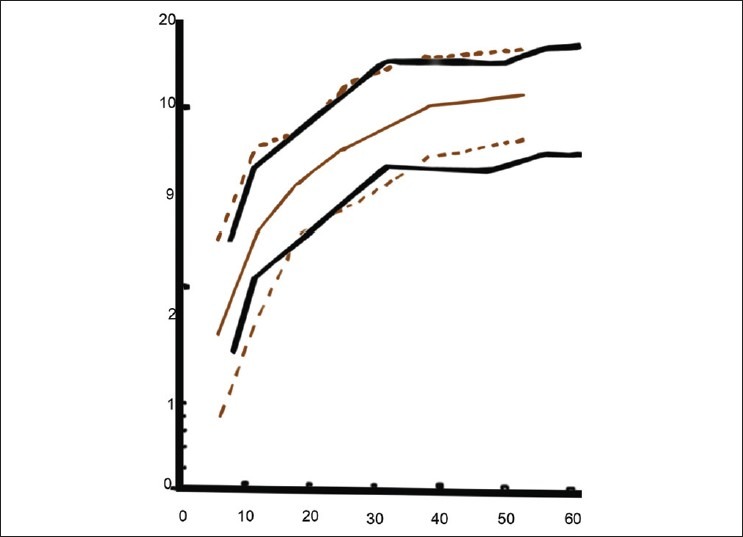
Graph with dark black and bold lines is the normative data of our study. The dotted grey graph is the normative data of Lea's study
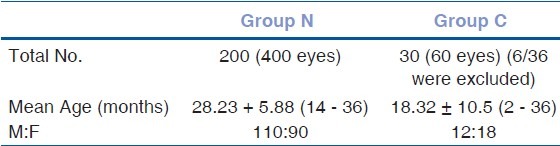
Table 1.
Distribution in group N and C
While comparing LG to CAC using group N and C, we found that VA acquired with CAC was found to be better than LG. In spite of that, there was a strong correlation between the two [Figs. 2 and 3, Table 2]. This difference in visual acuity was significant with P < 0.0001 when we compared binocular visual acuity of LG with CAC using students t-test.
Figure 2.
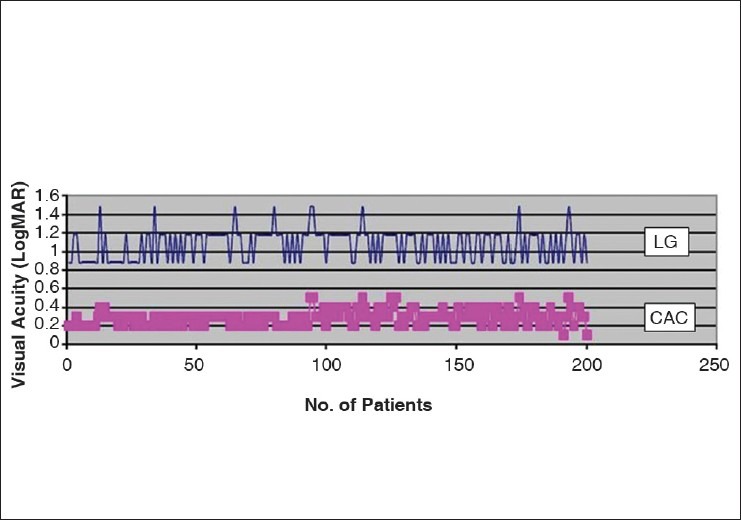
Comparing Binocular visual acuity using lea grating and cardiff acuity card
Figure 3.
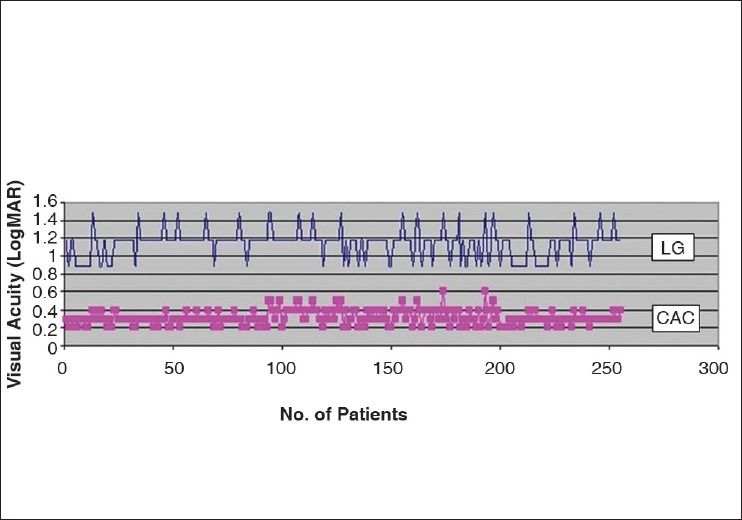
Comparing Monocular visual acuity using lea grating and cardiff acuity card
Table 2.
Comparing visual acuity using lea grating and cardiff acuity card
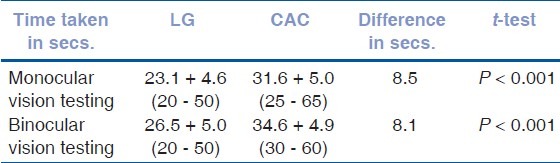
The time taken for testing with LG significantly was less that that with CAC [Table 3].
Table 3.
Comparing time taken using lea grating and cardiff acuity card
Discussion
LG and CAC are comparing different aspects of vision. LG utilize gratings, which at best tells us the resolution acuity and perhaps do not truly represent recognition acuity while CAC test utilizes pictorial optotypes, which are of the same size but made on the principle of the vanishing optotypes beyond the resolution distance.[3] In our study, VA with CAC was significantly different (better) than that with LG, but the two showed a strong correlation. Thus, the 2 tests individually would give reliable results, but cannot be interchanged along different visits.
Our study showed that both the tests were useful in checking VA in preverbal children above 6 months. It has been suggested that CAC being pictorial, may bridge the gap of resolution and recognition acuity and generate more interest among children, especially those more than 1 year old.[3,4]
Both tests were quick. LG was faster by ~8 seconds than CAC. A difference of even 8 - 9 seconds is important while checking vision in children who have a short attention span.
In a country like ours where financial constrains are important concerns, LG (~ Rs 10,000) prove to be more cost-effective option compared to TAC (~ Rs 1,75,000) and CAC (~ Rs 40,000).
Also, paddle-held cards are more convenient to use.
LG is a quicker and more cost-effective test for vision assessment of preverbal children. Nevertheless, further studies with masked observer, larger sample size including more children in amblyopic age group and sub-group analysis are desirable.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Dobson V, Salem D, Mayer DL, Moss C, Sebris SL. Visual acuity screening of children 6 months to 3 years of age. Invest Ophthalmol Vis Sci. 1985;26:1057–63. [PubMed] [Google Scholar]
- 2.Sharma P, Bairagi D, Sachdeva MM, Kaur K, Khokhar S, Saxena R. Comparative evaluation of teller and cardiff acuity tests in normals and unilateral amblyopes in under-two-year-olds. Indian J Ophthalmol. 2003;51:341–5. [PubMed] [Google Scholar]
- 3.Adoh TO, Woodhouse JM. The Cardiff Acuity Test used for measuring visual acuity development in toddlers. Vision Res. 1994;14:1063–6. doi: 10.1016/0042-6989(94)90168-6. [DOI] [PubMed] [Google Scholar]
- 4.Kushner BJ, Lucchese NJ, Morton GV. Grating visual acuity with Teller Cards compared with Snellen visual acuity in literate patients. Arch Ophthalmol. 1995;113:485–93. doi: 10.1001/archopht.1995.01100040107035. [DOI] [PubMed] [Google Scholar]


