Abstract
The purpose of this report is to evaluate the efficacy and safety of combined intravitreal injection of bevacizumab and intravitreal triamcinolone acetonide (IVTA) for recurrent inflammatory choroidal neovascular membrane (CNVM). It was a prospective interventional study of a young female, who was a known case of Vogt-Koyanagi-Harada syndrome. She presented with an inflammatory choroidal neovascualar membrane and signs of panuveitis in the right eye. She underwent a complete ophthalmic examination. She was given intravitreal injection of bevacizumab and IVTA at different sites. There was complete regression of CNVM and ocular inflammation within a week. After six months, she had recurrence of CNVM in the same eye, which was treated similarly. There was a complete resolution of CNVM and ocular inflammation after the combination therapy and systemic steroids, until one year of follow-up. No serious systemic or ocular adverse events were noted. Combination therapy appears to be an effective and safe method in the management of recurrent inflammatory CNVM.
Keywords: Bevacizumab, choroidal neovacular membrane, panuveitis, triamcinolone acetonide, Vogt-Koyanagi-Harada syndrome
Chronic inflammatory insults, gradually destroy the choriocapillaris and Bruch's membrane.[1] Corticosteroids decrease vascular permeability by stabilizing the basement membrane of the CNVM and decreasing cytokine production, which may prevent vascular budding. Currently, intravitreal anti-vascular endothelial growth factors (VEGF) is widely used in clinical practice for ocular neovascular disease. We herein, report the management of a 17-year-old, Omani female, who presented with recurrent inflammatory CNVM secondary to Vogt-Koyanagi-Harada syndrome (VKH) syndrome. She was treated with both intravitreal bevacizumab and triamcinolone acetonide (IVTA) at the same sittings. The safety and the outcome of the therapy were evaluated.
Case Report
It is a prospective interventional case study of a female referred for sudden decrease in vision of a week duration in the right eye (RE). She was a known case of Vogt-Koyanagi-Harada syndrome, which, diagnosed five years ago was managed in another institute. The fundus pictures and fundus fluorescein angiography (FA), done at the time of the first episode recovered from the patient is shown in Fig. 1. At the time of referral to us, she was not on any topical or systemic medications. She underwent a complete ocular examination, intraocular pressure recording (IOP), optical coherence tomography (OCT) and FA. She was given intravitreal injection of bevacizumab (1.25 mg) and 2 mg /0.05 ml of intravitreal triamcinolone acetonide (IVTA) at the same sitting at different sites after obtaining a written consent from her parent. After six months, she had recurrence of peripapillary CNVM in the same eye. She again underwent combination intravitreal therapy. The pros and cons of the procedure were discussed with the parent and the patient, and were in accordance with the ethical standards of the institution.
Figure 1.
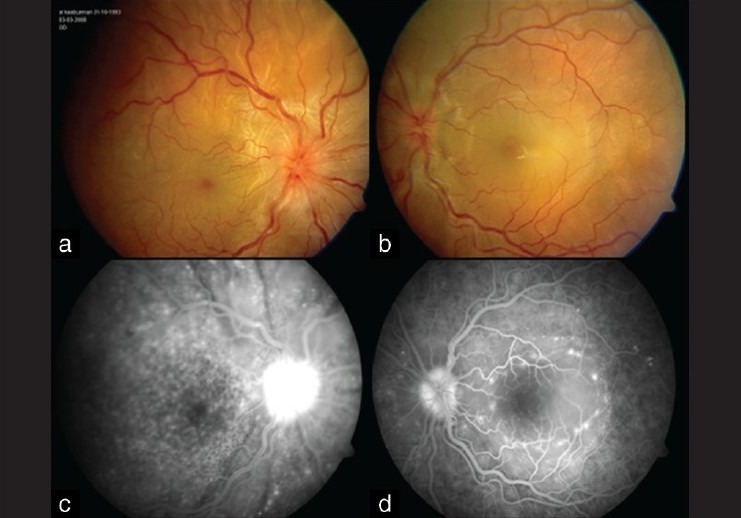
Color Fundus photo and fluorescein angiogram (FA) of both eyes. (a and b) shows optic disc hyperemia and edema with multifocal serous retinal detachment. (c and d) show FA pictures with multiple hyper fluorescent spots with pooling of fluorescein in the sub retinal space
The vision at presentation was 20/200 in the RE, IOP 14 mmHg. She had bilateral panuveitis, RE fundus examination showed disc hyperemia, peripapillary and subfoveal CNVM with macular exudation [Fig. 2a]. Periphery showed discrete, multiple, deep retinal, yellow spots suggestive of Dalen-Fuchs spots. Optical coherence tomography and FA in the RE were suggestive of CNVM involving the macula and peripapillary zone Figs. 2b and d. She underwent both intravitreal bevacizumab and IVTA at the same sitting at different sites and was given topical antibiotics for one week. She was also given systemic (Tab Prednisolone 40 mg) and topical steroids, which was slowly tapered with resolution of bilateral panuveitis. Within a week, postoperatively, there was improvement of vision to 20/30 in the RE. Repeat FA and OCT showed complete resolution of macular edema and CNVM with decrease in ocular inflammation [Figs. 2c and e]. After six months, she presented with scotomas in the same eye. She maintained 20/30 vision. There were signs of bilateral ocular inflammation more in the RE. Right eye showed blurred disc margins with peripapillary, yellowish subretinal lesion with haemorrhage, [Fig. 3a]. FA revealed peripapillary CNVM in the RE [Fig. 3b]. She again underwent combination intravitreal therapy. She was also given a immunosuppressive dose of oral steroids. There was regression of CNVM over a period of 1 month and she maintained 20/30 vision until last follow-up of 1 year [Fig. 3c].
Figure 2.
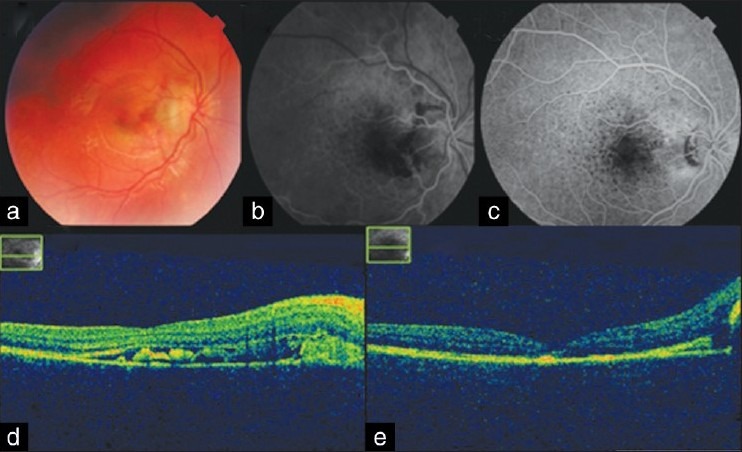
Right eye, fundus photo, fluorescein angiogram (FA), and Opticalcoherence tomography images (OCT). (a) Color photo shows temporal peripapillary and macular exudation. (b) FA, Early frames showing peripapillary hyperfluorescence and Blocked fluorescence at the macula. (c) FA frame showing regression of CNVM (d) OCT, image suggestive of CNVM. (e) OCT, after one week showing regression of CNVM and exudation
Figure 3.
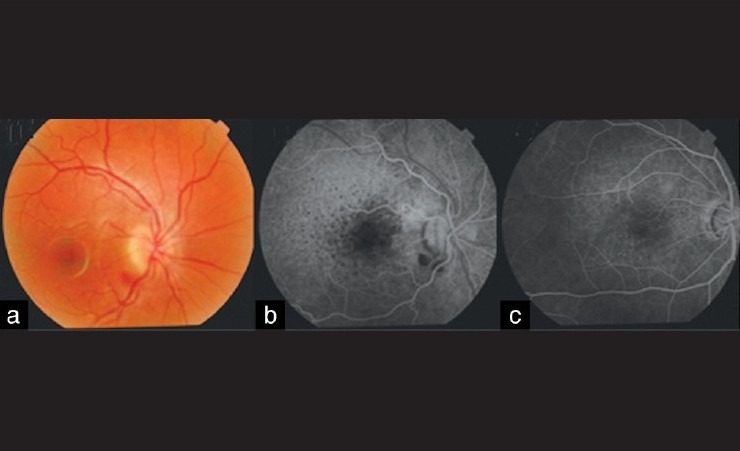
Right eye, fundus and fluorescein angiogram frames at the time of recurrence of CNVM six months later. (a) Photo showing blurring of optic disc margins with temporal peripapillary yellowish, subretinal lesion with haemorrhage. (b) FA, early frames showing peripapillary hyperfluorescence and area of blocked fluorescence. (c) FA, frame showing regression of CNVM
Discussion
Vogt-Koyanagi-Harada syndrome causes chronic, bilateral panuveitis with recurrent remissions. Choroidal neovascular membrane (CNVM) is one of the complications of chronic posterior uveitis, and is found in 15% of VKH syndrome patients.[1] Vascular endothelial growth factors (VEGF) have been implicated as one of the causative factors for increased vascular leakage and new vessel formation. Intravitreal bevacizumab has led to significant visual improvement and regression of inflammatory ocular neovascularization in various inflammatory ocular diseases.[2,3] Recently, CNVM secondary to VKH syndrome in a 14-year-old had a favourable outcome following intravitreal bevacizumab therapy.[3] Corticosteroids are investigated for angiostatic and anti-permeability properties. Immunosuppression is required to dampen the chronic inflammatory drive.[4] Therefore, in this case, a combination of intravitreal anti VEGF and corticosteroid with systemic immunosuppressive therapy was effective in the management of inflammatory CNVM with no serious systemic or ocular side effects.
Thus, the ideal therapeutic goal should be to achieve not only CNVM eradication but also inflammation reduction and VEGF down regulation in order to produce a sustained effect.[5]
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Wu L, Evans T, Saraiva M, Schlaen A, Couto C. Intravitreal bevacizumab for choroidal neovascularization secondary to Vogt–Koyanagi–Harada syndrome. Jpn J Ophthalmol. 2009;53:57–60. doi: 10.1007/s10384-008-0600-4. [DOI] [PubMed] [Google Scholar]
- 2.Mansour AM, Mackensen F, Arevalo JF, Ziemssen F, Mahendradas P, Mehio-Sibai A, et al. Intravitreal bevacizumab in inflammatory ocular neovascularization. Am J Ophthalmol. 2008;146:410–6. doi: 10.1016/j.ajo.2008.05.024. [DOI] [PubMed] [Google Scholar]
- 3.Raffa L, Bawazeer A. Intravitreal bevacizumab injection in a 14-year-old Vogt-Koyanagi-Harada patient with choroidal neovascular membrane. Can J Ophthalmol. 2009;44:615–6. doi: 10.3129/i09-144. [DOI] [PubMed] [Google Scholar]
- 4.Dhingra N, Kelly S, Majid MA, Bailey CB, Dick AD. Inflammatory choroidal neovascular membrane in posterior uveitis-pathogenesis and treatment. Indian J Ophthalmol. 2010;58:3–10. doi: 10.4103/0301-4738.58467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yip PP, Woo CF, Tang HH, Ho CK. Triple therapy for neovascular age-related macular degeneration using single-session photodynamic therapy combined with intravitreal bevacizumab and triamcinolone. Br J Ophthalmol. 2009;93:754–8. doi: 10.1136/bjo.2008.150987. [DOI] [PMC free article] [PubMed] [Google Scholar]


