Abstract
AIM: To investigate the relationship between Helicobacter pylori (H. pylori) seropositivity and the presence of microalbuminuria.
METHODS: Between December 2003 and February 2010, asymptomatic individuals who visited the Seoul National University Healthcare System Gangnam Center for a routine check-up and underwent tests for H. pylori immunoglobulin G antibodies and urinary albumin to creatinine ratio (UACR) were included. All study subjects completed a structured questionnaire, anthropometric measurements and laboratory tests. Anti-H. pylori immunoglobulin G was identified using an enzyme-linked immunosorbent assay kit. A random single-void urine sample, collected using a clean-catch technique, was obtained to determine the UACR. The presence of microalbuminuria was defined as a UACR from 30 to 300 μg/mg. The presence of diabetes mellitus (DM) was defined as either a fasting serum glucose level greater than or equal to 126 mg/dL or taking anti-diabetic medication. Multiple logistic regression analysis was performed to identify the risk factors. The dependent variable was microalbuminuria, and the independent variables were the other study variables.
RESULTS: A total of 2716 subjects (male, 71.8%; mean age, 54.9 years) were included. Among them, 224 subjects (8.2%) had microalbuminuria and 324 subjects (11.9%) had been diagnosed with DM. Subjects with microalbuminuria had a significantly higher H. pylori seropositivity rate than subjects without microalbuminuria (60.7% vs 52.8%, P = 0.024). Multivariate analysis after adjustment for age, body mass index (BMI), waist circumference, and glucose and triglyceride levels showed that H. pylori seropositivity was significantly associated with microalbuminuria [odds ratio (OR), 1.40, 95% CI, 1.05-1.89, P = 0.024]. After the data were stratified into cohorts by glucose levels (≤ 100 mg/dL, 100 mg/dL < glucose < 126 mg/dL, and ≥ 126 mg/dL or history of DM), H. pylori seropositivity was found to be significantly associated with microalbuminuria in diabetic subjects after adjusting for age, BMI and serum creatinine level (OR, 2.21, 95% CI, 1.20-4.08, P = 0.011). In addition, the subjects were divided into five groups. Those without microalbuminuria (an UACR of < 30 μg/mg) were divided into four groups in accordance with their UACR values, and subjects with microalbuminuria comprised their own group. Notably, H. pylori seropositivity gradually increased with an increase in UACR (P = 0.001) and was highest in subjects with microalbuminuria (OR, 2.41, 95% CI, 1.14-5.11). This suggests that H. pylori seropositivity is positively associated with microalbuminuria in diabetic subjects.
CONCLUSION: H. pylori seropositivity was independently associated with microalbuminuria, and the prevalence of H. pylori seropositivity was associated with the severity of UACR in diabetic subjects.
Keywords: Helicobacter pylori, Seropositivity, Microalbuminuria, Atherosclerosis, Diabetes
INTRODUCTION
Helicobacter pylori (H. pylori) infection has been implicated in various extragastric conditions, including coronary heart disease and ischemic cerebrovascular disorder caused by predisposing chronic inflammation and atherosclerosis[1-5]. The association between H. pylori seropositivity and coronary artery calcium scores was recently reported[6]. Moreover, H. pylori infection was found to be associated with reduced high density lipoprotein and elevated low density lipoprotein levels in serum[7,8]. Furthermore, a prospective single-center study showed that H. pylori eradication had beneficial effects on insulin resistance, lipid abnormalities and low-grade inflammation[9]. These findings suggest a role for H. pylori infection in subjects with metabolic syndrome, including diabetes.
In contrast, microalbuminuria, which is defined as an increased urinary albumin to creatinine ratio (UACR) of 30-300 μg/mg[10], has been known to be a strong predictor of the development of diabetic nephropathy[11]. It has also been demonstrated that microalbuminuria is a risk factor for cardiovascular disease in the general and diabetic populations[12-14]. Although the mechanism linking microalbuminuria to cardiovascular morbidity remains unclear, one possible explanation is that the increased urinary leakage of albumin reflects vascular damage, i.e., endothelial dysfunction or low-grade chronic inflammation[15]. In addition, some studies have reported a relationship between microalbuminuria and metabolic syndrome, suggesting that insulin resistance underlies the pathogenesis of microalbuminuria[16-18].
Our hypothesis was that if H. pylori infection is involved in the pathogenesis of atherosclerosis, a significant association might exist between H. pylori infection and microalbuminuria, which is an early marker of atherosclerosis. Therefore, we aimed to investigate the relationship between H. pylori infection and microalbuminuria in subjects presenting for a routine health check-up.
MATERIALS AND METHODS
Study population
This cross-sectional study was conducted at the Seoul National University Hospital Gangnam Healthcare Center between March 2003 and February 2010. During the study period, a total of 2737 asymptomatic individuals visited our center for a routine check-up, including H. pylori serology and UACR tests. Among them, 21 subjects who showed macroalbuminuria exceeding 300 μg/mg were excluded. Accordingly, 2716 individuals comprised the study population. The presence of diabetes mellitus (DM) was defined as either a fasting serum glucose level greater than or equal to 126 mg/dL or taking anti-diabetic medication. This study was approved by the Institutional Review Board of Seoul National University Hospital, which waived the requirement for informed consent.
Clinical and laboratory assessments
All study subjects completed a structured questionnaire and underwent anthropometric measurements and laboratory tests. A current smoker was defined as a subject who had smoked 100 or more cigarettes during his lifetime and smoked daily at the time of the examination[19]. Height and body weight were measured using a digital scale, and body mass index (BMI) was calculated as follows: BMI = body weight (kg)/height squared (m2). Systolic and diastolic blood pressures were measured in a sitting position after a 5-min rest, twice a day; mean values were used in the analysis. Blood samples were collected after at least a 12 h of fasting and used to determine glucose, triglyceride, high density lipoprotein cholesterol, and creatinine levels. Serum creatinine concentrations were determined using the Jaffe rate reaction. Anti-H. pylori immunoglobulin G was identified using an enzyme-linked immunosorbent assay kit (H. pylori-EIA-Well, Radim, Italy) and an automatic analyzer, Alisei® (Seac, Italy). The cut-off values were set according to the manufacturer’s instructions.
A random single-void urine sample using a clean-catch technique after at least 12 h of fasting was obtained to determine the UACR (μg/mg). Urinary albumin excretion was measured using an immunoturbidimetric assay, and urinary creatinine was measured using the Jaffe rate reaction. Microalbuminuria was defined as a UACR from 30 μg/mg to 300 μg/mg.
Statistical analysis
Analyses were performed using the SPSS statistical package (Version 17.0, SPSS, Inc., Chicago, IL, United States). A Pearson χ2 test was used to examine associations between microalbuminuria and the study variables, and P values of < 0.05 were considered statistically significant. Multiple logistic regression analysis was performed to identify risk factors. The dependent variable was microalbuminuria, and the independent variables were the other study variables. Odds ratios (OR) and the relevant 95% CI are presented for all of the potential risk factors.
RESULTS
Clinical characteristics of the study population
The mean age of the 2716 study subjects was 54.9 years, and 71.8% were men. Of the subjects, 224 (8.2%) had microalbuminuria, and 324 (11.9%) met the criteria for DM, either by taking diabetic medications or showing fasting serum glucose level in the diabetic range (≥ 126 mg/dL). BMI and the serum glucose, triglyceride and creatinine levels were found to be significantly higher in subjects with microalbuminuria than in those without microalbuminuria. In addition, subjects with microalbuminuria had a significantly higher H. pylori seropositivity rate than subjects without microalbuminuria (Table 1).
Table 1.
Baseline characteristics
| Normal (n = 2492) | Microalbuminuria (n = 224) | P value | |
| Male | 1 781 (71.5) | 170 (75.9) | 0.159 |
| Age1 (yr) | 54.6 (9.1) | 57.7 (10.5) | < 0.001 |
| BMI1 (kg/m2) | 24.2 (2.8) | 25.5 (3.4) | < 0.001 |
| Waist circumference1 (cm) | 86.9 (7.6) | 89.8 (8.8) | < 0.001 |
| Glucose1 (mg/dL) | 102.4 (19.5) | 118.3 (33.2) | < 0.001 |
| Triglyceride1 (mg/dL) | 129.1 (78.2) | 161.2 (117.2) | < 0.001 |
| HDL cholesterol1 (mg/dL) | 52.7 (12.3) | 50.2 (12.6) | 0.005 |
| Creatinine1 (mg/dL) | 1.0 (0.2) | 1.0 (0.2) | 0.026 |
| SBP1 (mmHg) | 119.0 (14.7) | 119.2 (15.6) | 0.899 |
| DBP1 (mmHg) | 78.6 (11.2) | 78.1 (11.8) | 0.577 |
| Hypertension | 259 (10.4) | 24 (10.7) | 0.880 |
| Diabetes mellitus | 256 (10.3) | 68 (30.4) | < 0.001 |
| Current smoking | 364 (16.6) | 40 (20.4) | 0.170 |
| H. pylori seropositivity | 1317 (52.8) | 136 (60.7) | 0.024 |
Data are presented as the mean ± SD. BMI: Body mass index; HDL: High density lipoprotein; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; H. pylori: Helicobacter pylori.
Risk factors of microalbuminuria
The results of the univariate and multivariate analyses of the risk factors for microalbuminuria are shown in Table 2. Multivariate analysis after adjustment for age, waist circumference, glucose, triglyceride and BMI showed that H. pylori seropositivity was statistically associated with microalbuminuria (OR, 1.40, 95% CI, 1.05-1.89, P = 0.024; Table 2). Because serum glucose level is the most well-known factor determining microalbuminuria, we performed the analysis after stratifying the cohort by glucose levels (≤ 100 mg/dL, 100 mg/dL < glucose < 126 mg/dL, and ≥ 126 mg/dL or history of DM) to reduce the confounding effect of serum glucose level. As a result, H. pylori seropositivity was significantly associated with microalbuminuria in diabetic subjects after adjusting for age, BMI and serum creatinine level (OR, 2.21, 95% CI, 1.20-4.08, P = 0.011). However, the relation between H. pylori seropositivity and microalbuminuria was not statistically significant in non-diabetic subjects.
Table 2.
Univariate and multivariate analysis assessing independent risk factors of microalbuminuria
| Variables |
Univariate analysis |
Multivariate analysis |
||||
| OR | 95% CI | P value | OR | 95% CI | P value | |
| H. pylori seropositivity | 1.38 | 1.04-1.82 | 0.024 | 1.40 | 1.05-1.89 | 0.024 |
| Age (yr) | 1.04 | 1.02-1.05 | < 0.001 | 1.04 | 1.02-1.06 | < 0.001 |
| Sex | 1.28 | 0.91-1.73 | 0.159 | - | - | - |
| BMI | 1.15 | 1.09-1.20 | < 0.001 | 1.15 | 1.04-1.27 | 0.005 |
| WC | 1.05 | 1.03-1.07 | < 0.001 | 0.98 | 0.94-1.01 | 0.213 |
| Glucose | 1.02 | 1.02-1.03 | < 0.001 | 1.02 | 1.01-1.12 | < 0.001 |
| Triglyceride | 1.00 | 1.00-1.005 | < 0.001 | 1.00 | 1.00-1.00 | 0.001 |
| HDL cholesterol | 0.98 | 0.97-0.99 | 0.004 | 1.00 | 0.99-1.01 | 0.959 |
| Creatinine | 2.87 | 1.38-5.96 | 0.005 | 1.57 | 0.71-3.51 | 0.267 |
| Smoking | 1.29 | 1.86-1.87 | 0.171 | - | - | - |
| Hypertension | 1.04 | 0.67-1.61 | 0.880 | - | - | - |
| SBP | 1.00 | 0.99-1.01 | 0.894 | - | - | - |
| DBP | 1.00 | 0.98-1.01 | 0.558 | - | - | - |
H. pylori: Helicobacter pylori; OR: Odds ratio; BMI: Body mass index; WC: Waist circumference; HDL: High density lipoprotein; SBP: Systolic blood pressure; DBP: Diastolic blood pressure.
Helicobacter pylori infection and microalbuminuria in diabetic subjects
The seropositivity rates for H. pylori in diabetic subjects and non-diabetic subjects were 50% (162/324) and 54% (1291/2392), respectively. Because H. pylori seropositivity was found to be significantly associated with an increased prevalence of microalbuminuria in diabetic subjects, we evaluated the relation between the severity of UACR and H. pylori seropositivity. The subjects were divided into five groups. Those without microalbuminuria (an UACR of < 30 μg/mg) were divided into four groups in accordance with their UACR values, and subjects with microalbuminuria comprised their own group. The percentage of H. pylori seropositivity was found to gradually increase with UACR (P = 0.001; Figure 1), and the highest rate was observed in subjects with microalbuminuria (OR, 2.41, 95% CI, 1.14-5.11; Table 3), suggesting that H. pylori seropositivity is positively associated with microalbuminuria in diabetic subjects.
Figure 1.
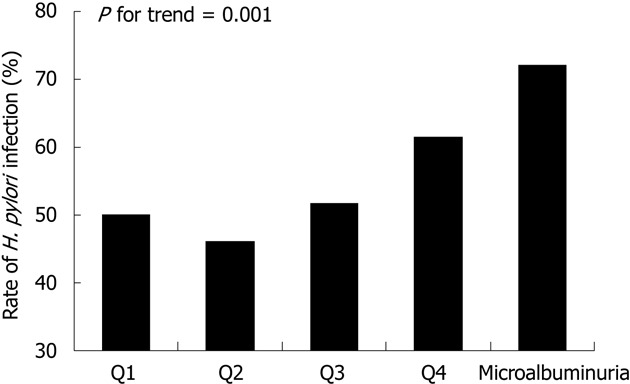
The rate of Helicobacter pylori seropositivity according to the urinary albumin to creatinine ratio in diabetic subjects. The subjects were divided into five groups: subjects without microalbuminuria were divided into four groups in accordance with their urine albumin to creatinine ratio values, and subjects with microalbuminuria comprised their own group: Q1, < 4.9 μg/mg; Q2, 5.0-7.9 μg/mg; Q3, 8.0-13.9 μg/mg; Q4, 14.0-29.9 μg/mg and microalbuminuria, > 30 μg/mg. H. pylori: Helicobacter pylori.
Table 3.
Relationship of the severity of the urine albumin to creatinine ratio to Helicobacter pylori seropositivity in diabetes subjects
| Urine albumin-creatinine ratio (μg/mg) | n | H. pylori seropositivity (%) | OR (95% CI) | P for trend |
| Q1 (< 4.9) | 64 | 50.0 | Reference | 0.001 |
| Q2 (5.0-7.9) | 63 | 46.0 | 0.86 (0.42-1.01) | |
| Q3 (8.0-13.9) | 64 | 51.6 | 1.10 (0.36-2.23) | |
| Q4 (14.0-29.9) | 65 | 61.5 | 1.55 (0.75-3.19) | |
| Microalbuminuria | 68 | 72.1 | 2.41 (1.14-5.11) |
H. pylori: Helicobacter pylori; OR: Odds ratio.
DISCUSSION
This study shows that H. pylori seropositivity is independently associated with the presence of microalbuminuria, and the prevalence of H. pylori seropositivity shows a positive correlation with the severity of urine albumin creatinine ratio in diabetic subjects. These findings suggest that H. pylori infection might affect microvascular damage and possibly contributes to pathogenesis of early atherosclerosis in diabetes.
The mechanisms underlying increased urinary albumin excretion are complex, but endothelial cell dysfunction appears be a major pathogenic contributor[20]. Moreover, microalbuminuria is known to be associated with atherogenic risk factors, such as hypertension, hyperglycemia, central obesity and hyperinsulinemia[21]. In the present study, we consistently found that metabolic variables, such as glucose, triglyceride and BMI were significantly associated with microalbuminuria. In particular, H. pylori seropositivity was found to be positively related to microalbuminuria after adjusting for other variables, which suggests that H. pylori infection might participate in the pathogenesis of endothelial dysfunction. There have been some studies suggesting the association between H. pylori infection and endothelial dysfunction; Oshima et al[22] reported that H. pylori seropositivity was associated with elevated C-reactive protein and soluble intercellular adhesion molecule-1. This indicates that chronic H. pylori infection might be involved in the pathogenesis of atherosclerosis. Prasad et al[23] showed that the immunoglobulin-G antibody response to pathogens was an independent risk factor for endothelial dysfunction and coronary atherosclerosis.
A possible mechanism linking H. pylori infection and endothelial dysfunction is the association between H. pylori infection and insulin resistance. Recently, a systematic review has reported a positive association between H. pylori infection and a homeostatic model of assessing insulin resistance[24]. H. pylori infection was significantly associated with metabolic syndrome in a large Japanese population[25]. Furthermore, Gunji et al[26] found that H. pylori infection significantly increases insulin resistance in the asymptomatic population. A recent prospective study showed the beneficial effect of H. pylori eradication on insulin resistance, serum lipid and low-grade inflammation[27]. It remains uncertain how the presence of H. pylori affects the pathogenic process of insulin resistance. The disturbance of proinflammatory and vasoactive substances, such as tumor necrosis factor-α, interlukin-6 and c-reactive protein, may be involved in the pathogenesis of insulin resistance[28,29]. Moreover, the reactive oxygen species caused by an H. pylori infection also affects insulin resistance[30,31].
Many studies have demonstrated that elevated blood pressure, poor glycemic control, older age and insulin resistance are associated with microalbuminuria in subjects with diabetes[32,33]. In this study, we stratified the study population according to glucose levels to reduce the confounding effect, and the association between H. pylori seropositivity and microalbuminuria was more potent in diabetic subjects than in non-diabetic and pre-diabetic subjects. Diabetic patients are known to have impaired function of cellular and humoral immunity, and consequently, the direct invasion of the arterial wall by bacteria might be more frequent in these patients than in non-diabetic ones. Indeed, some previous studies have found a higher prevalence of H. pylori infection among diabetic patients[34,35]. On the other hand, other studies did not detect an association between H. pylori infection and diabetes[36,37], and these contradictory results among studies might have resulted from differing methods used by the studies and from the uneven epidemiological distribution of H. pylori infection.
This study has several advantages. First, to the best our knowledge, this is the only study of the association between H. pylori infection and microalbuminuria. Second, it utilized a large study population, and we constructed a multiple regression model containing many metabolic confounding factors. Third, subjects in this study were an apparently healthy population that presented for screening, and such populations seems to approximate the general population.
Nevertheless, the study has several limitations. First, it does not provide details regarding the nature of the causative relation between H. pylori seropositivity and microalbuminuria because of the cross-sectional study design. Second, although the H. pylori seropositivity does not indicate current H. pylori infection, seropositivity for H. pylori-specific immunoglobulin G antibody was taken as a surrogate of H. pylori infection status in the present study. Thus, there might be some false-positive or false-negative subjects. Third, we did not evaluate H. pylori-induced inflammatory and virulence factors, such as the cag A gene, which could contribute to the pathogenesis of H. pylori-induced early atherosclerosis.
In conclusion, H. pylori seropositivity was independently associated with the presence of microalbuminuria, and the prevalence of H. pylori seropositivity was positively correlated with the severity of urine albumin creatinine ratio in diabetic subjects. Our findings suggest that H. pylori infection might be involved in the pathogenesis of early atherosclerosis in diabetes.
COMMENTS
Background
Helicobacter pylori (H. pylori) infection has been implicated in various extragastric conditions including coronary heart disease and ischemic cerebrovascular disorder, caused by predisposing chronic inflammation and atherosclerosis. On the other hand, microalbuminuria is a known early marker of renal and cardiovascular diseases. Their hypothesis was that if H. pylori infection is involved in the pathogenesis of atherosclerosis, a significant association might exist between H. pylori infection and microalbuminuria, which is an early marker of atherosclerosis.
Research frontiers
Recent studies have reported the association between H. pylori infection and endothelial dysfunction. H. pylori infection significantly increases insulin resistance in the asymptomatic population and it also associated with metabolic syndrome in a large Japanese population. Moreover, the beneficial effect of H. pylori eradication on insulin resistance was reported.
Innovations and breakthroughs
This study showed that H. pylori seropositivity is independently associated with presence of microalbuminuria and the prevalence of H. pylori seropositivity showed a positive correlation with the severity of the urine albumin creatinine ratio in diabetic subjects.
Applications
This study suggests that H. pylori infection might affect microvascular damage and possibly contributes to the pathogenesis of early atherosclerosis in diabetes.
Peer review
The authors have studied the relationship between the occurrence of H. pylori and microalbuminuria in a healthy population. The association between H. pylori and microalbuminuria has only recently been reported and has not been studied in a larger setting. Thus, the paper is of importance and novel. The paper is well written and well presented. Regarding ethics, the local review board had waived the need for written consent.
Footnotes
P- Reviewers Vorobjova T, Paulssen EJ, Wang JT S- Editor Gou SX L- Editor A E- Editor Xiong L
References
- 1.Pellicano R, Franceschi F, Saracco G, Fagoonee S, Roccarina D, Gasbarrini A. Helicobacters and extragastric diseases. Helicobacter. 2009;14 Suppl 1:58–68. doi: 10.1111/j.1523-5378.2009.00699.x. [DOI] [PubMed] [Google Scholar]
- 2.Vizzardi E, Bonadei I, Piovanelli B, Quinzani F, Ricci C, Lanzini A, Dei Cas L. Helicobacter pylori and ischemic heart disease. Panminerva Med. 2011;53:193–202. [PubMed] [Google Scholar]
- 3.Sung KC, Rhee EJ, Ryu SH, Beck SH. Prevalence of Helicobacter pylori infection and its association with cardiovascular risk factors in Korean adults. Int J Cardiol. 2005;102:411–417. doi: 10.1016/j.ijcard.2004.05.040. [DOI] [PubMed] [Google Scholar]
- 4.Danesh J, Collins R, Peto R. Chronic infections and coronary heart disease: is there a link? Lancet. 1997;350:430–436. doi: 10.1016/S0140-6736(97)03079-1. [DOI] [PubMed] [Google Scholar]
- 5.Nazmi A, Diez-Roux AV, Jenny NS, Tsai MY, Szklo M, Aiello AE. The influence of persistent pathogens on circulating levels of inflammatory markers: a cross-sectional analysis from the Multi-Ethnic Study of Atherosclerosis. BMC Public Health. 2010;10:706. doi: 10.1186/1471-2458-10-706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park MJ, Choi SH, Kim D, Kang SJ, Chung SJ, Choi SY, Yoon DH, Lim SH, Kim YS, Yim JY, et al. Association between Helicobacter pylori Seropositivity and the Coronary Artery Calcium Score in a Screening Population. Gut Liver. 2011;5:321–327. doi: 10.5009/gnl.2011.5.3.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jia EZ, Zhao FJ, Hao B, Zhu TB, Wang LS, Chen B, Cao KJ, Huang J, Ma WZ, Yang ZJ, et al. Helicobacter pylori infection is associated with decreased serum levels of high density lipoprotein, but not with the severity of coronary atherosclerosis. Lipids Health Dis. 2009;8:59. doi: 10.1186/1476-511X-8-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim HL, Jeon HH, Park IY, Choi JM, Kang JS, Min KW. Helicobacter pylori infection is associated with elevated low density lipoprotein cholesterol levels in elderly Koreans. J Korean Med Sci. 2011;26:654–658. doi: 10.3346/jkms.2011.26.5.654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gen R, Demir M, Ataseven H. Effect of Helicobacter pylori eradication on insulin resistance, serum lipids and low-grade inflammation. South Med J. 2010;103:190–196. doi: 10.1097/SMJ.0b013e3181cf373f. [DOI] [PubMed] [Google Scholar]
- 10.National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39:S1–266. [PubMed] [Google Scholar]
- 11.Mogensen CE, Chachati A, Christensen CK, Close CF, Deckert T, Hommel E, Kastrup J, Lefebvre P, Mathiesen ER, Feldt-Rasmussen B. Microalbuminuria: an early marker of renal involvement in diabetes. Uremia Invest 1985- 1986;9:85–95. doi: 10.3109/08860228509088195. [DOI] [PubMed] [Google Scholar]
- 12.Borch-Johnsen K, Feldt-Rasmussen B, Strandgaard S, Schroll M, Jensen JS. Urinary albumin excretion. An independent predictor of ischemic heart disease. Arterioscler Thromb Vasc Biol. 1999;19:1992–1997. doi: 10.1161/01.atv.19.8.1992. [DOI] [PubMed] [Google Scholar]
- 13.Jørgensen L, Jenssen T, Johnsen SH, Mathiesen EB, Heuch I, Joakimsen O, Fosse E, Jacobsen BK. Albuminuria as risk factor for initiation and progression of carotid atherosclerosis in non-diabetic persons: the Tromsø Study. Eur Heart J. 2007;28:363–369. doi: 10.1093/eurheartj/ehl394. [DOI] [PubMed] [Google Scholar]
- 14.Yudkin JS, Forrest RD, Jackson CA. Microalbuminuria as predictor of vascular disease in non-diabetic subjects. Islington Diabetes Survey. Lancet. 1988;2:530–533. doi: 10.1016/s0140-6736(88)92657-8. [DOI] [PubMed] [Google Scholar]
- 15.Deckert T, Feldt-Rasmussen B, Borch-Johnsen K, Jensen T, Kofoed-Enevoldsen A. Albuminuria reflects widespread vascular damage. The Steno hypothesis. Diabetologia. 1989;32:219–226. doi: 10.1007/BF00285287. [DOI] [PubMed] [Google Scholar]
- 16.Sheng CS, Hu BC, Fan WX, Zou J, Li Y, Wang JG. Microalbuminuria in relation to the metabolic syndrome and its components in a Chinese population. Diabetol Metab Syndr. 2011;3:6. doi: 10.1186/1758-5996-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee JE, Huh W, Son HJ, Kim YG, Kim DJ, Lee MK, Oh HY. Association of metabolic syndrome with microalbuminuria in non-hypertensive type 2 diabetic patients. Nephron Clin Pract. 2007;106:c98–103. doi: 10.1159/000102996. [DOI] [PubMed] [Google Scholar]
- 18.Choi HS, Ryu SH, Lee KB. The relationship of microalbuminuria with metabolic syndrome. Nephron Clin Pract. 2006;104:c85–c93. doi: 10.1159/000093995. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention (CDC) Cigarette smoking among adults--United States, 1994. MMWR Morb Mortal Wkly Rep. 1996;45:588–590. [PubMed] [Google Scholar]
- 20.Glassock RJ. Is the presence of microalbuminuria a relevant marker of kidney disease? Curr Hypertens Rep. 2010;12:364–368. doi: 10.1007/s11906-010-0133-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim YI, Kim CH, Choi CS, Chung YE, Lee MS, Lee SI, Park JY, Hong SK, Lee KU. Microalbuminuria is associated with the insulin resistance syndrome independent of hypertension and type 2 diabetes in the Korean population. Diabetes Res Clin Pract. 2001;52:145–152. doi: 10.1016/s0168-8227(01)00228-5. [DOI] [PubMed] [Google Scholar]
- 22.Oshima T, Ozono R, Yano Y, Oishi Y, Teragawa H, Higashi Y, Yoshizumi M, Kambe M. Association of Helicobacter pylori infection with systemic inflammation and endothelial dysfunction in healthy male subjects. J Am Coll Cardiol. 2005;45:1219–1222. doi: 10.1016/j.jacc.2005.01.019. [DOI] [PubMed] [Google Scholar]
- 23.Prasad A, Zhu J, Halcox JP, Waclawiw MA, Epstein SE, Quyyumi AA. Predisposition to atherosclerosis by infections: role of endothelial dysfunction. Circulation. 2002;106:184–190. doi: 10.1161/01.cir.0000021125.83697.21. [DOI] [PubMed] [Google Scholar]
- 24.Polyzos SA, Kountouras J, Zavos C, Deretzi G. The association between Helicobacter pylori infection and insulin resistance: a systematic review. Helicobacter. 2011;16:79–88. doi: 10.1111/j.1523-5378.2011.00822.x. [DOI] [PubMed] [Google Scholar]
- 25.Gunji T, Matsuhashi N, Sato H, Fujibayashi K, Okumura M, Sasabe N, Urabe A. Helicobacter pylori infection is significantly associated with metabolic syndrome in the Japanese population. Am J Gastroenterol. 2008;103:3005–3010. doi: 10.1111/j.1572-0241.2008.02151.x. [DOI] [PubMed] [Google Scholar]
- 26.Gunji T, Matsuhashi N, Sato H, Fujibayashi K, Okumura M, Sasabe N, Urabe A. Helicobacter pylori infection significantly increases insulin resistance in the asymptomatic Japanese population. Helicobacter. 2009;14:144–150. doi: 10.1111/j.1523-5378.2009.00705.x. [DOI] [PubMed] [Google Scholar]
- 27.Kanbay M, Gür G, Yücel M, Yilmaz U, Boyacioğlu S. Does eradication of Helicobacter pylori infection help normalize serum lipid and CRP levels? Dig Dis Sci. 2005;50:1228–1231. doi: 10.1007/s10620-005-2764-9. [DOI] [PubMed] [Google Scholar]
- 28.Aebischer T, Meyer TF, Andersen LP. Inflammation, immunity, and vaccines for Helicobacter. Helicobacter. 2010;15 Suppl 1:21–28. doi: 10.1111/j.1523-5378.2010.00777.x. [DOI] [PubMed] [Google Scholar]
- 29.Basso D, Plebani M, Kusters JG. Pathogenesis of Helicobacter pylori infection. Helicobacter. 2010;15 Suppl 1:14–20. doi: 10.1111/j.1523-5378.2010.00781.x. [DOI] [PubMed] [Google Scholar]
- 30.Aslan M, Horoz M, Nazligul Y, Bolukbas C, Bolukbas FF, Selek S, Celik H, Erel O. Insulin resistance in H pylori infection and its association with oxidative stress. World J Gastroenterol. 2006;12:6865–6868. doi: 10.3748/wjg.v12.i42.6865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kebapcilar L, Sari I, Renkal AH, Alacacioglu A, Yuksel A, Ilhan E, Alkan B, Yuksel D, Kozaci DL, Gunay N. The influence of Helicobacter pylori eradication on leptin, soluble CD40 ligand, oxidative stress and body composition in patients with peptic ulcer disease. Intern Med. 2009;48:2055–2059. doi: 10.2169/internalmedicine.48.2562. [DOI] [PubMed] [Google Scholar]
- 32.Remuzzi G, Schieppati A, Ruggenenti P. Clinical practice. Nephropathy in patients with type 2 diabetes. N Engl J Med. 2002;346:1145–1151. doi: 10.1056/NEJMcp011773. [DOI] [PubMed] [Google Scholar]
- 33.De Cosmo S, Minenna A, Ludovico O, Mastroianno S, Di Giorgio A, Pirro L, Trischitta V. Increased urinary albumin excretion, insulin resistance, and related cardiovascular risk factors in patients with type 2 diabetes: evidence of a sex-specific association. Diabetes Care. 2005;28:910–915. doi: 10.2337/diacare.28.4.910. [DOI] [PubMed] [Google Scholar]
- 34.Hamed SA, Amine NF, Galal GM, Helal SR, Tag El-Din LM, Shawky OA, Ahmed EA, Abdel Rahman MS. Vascular risks and complications in diabetes mellitus: the role of helicobacter pylori infection. J Stroke Cerebrovasc Dis. 2008;17:86–94. doi: 10.1016/j.jstrokecerebrovasdis.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 35.Gulcelik NE, Kaya E, Demirbas B, Culha C, Koc G, Ozkaya M, Cakal E, Serter R, Aral Y. Helicobacter pylori prevalence in diabetic patients and its relationship with dyspepsia and autonomic neuropathy. J Endocrinol Invest. 2005;28:214–217. doi: 10.1007/BF03345375. [DOI] [PubMed] [Google Scholar]
- 36.Bures J, Smahelová A, Kopácová M, Rejchrt S. [Clinical importance of Helicobacter pylori infection in patients with diabetes mellitus] Vnitr Lek. 2004;50:350–353. [PubMed] [Google Scholar]
- 37.Demir M, Gokturk HS, Ozturk NA, Kulaksizoglu M, Serin E, Yilmaz U. Helicobacter pylori prevalence in diabetes mellitus patients with dyspeptic symptoms and its relationship to glycemic control and late complications. Dig Dis Sci. 2008;53:2646–2649. doi: 10.1007/s10620-007-0185-7. [DOI] [PubMed] [Google Scholar]


