Abstract
Objectives
The coronary artery calcium (CAC) score has been shown to predict future cardiac events. However the extent to which the added value of a CAC score to the diagnostic performance of myocardial perfusion imaging (MPI) by single photon emission computed tomography (SPECT) is unclear. The purpose of this study is to investigate the correlation between CAC score and SPECT in patients with suspected coronary artery disease.
Methods
A retrospective review of the CAC scores by use of the Agatston calcium scoring method and cardiac SPECT diagnostic reports was conducted in 48 patients, who underwent both coronary computed tomography (CT) and SPECT examinations due to suspected coronary artery disease. A Pearson correlation test was used to determine the relation between CAC scores and MPI-SPECT assessments with regard to the evaluation of the extent of disease.
Results
Forty-seven percent of the patients had CAC scores more than 100, while 42% of these patients demonstrated abnormal, or probably abnormal, MPI-SPECT. Of the 23% of patients with a zero CAC score, only 7% had normal MPI-SPECT findings. No significant correlation was found between the CAC scores and MPI-SPECT assessments (r value ranged from 0.012 to 0.080), regardless of the degree of coronary calcification.
Conclusions
There is a lack of correlation between the CAC scores and the MPI-SPECT findings in the assessment of the extent of coronary artery disease. CAC scores and MPI-SPECT should be considered complementary approaches in the evaluation of patients with suspected coronary artery disease.
Keywords: Coronary artery disease, Coronary calcium score, Coronary computed tomography, Myocardial perfusion imaging
1. Introduction
Multi-slice computed tomography (CT) has been increasingly used to detect coronary artery calcium and diagnose coronary artery stenosis. Quantifying the amount of coronary artery calcium (CAC) with non-enhanced CT scans has been widely accepted as a reliable non-invasive technique for screening patients with a potential risk of developing major cardiac events, and is usually quantified using the Agatston score.[1]–[4] The clinical application of CAC scoring has been supported by evidence showing that the absence of calcium reliably excludes obstructive coronary artery stenosis,[5] and that the amount of CAC is a strong predictor for risk assessment of myocardial infarction and sudden cardiac death, independent of conventional coronary risk factors.[6],[7] However, its predictive value is, in the end, determined by the patients' symptoms. In symptomatic patients, CAC scoring is considered as being only marginally related to the degree of coronary stenosis, and it is well known that both obstructive and non-obstructive coronary artery disease (CAD) can occur in the absence of calcification.[8],[9] According to these reports, low CAC scores are less valuable in the prediction of the prevalence, or severity, of coronary artery disease caused by the non-calcified coronary plaques.
Myocardial perfusion imaging (MPI) with gated single photon emission computed tomography (SPECT) has been widely used in the diagnosis of CAD and risk stratification with high diagnostic accuracy[10],[11] when compared to CT angiography. The presence of ischemia could be used to classify the patients as having CAD and candidates for receiving aggressive medical therapy and management. However, a normal MPI does not necessarily exclude significant coronary stenosis, while high CAC scores sometimes do not result in abnormal perfusion on MPI.[12]–[14] Thus, the exact relationship between CAD and MPI is not very clear. The purpose of this study is to correlate CAC scores with MPI by SPECT in a group of patients with suspected CAD. An important strength of this study is that simultaneous assessment of MPI and CAC scores was performed on all consecutive patients with suspected CAD, thus, the results could be applicable to similar populations of patients undergoing MPI examination.
2. Methods
2.1. Patient data collection
This retrospective study consisted of 48 patients (33 men and 15 women; mean age 61.7 years; range 44–81 years) with suspected coronary artery disease who underwent both multi-slice CT and MPI-SPECT examinations within two weeks. Patients who were referred first by general practitioners for coronary CT scans, and then, for MPI-SPECT by nuclear physicians, met the following inclusion criteria: no previous history of CAD; typical or atypical chest pain, dyspnea or signs of myocardial perfusion on a resting or stress ECG test. Medical history, including cardiovascular risk factors, blood pressure, lipid profile, electrocardiography (ECG) and 10-year CAD risk, predicted on the basis of the Framingham risk score, was obtained for all patients (pretest probability: low to moderate). Patients were excluded if they had a previous history of myocardial infarction, unstable angina, percutaneous coronary intervention (angioplasty) or coronary bypass surgery; allergy to contrast medium and renal insufficiency (serum creatinine > 1.5 mg/dL). All patients were in a stable condition at the time of the study. The study was approved by the local ethics research committee and written informed consent was obtained from all patients. The characteristics of the study population are summarised in Table 1.
Table 1. Patient demographics.
| Males | 33/ (69%) |
| Females | 15/ (31%) |
| Age (years, mean ± SD) | 61.7 (9.8) |
| Cardiovascular risk factors | |
| Smoking | 13 (27%) |
| Hypertension | 41 (83%) |
| Diabetes | 8 (17%) |
| Dyslipidemia | 13 (27%) |
| Angina pectoris | |
| Atypical | 7 (14.6) |
| Typical | 41 (85.4%) |
2.2. Coronary CT scanning protocol
All patients were scanned on a dual-source CT scanner (Somatom Definition, Siemens Medical Solutions, Forchheim, Germany). A non-enhanced scan was performed for CAC scoring. Scanning parameters were as follows: detector collimation 2 × 32 × 0.6 mm, slice collimation 2 × 64 × 0.6 mm by means of a z-flying focal spot, gantry rotation time 330 ms, pitch of 0.2–0.5 depending on the heart rate, tube current time product 350 mAs and tube potential 120 kV. CT scans were performed from the level of the tracheal bifurcation to the diaphragm. Non-enhanced CT scans were performed with prospective ECG-triggering with images acquired at three mm slice thickness.
2.3. Coronary artery calcium scoring
Coronary artery calcifications were quantified using calcium scoring software (Syngo CaScore, Siemens) and measurments were performed by a qualified CT technologist using the standard Agatston calcium scoring algorithm.[4] The extent of CAD was determined according to the recommended CT calcium score guidelines using five CAC score categories: none (0), minimal or low (1–10), mild (11–100), moderate (101–400) and extensive or high (401 or greater).
2.4. MPI-SPECT imaging protocol
Rest and stress ECG-gated MPI protocols were performed in all patients using technetium (99mTc)-tetrofosmin (500 MBq). The stress test was performed on an exercise-modified Bruce treadmill and associated (such as adenosine infusion) protocol. Images were acquired on a triple-head SPECT camera (ADAC Vertex with VXGP collimators) using a low-energy, high-resolution, parallel-hole collimator with a 360 rotation in a continuous mode. All projection images were stored in a 64 × 64 × 16 acquisition and processing frame matrix size.
2.5. MPI-SPECT image analysis
The myocardial perfusion assessment was performed by a nuclear physician with more than 10 years of experience in nuclear cardiology using a 20-segment model, and myocardial perfusion for each segment was evaluated using a five-point continuous scoring system as recommended by Xu et al.[15] (0: normal; 1: mildly abnormal; 2: moderately abnormal; 3: severely abnormal; 4: absence of segmental uptake). The observer was blinded to any clinical information and CAC scores. The segmental perfusion scores during rest and stress were added to calculate the summed rest score (SRS) and the summed stress score (SSS). The summed difference score (SDS) was calculated by subtracting the SRS from the SSS.
2.6. Statistical analysis
Data were entered into SPSS V 19.0 for analysis (SPSS, Chicago, Illinois). All continuous variables were expressed as mean ± SD. A one way analysis of variance (ANOVA) was used for analysis of continuous variables and a Pearson test was used to demonstrate the correlation between CAC and MPI scores. A P value of less than 0.05 indicated statistically significant difference.
3. Results
Table 2 lists the CAC and MPI-SPECT scores as assessed in these patients. There are variable degrees of differences between the CAC and corresponding MPI-SPECT scores. Figure 1 shows the distribution of CAC and MPI scores among these 48 patients. Forty-seven percent of the patients had moderate and extensive calcifications with CAC scores more than 100, while 42% of these patients demonstrated abnormal, or probably abnormal, MPI assessments. Analysis of the relationship between overall CAC scores and MPI assessments indicated no correlation with a Pearson correlation factor r of 0.019 (Figure 2).
Table 2. Percentages of coronary artery calcium score and MPI-SPECT results.
| CAC 0 | 23% |
| CAC 1–10 | 9% |
| CAC 11–100 | 21% |
| CAC 101–400 | 21% |
| CAC > 400 | 26% |
| Mean summed stress score | 6 (2–10) |
| Mean summed rest score | 2 (0–6) |
| Summed difference score | 4 (0–8) |
| MPI normal | 7% |
| MPI mildly abnormal | 17% |
| MPI moderately abnormal | 34% |
| MPI severe abnormal | 15% |
| MPI absence of segmental uptake | 27% |
CAC: coronary artery calcium; MPI: myocardial perfusion imaging.
Figure 1. Distribution of the CAC scores with myocardial perfusion imaging among the 48 patients with suspected coronary artery disease.
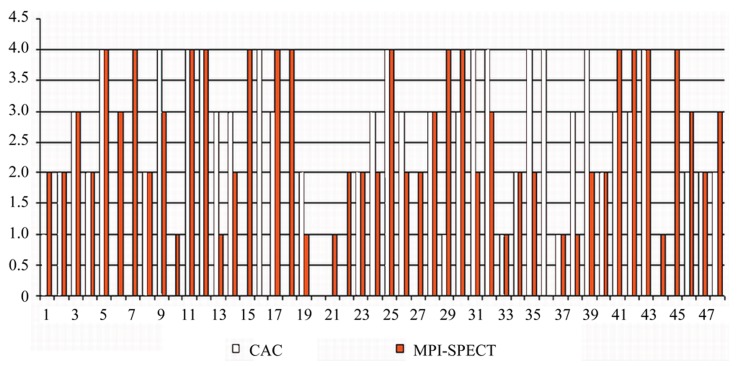
As shown in the figure, there is a significant discordance between the CAC and MPI-SPECT score, with abnormal SPECT scores (range from 1 to 4) noticed in 10 patients with a zero CAC. CAC: coronary artery calcium; MPI-SPECT: myocardial perfusion imaging with gated single photon emission computed tomography.
Figure 2. Graph shows that there is a lack of correlation between coronary artery calcium scores and the corresponding myocardial perfusion SPECT assessments, with r value of 0.019.
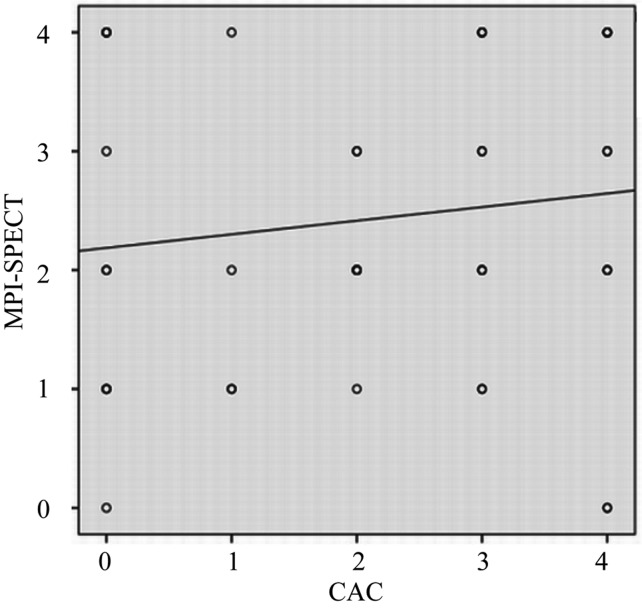
CAC: coronary artery calcium; MPI-SPECT: myocardial perfusion imaging with gated single photon emission computed tomography (SPECT).
A zero CAC score was found in 23% of the patients; however, only 7% of these were noted to demonstrate the normal MPI-SPECT results. Of 10 patients with a zero CAC score, abnormal MPI-SPECT scores were found to range from 1 to 4 (mean score 2.6). In contrast, normal MPI-SPECT scores were found in two patients with a CAC score of four. A CAC score of 1–10 was identified in 9% of the patients with probably normal MPI-SPECT findings in 17% of the patients. A CAC score of 11–100 was found in 21% of patients with equivocal MPI-SPECT findings in 34% of the patients. A CAC score of the 101–400 was reported in 21% of the patients with probably abnormal MPI-SPECT findings in 15% of these patients. Similarly, there was no correlation between the CAC scores and MPI assessments in the group of patients with low to moderate calcification, with a Pearson correlation factor r of 0.012.
Extensive calcifications (CAC score > 400) were noticed in 26% patients, while 27% of patients were found to have abnormal MPI. Again, there was no correlation between the CAC scores and MPI assessments in the group of patients with extensive calcification, with a Pearson correlation factor r of 0.080.
4. Discussion
Although based on a relatively small sample size, this study presents important findings which are considered valuable for the clinical diagnosis of patients with suspected coronary artery disease. There is a lack of correlation between the CAC scores and MPI-SPECT assessments, with a significant difference observed between these scoring techniques, especially in the patients with zero or mild calcification (CAC scores 0–100). Thus, CAC scores cannot be reliably used as single parameters to predict the disease prognosis in this group of patients.
CAC score using multi-slice CT has been validated as a useful imaging tool for risk stratification and reclassification of risk of coronary artery disease.[16] The CAC score is a highly sensitive marker with increased prognostic value for determining the atherosclerotic disease compared with conventional cardiovascular risk factors. However, issues have been raised as to whether using only a CAC score is a reliable tool of determining the extent of CAD, since non-calcified coronary artery plaque may not be detected. There is growing evidence to show the discrepancy between low CAC and corresponding myocardial perfusion findings.[8],[17],[18] This is confirmed by the results in this analysis as there is no correlation between the CAC scores and MPI assessments, whether the analysis is based on a comparison of overall CAC scores and MPI assessments, or on low or high CAC scores with corresponding MPI assessments.
Several studies have reported the presence of obstructive non-calcified plaque in 8.7% of symptomatic patients with zero or low calcium scores.[8],[17] Cheng et al.[17] reported that low, but detectable, CAC scores were less reliable in predicting the plaque burden due to their association with high overall non-calcified coronary artery plaque. Similarly, Greenland, et al.[18] demonstrated a CAC of zero did not usually eliminate the risk of future CAD events. Our results are in line with those findings. Twenty-three percent patients had a zero CAC score with only 7% of these patients verified by the myocardial perfusion SPECT to be normal. It could be concluded that low CAC scores are significantly less predictive of the prevalence, or severity, of underlying non-calcified coronary plaque,[19] although further studies based on a larger cohort of patients should be conducted.
It has been reported that the MPI-SPECT in cardiac imaging is a widely accepted test for the diagnostic and prognostic evaluation of patients with known, or suspected, CAD.[10],[20] This study indicates that MPI-SPECT may provide more accurate assessments of the extent of CAD, or the prediction of disease outcomes, than CAC alone, given that, in patients with zero CAC, some could demonstrate abnormal myocardial perfusion. Schaap, et al.[21] in their recent study concluded that a CAC score did not significantly improve the diagnostic performance of SPECT in patients with significant CAD. The association between CAC and MPI-SPECT demonstrates that as the CAC score increases, so does the occurrence and severity of myocardial perfusion abnormalities.[22],[23] High values of CAC often indicate the presence of stenotic lesions and are associated with an increased risk of adverse cardiovascular events.[16],[24],[25] Similarly, our study shows that patients with a high calcium score had abnormal, or probably abnormal, MPI-SPECT results, although the correlation between these imaging modalities was not significant. However, studies have been reported that patients with a high CAC score did not demonstrate a significantly different percentage of abnormal MPI findings than in patients with a low CAC score.[12],[14] A high CAC in patients with normal MPI-SPECT reflects non-obstructive atherosclerosis, which is regarded as a preclinical state with strong predictive value for the development of CAD, thus, aggressive risk factor modification should be recommended according to the guidelines.[26] A CAC score and MPI should be considered complementary approaches rather than individual parameters in the assessment of patients with suspected CAD.
Several limitations in this study should, however, be acknowledged. Firstly, only a limited number of patients were included in this study and further studies based on a larger cohort are needed. Secondly, this study is only a retrospective analysis of the diagnostic reports without the inclusion of follow-up details on patients, thus, there is no information available about the disease outcomes, such as major cardiac events relative to the CAC or MPI scores. Thirdly, the cut off value for CAC at 401 or greater in this study is much lower than the suggested value in the literature (> 700),[27],[28] thus, this could affect the diagnostic specificity in detecting significant CAD. Lastly, the diagnostic accuracy of coronary CT angiography was not assessed with regard to the evaluation of the degree of coronary stenosis, with no correlation to subsequent myocardial perfusion analysis, thus, no information is available about the diagnostic value in terms of sensitivity and specificity. This could be explained by the fact that the current study only focused on the correlation between CAC and MPI-SPECT. Recent evidence shows that coronary calcium scores assessed with non-enhanced CT might be supported by coronary CT angiography or coronary CT angiography might be performed alone with the aim of acquiring more diagnostic information.[29],[30] Further studies are required to investigate the potential value of coronary CT angiography for both calcium scoring and assessment of coronary stenosis.
In conclusion, this study demonstrates the lack of direct correlation between the CAC score and the corresponding myocardial perfusion assessed by SPECT in patients with suspected coronary artery disease. In particular, in patients with a zero or low CAC scores, myocardial perfusion imaging shows potential abnormalities in some patients which indicates significant lack of agreement between these two methods. This highlights the limitations in using CAC scores alone as a predictor of coronary disease outcomes. Coronary calcium score should be combined with myocardial perfusion imaging in low-to-intermediate risk patients to improve the diagnostic performance.
Acknowledgments
We would like to thank Dr Nat Lenzo for his assistance in the data collection, and are grateful to the support by staff from Envision Medical Imaging.
References
- 1.Oudkerk M, Stillman AE, Halliburton SS, et al. Coronary artery calcium screening: current status and recommendations from the European Society of Cardiac Radiology and North American Society for Cardiovascular Imaging. Int J Cardiovasc Imaging. 2008;24:645–671. doi: 10.1007/s10554-008-9319-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Greenland P, Bonow RO, Brundage BH, et al. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography) Circulation. 2007;115:402–426. doi: 10.1161/CIRCULATIONAHA..107.181425. [DOI] [PubMed] [Google Scholar]
- 3.Hoffmann U, Siebert U, Bull-Stewart A, et al. Evidence for lower variability of coronary artery calcium mineral mass measurements by multidetector computed tomography in a community based cohort—consequences for progression studies. Eur J Radiol. 2006;57:396–402. doi: 10.1016/j.ejrad.2005.12.027. [DOI] [PubMed] [Google Scholar]
- 4.Agatston AS, Janowitz WR, Hildner FJ, et al. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 5.Keelan PC, Bielak LF, Ashai K, et al. Long-term prognostic value of coronary calcification detected by electron-beam computed tomography in patients undergoing coronary angiography. Circulation. 2001;104:412–417. doi: 10.1161/hc2901.093112. [DOI] [PubMed] [Google Scholar]
- 6.Wong ND, Hsu JC, Detrano RC, et al. Coronary artery calcium evaluation by electron beam computed tomography and its relation to new cardiovascular events. Am J Cardiol. 2000;86:495–498. doi: 10.1016/s0002-9149(00)01000-6. [DOI] [PubMed] [Google Scholar]
- 7.Arad Y, Spadaro LA, Goodman K, et al. Prediction of coronary events with electron beam computed tomography. J Am Coll Cardiol. 2000;36:1253–1260. doi: 10.1016/s0735-1097(00)00872-x. [DOI] [PubMed] [Google Scholar]
- 8.Gottlieb I, Miller JM, Arbab-Zadeh A, et al. The absence of coronary calcification does not exclude obstructive coronary artery disease or the need for revascularization in patients referred for conventional coronary angiography. J Am Coll Cardiol. 2010;55:627–634. doi: 10.1016/j.jacc.2009.07.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chang SM, Nabi F, Xu J, et al. The coronary artery calcium score and stress myocardial perfusion imaging provide independent and complementary prediction of cardiac risk. J Am Coll Cardiol. 2009;54:1872–1882. doi: 10.1016/j.jacc.2009.05.071. [DOI] [PubMed] [Google Scholar]
- 10.Fallahi B, Beiki D, Gholamrezanezhad A, et al. Single Tc99m Sestamibi injection, double acquisition gated SPECT after stress and during low-dose dobutamine infusion: a new suggested protocol for evaluation of myocardial perfusion. Int J Cardiovasc Imaging. 2008;24:825–835. doi: 10.1007/s10554-008-9328-y. [DOI] [PubMed] [Google Scholar]
- 11.Elhendy A, van Domburg RT, Sozzi FB, Poldermans D, Bax JJ, Roelandt JR. Impact of hypertension on the accuracy of exercise stress myocardial perfusion imaging for the diagnosis of coronary artery disease. Heart. 2001;85:655–661. doi: 10.1136/heart.85.6.655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosman J, Shapiro M, Pandey A, VanTosh A, Bergmann SR. Lack of correlation between coronary artery calcium and myocardial perfusion imaging. J Nucl Cardiol. 2006;13:333–337. doi: 10.1016/j.nuclcard.2006.01.023. [DOI] [PubMed] [Google Scholar]
- 13.Thompson RC, McGhie AI, Moser KW, et al. Clinical utility of coronary calcium scoring after nonischemic myocardial perfusion imaging. J Nucl Cardiol. 2005;12:393–400. doi: 10.1016/j.nuclcard.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 14.Schuijf JD, Wijns W, Jukema W, et al. Relationship between noninvasive coronary angiography with multi-slice computed tomography and myocardial perfusion imaging. J Am Coll Cardiol. 2006;48:2508–2514. doi: 10.1016/j.jacc.2006.05.080. [DOI] [PubMed] [Google Scholar]
- 15.Xu Y, Fish M, Gerlach J, et al. Combined quantitative analysis of attenuation corrected and non-corrected myocardial perfusion SPECT: method development and clinical validation. J Nucl Cardiol. 2010;17:591–599. doi: 10.1007/s12350-010-9220-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Detrano R, Guerci AD, Carr JJ, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–1345. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 17.Cheng VY, Lepor NE, Madyoon H, et al. Presence and severity of noncalcified coronary plaque on 64-slice computed tomographic coronary angiography in patients with zero and low coronary artery calcium. Am J Cardiol. 2007;99:1183–1186. doi: 10.1016/j.amjcard.2006.12.026. [DOI] [PubMed] [Google Scholar]
- 18.Greenland P, Labree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004;291:210–215. doi: 10.1001/jama.291.2.210. [DOI] [PubMed] [Google Scholar]
- 19.Sun Z, Cao Y, Li H. Multislice computed tomography angiography in the diagnosis of coronary artery disease. J Geriatric Cardiol. 2011;8:104–113. doi: 10.3724/SP.J.1263.2011.00104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bateman TM, Heller GV, McGhie AI, et al. Diagnostic accuracy of rest/stress ECG-gated Rb-82 myocardial perfusion PET: comparison with ECG-gated Tc-99m sestamibi SPECT. J Nucl Cardiol. 2006;13:24–33. doi: 10.1016/j.nuclcard.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 21.Schaap J, Kauling RM, Boekholdt SM, et al. Usefulness of coronary calcium scoring to myocardial perfusion SPECT in the diagnosis of coronary artery disease in a predominantly high risk population. Int J Cardiovasc Imaging. doi: 10.1007/s10554-012-0118-1. [DOI] [PubMed] [Google Scholar]
- 22.Oudkerk M, Stillman AE, Halliburton SS, et al. Coronary artery calcium screening: current status and recommendations from the European Society of Cardiac Radiology and North American Society for Cardiovascular Imaging. Eur Radiol. 2008;18:2785–2807. doi: 10.1007/s00330-008-1095-6. [DOI] [PubMed] [Google Scholar]
- 23.Bybee KA, Lee J, Markiewicz R, et al. Diagnostic and clinical benefits of combined coronary calcium and perfusion assessment in patients undergoing PET/CT myocardial perfusion stress imaging. J Nucl Cardiol. 2010;17:188–196. doi: 10.1007/s12350-009-9159-9. [DOI] [PubMed] [Google Scholar]
- 24.Arad Y, Goodman KJ, Roth M, et al. Coronary calcification, coronary disease risk factors, C-reactive protein, and atherosclerotic cardiovascular disease events: the St. Francis Heart Study. J Am Coll Cardiol. 2005;46:158–165. doi: 10.1016/j.jacc.2005.02.088. [DOI] [PubMed] [Google Scholar]
- 25.Berman DS, Wong ND, Gransar H, et al. Relationship between stress-induced myocardial ischemia and atherosclerosis measured by coronary calcium tomography. J Am Coll Cardiol. 2004;44:923–930. doi: 10.1016/j.jacc.2004.06.042. [DOI] [PubMed] [Google Scholar]
- 26.Choudhary G, Shin V, Punjani S, et al. The role of calcium score and CT angiography in the medical management of patients with normal myocardial perfusion imaging. J Nucl Cardiol. 2010;17:45–51. doi: 10.1007/s12350-009-9158-x. [DOI] [PubMed] [Google Scholar]
- 27.Schepis T, Gaemperli O, Koepfli P, et al. Added value of coronary artery calcium score as an adjunct to gated SPECT for the evaluation of coronary artery disease in an intermediate-risk population. J Nucl Med. 2007;48:1424–1430. doi: 10.2967/jnumed.107.040758. [DOI] [PubMed] [Google Scholar]
- 28.Ghardri JR, Pazhenkottil AP, Nkoulou RN, et al. Very high coronary calcium score unmasks obstructive coronary artery disease in patients with normal SPECT MPI. Heart. 2011;97:998–1003. doi: 10.1136/hrt.2010.217281. [DOI] [PubMed] [Google Scholar]
- 29.Rubinshtein R, Gaspar T, Halon DA, et al. Prevalence and extent of obstructive coronary artery disease in patients with zero or low calcium score undergoing 64-slice cardiac multidetector computed tomography for evaluation of a chest pain syndrome. Am J Cardiol. 2007;99:472–475. doi: 10.1016/j.amjcard.2006.08.060. [DOI] [PubMed] [Google Scholar]
- 30.van Werkhoven, Shuijf JD, Gaemperli O, et al. Incremental prognostic value of multi-slice computed tomography coronary angiography over coronary artery calcium scoring in patients with suspected coronary artery disease. Eur Heart J. 2009;30:2622–2629. doi: 10.1093/eurheartj/ehp272. [DOI] [PubMed] [Google Scholar]


