Abstract
Objective
To assess the secular trends in the etiology and comorbidity of patients hospitalized with congestive heart failure (CHF).
Methods
Data of 7,319 patients (mean age 59.6 years, 62.1% male) with a primary discharge diagnosis of CHF, hospitalized from January 1, 1993 to December 31, 2007 at the Chinese People's Liberation Army (PLA) General Hospital were extracted and analyzed. These patients were divided into three groups according to hospitalization period: 1993–1997 (n = 1623), 1998–2002 (n = 2444), and 2003–2007 (n = 3252). The etiological characteristics and comorbidities were assessed.
Results
Over the study period, the proportion of patients with ischemic heart disease (IHD) increased from 37.2% during the period 1993–1997 to 46.8% during the period 2003–2007, while that with valvular heart disease (VHD) decreased from 35.2% during the period 1993–1997 to 16.6% during the period 2003–2007 (both P < 0.05). Atrial fibrillation (AF) was the most common comorbidity of heart failure (23.2%, 23.0% and 20.6%, respectively, in the three periods). Compared to that of the period of 1993–1997 with that of, the proportion of patients with myocardial infarction, pneumonia, renal function impairment and hepatic cirrhosis of the period of 2003–2007 increased significantly (P < 0.05) and the proportion of patients with chronic obstructive pulmonary disease and atrial fibrillation decreased significantly (P < 0.05).
Conclusions
This study implies that IHD has became a more common etiology of CHF, while VHD has deceased as an etiology of CHF in Chinese patients during the last two decades.
Keywords: Atrial fibrillation, Congestive heart failure, Comorbidity, Etiology, Hospitalization
1. Introduction
Congestive heart failure (CHF) is the final result of many diseases affecting the heart.[1],[2] As the population is ageing, and with an increasing number of individuals now surviving myocardial infarction (MI), the prevalence of CHF is increasing.[1]–[3] The etiological characteristics, drug therapy, and prognosis of patients with CHF have been well described by a number of community-based and hospital-based registries as well as by clinical trials of CHF treatment.[4]–[11] However, such studies have been performed mainly in industrialized countries, and the results may not be directly translatable from one country to another with different population and healthcare system due to variations of population and different qualities of care, which may be important cofactors in the interactions among disease severity and outcome.[12] Furthermore, race is an important determinant of certain clinical outcomes in cardiovascular diseases.[13],[14] Since very little information is available on the etiological characterristics and prognosis of patients with CHF in China, further studies are required to see if the results reported in Industrialized countries are applicable to the Chinese population. The aim of this study is to evaluate the etiological characterristics and the prevalence of comorbidities in Chinese patients hospitalized with CHF.
2. Methods
2.1. Patient selection and data analysis
The data were retrieved from the hospital administrative databases of the Chinese People's Liberation Army (PLA) General Hospital, Beijing. The patients chosen for the study are identified by screening of the database for International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) principal discharge diagnoses of CHF (ICD-9-CM codes 428, 428.1 and 428.9).[15] All 7,319 patients (4,543 males, 2,776 females) in the database with a principal ICD-9-CM discharge diagnosis of CHF who were admitted to the hospital from January 1, 1993 to December 31, 2007 were identified. Sixteen comorbidity variables (ischemic heart disease, hypertension, valvular heart disease, diabetes mellitus, pulmonary heart disease, cardiomyopathy, congenital heart disease, anemia, atrial fibrillation (AF), myocardial infarction (MI), pneumonia, chronic obstructive pulmonary disease (COPD), gastrointestinal bleeding, cerebrovascular disease, impaired renal function, and hepatic cirrhosis) were identified using an ICD-9-CM discharge diagnosis coding scheme. In evaluation of trends in hospital outcomes for CHF throughout the 15-year study period, analysis were performed in 5-year intervals: from January 1, 1993 to December 31, 1997; from January 1, 1998 to December 31, 2002; and from January 1, 2003 to 2007, 31. Comparative analysis was performed to explore the etiology and comorbidities of CHF in each group.
2.2. Etiology definition
We attempted to determine the etiology of CHF from the clinical and laboratory data in the medical records. History of coronary revascularization, electrocardiographic evidence of MI, or self-reported history of MI or angina accompanied by antianginal medication use was considered definite evidence of ischemic heart disease. Hypertensive heart disease was established by medical documentation of long-lasting hypertension and concentric left ventricular hypertrophy in which the left ventricle (LV) wall thickness in the interventricular septum and/or posterior wall was more than 11 mm. Diabetes mellitus was considered present if the participant reported a history of diabetes or use of anti-diabetic medications. Valvular heart disease was determined mainly by the past history (rheumatic fever and/or the long-lasting heart murmur), physical examination, and echocardiographic findings of mitral and/or aortic valve disorders; Valvular heart disease also included patients who had undergone surgical repair. Congenital heart diseases were diagnosed by echocardiography and/or a cardiac catheterization; Congenital heart diseases also included patients who had undergone surgical repair. The criteria for cardiomyopathy comprised the absence of signs of ischemic, valvular or congenital or hypertensive heart disease and in the absence of a known cardiac or systemic cause. The diagnosis of AF was based on a 12-lead standard electrocardiogram performed at the time of admission. The diagnosis of pneumonia was based on clinical presentation, chest X-ray and lab test. Cerebrovascular disease was based on a history of stroke, transient ischemic attack, or carotid intervention. Impaired renal function was defined as an estimated glomerular filtration rate (eGFR) < 60 mL/min per 1.73 m2 body surface area.[16] Anemia was defined as a hemoglobin level ≤ 12 g/dL for women and ≤ 13 g/dL for men, throughout hospitalization. The history of pulmonary heart disease, hyperthyroidism, COPD, hematonosis, cirrhosis, cancer, and gastrointestinal bleeding was recorded if documented by the physician in the admitting notes, and if the clinical diagnoses and criteria conformed to the World Health Organization (WHO) standard.
2.3. Statistics
Continuous variables were provided as means ± SD and categorical variables were shown as percentages. Categorical variables were compared using the χ2 test, and the continuous variables were compared among the three groups using ANOVA test. Analyses were done with SSPS 16.0 software (SPSS, Inc., Chicago, IL, USA).
3. Results
3.1. Demographics of patients
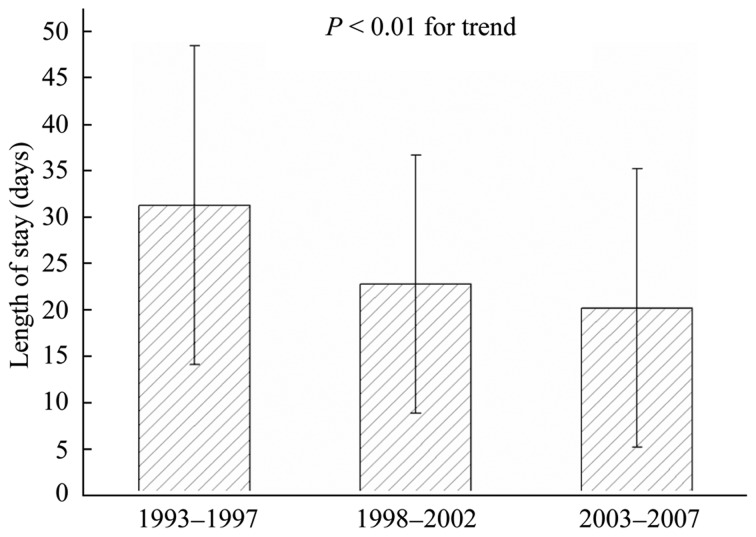
During the study period, a total of 7,319 hospital admissions occurred at the Chinese PLA General Hospital according to the ICD-9-CM codes for CHF, and 4,543 (62.1%) of which were male. The mean age for the study population was 59.6 ± 16.9 years; the mean age for male and female was 61.4 ± 16.3 years and 56.6 ± 17.4 years, respectively. The mean age for hospitalized patients during the three periods respective was 56.0 ± 17.5 years, 57.8 ± 17.6 years and 62.7 ± 15.5 years, which presented an upward trend (P < 0.01) (Figure 1). The average length of hospitalization for the three respective periods were 31.3 ± 17.4 days, 22.7 ± 14.1 days and 20.1 ± 15.2 days, which presented a downward trend (P < 0.01) (Figure 2).
Figure 1. The trend of the mean age of hospitalized patients with congestive heart failure in three different periods.
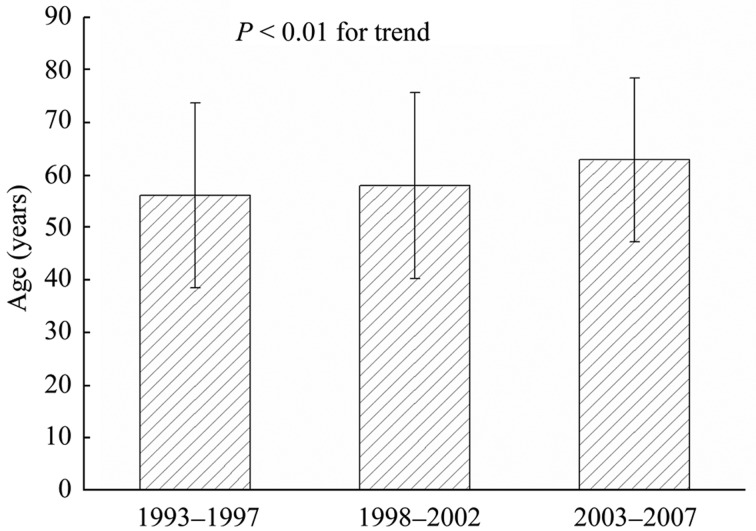
Figure 2. The trend of the average length of stay in hospital by patients with congestive heart failure in three different periods.
3.2. Etiology and comorbidities
The major etiology of CHF in the entire 15 years, were ischemic heart disease (42.7%), hypertension (36.7%), valvular heart disease (26.1%) and diabetes mellitus (17.4%). The proportion of patients with ischemic heart disease, hypertension and diabetes mellitus increased respectively from 37.2%, 23.3% and 12.3 % during 1993–1998 to 46.8%, 46.7% and 21.1% during 2003–2007 (P < 0.05). Meanwhile, the proportion of patients with valvular heart disease decreased from 35.2% during 1993–1998 to 16.6% during 2003–2007 (P < 0.05). Among the minor etiology, the proportion of pulmonary heart disease and congenital heart disease showed a down-ward trend during the three periods (9.7%, 10.1% and 8.1%; 5.9%, 3.0% and 1.6%, respectively) (P < 0.05), and cardiomyopathy and anemia presented a upward trend (6.7%, 5.7% and 8.2%; 2.7%, 1.8% and 4.8%, respectively) (P < 0.01) (Table 1).
Table 1. Etiology and comorbidites reported in patients primarily hospitalized for CHF according to the year of admission.
| Overall (n = 7319) | 1993–1997 (n = 1623) | 1998–2002 (n = 2444) | 2003–2007 (n = 3252) | P value | |
| Etiology | |||||
| Ischemic heart disease | 3125 (42.7) | 604 (37.2) | 999 (40.9) | 1522 (46.8)#* | < 0.001 |
| Hypertension | 2687 (36.7) | 378 (23.3) | 790 (32.3)† | 1519 (46.7)#* | < 0.001 |
| Valvular heart disease | 1912 (26.1) | 572 (35.2) | 799 (32.7) | 541 (16.6)#* | < 0.001 |
| Diabetes mellitus | 1275 (17.4) | 199 (12.3) | 389 (15.9)† | 687 (21.1)#* | < 0.001 |
| Pulmonary heart disease | 667 (9.1) | 157(9.7) | 247(10.1) | 263 (8.1)* | 0.022 |
| Cardiomyopathya | 515 (7.0) | 109 (6.7) | 140 (5.7) | 266 (8.2)* | 0.001 |
| Anemia | 243 (3.3) | 43 (2.7) | 43 (1.8) | 157 (4.8)#* | < 0.001 |
| Congenital heart diseaseb | 220 (3.0) | 96 (5.9) | 72 (3.0)† | 52 (1.6)#* | < 0.001 |
| Comorbidities | |||||
| Atrial fibrillation | 1610 (22.0) | 377 (23.2) | 562 (23.0) | 671 (20.6) | 0.041 |
| Myocardial infarction | 893 (12.2) | 179 (11.0) | 235 (9.6) | 479 (14.7)#* | < 0.001 |
| Pneumonia | 809 (11.1) | 145 (8.9) | 192 (7.9) | 472 (14.5)#* | < 0.001 |
| COPD | 688 (9.4) | 210 (12.9) | 206 (8.4)† | 272 (8.4)# | < 0.001 |
| Renal function impairment | 496 (6.8) | 84 (5.2) | 115 (4.7) | 297 (9.1)#* | < 0.001 |
| Cerebrovascular disease | 225 (3.1) | 45 (2.8) | 56 (2.3) | 124 (3.8)* | 0.003 |
| Hepatic cirrhosis | 141 (1.9) | 22 (1.4) | 42 (1.7) | 77 (2.4)# | 0.035 |
| Gastrointestinal bleeding | 76 (1.0) | 12 (0.7) | 21 (0.9) | 43 (1.3) | 0.094 |
Data are expressed as number (percentage) of patients. *P < 0.05 compared with 1998–2002 group; #P < 0.05 compared with 1993–1997 group; †P < 0.05 compared with 1993–1997 group; aExcludes cardiomyopathy complicating: pregnancy, puerperium, and ischemic cardiomyopathy; bCongenital malformation of cardiac septa: including atrial septal defect, ventricular septal defect, and tetralogy of Fallot. COPD: chronic obstructive pulmonary disease.
The percentages of CHF comorbidities of all patients were as follows: AF (22.0%), MI (12.2%), pneumonia (11.1%), COPD (9.4%), renal function impairment (6.8%), cerebrovascular disease (3.1%), hepatic cirrhosis (1.9%) and gastrointestinal bleeding (1.0%). Comparing the period of 1993– 1997 with that of 2003–2007, the proportion of patients with MI, pneumonia, renal function impairment and hepatic cirrhosis increased significantly (P < 0.05). However, the proportion of patients with COPD and AF decreased significantly (P < 0.05) (Table 1).
4. Discussion
This study has a number of important strengths. Not only does it describe the etiological characteristics of heart failure over the last 15 years, but also describes the comorbidities in patients primarily hospitalized for CHF based on their admission history.
A number of community-based and hospital-based study have shown that ischemic heart disease has become the most important cause of CHF in Western population.[4]–[11] About 42.7% of the CHF cases in our study population were attributed to ischemic heart disease, which is very close to that found in EPICAL study (46.3% attributed to ischemic heart disease).[17] In a hospital-based study done in Fukuoka, Japan, ischemic heart disease was the underlying cause of CHF in 45% of patients.[18] Our study also found that hypertension and diabetes mellitus were common causes of heart failure (about 36.7% and 17.4%, respectively), but were much lower than the corresponding findings in Western populations (about 60%–70% and 22%–44%, respectively).[19],[20] However, valvular heart disease was very common in our study (about 35.2%, 32.7% and 16.6% in three periods, respectively). Prevalence of rheumatic valvular heart disease in China was much higher than that in Western populations.[20] Multivariate analysis of results from a populationbased study has shown that rheumatic valvular heart disease is one of the risk factors for development of AF in developing countries.[21] Other Chinese investigations found that the causes of CHF had shifted from valvular disease to ischemic heart disease during the past two decades. Valvular disease had fallen from 46.8% to 8.9% (an average of 28%, which is similar to the present study), whereas ischemic heart disease had increased from 31.1% to 55.7%.[22],[23] Pulmonary heart disease and anemia also occurred at a much higher prevalence than in Western populations. Differences between developed and developing countries, patient selection and/or racial variation may explain these results.
In the present study, we found that comorbidities were common in patients with CHF and showed an upward trend during the study period (Table 1). The most common precipitating factor of CHF was AF. In the previous studies, the prevalence of AF in patients with CHF has been reported to be 30%–50%,[24],[25] but we found AF in 22.0% of total cases, which is relatively lower than that in Western populations. However, the prevalence of AF increasing with age is consistent with Western populations and similar to the results of another study in China.[26] In addition, AF and CHF are interrelated conditions, each promoting the other, and both associated with increased mortality. CHF leads to structural and electrical atrial remodeling, thus creating the basis for the development and perpetuation of AF; and AF may lead to hemodynamic deterioration and the develop ment of tachycardia mediated cardiomyopathy. MI, pneumonia and COPD were the predominantly precipitating factors. It is commonly recognized that elderly patients with MI, pneumonia and COPD often develop CHF. Renal function impairment was the most frequent coexisting comorbidity in this study. In a meta-analysis of 16 studies, Smith et al.[27] found that 63% of 80,098 patients with CHF had some degree of concomitant impaired renal function, and 29% presented with severe renal failure. Worsening renal function is strongly independent of general mortality in patients with CHF.[28]
The present study has the inherent limitations of a retrospective cohort design. Some methodological limitations of this study should be acknowledged. With the data collected retrospectively from a hospital-wide administrative data set, the study includes only patients discharged with principal ICD-9-CM diagnoses reflective of relatively uncomplicated CHF. Thus, our study results may not be inclusive of patients with other heart failure-related principal ICD-9-CM diagnoses. In addition, patients with CHF are identified from medical records, so the incidence of CHF might have been underestimated. Therefore, some patients might have been excluded because the information in clinical records did not fulfill the diagnostic criteria. As a result of inadequate clinical information pertaining to functional capacity, physical examination findings and laboratory results, medication and disease severity may not be fully captured in hospital administrative data sets.
In summary, our study indicates that the major cause of CHF in China populations is different from that in Western populations and the proportion of comorbidities in patients with CHF increased over the study period.
References
- 1.Jessup M, Brozena S. Heart failure. N Engl J Med. 2003;348:2007–2018. doi: 10.1056/NEJMra021498. [DOI] [PubMed] [Google Scholar]
- 2.Huynh BC, Rovner A, Rich MW. Long-term survival in elderly patients hospitalized for heart failure: 14-year follow-up from a prospective randomized trial. Arch Intern Med. 2006;166:1892–1898. doi: 10.1001/archinte.166.17.1892. [DOI] [PubMed] [Google Scholar]
- 3.Massie BM, Shah NB. Evolving trends in the epidemiologic factors of heart failure: rationale for preventive strategies and comprehensive disease management. Am Heart J. 1997;33:703–712. doi: 10.1016/s0002-8703(97)70173-x. [DOI] [PubMed] [Google Scholar]
- 4.Levy D, Kenchaiah S, Larson MG, et al. Long-term trends in the incidence of and survival with heart failure. N Engl J Med. 2002;347:1397–1402. doi: 10.1056/NEJMoa020265. [DOI] [PubMed] [Google Scholar]
- 5.Tsutsui H, Tsuchihashi-Makaya M, Kinugawa S, et al. JCARE-GENERAL Investigators. Characteristics and outcomes of patients with heart failure in general practices and hospitals. Circ J. 2007;71:449–454. doi: 10.1253/circj.71.449. [DOI] [PubMed] [Google Scholar]
- 6.Cohen-Solal A, Desnos M, Delahaye F, et al. A national survey of heart failure in French hospitals. Eur Heart J. 2000;21:763–769. doi: 10.1053/euhj.1999.1762. [DOI] [PubMed] [Google Scholar]
- 7.Koseki Y, Watanabe J, Shinozaki T, et al. Characteristics and 1-year prognosis of medically treated patients with chronic heart failure in Japan. Circ J. 2003;67:431–436. doi: 10.1253/circj.67.431. [DOI] [PubMed] [Google Scholar]
- 8.Pulignano G, Del Sindaco D, Tavazzi L, et al. Clinical features and outcomes of elderly outpatients with heart failure followed up in hospital cardiology units: Data from a large nationwide cardiology database (IN-CHF Registry) Am Heart J. 2002;143:45–55. doi: 10.1067/mhj.2002.119608. [DOI] [PubMed] [Google Scholar]
- 9.Mosterd A, Cost B, Hoes AW, et al. The prognosis of heart failure in the general population: The Rotterdam Study. Eur Heart J. 2001;22:1318–1327. doi: 10.1053/euhj.2000.2533. [DOI] [PubMed] [Google Scholar]
- 10.Goldberg RJ, Ciampa J, Lessard D, et al. Long-term survival after heart failure: a contemporary population-based perspective. Arch Intern Med. 2007;167:490–496. doi: 10.1001/archinte.167.5.490. [DOI] [PubMed] [Google Scholar]
- 11.Cowie MR, Wood DA, Coats AJ, et al. Survival of patients with a new diagnosis of heart failure: a population based study. Heart. 2000;83:505–510. doi: 10.1136/heart.83.5.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ko DT, Tu JV, Masoudi FA, et al. Quality of care and outcomes of older patients with heart failure hospitalized in the United States and Canada. Arch Intern Med. 2005;165:2486–2492. doi: 10.1001/archinte.165.21.2486. [DOI] [PubMed] [Google Scholar]
- 13.Deswal A, Petersen NJ, Urbauer DL, et al. Racial variations in quality of care and outcomes in an ambulatory heart failure cohort. Am Heart J. 2006;152:348–354. doi: 10.1016/j.ahj.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 14.Newton JD, Blackledge HM, Squire IB. Ethnicity and variation in prognosis for patients newly hospitalised for heart failure: a matched historical cohort study. Heart. 2005;91:1545–1550. doi: 10.1136/hrt.2004.057935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Washington, D.C.: Public Health Service, U.S. Department of Health and Human Services; 1988. International Classification of Diseases, Ninth Revision, Clinical Modification. [Google Scholar]
- 16.Folsom AR, Yamagishi K, Hozawa A, et al. Absolute and attributable risks of heart failure incidence in relation to optimal risk factors. Circ Heart Fail. 2009;2:11–17. doi: 10.1161/CIRCHEARTFAILURE.108.794933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zannad F, Briancon S, Juilliere Y, et al. Incidence, clinical and etiologic features, and outcomes of advanced chronic heart failure: the EPICAL Study. Epidémiologie de l'Insuffisance Cardiaque Avancée en Lorraine. J Am Coll Cardiol. 1999;33:734–742. doi: 10.1016/s0735-1097(98)00634-2. [DOI] [PubMed] [Google Scholar]
- 18.Tsuchihashi M, Tsutsui H, Kodama K, et al. Clinical characteristics and prognosis of hospitalized patients with congestive heart--a study in Fukuoka, Japan. Jpn Circ J. 2000;64:953–959. doi: 10.1253/jcj.64.953. [DOI] [PubMed] [Google Scholar]
- 19.Adams KF, Jr, Fonarow GC, Emerman CL, et al. Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the acute decompensated heart failure national registry (ADHERE) Am Heart J. 2005;149:209–216. doi: 10.1016/j.ahj.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 20.Goda A, Yamashita T, Suzuki S, et al. Prevalence and prognosis of patients with heart failure in Tokyo: a prospective cohort of Shinken Database 2004–5. Int Heart J. 2009;50:609–625. doi: 10.1536/ihj.50.609. [DOI] [PubMed] [Google Scholar]
- 21.Vora A. Management of atrial fibrillation in rheumatic valvular heart disease. Curr Opin Cardiol. 2006;21:47–50. doi: 10.1097/01.hco.0000198985.78508.55. [DOI] [PubMed] [Google Scholar]
- 22.Cao YM, Hu DY, Wu Y, et al. A pilot survey of the main causes of chronic heart failure in patients treated in primary hospitals in China. Zhonghua Nei Ke Za Zhi. 2005;44:487–489. [PubMed] [Google Scholar]
- 23.Shanghai Investigation Group of Heart Failure , compiler. The evolving trends in the epidemiologic factors and treatment of hospitalized patients with congestive heart failure in Shanghai during the years of 1980, 1990 and 2000. Zhonghua Xin Xue Guan Bing Za Zhi. 2002;30:24–26. [Google Scholar]
- 24.Swedberg K, Olsson LG, Charlesworth A, et al. Prognostic relevance of atrial fibrillation in patients with chronic heart failure on long-term treatment with betablockers: Results from COMET. Eur Heart J. 2005;26:1303–1308. doi: 10.1093/eurheartj/ehi166. [DOI] [PubMed] [Google Scholar]
- 25.Rusinaru D, Leborgne L, Peltier M, et al. Effect of atrial fibrillation on long-term survival in patients hospitalised for heart failure with preserved ejection fraction. Eur J Heart Fail. 2008;10:566–572. doi: 10.1016/j.ejheart.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 26.Yang JF, Liu B, Liu DG, et al. Prevalence and risk factors of atrial fibrillation in preterminal inpatients aged 60 years and over. Chin Med J (Engl) 2008;121:2046–2049. [PubMed] [Google Scholar]
- 27.Smith GL, Lichtman JH, Bracken MB, et al. Renal impairment and outcomes in heart failure. J Am Coll Cardiol. 2006;47:1987–1996. doi: 10.1016/j.jacc.2005.11.084. [DOI] [PubMed] [Google Scholar]
- 28.Sarraf M, Masoumi A, Schrier RW. Cardiorenal syndrome in acute decompensated heart failure. Clin J Am Soc Nephrol. 2009;4:2013–2026. doi: 10.2215/CJN.03150509. [DOI] [PubMed] [Google Scholar]


