Abstract
Material and method:
Using the survey data obtained from doctors in Connecticut, we estimate the “true” costs of defensive medicine and medical malpractice awards via litigation in the overall aggregate picture of U.S. national annual health expenditures.
Results and discusion:
Progressives claim that these costs amount only to approximately 2% of total annual health expenditures, while conservatives claim that these costs are much higher, in the neighborhood of 10%. Conservatives want to reform the current medical malpractice system because the savings could be significant. Progressives claim that this issue is a “red herring” in the overall picture of health care reform and that other factors such as hospital costs, payments to physicians and pharmaceutical prices are the largest contributors to runaway health care costs, currently amounting to 18% of GDP. The health of the national economy, deficit reduction and future prosperity will depend upon the speed and quality of the cost reducing solutions.
Conclusion:
An in-depth look into cost and profit structure of each provider’s procedure and legislative push for price and quality transparency of the informed and educated constituents are recommended to improve this serious national, socio-economic problem.
Key words: Medical malpractice, defansive medicine.
1. INTRODUCTION
Healthcare reform is one of the most contentious public policy issues in the United States. The United States spends over $2.5 trillion every year on healthcare expenditures. This translates into 18% of GDP or over $ 8,000.00 per person. As a comparison, Japan spends approximately 9% of its gross domestic product and Germany spends 11% of GDP on health outlays. Almost 50 million Americans have no health insurance. An estimated 100 million additional Americans are underinsured. Should they encounter a serious illness for a prolonged period of time these individuals will likely be forced into bankruptcy. An estimated 18,000 Americans die each year as a direct result of not having health insurance coverage. United States of America is ranked 37th in health outcomes among industrialized countries despite spending the largest sum per capita of any nation on medical care. The U.S. performs particularly poorly in categories such as infant mortality and life expectancy. On average a Japanese or Swedish citizen lives four years longer than a US citizen.
Over the past century several attempts have been made by the federal government to reform and improve the American healthcare system. Finally in 2003, President George W. Bush signed into law a prescription drug program for seniors known as Medicare part D, that was designed to help seniors fund their considerable expenditures on prescription drugs.
Conservatives have long argued that medical malpractice laws should be fundamentally reformed in order to control escalating health care costs. In state civil justice systems that lack reasonable limits on liability, multi-million dollar jury awards and settlements in medical liability cases have forced many insurance companies to either leave the market or substantially raise costs. Increasingly, physicians in these states are choosing to stop practicing medicine, abandon high-risk parts of their practices, or move their practices to other states.
Progressives further allege that we do not have a medical malpractice crisis but an epidemic of medical errors. According to the Institute of Medicine report published in 2000, as many as 98,000 Americans die each year because of preventable medical errors. Other research reports indicate that this figure could be as high as 200,000 deaths annually because of mistakes in hospitals, doctors‘ offices and other health care facilities.
In 2009, President Barack Obama introduced a comprehensive healthcare reform bill and signed it into law in March 2010. The Affordable Care Act extends coverage to additional 32 million Americans and introduces various other reform measures. The 2010 Affordable Care Act mandates that $.80 of every dollar be spent on medical expenditures (as opposed to insurance company profits), thereby transforming the private insurance companies into highly regulated institutions. President Barack Obama included $250 million of grants in the 2010 healthcare reform bill to further study medical malpractice reform at the state level.
In 2008, the Congressional Budget Office estimated that by the year 2082 the entire federal budget will be spent on health care costs if the current growth rate of healthcare expenditures continues at the present course. Clearly, this will not happen. Compensation of doctors, especially specialists, will be under considerable scrutiny in the future. Payments to hospitals both from the Medicare program and from private insurance companies will be revisited. Prices of pharmaceuticals, especially of brand drugs, will attract additional attention from policymakers and the public.
In this academic article, doctors in the state of Connecticut have been surveyed and interviewed in order to attain quantitative and qualitative information regarding the topic of medical malpractice reform and the prevalence of defensive medicine. This research should shed a new light on this important topic of public policy, both at the state and federal level.
Theory of Tort Law
Cooter and Ulen (2004) define the tort law, economically, as the attempt to make injurers internalize the externalities they cause, in situations where transaction costs are too high to do this through property or contract rights. The traditional theory of tort liability was developed at the turn of the 20th century. It specified three elements of a tort that must be present for the plaintiff to recover damages:
harm
causation
breach of duty
There is some harm that cannot be undone – an amputated leg, for example, or other permanent injury— but there may be some amount of money that would compensate for it. American courts have traditionally been willing to compensate victims for tangible losses – (e.g. medical costs, lost income), but less willing to compensate for intangible losses or losses that are difficult to measure, such as emotional harm, pain and suffering, or loss of companionship. Over the years, however, American courts in particular have expanded the list of compensable harms to include many of the above mentioned intangibles.
According to the National Commission on Fiscal Responsibility and Reform (—the Bowles–Simpson report—) most experts agree that the current tort system in the United States leads to an increase in health care costs. The Commission recommends an aggressive set of reforms to the tort system. Among the policies pursued, the following should be included:
Modifying the -collateral source rule to allow outside sources of income collected as a result of an injury (for example, workers‘ compensation benefits or insurance benefits) to be considered in deciding awards;
Imposing a statute of limitations – perhaps one to three years – on medical malpractice lawsuits;
Replacing joint-and-several liability with a fair-share rule, under which a defendant in a lawsuit would be liable only for the percentage of the final award that was equal to his or her share of responsibility for the injury;
Creating specialized - health courts for medical malpractice lawsuits; and
Allowing - safe haven rules for providers who follow - best practices of care. Many experts also believe that statutory caps on punitive and non-economic damages should be imposed.
CBO finds that even if the country enacted the entire menu of tort restrictions listed, it can go no farther than to find a small percentage of health care savings, -about 0.5% or $11 billion a year at the current level–far lower than advocates have estimated.
2. LITERATURE REVIEW
Medical malpractice and defensive medicine have been major issues since the 1970s. In recent years medical malpractice became a national political issue with the publication of the IOM report of the Institute of Medicine (Kohn, Corrigan, & Donaldson, 1999). The Studdert et al. (2005) study utilized a survey methodology and showed that it was not unusual for physicians to make treatment decisions largely to avoid legal liability as opposed to medical reasons. The Kessler and McClellan (1997) study used econometrics that compared the cost of treatment of Medicare patients in different states and reported results that were consistent with the results of the Studdert et al. study. Gaba (2000) reported on how anesthesiologists successfully had addressed safety issues and had been rewarded with lower rates for malpractice insurance. Gallagher, Waterman, Ebers, Fraser, and Levinson (2003) reported that physicians and patients have differing views as to the desirability of reporting treatment errors to the affected patient.
Many practitioners were surprised when the report was issued, since many of the safety practices that they had been struggling to enact were not included in the list of 11 suggestions. Only 3 of the 11 measures—, anti-coagulation for prevention of deep venous thrombosis, antibiotic prophylaxis to prevent surgical infections and use of pressure relieving materials to reduce ulcers—, are traditionally recognized as safety issues (Leape et al., 2002).
McDonald, Winer, and Hui (2000) found that the Institute of Medicine‘s report on the large number of deaths due to medical errors contained a number of limitations that were not disclosed in the report, so that the numbers reported should be interpreted with caution. McDonald et al. agreed with sections of the report that advocated research into the causes of medical error and what steps could be enacted to reduce medical error.
The Harvard Medical Practice Study provided much of the support for the report of the Institute of Medicine. Thirty-five percent of physicians and 42% of the public reported that they or a member of their family had experienced a medical error. Surprisingly, neither the physicians nor the lay group viewed medical errors as the most important issue in health care (Blendon et al., 2002). Physicians felt that the high cost of malpractice insurance was the most important issue, while the public viewed the high cost of treatment as the most important problem in healthcare.
The Studdert et al. (2005) study of Pennsylvania physicians is a significant contribution to the literature of defensive medicine due to its large sample and high response rate. This study consisted of a mail survey of physicians in six specialties at a high risk of litigation (emergency room, general surgery, orthopedic surgery, neurosurgery, obstetrics/gynecology, and radiology) in Pennsylvania in May 2003. The main outcome measure was the number of physicians, in each specialty reporting defensive medicine or changes in the scope of practice and characteristics of defensive medicine (assurance and avoidance behavior). The results of the study indicated that 824 physicians (65%) completed the survey, with nearly all (93%) reporting practicing defensive medicine. Assurance behavior ,such as ordering tests, performing diagnostic procedures, and referring patients for consultation was very common (92%). Among practitioners of defensive medicine who detailed their most recent defensive act, 43% reported using imaging technology in clinically unnecessary circumstances. Forty-two percent of respondents reported that they had taken steps to restrict their practice in the previous 3 years, including eliminating procedures prone to complications, such as trauma surgery, and avoiding patients with complex medical problems or who were perceived as litigious (Studdert et al., 2005). The Studdert et al. (2005) study found that defensive medicine was highly prevalent among physicians in Pennsylvania who paid the most for liability insurance, with potentially serious implications for cost, access, and both technical and interpersonal quality of care. Studdert et al. (2005) found that 93% of respondents reported that they sometimes or often engaged in at least one of the six forms of defensive medicine outlined in the survey, and 82% of those who reported practicing defensive medicine detailed their most recent act. The Studdert et al. study examined adverse events that occurred to hospitalized patients and discovered that approximately onethird of these events were unpreventable. Therefore, the remaining two-thirds of adverse events were, in a sense, preventable (Leape et al., 2002).
3. METHODS
According to Brennan et al. (2006) measurement of defensive medicine poses several daunting challenges for researchers. Distinctions between inappropriate and appropriate clinical practice are unclear in many clinical situations. It can be difficult to disentangle liability motivations from the manifold factors that influence clinical decision-making. This approach has the advantage of being able to sidestep the trickiest methodological challenges, namely, the dual questions of what constitutes and what motivates inappropriate care. Respondents themselves are called upon to make these determinations by reflecting on their own clinical decision-making. I selected a cluster of specialties at the high end of the liability risk spectrum in a state that has been impacted by the latest medical malpractice crisis.
The main limitation of all survey research in this area is response bias. Findings were based on what doctors had indicated. Survey was developed and fielded in association with Griffin Hospital (Derby, CT.) and Yale-New Haven Hospital. A stratified random sample was made of 100 physicians in various specialties (emergency medicine, general surgery, neurosurgery, obstetrics/gynecology, orthopedic surgery, radiology etc.). Among these were specialists who paid the most for liability insurance in the last several years and they also saw the most dramatic hikes in premiums. Sampling was proportionate by specialty, except that gynecologists were oversampled to ensure adequate representation. The survey instrument was a ten page questionnaire using topics and response categories suggested by the key informant interviews. The questionnaire was pretested on ten (10) Connecticut physicians in the target specialties who were debriefed and cognitive interviews focusing on comprehension and appropriateness of question topics, wording, response options, and layout. After revision, the questionnaire contained 45 questions. The survey was mailed in February and March 2011, along with a cover letter and a consent form. The adjusted response rate after exclusion of five non-eligible physicians was 33%, which is considered good in a survey of physicians. The data were analyzed using the SPSS version 17.0 statistical software package with appropriate corrections for the survey design. Subgroup comparisons were made using Pearson Chi- square analysis.
3.1. Hypotheses
H01: Defensive medicine remains prevalent in Connecticut after tort reforms have been enacted.
HA1: Defensive medicine is no longer prevalent in Connecticut after tort reforms have been enacted.
H01: The cost of defensive medicine with respect to aggregate health care expenditures is less than 5 %.
HA1: The cost of defensive medicine with respect to aggregate health care expenditures is more than 5 %.
H01: Connecticut doctors favor proposed alternative dispute resolution mechanisms
HA1: Connecticut doctors do not favor proposed alternative dispute resolution mechanisms
3.2. Research Design
The current quantitative study was a continuation of the previous findings of the Studdert et al. (2005) study. The current study utilized a survey instrument similar to the one used in the Studdert et al. study in order to determine if defensive medicine is equally as extensive in a different geographic location at a later point in time. The purpose of the current study was to determine if physicians located in Connecticut engaged in defensive medicine to the same degree as previously reported in a study of Pennsylvania physicians. The Pennsylvania research strongly suggested that physicians frequently engaged in and refrained from actions primarily for defensive reasons, rather than for the patient‘s welfare. Defensive medicine may represent wasted resources, and obtaining a reliable estimate as to the size and nature of defensive medicine is an important part of the public policy debate concerning medical malpractice reform and malpractice caps.
3.3. Sampling Design
The current study used a survey methodology to obtain evidence as to the prevalence of defensive medicine among licensed physicians in Connecticut. The study approached the issue of the prevalence of defensive medicine from the epistemological viewpoint that some level of defensive medicine was present in the target population and that level could be estimated with a certain confidence interval, assuming the underlying assumptions of the study are correct.
3.4. Data Procedures, Methodology Restrictions and Ethical Implications
Surveys were mailed to licensed physicians in a portion of Connecticut, along with a letter that explained the purpose of the survey. The data was processed using SPSS computer software on researcher‘s personal computer. The design of the current study had several limitations. One primary limitation was that the survey asked physicians questions regarding their medical practice; the predictive power of the survey depended on how truthful the physicians were in responding. The second limitation to the study was that the Studdert et al. (2005) study was limited to high-risk specialties, while the current study had no such limitation. The third limitation was that the population in Connecticut probably has an older average age that might affect the willingness of physicians to take risk.
All participants for this study volunteered, and no personal identifying or confidential information was collected. Participants could withdraw at any time during the research. There was minimal potential for harm to the study participants as a result of the study. Permission was obtained from the medical professionals to proceed before any data was collected. A cover letter included with each survey provided information on how the information that was collected would be used and provided a contact telephone number should the participant have any concerns.
4. FINDINGS AND ANALYSIS
73 doctors knew someone who was involved or affected by medical malpractice, while 27 physicians had no knowledge of such colleagues. In 36% of cases, a lawsuit was initiated, while in 28% of cases a settlement was reached. Nine percent of cases received a threatening letter from a lawyer and 24% indicated other forms of legal action.
In the sample, 39% were personally involved in medical malpractice (12% on several occasions), 61% were never involved in a medical malpractice case. The majority of respondents were somewhat familiar with medical malpractice laws in the United States. Three quarters of them believe that the laws on the books are not fair and just, while one quarter are not sure or have no opinion. It is interesting to note, that not a single respondent indicated that the current malpractice laws are fair and just.
Two thirds of respondents feel that federal medical malpractice reform is necessary, 13% had the opposing view and 21% are not sure or have no opinion. 73% are either concerned or very concerned about the medical malpractice. The median cost of liability coverage is $15,000.00, while the average cost of liability coverage is around $27,000.00. Family physician pays about $15,000.00 in premiums, while a neurosurgeon pays upwards of $100,000.00. Almost 80% either agree or strongly agree that defensive medicine is a serious issue. More than half of all respondents (51%) practice overly defensive medicine because of fear of litigation. However, 55% indicate that it is not likely that within the next 12 months they will personally reduce or eliminate high risk aspects of their practice because of the medical liability threat. 55% of respondents indicated that they view every patient as a potential malpractice lawsuit. Doctors were bothered by the fact that they have to keep detailed treatment documentation.
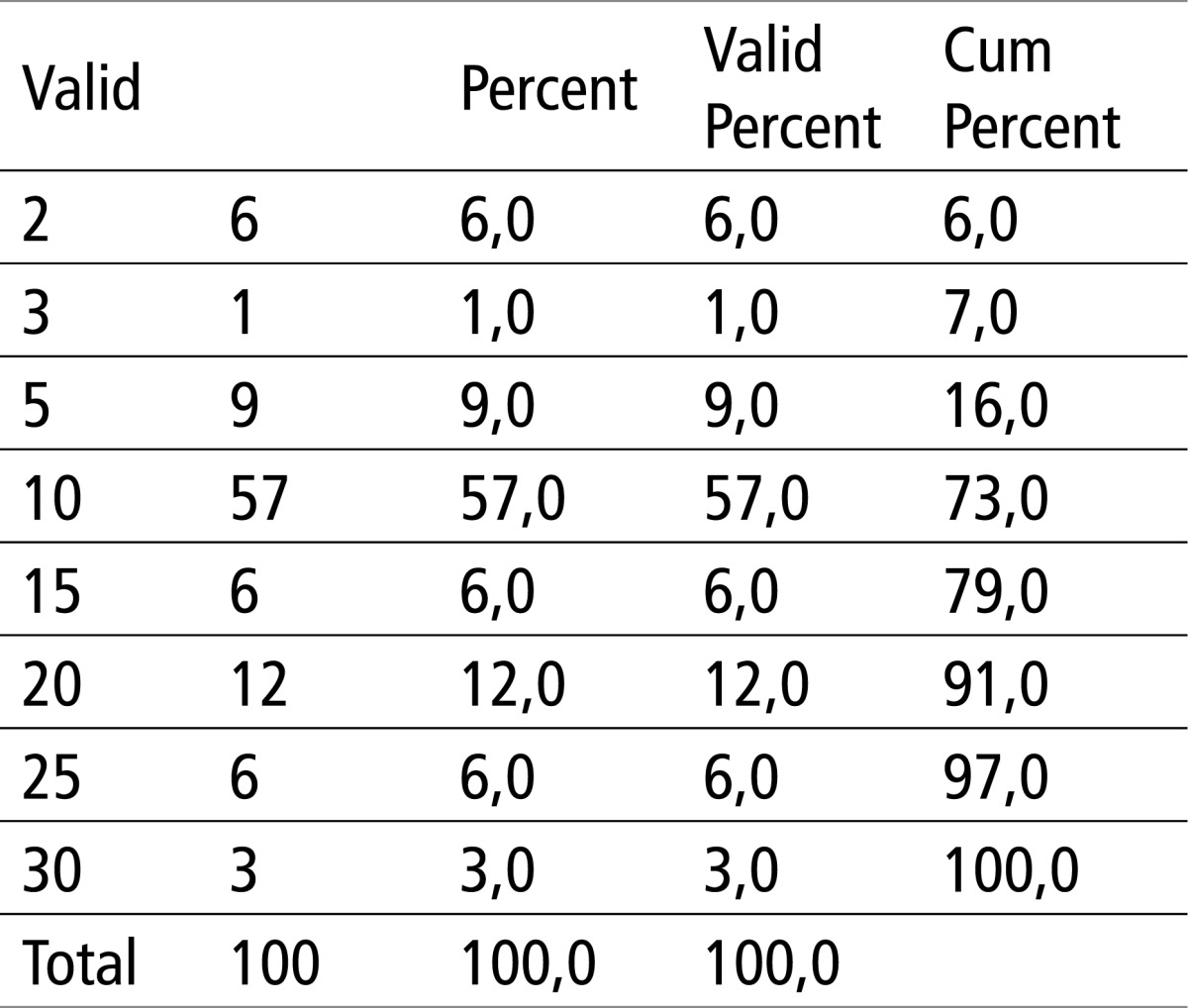
More than half of all respondents indicated that because of concerns regarding liability, they on occasion order more tests than they normally would, based on judgment of what is medically needed. Similarly, 49% sometimes refer patients to specialists because of liability concerns and 36% sometimes prescribe more medication than they would (based on their clinical judgment). Almost one third of physicians indicated that they rarely avoid personally conducting certain procedures or interventions because of concerns about malpractice liability. Regarding the perceived cost of defensive medicine, 57% believe that the practice of so-called defensive medicine contributes 10% to aggregate healthcare expenditures in Connecticut. 42% of physicians are concerned or strongly concerned that they will be involved in a malpractice case sometimes in the next 10 years. 27% disagree with the statement “ I feel pressured in my day-to-day practice by the threat of malpractice litigation”.
Many felt as victims of the current system, as malpractice laws unfairly punish doctors, increase overall health-care cost, promote defensive medicine, do not improving patient care, and benefit the attorneys. Unnecessary tests such as CT/MRI scans were frequently ordered in order to protect physicians from lawsuits. One specialist indicated that lawyers should receive less than 10% of settlements.
Doctors favored the elimination of interest on judgments, giving judges more latitude to adjust verdicts and limiting pain and suffering to $250,000. The prevailing view was that the malpractice environment in Connecticut locally and in the United States of America nationally is reducing the amount of good medical care that the system can provide to a patient per dollar spent.
Almost two thirds of all respondents indicated new technology contributes substantially to the rise of medical costs. 82% indicated that insurance companies contribute significantly to the rise in medical costs. 70% of doctors indicated that drugs are a significant factor in the rise of medical costs.
Among the respondents who detailed their restrictions on practice, the most common reports were stopping practice altogether or eliminating specific high-risk procedures; for example, emergency or trauma surgery by orthopedic surgeons, neurosurgeons, and general surgeons; complex obstetrics by obstetrician/gynecologists; and mammograms by radiologists. Many surgeons also reported avoidance of patients perceived to be risky propositions, either because of their clinical complexity or personal propensity for litigation, such as children and patients covered by workers‘ compensation and medical assistance.
4.1. Analysis
Technology plays a key role in defensive medicine and in malpractice liability generally. Specialists reported using technology to pacify demanding patients, bolster their own self-confidence, or create a trail of evidence that they had confirmed or excluded particular disease entities. Advances in diagnostic and therapeutic technologies make early detection of cancer both feasible and beneficial, and increase the likelihood that a missed diagnosis will be ruled negligent and assessed substantial damages.
4.2. Quality Effects
This study suggests that certain types of patients commonly prompt specialist physicians to behave defensively, especially those who are seen as demanding, emotional, or unpredictable. Two contrasting behavioral responses were evident. Specialists who perceived or anticipated adversarial relationships with patients often indulged their demands for expensive but unnecessary diagnostic studies.
4.3. Recommendations for Future Study
Several issues discovered in the present study would benefit from the further research. The Pennsylvania study (Studdert et al., 2005) found a relationship between the burden of malpractice insurance and the prevalence of defensive medicine. A similar relationship was not found in this study. There is a need to study possible alternatives to the current medical malpractice system and to look for a system that allows more of the resources allocated for malpractice insurance to go to the injured patients and less to be spent on unnecessary tests and procedures.
This study surveyed physicians in Connecticut. Other parts of the country could be studied to see if the defensive medicine that was found in both Pennsylvania and Connecticut would also be found in other parts of the country to determine if the findings of these two studies could be extended to the nation as a whole. If one area of the country was found to have lower levels of defensive medicine, then that area could be studied to determine what factors led to the lower levels of defensive medicine.
The American medical malpractice system could also learn from other advanced countries experiences with this complex issue. For example, New Zealand has a comprehensive system of compensation for all personal injuries, whether they occur at work, on the highway, in the home, in the hospital, or anywhere else. The intent of the scheme is to compensate all instances of physical or mental harm caused by accident but excluding those arising from illness or old age. The scope of the scheme is broad, but excluded are (1) the effects of a cardiovascular or cerebrovascular episode unless it is work-related and the result of undue strain, or unless the episode results from an injury by accident; and (2) physical or mental damage caused exclusively by disease, infection, or the aging process. Administered by a nonprofit, autonomous governmental organization (the Accident Compensation Corporation), the New Zealand program compensated for total disability, in periodic payments, at a level of 80 percent of earnings up to a prescribed ceiling. Proportionate adjustments are made for partial disability. The benefit level is fixed at 80 percent to create an incentive for rehabilitation. Payments are made for disability, adjusted for inflation, until age sixty-five, when pensions take over. In addition to payment for loss of earnings, reasonable costs of medical and dental treatment are covered, as well as reasonable costs of transport to the doctor or hospital for initial treatment and for further rehabilitative treatment, rehabilitation, and retraining assistance; payment for reasonable cost of necessary constant personal attention of the injured person following the accident; lump sum for permanent physical disability; lump sum for pain and suffering; lump sum to dependent spouse and dependent children; and other benefits.
The program is financed by the contributions from employers and employees and the self-employed, together with payments from owners of motor vehicles and a small supplement from general taxation.24 The New Zealand physician or surgeon pays a levy based on income at the rate of 1.5 percent, or $3000 up to the maximum levied income of $105,000. These payments cover the physician for his or her own incapacity and also release the physician entirely from all risk of claims for damages from others.
Sweden introduced a voluntary patient insurance scheme administered by a consortium of insurers headed by Skandia Life. The scheme is funded and paid by the county councils on a per capita basis. Injured patients may elect to bring an action in tort or may receive compensation under the patient compensation program without having to prove fault. The program was not enacted by the Swedish government but is the result of an agreement between the Federation of County Councils and a consortium of Swedish insurers. Although the program is generally described as no-fault, it is not strictly so because error underlies most payments: Such an error, however, does not have to be proved negligent; error may be assumed where the outcome is unusual.
In 1980, Sweden introduced a pharmaceutical scheme, which is also a voluntary,
non-statutory system covering injuries from vaccination and blood products. Impelled by the threat of legislation, the program is paid for by the drug industry, and premiums are based on each company’s market share. Five types of injury are covered under the Swedish compensation system: (1) treatments, (2) timing and accuracy of diagnosis, (3) accidents, (4) infections, and (5) injuries caused by diagnostic procedures. To be compensated, an individual must have reported sick for a minimum of fourteen days or been hospitalized for at least ten days, or have suffered permanent injury, or died.
Finland has introduced comprehensive pharmaceutical and treatment injury insurance modeled after the Swedish system. The Patient Injury Act of 1996 permits payments for loss of earnings, loss of amenities, and pain and suffering. Ninety-three percent of all medical care is provided by the State.
5. CONCLUSIONS
This study expands upon the very good foundation of the Studdert et al. (2005) research in Pennsylvania. The Pennsylvania study, with a large sample of 824 physicians represented the standard for defensive medicine studies due to the large size of the sample and hence the predictive power of the study. The current study used a similar survey instrument on a different population, approximately eight years later. The purpose of this study was to compare and contrast the findings with a different population. The original study sampled the universe of physicians in Pennsylvania. Study sampled licensed physician in Connecticut. Similar survey interments were used for the two studies. The primary motivation for using this instrument was to allow a comparison of the findings of the two studies without any issues relating to differences in the specific wording of the questions on the two instruments. Connecticut instituted medical malpractice reform in 2002 and this fact may have affected the results. One might expect that the passage of tort reform would reduce the prevalence of defensive medicine. However, defensive medicine was found to be quite prevalent despite the passage of tort reform. Chapter 5 of the current study focuses on four major topics: hypothesis testing results, discussions, conclusions, and recommendations.
5.1. Hypothesis Testing
H01: Defensive medicine remains prevalent in Connecticut after tort reforms have been enacted.
HA1: Defensive medicine is no longer prevalent in Connecticut after tort reforms have been enacted.
The basic hypothesis of the study was that defensive medicine was prevalent in Connecticut, and therefore the null hypothesis was that defensive medicine was not found to be prevalent in Connecticut. According to the responses from Connecticut doctors, defensive medicine is still widely prevalent in the state.
H01: The cost of defensive medicine with respect to the aggregate health care expenditures is less than 5 %.
HA1: The cost of defensive medicine with respect to aggregate health care expenditures is more than 5 %
It is clear from the conducted survey in the State of Connecticut that the majority of physicians believe that the practice of defensive medicine contributes more than five percent to overall health care costs.
H01: Connecticut doctors favor proposed alternative dispute resolution mechanisms
HA1: Connecticut doctors do not favor proposed alternative dispute resolution mechanisms
Based on qualitative interviews and survey responses, most doctors in this sample think that health panel arbitration should be utilized. In addition, many of them indicate that mediation should be required as a (first) resort in medical malpractice disputes. Furthermore, some type of no-fault insurance should be implemented as compensation mechanism, according to the majority of survey respondents.
Based on the above results, a substantial percentage of Connecticut physicians clearly favor some of the proposed ADR alternatives to the current tort system.
The findings from this study suggested that the issue of defensive medicine, with its associated costs and waste of medical resources, has not been addressed by Connecticut‘ s tort reform to date.
Many of the physicians indicated on the survey form the specific tests that they would order primarily or exclusively for defensive reasons. Most of these tests were relatively harmless procedures such as CT scans, but the cost of these unnecessary procedures is likely to be large in the aggregate and unwarranted procedures may cause actual harm to the patient, in addition to wasting medical resources. This expense is borne by the patient and society as a whole. If the patient has medical insurance, most of the cost will be borne by the insurer, but the waste represents a significant waste of resources for the medical system as a whole. The physicians that responded provided a large variety of defensive measures in which they engaged. Many of the unnecessary tests that were ordered had minimal discomfort for the patient, such as CT scans and blood tests, but other procedures, such as biopsies, could cause considerable discomfort to the patients, and as well as some danger to the patient‘s well-being. Several definite classes of negative outcomes are associated with defensive medicine: the economic loss associated with the cost of unnecessary tests, the possible harm to the patient from tests that are not medically indicated, and the separation of interests between the patient and the physician who has to make decisions as protection from malpractice litigation. The physician cannot offer the best advice to the patient so long as the physician is worried about his or her actions being questioned subsequently in an adversarial legal proceeding.
Figure 1.
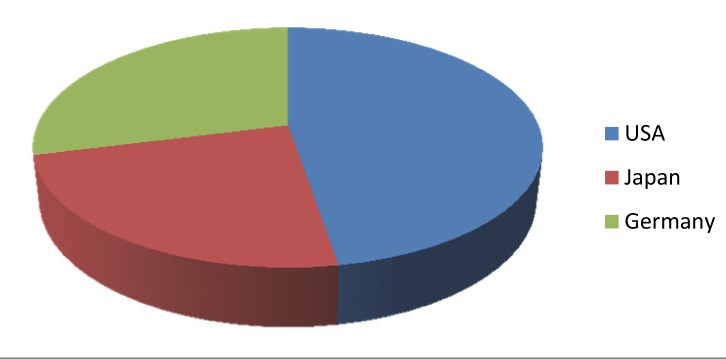
Healthcare expenditures of GDP
Figure 2.
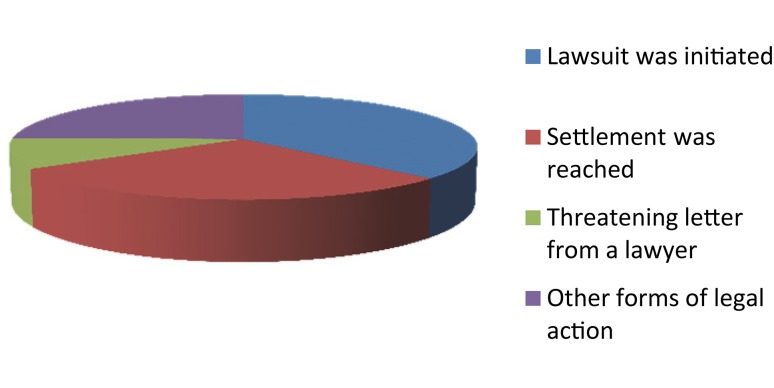
Legal manifestations of medical malpratice
Table 1.
Characteristics of Phyiscians
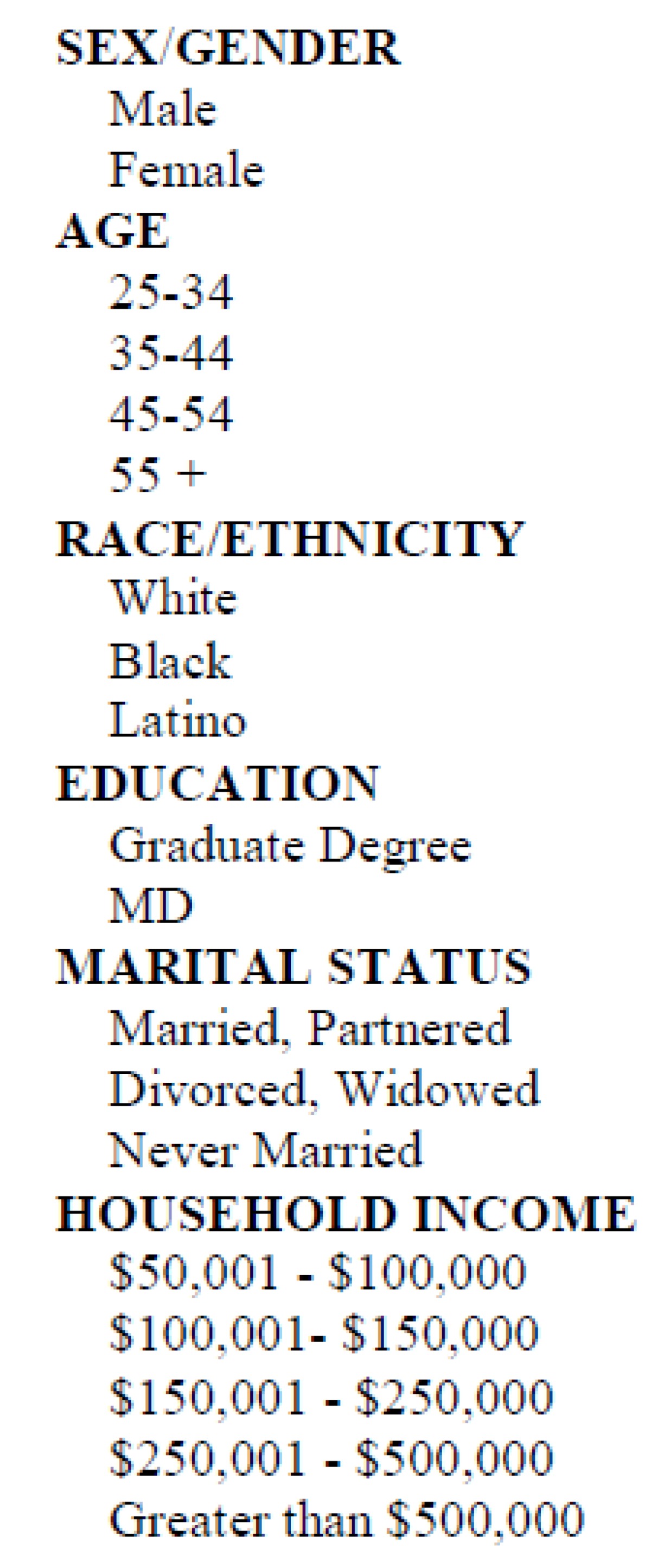 |
Table 2.
Characteristics of Phyiscians status
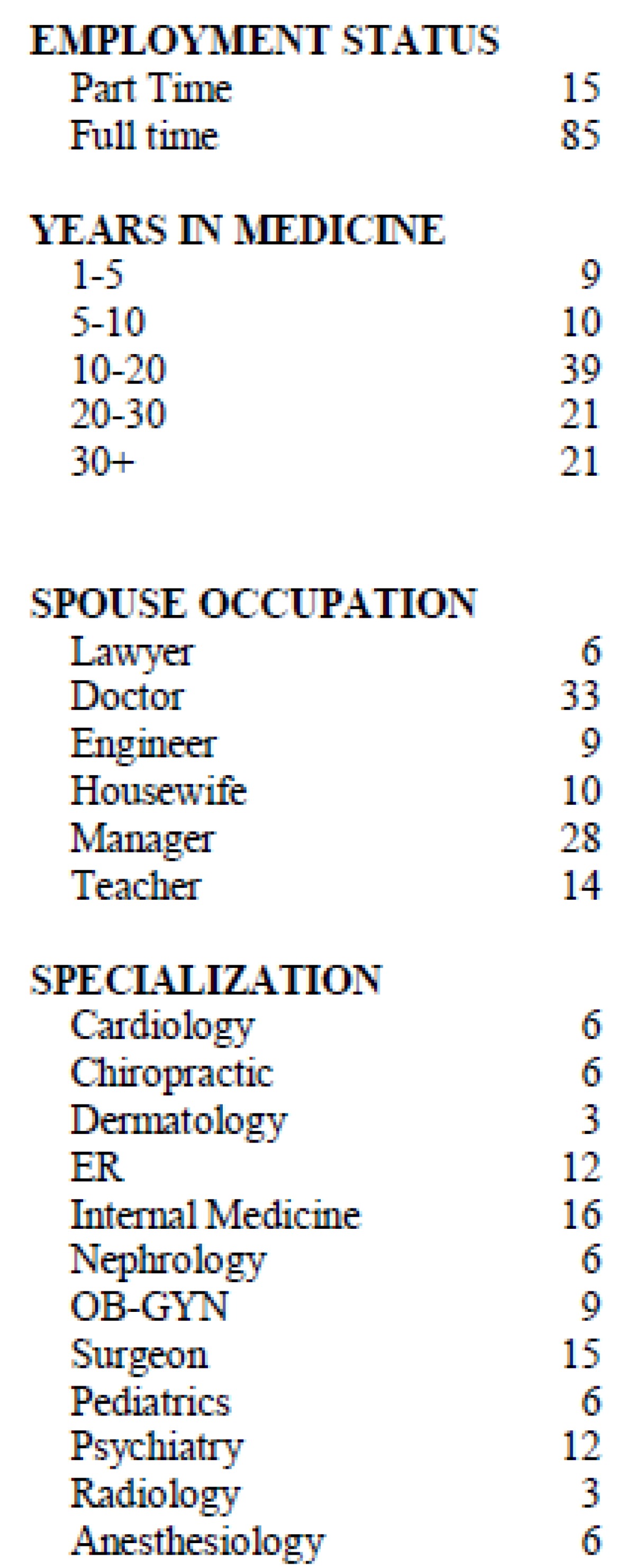 |
Table 3.
Cost of „defensive medicine” regarding health cost (%)?
 |
Conflict of interest
none declared
REFERENCES
- 1.Anderson R. Billions for defense. Retrieved October 6, 2010, from Archives of Internal Medicine Web site at http://archiate.ama-assn.org .
- 2.Baicker K, Chandra A. Defensive medicine and disappearing doctors? Regulation. 2003;28(3):24–31. [Google Scholar]
- 3.Bechhofer F, Paterson L. New York: Routledge; 2000. Principles of research design in the social sciences. [Google Scholar]
- 4.Blendon R, DesRoches C, Brodie M, Benson J, Rosen A, Schneider E. Views of practicing physicians and the public on medical errors. New England Journal of Medicine. 2002;347(24):1933–1940. doi: 10.1056/NEJMsa022151. [DOI] [PubMed] [Google Scholar]
- 5.Brewerton P, Millward L. Thousand Oaks, CA: Sage; 2001. Organizational research methods. [Google Scholar]
- 6.Brilla R, Evers S, Deutschlander A, Wartenberg KE. Are neurology residents in the United States being taught defensive medicine? Clinical Neurology and Neurosurgery. 2006;108:374–77. doi: 10.1016/j.clineuro.2005.05.013. [DOI] [PubMed] [Google Scholar]
- 7.California Medical Association. Newport Beach, CA: Future Cost Analysts; 1985. Actuarial study of professional liability insurance. [Google Scholar]
- 8.Elmore J, Taplin S, Barlow W, Cutter G, DeOrsi CJ, Hendrick RE, et al. Does litigation influence medical practice? Radiology. 2005;236:37–46. doi: 10.1148/radiol.2361040512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gaba D. Anesthesiology as a model for patient safety in health care. BMJ. 2000;320:785–788. doi: 10.1136/bmj.320.7237.785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gallagher T, Waterman A, Ebers A, Fraser V, Levinson W. Patients’ and physicians’ attitude regarding the disclosure of medical errors. Journal of the American Medical Association. 2003 Feb;289:1001–1007. doi: 10.1001/jama.289.8.1001. [DOI] [PubMed] [Google Scholar]
- 11.Grant D, McInnes MM. Malpractice experience and the incidence of cesarean delivery: A physicianlevel longitudinal analysis. Inquiry. 2004;41:170–188. doi: 10.5034/inquiryjrnl_41.2.170. [DOI] [PubMed] [Google Scholar]
- 12.Have P. London: Sage; 2004. Understanding qualitative research and ethno-methodology. [Google Scholar]
- 13.Heaton J. London: Sage Hell; Reworking qualitative data. [Google Scholar]; Hellinger FJ, Encinosa WE. The impact of state laws limiting malpractice damage awards on health care expenditures. American Journal of Public Health. 2006;96:1375–81. doi: 10.2105/AJPH.2005.077883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kachalia A, Choudhry NK, Studdert DM. Physician responses to the malpractice crisis: From defense to offense. Journal of Law and Medical Ethics. 2005;33:416–28. doi: 10.1111/j.1748-720x.2005.tb00509.x. [DOI] [PubMed] [Google Scholar]
- 15.Kessler D, McClellan M. The effects of malpractice pressure and liability reforms on physicians’ perceptions of medical care. Law and Contemporary Problems. 1997;80:81–100. [Google Scholar]
- 16.Kessler D, McClellan M. Do doctors practice defensive medicine? Quarterly Journal of Economics. 1996;111:353–390. [Google Scholar]
- 17.King G, Keohane R, Verba S. Princeton, NJ: Princeton University Press; 1994. Designing social inquiry. [Google Scholar]
- 18.Kohn LT, Corrigan JM, Donaldson M, editors. Washington, DC: Institute of Medicine; 1999. To Err Is Human: Building a safer health system. [PubMed] [Google Scholar]
- 19.Leape L, Berwick D, Bates D. What practices will most improve safety? Journal of the American Medical Association. 2002;288:501–507. doi: 10.1001/jama.288.4.501. [DOI] [PubMed] [Google Scholar]
- 20.McDonald C, Weiner M, Hui S. Deaths due to medical errors are exaggerated in Institute of Medicine report. Journal of the American Medical Association. 2000;284:93–95. doi: 10.1001/jama.284.1.93. [DOI] [PubMed] [Google Scholar]
- 21.Morgan G, Smirich L. The case for qualitative research. Academy of Management Review. 1980;5:491–500. [Google Scholar]
- 22.Nelson L, Morrisey M, Kilgore M. Vol. 85. The Milbank Quarterly; 2007. Damages caps in medical malpractice cases; pp. 259–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Novelli P, et al. Professional liability insurance and its effects: Report of a survey of ACOGfs membership. Report prepared for the American College of Obstetricians and Gynecologists Washington D.C. 1983. Aug,
- 24.Reynolds RA, Rizzo JA, Gonzalez ML. The cost of medical professional liability. JAMA. 1987;257:2776–2781. [PubMed] [Google Scholar]
- 25.Ryan K, Schnatz P, Greene J, Curry S. Change in cesarean section rate as a reflection of the present malpractice crisis. Connecticut Medicine. 2005;69(3):139–41. [PubMed] [Google Scholar]
- 26.Studdert D, Mello M, Sage W. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA. 2005;293:2609. doi: 10.1001/jama.293.21.2609. [DOI] [PubMed] [Google Scholar]
- 27.Summerton N. Positive and negative factors in defensive medicine: A questionnaire study of general practitioners. BMJ. 1995;310:27–29. doi: 10.1136/bmj.310.6971.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.U.S. Congress, Office of Technology Assessment. Washington, DC: U.S. Government Printing Office; 1994. Jul, Defensive Medicine and Medical Malpractice, OTA-H.602. [Google Scholar]
- 29.Waters TM, Budetti PP, Claxton G, Lundy JP. Impact of state tort reforms on physician malpractice payments. Health Affairs. 2007;26:500–509. doi: 10.1377/hlthaff.26.2.500. [DOI] [PubMed] [Google Scholar]
- 30.Williams M, May T. London: Routledge; 1996. Introduction to the philosophy of social research. [Google Scholar]
- 31.Zuckerman S, Bovbjerg RR, Sloan F. Effects of tort reforms and other factors on medical malpractice insurance premiums. Inquiry. 1990;27(2):167–82. [PubMed] [Google Scholar]


