Abstract
Objectives
To determine how patients with sickle cell disease (SCD) perceive the quality of care that they receive from their primary healthcare providers.
Design
A questionnaire-based pilot study was used to elicit the views of patients about the quality of care they have been receiving from their primary healthcare providers and what they thought was the role of primary care in SCD management.
Setting
Sickle Cell Society and Sickle Cell and Thalassaemia Centre, in the London Borough of Brent.
Participants
One hundred questionnaires were distributed to potential participants with SCD between November 2010 and July 2011 of which 40 participants responded.
Main outcome measures
Analysis of 40 patient questionnaires collected over a nine-month period.
Results
Most patients are generally not satisfied with the quality of care that they are receiving from their primary healthcare providers for SCD. Most do not make use of general practitioner (GP) services for management of their SCD. Collecting prescriptions was the reason most cited for visiting the GP.
Conclusion
GPs could help improve the day-to-day management of patients with SCD. This could be facilitated by local quality improvement schemes in areas with high disease prevalence. The results of the survey have been used to help develop a GP education intervention and a local enhanced service to support primary healthcare clinicians with SCD's ongoing management.
Introduction
Sickle cell disease (SCD) is the most common inherited blood disorder in England. Without prompt diagnosis and proper treatment, it can be a serious source of morbidity and mortality. SCD is caused by a single amino acid substitution of valine for glutamic acid in the sixth position of the beta (β)-chain of the haemoglobin tetramer.1,2 The disease damages and changes the shape of red blood cells. The change in shape is a response to cell deoxygenation. When the oxygen uptake of the cell is low, the cells change their shape from a healthy round disk to a crescent (sickle shape), holly leaf or other similarly distorted shape. The sickled cells are rigid, less malleable and stickier than a normal cell; consequently, they may stick to each other and obstruct blood vessels. This obstruction causes harsh and painful complications. The complications can lead to frequent hospital visits and proper management of SCD is needed to minimize the risk of developing such complications.3
SCD clinical guidelines recommend that patients see a general practitioner (GP) for routine examination every six months and more often if new problems arise or their treatment protocol changes.4 In addition, immunizations, prescriptions and other preventive care measures need to be delivered effectively by GPs to prevent recurring infections and pain crisis.5
An analysis of emergency department admissions between January 2008 and July 2010 in the Northwest London Borough of Brent showed that patients with SCD tend to use the emergency department rather than seek advice and support from their GP.6 A focus group aimed at obtaining patient perspectives held in Brent showed that one of the reasons patients utilize the emergency department over their GP is because they perceive GPs as having limited knowledge of SCD.7 A primary care educational intervention has been designed, informed by these studies. To further triangulate the experience of patients, this pilot study was designed to elicit the views of patients about the quality of care they have been receiving from their primary healthcare providers and what they thought was the role of primary care in SCD management.
Methods
Study design and questionnaire
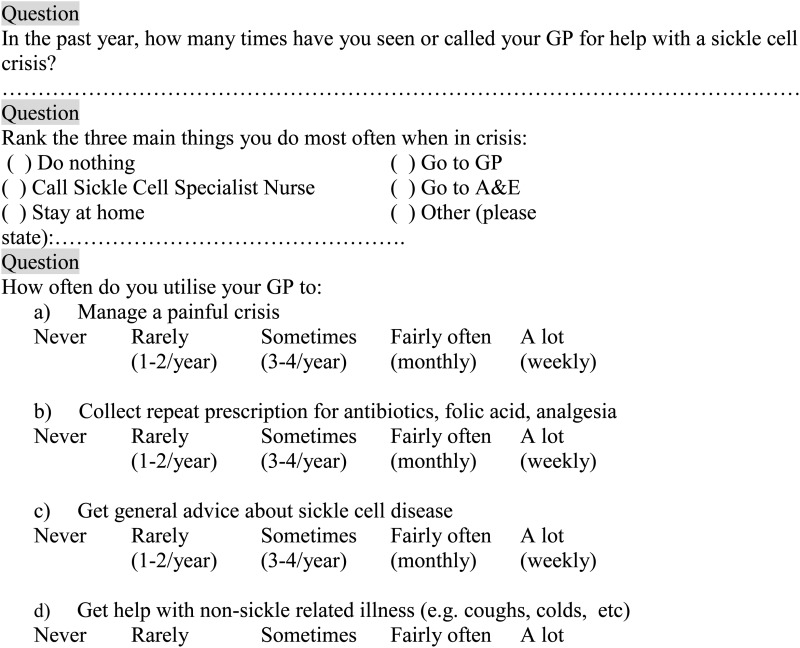
The study consisted of the development and administration of a 14-item study-specific questionnaire devised by a sickle cell steering committee which examined patients’ perceptions towards SCD and key management issues in primary care including severity of disease, how many times patients visited the Emergency Department in the last year, how many times patients saw or called their GP for sickle and non-sickle-related illnesses and general questions about GP satisfaction (Box 1). The validation process for the questionnaire followed several drafts reviewed by seven GPs practising across inner London, a professor of paediatric haematology specializing in SCD, a haematologist specializing in SCD in adults, a SCD specialist nurse, a SCD social worker, a SCD clinical psychologist, a number of quality improvement project managers, public health specialists, patient representatives with SCD and directors of the Sickle Cell Society (a national UK sickle cell charity). The pilot study is in itself part of the mechanism of validation for a larger questionnaire study.
Box 1. A selection of questions from the patient questionnaire.
Participants
One hundred questionnaires were distributed by post and in person (CN and PO) over a nine-month period from November 2010 to July 2011 to members of the Sickle Cell Society and to patients who attended the Sickle Cell and Thalassaemia Centre, using a purposive sampling method. Forty questionnaires were completed and suitable for analysis (OO and KJP).
Results
A response rate of 40% was achieved. Fifty percent (20) were completed by men and 50% (20) by women. The highest percentage of respondents (27%) was in the age range of 25–39 years. Five percent of respondents were aged 65+ years. The majority (62%) of the respondents were in good health and mobile. Nineteen (47%) respondents did not use their GP to manage a painful crisis and preferred to attend the emergency department. Twenty-four (59%) respondents went to their GP to collect repeat prescriptions. Twenty-two (55%) respondents did not visit their GP to get general advice about SCD (Table 2). Nine (23%) rarely visited their GP with four (10%) visiting sometimes or fairly often (Table 1). When asked how satisfied patients are with assistance given by their GP to help manage their SCD based on a scale of 0–10 (0 being not satisfied at all and 10 being very satisfied), the majority (54%) scored satisfaction with their GP as 5 or less while 43% scored a 6 or above and 3% did not answer the question at all. Collecting prescriptions was the reason most cited for visiting the GP's office (Table 2). Some examples of comments around the services provided by GPs include:
‘The GP should know about this disease’. (Patient Questionnaire 1)
‘The GP does not know anything about SCD pain and crisis. I would rather manage … at home or [go] to A + E where immediate action will be taken rather than call the GP who will ask us to book an appointment and more or less does not understand how to manage the pain or how severe or serious the pain is’. (Patient Questionnaire 2)
Table 2.
Support currently received from general practitioner
| Number of respondents | % of respondents | |
|---|---|---|
| Pain control | 14 | 35 |
| Collecting prescription | 37 | 93 |
| General SCD advice | 3 | 8 |
| Contraception | 2 | 5 |
| Other (please state) | 1 | 3 |
SCD, sickle cell disease
Table 1.
How often do you use your general practitioner to get general advice about sickle cell disease?
| Number of respondents | % of respondents | |
|---|---|---|
| Never | 22 | 55 |
| Rarely | 9 | 23 |
| Sometimes | 4 | 10 |
| Fairly often | 4 | 10 |
| Not answered | 1 | 3 |
Discussion
Key findings
The results from the survey show that many patients are generally not satisfied with the quality of care that they are receiving from their primary healthcare providers for SCD. Thus, most do not make use of GP services for management of their SCD. More importantly, the majority of the group did wish for greater involvement from their GP services, even if it was just to refer them to a tertiary care facility or social support.
Comparison with existing literature
Primary care satisfaction and SCD
There are few data collected about SCD patients and their level of satisfaction with primary care services. However, one study showed a 46% non-adherence rate for routine primary care appointments for SCD patients during an eight-month period.8 One of the reasons cited for the non-adherence was patient–provider relationships. Those with a positive patient and GP relationship were more likely to attend their clinic appointments.9,10 Other studies of chronic disease management showed that poor communication, multiple treating physicians, long waiting periods and past negative experiences with healthcare providers all contributed to patient dissatisfaction with primary care and poor attendance at clinics.11
Patient satisfaction as an indicator of health outcomes
Patient satisfaction is an important indicator of health outcomes. Researchers and healthcare providers have become increasingly interested in measuring patient satisfaction as an indicator of quality of care. Assessing patient satisfaction is a core requirement of contract for GPs in the UK.12 One study showed that assessing patient satisfaction allows GPs to investigate ‘the extent to which their service meets the needs of their client group’.13 Another study showed that satisfied patients are more likely to follow treatment protocol because the patient is more likely to believe that the treatment will be effective.14 In order for satisfaction to be measured in a meaningful way, a valid and reliable measure should be applied. The use of patient questionnaires has been one reliable way to assess patient satisfaction.12
The use of questionnaires to measure patient satisfaction
Properly constructed patient questionnaires have been found to be useful in measuring patient satisfaction,12 but they may also be valuable more specifically for measuring patient satisfaction in primary care and for primary care management of SCD. One study showed that a questionnaire was a valid and valuable tool to use in assessing the health-related quality of life in children with SCD and could serve as ‘an important adjunct to determine the effect of SCD on the lives of children’.15 Other studies showed questionnaires as a valuable tool in measuring quality of care or patient satisfaction in primary care16 particularly where the questionnaire assesses a specific area that enables the GP or other healthcare provider to identify with which aspects of service patients are less satisfied. This allows for the opportunity to improve a specified area.17
Strengths and limitations of this study
Our pilot study successfully identified issues with SCD management at the primary care level through the use of a questionnaire which could help inform the planning of a larger survey. Moreover, this study also identified a need to improve patient satisfaction and engagement with primary care. Raising awareness among GPs about SCD management was identified as a key method to improve GP–patient relationships and improve primary care clinic attendance.
Although this pilot study increases our understanding of the barriers associated with SCD management in primary care, it has certain limitations which could limit its transferability to areas outside of Northwest London. The questionnaire was based in an area with high prevalence of SCD and the sample size was small and consisted of purposive or volunteer sample. In addition, it is unclear how the identification of barriers in SCD management in primary care relates to the actual uptake of primary versus secondary care in SCD. Future studies would need to examine this link.
Conclusions
Despite its limitations, the study, along with the results of the focus group discussion which reinforced these findings,6 provides some valuable information that will give an opportunity to develop a disease-specific intervention which aims to improve patient care and help to ensure that management in primary care is optimized through the establishment of a local enhanced service. In the next stage of this project, we will implement this intervention and evaluate its impact on the management of patients with SCD by general practices in Northwest London.
DECLARATIONS
Competing interests
None declared
Funding
We thank the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care (CLAHRC) for NW London programme and NHS Brent for funding this project. The Department of Primary Care & Public Health at Imperial College London is grateful for support from the NIHR Biomedical Research Centre scheme and the Imperial Centre for Patient Safety and Service Quality
Ethical approval
Ethical approval was not required for this work as it is part of a service evaluation and improvement project
Guarantor
GA
Contributorship
KJP, YK and AM originally conceived the study; OO and KJP conducted the data analysis; GA wrote the first draft; all authors contributed in the revision of the manuscript
Acknowledgements
We thank the Sickle Cell Steering Committee and the Sickle Cell Society, a registered nationwide charity in the London Borough of Brent, who assisted with the administration of the patient questionnaires. We also thank the participants who completed the questionnaires; NHS Brent; and the Brent Sickle Cell and Thalassaemia Centre for their help with this project
Reviewer
Kamran Abbasi
Disclaimer
This article presents independent research commissioned by the National Institute for Health Research (NIHR) under the Collaborations for Leadership in Applied Health Research and Care (CLAHRC) programme for North West London. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health
References
- 1.Pack-Mabien A, Haynes J A primary care provider's guide to preventive and acute care management of adults and children with sickle cell disease. J Am Acad Nurse Pract 2009;21:250–7 [DOI] [PubMed] [Google Scholar]
- 2.Pace BS, Zein S Understanding mechanisms of γ-globin gene regulation to develop strategies for pharmacological fetal hemoglobin induction. Dev Dyn 2006;235:1727–37 [DOI] [PubMed] [Google Scholar]
- 3.AlJuburi G, Laverty A, Green SA, et al. Trends in hospital admissions for sickle cell disease in England, 2001/02–2009/10. J Public Health (Oxf) first published online 31 May 2012:1–7 [DOI] [PubMed] [Google Scholar]
- 4.NHS Sickle Cell and Thalassaemia Screening Programmes. Sickle Cell Disease in Childhood Standards and Guidelines for Clinical Care, 2nd edn NHS Sickle Cell and Thalassaemia Screening Programmes, London, 2010 [Google Scholar]
- 5.Wong WY Prevention and management of infection in children with sickle cell anaemia. Paediatr Drugs 2001;3:793–801 [DOI] [PubMed] [Google Scholar]
- 6.Green SA, AlJuburi G, Amobi C, et al. Characterising emergency admissions of patients with sickle cell crisis in NHS Brent: observational study. J R Soc Med Sh Rep 2012;3:3737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.AlJuburi G, Phekoo KJ, Okoye O, et al. Patients’ views on improving sickle cell disease management in primary care: focus group discussion. J R Soc Med Sh Rep 2012. (submitted) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robinson N, Huber H, Jenkins P, et al. Improving Access to Medical Care for Children with Sickle Cell Disease. The 29th Annual Meeting of the National Sickle Cell Disease Program, Memphis, TN, April 2006
- 9.Freed LH, Ellen JM, Irwin CE Jr, et al. , Determinants of adolescents’ satisfaction with health care providers and intentions to keep follow-up appointments. J Adolesc Health 1998;22:475–9 [DOI] [PubMed] [Google Scholar]
- 10.Modi AC, Crosby LE, Guilfoyle SM, Lemanek KL, Witherspoon D, Mitchell MJ Barriers to treatment adherence for pediatric patients with sickle cell disease and their families. Child Health Care 2009;38:107–22 [Google Scholar]
- 11.McCarthy K, McGee HM, O'Boyle CA Outpatient clinic waiting times and non-attendance as indicators of quality. Psychol Health Med 2000;5:287–93 [Google Scholar]
- 12.Grogan S, Conner M, Norman P, Willits D, Porter I Qual Health Care 2000;9:210–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Avis M, Bond M, Arthur A Satisfying solutions? A review of some unresolved issues in the measurement of patient satisfaction. J Adv Nurs 1995;22:316–22 [DOI] [PubMed] [Google Scholar]
- 14.Hardy GE, West MA, Hill F Components and predictors of patient satisfaction. Br J Health Psychol 1996;1:65–85 [Google Scholar]
- 15.Panepinto JA, O'Mahar KM, DeBaun MR, Rennie KM, Scott JP Child Health Care Questionnaire in sickle cell disease. J Pediatr Hematol Oncol 2004;26:574–8 [DOI] [PubMed] [Google Scholar]
- 16.Raat H, Landgraf JM, Bonsel GJ, et al. Reliability and validity of the Child Health Questionnaire – Child Form (CHQ-CF87) in a Dutch adolescent population. Qual Life Res 2002;11:575–81 [DOI] [PubMed] [Google Scholar]
- 17.Harris LE, Swindle RW, Mungai SM, et al. Measuring patient satisfaction for quality improvement. Med Care 1999;37:1207–13 [DOI] [PubMed] [Google Scholar]


