Abstract
Objectives
To introduce atraumatic (Sprotte) lumbar puncture needles and compare complication rates with traumatic (Quincke) needles.
Design
Complication rates associated with traumatic needle use were retrospectively analysed over a four-week period. Atraumatic needles were then implemented and a prospective analysis of the complication rates was undertaken for a further six weeks.
Setting
A single-centre acute neurology unit in a London teaching hospital
Participants
Traumatic needles (n = 24 patients); atraumatic needles (n = 36 patients)
Main outcome measures
Headache rates, use of over-the-counter medications, further medical assistance, time off work, nausea and vomiting, traumatic taps (as per the count of red blood cells per millilitre in the first sample of cerebrospinal fluid [CSF]) and back pain.
Results
A comparison of traumatic and atraumatic needles revealed a significant reduction in the incidence of post-lumbar puncture headaches (*P < 0.01), headaches requiring over-the-counter medication (*P < 0.00001), need for further medical assistance (*P < 0.006), time off work (*P < 0.003), nausea and vomiting (*P < 0.01) and traumatic taps as per the count of red blood cells per millilitre in the first sample of CSF (*P < 0.02). There was no significant difference in the incidence of back pain (P > 0.05).
Conclusions
Most complication outcomes are significantly lower with the use of atraumatic lumbar puncture needles. We present for the first time in the literature that the rate of ‘traumatic taps’ are significantly lower with atraumatic needles. The implementation of atraumatic needles in an acute neurology service is safe and produces reliable, reproducible results in keeping with previously published randomized controlled trials.
Introduction
The most common complication occurring after lumbar puncture is low-pressure headache.1 The mechanism by which this complication occurs is thought to be a continued cerebrospinal fluid (CSF) leak through a dural tear.2,3 Atraumatic (Sprotte) needles, with their characteristic pencil-point tip, were first developed in 1951.3 They have been in use since the early 1990s4 and have been shown to significantly reduce the incidence of postlumbar-puncture headache (PLPH) in numerous studies, including randomized prospective studies and double-blind randomized controlled trials.5–7 PLPH is defined as a headache appearing within 12 days from lumbar puncture although usually appearing within 24–48 h.6 As a result of the decreased incidence of PLPH with atraumatic needles they are widely used in spinal anaesthesia7 but their use in other clinical specialities is still limited.6 Their implementation has been recommended in several neurology publications5,7 but the uptake is poor in the UK (unlike the rest of Europe) due to concerns of cost, lack of familiarity with technique, perceived learning curve and availability. Here we retrospectively assessed the complication rates associated with the use of traumatic (Quincke) needles and compared this prospectively with atraumatic needles after their implementation into a regional acute neurology service.
Figure 1.
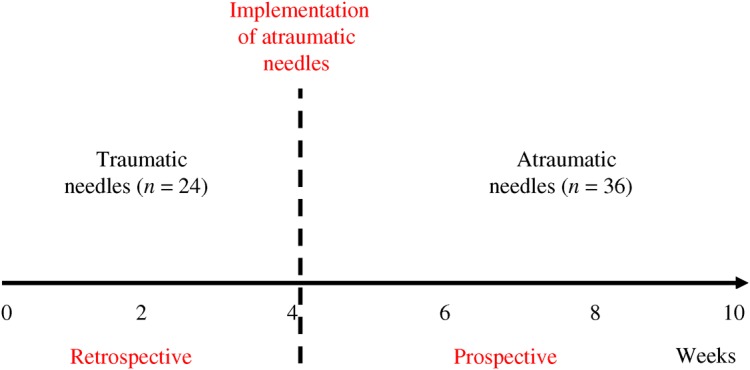
Audit timeline
Methods
The study took place in a single-centre acute neurology service planned investigation unit. The incidence of complications was audited by collecting retrospective data from 24 patients aged 53.5 ± 17.2 years (mean ± SD) who had undergone traumatic (Quincke) lumbar punctures using 22-G needles over the previous four weeks. The use of 22-G atraumatic (Sprotte) needles was then implemented and data were prospectively collected from 36 patients aged 47.9 ± 16.9 (mean ± SD) over six weeks. Data were collected by the authors using a telephone questionnaire (Figure 2). The lumbar punctures were performed for an unselected set of neurological conditions. They were performed with the patient in the left lateral position at the L3/4 or L4/5 level and the stylet was replaced prior to needle withdrawal. With regard to the traumatic needles the bevel was inserted upwards (perpendicular to the long axis of the patient). CSF was gained at the first or second attempt. The same volume of CSF (∼4 mL) was collected from all patients and volume was measured in the hospital laboratories to which the samples were sent for analysis. All patients were asked to remain flat for 30 min postprocedure. Patients undergoing therapeutic lumbar punctures for raised intracranial pressure were excluded from the study.
Figure 3.
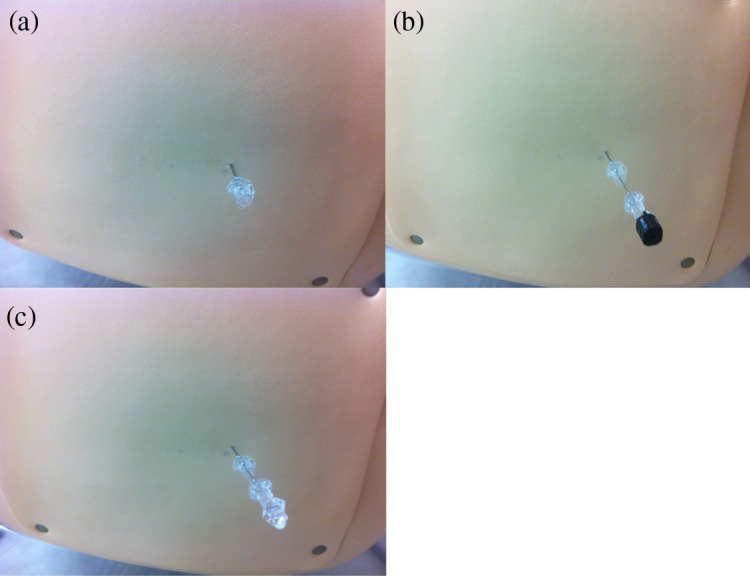
Atraumatic lumbar puncture needle technique. The technique for the use of atraumatic needles is easy to learn with a minimal learning curve for health-care workers already able to perform lumbar punctures using Quincke ‘traumatic’ needles. The Quincke needles have sharp tips, while the Sprotte needles are blunted. The most notable difference is the requirement for an introducer needle (a). This is a sharp-tipped 18-G needle through which the atraumatic needle passes. Once this is inserted approximately 2 cm deep to the skin (dependent on the amount of adipose tissue present) the atraumatic needle is then advanced (b). The tactile feedback using an atraumatic needle is different from traumatic needles but this is easily learnt. In younger patients the spinal ligaments tend to be tougher and require slightly more pressure to pass through. The stylet is withdrawn from the atraumatic needle and cerebrospinal fluid is attained (c). A manometer can then be attached to the end of the needle to measure the opening pressure
Figure 2.
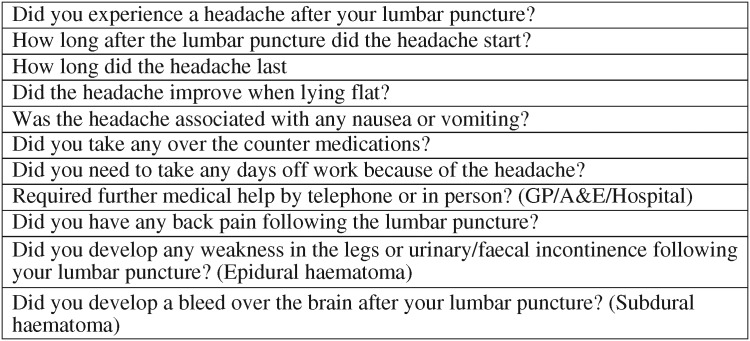
Questionnaire used for data collection
Two patients in the traumatic group and six patients in the atraumatic group were not contactable and therefore excluded from the study. Data on complication rates were collected by telephone questionnaire at least 12 days after they had undergone their lumbar puncture. Laboratory data on the number of red blood cells per millilitre of CSF in the first sample were analysed and used as an index for ‘traumatic’ taps.
Non-parametric comparisons of independent data-sets, such as the comparison of postprocedure headache between the traumatic and atraumatic groups, were analysed using a chi-squared test with a P ≤ 0.05. A Mann-Whitney U test was used to analyse the difference in red blood cells per millilitre in the first CSF sample following the two types of lumbar puncture.
Results
A comparison of traumatic (Quincke) and atraumatic (Sprotte) needles revealed a significant reduction in the incidence of postlumbar puncture headaches overall (*P < 0.01), headaches requiring over-the-counter medication (*P < 0.00001), need for further medical assistance (*P < 0.006), time off work (*P < 0.003), nausea and vomiting (*P < 0.01) and traumatic taps as per the count of red blood cells per millilitre in the CSF (*P < 0.02). There was no significant difference in the incidence of back pain (P > 0.05). There was no significant difference between the number of red blood cells per millilitre of CSF and the headache rate (P = 0.22) (Table 1).
Table 1.
Summary of results
| Traumatic (Quincke) | Atraumatic (Sprotte) | P value | |
|---|---|---|---|
| Total no. of patients | 24 | 36 | |
| Not contactable | 2/24 (8%) | 6/36 (17%) | |
| No headache | 12/22 (55%) | 22/30 (73%) | |
| Headache | 10/22 (45%) | 8/30 (27%) | *<0.01 |
| Requiring analgesia | 8/22 (36%) | 4/30 (13%) | *<0.00001 |
| Requiring further medical assistance | 5/22 (23%) | 0/30 (0%) | *<0.006 |
| Requiring time off work | 6/22 (27%) | 1/30 (3%) | *<0.003 |
| Back pain | 6/22 (27%) | 4/30 (13%) | 0.10 |
| Nausea or vomiting | 4/22 (18%) | 1/30 (3%) | *<0.01 |
| Average red bloods cells (RBC) in CSF | 438 RBC/mL | 58 RBC/mL | *P < 0.02 |
CSF, cerebrospinal fluid
Discussion
To the authors' knowledge this is the first report in the current literature that the use of atraumatic lumbar puncture needles has a lower rate of ‘traumatic taps’, as determined by the red blood cell count in the first sample of CSF taken, compared with the traumatic needles. In line with previously published randomized controlled studies we have also shown that the introduction of atraumatic lumbar puncture needle use to an acute neurology service in a London teaching hospital produces significant reductions in all complication rate outcome measures except back pain. The main limit to our study is the small number of participants due to the single-centre nature and short study duration.
A number of trials have been published comparing the incidence of headache and other complications following the use of traumatic versus atraumatic lumbar puncture needles across a wide variety of clinical settings. The initial studies over 20 years ago investigated the rate of postlumbar puncture headache following spinal anaesthesia using needles of gauge 24–29.8 Compared with our findings these studies had much lower incidences of postlumbar puncture headache for both traumatic and atraumatic needles of around 25% and 11%, respectively. This lower incidence for both needle types is thought to be due to the smaller gauge of the needles and delivery of spinal anaesthesia, both of which have been shown to be independent predictors of postlumbar puncture headache.9,10 These fine bore needles are suitable for spinal anaesthesia but when accurate pressure measurement and sampling of CSF is mandated needles of size 22 G or larger are required.11 Randomized controlled trials comparing the use of atraumatic versus traumatic 22-G needles have in some studies shown a significant improvement from 36% to 3%, respectively,12 while other studies have shown only a modest improvement from 42% traumatic to 33% atraumatic and 54% traumatic to 29% atraumatic.13 The latter studies are more in keeping with our results of 45% traumatic improving to 27% atraumatic. The discrepancy in the reported incidences may be due to the differing criteria used in these studies to delineate which headaches are likely due to ‘low pressure’ aetiology. Some studies reported all headaches while others only count headaches that had convincing low-pressure features, such as change in intensity with posture. Furthermore, other studies only included headaches of moderate-to-severe nature and discounted milder headaches. Interestingly studies which did not report the milder headaches have similar incidence rates to the group in our study which required over-the-counter medications. This suggests therefore that our results are in line with other published studies regarding headache incidence when the needle size and reporting criteria are accounted for.
Few studies in the literature have published rates of patients requiring over-the-counter medications or seeking further medical assistance. A randomized controlled study of 97 patients using a similar gauge of traumatic and atraumatic needles found rates of over-the-counter medication requirement to be 54% and 34%, respectively. In addition, patients requiring further medical attention (general practitioner consultation, hospital admission or hospital telephone call) were 18% in the traumatic group compared with 5% in the atraumatic group.13 This is consistent with our findings of 23% and 0%, respectively. As would be expected with a blunt tip needle the rate of ‘traumatic’ lumbar punctures, as determined by the red blood cell count in the first sample of CSF taken, is significantly lower than with the traumatic needles. To our knowledge this is the first report of this in the current literature but will require further correlation with larger studies.
Lumbar punctures are performed by a variety of physicians including anaesthetists, neurologists, general physicians, haematologists, oncologists and emergency department physicians. Their use is either diagnostic, for a wide range of infective or neuro-inflammatory conditions, or therapeutic, such as during spinal anaesthesia, intrathecal chemotherapy delivery and in the treatment of raised intracranial pressure. In some cases a tear in the dura following a lumbar puncture is thought to be beneficial and is hypothesized to be the reason why lumbar punctures in patients with raised intracranial pressure have a symptomatic benefit lasting longer than the physiological time it takes to reproduce the CSF removed.14 In the majority of cases, however, a CSF leak following a lumbar puncture from a dural tear is an unwanted side-effect which can be debilitating. This can lead to severe headaches, nausea, vomiting, tinnitus, diplopia, hearing impairment and in some cases development of subdural haemorrhages15 or venous sinus thrombosis.16
Factors which have been found to affect headache postlumbar puncture include age, needle gauge, needle type, bevel direction, reinsertion of the stylet prior to removal and administration of spinal anaesthesia.9–11 Factors for which there is no beneficial prophylactic evidence include lying flat for any period of time after the procedure, position of patient during the procedure, amount of CSF drained, caffeine and fluid intake post-procedure.9–11,17
Reasons stated for the lack of atraumatic needle use in the UK include lack of availability, comparative cost of the needles and concern about accuracy of pressure measurements. Atraumatic lumbar puncture needles are estimated to be 2–3 times the price of the standard traumatic needles. In a single institution over two months the significant reduction in complication rates represents cost efficiency and better patient care.17
Conclusion
A large evidence base now exists for the superiority of atraumatic lumbar puncture needles over traumatic needles but their use is still not commonplace in the UK compared with Europe. We have shown that the implementation of atraumatic lumbar puncture needle use is safe, has a minimal learning curve and produces reliable results in keeping with published complication rates. The rate of traumatic taps, using red blood cells per millilitre of CSF as a marker, is significantly lower. To increase the use of atraumatic lumbar puncture needles among the medical profession in the UK, greater awareness of the reduced complication rates, increased availability of needles and further training are required.
DECLARATIONS
Competing interests
None Declared
Funding
None
Ethical approval
None
Guarantor
VNV
Contributorship
Equal contribution on work from both authors
Acknowledgments
The authors would like to thank Dr Hari Jenksins (Consultant Neurologist) for helpful comments on the manuscript
Reviewer
Josef Finsterer
References
- 1.Lavi R, Rowe JM, Avivi I Lumbar puncture: it is time to change the needle. Eur Neurol 2010;64:108–13 Epub 14 July 2010 [DOI] [PubMed] [Google Scholar]
- 2.Angle PJ, Kronberg JE, Thompson DE, et al. Dural tissue trauma and cerebrospinal fluid leak after epidural needle puncture:effect of needle design, angle, and bevel orientation. Anaesthesiology 2003;99:1376–82 [DOI] [PubMed] [Google Scholar]
- 3.Turnbull DK, Shepherd DM Post-dural headache:pathogenesis, prevention and treatment. Br J Anaesth 2003;91:718–29 [DOI] [PubMed] [Google Scholar]
- 4.Kleyweg RP, Hertzberger LI, Carbaat PA Significant reduction in post-lumbar puncture headache using an atraumatic needle. A double-blind, controlled clinical trial. Cephalalgia 1998;18:635–7 [DOI] [PubMed] [Google Scholar]
- 5.Lavi R, Rowe JM, Avivi I Traumatic vs. atraumatic 22 G needle for therapeutic and diagnostic lumbar puncture in the hematologic patient: a prospective clinical trial. Haematologica 2007;92:1007–8 [DOI] [PubMed] [Google Scholar]
- 6.Arendt K, Demaerschalk BM, Wingerchuk DM, Camann W Atraumatic lumbar puncture needles: after all these years, are we still missing the point? Neurologist 2009;15:17–20 [DOI] [PubMed] [Google Scholar]
- 7.Bruce BB, Biousse V, Newman NJ Update on idiopathic intracranial hypertension. Am J Ophthalmol 2011;152:163–9 Epub 21 June 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vilming ST, Kloster R, Sandvik L The importance of sex, age, needle size, height and body mass index in post-lumbar puncture headache. Cephalalgia 2001;21:738–43 [DOI] [PubMed] [Google Scholar]
- 9.Turnbull DK, Shepherd DB Post-dural puncture headache: pathogenesis, prevention and treatment. Br J Anaesth 2003;91:718–29 Review [DOI] [PubMed] [Google Scholar]
- 10.Carson D, Serpell M Choosing the best needle for diagnostic lumbar puncture. Neurology 1996;47:33–7 [DOI] [PubMed] [Google Scholar]
- 11.Lavi R, Yarnitsky D, Rowe JM, Weissman A, Segal D, Avivi I Standard vs atraumatic Whitacre needle for diagnostic lumbar puncture: a randomized trial. Neurology 2006;67:1492–4 [DOI] [PubMed] [Google Scholar]
- 12.Luostarinen L, Heinonen T, Luostarinen M, Salmivaara A Diagnostic lumbar puncture. Comparative study between 22-gauge pencil point and sharp bevel needle. J Headache Pain 2005;6:400–4 Epub 1 August 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thomas SR, Jamieson DR, Muir KW Randomised controlled trial of atraumatic versus standard needles for diagnostic lumbar puncture BMJ 2000;321:986–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Amorim JA, Remígio DS, Damázio Filho O, de Barros MA, Carvalho VN, Valença MM Intracranial subdural hematoma post-spinal anesthesia: report of two cases and review of 33 cases in the literature. Rev Bras Anestesiol 2010;60:620–9, 344–9. Review [DOI] [PubMed] [Google Scholar]
- 15.Casado-Menéndez I, Uría DF, Jiménez L [Cerebral venous thrombosis as a complication following a diagnostic lumbar puncture]. Rev Neurol 2011;52:252–3 [PubMed] [Google Scholar]
- 16.Bezov D, Lipton RB, Ashina S Post-dural puncture headache: part I diagnosis, epidemiology, etiology, and pathophysiology. Headache 2010;50:1144–52 Epub 1 June 2010 [DOI] [PubMed] [Google Scholar]
- 17.Dakka Y, Warra N, Albadareen RJ, Jankowski M, Silver B Headache rate and cost of care following lumbar puncture at a single tertiary care hospital. Neurology 2011;77:71–4 Epub 18 May 2011 [DOI] [PubMed] [Google Scholar]


