Stress incontinence may be associated with benign joint hypermobility syndrome (BJHS), highlighting the importance of inquiring about such symptoms in nulliparous women.
Case report
A 20-year-old nulliparous woman was referred to the Department of Uro-neurology for unexplained urinary incontinence. She experienced incontinence most often with effort or exertion; however, this was particularly worse during coughing from exacerbations of chronic sinusitis. Symptoms were intrusive and she was requiring to use as many as 10 incontinence pads a day. In addition to this complaint, she also used to experience urinary urgency associated occasionally with incontinence, as well as urinary frequency, visiting the toilet once every 20 minutes in the daytime and waking up four times at night. There was no history of haematuria or dysuria, and she did not experience urinary tract infections.
She also reported constipation, and would open her bowels only once every three days and with rare episodes of faecal incontinence. She had symptoms akin to irritable bowel syndrome, with frequent abdominal bloating relieved by passing stools.
There was no evident urogenital prolapse. To evaluate her mixed incontinence, she had videourodynamics carried out (Figure 1). Screening showed a normal bladder outline which was normally sited and a closed bladder neck at rest. There was evidence for detrusor overactivity during the filling phase. When lying supine, coughing did not lead to any leakage of urine. When standing, asking the patient to cough produced descent of the bladder base with opening of the bladder neck, which led to incontinence. When she was asked to cough during the filling phase, there was evidence of beaking of the bladder neck, demonstrating urethral hypermobility. This was responsible for her stress incontinence. The patient voided a volume of 400 mL with a maximum flow rate (Qmax) of 61 mL/s and no postvoid residual.
Figure 1.
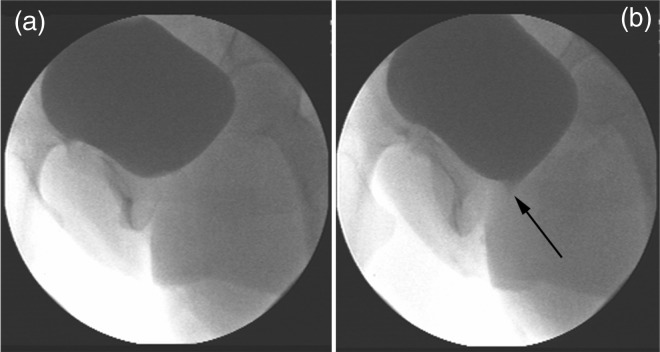
(a) View of the bladder after contrast filling. (b) Beaking of the bladder neck (indicated by arrow) produced on coughing, demonstrating urethral hypermobility. This was responsible for her stress incontinence
In view of the finding of urethral hypermobility, she was further asked about a possible disorder of collagen and, indeed, she gave a history of recurrent shoulder joint dislocation. She was seen by a rheumatology consultant and the patient was confirmed to have a BJHS. Diagnosis of this condition is made on clinical grounds using the Brighton criteria which assesses joint extensibility as well as associated symptoms that contribute to the syndrome (Table 1).1 A Beighton score of 4 (incorporated into the Brighton criteria) or more and longstanding generalized arthralgia, contribute major factors on the overall Brighton criteria. Associated symptoms contribute minor factors. A score of two major criteria, one major criteria and two minor criteria, or two minor criteria and an affected first-degree relative determines a diagnosis of BJHS.
Table 1.
The Brighton criteria for diagnosing benign joint hypermobility,1 incorporating the Beighton criteria
| Brighton Criteria for diagnosing BJHS (incorporating the Beighton criteria) |
MAJOR CRITERIA
|
MINOR CRITERIA
|
| Beighton Criteria |
(1 point gained for each side where the sign is found, except for lumbar hyperflexion)
|
The patient was found to be hypermobile bilaterally in thumbs, elbows, knees and lumbar spine, giving her a Beighton score of 7 out of 9. Her history was also positive for the major criteria of arthalgia for at least three months in four or more joints, with reported generalized aching and lower back pain. She also fulfilled a minor criterion with her history of recurrent dislocations of the shoulder. Of note, the patient's skin was not considered to be overly stretchable.
To understand the cause for her detrusor overactivity, a magnetic resonance imaging of her spine was performed to look for any evidence for spinal cord compression from vertebral subluxation or atlantoaxial dislocation, which may accompany disorders of collagen, and this was normal.
The patient is on regular follow-up with the Uro-neurology and Rheumatology Departments. Pelvic floor exercises have been started to strengthen her pelvic floor and prevent stress incontinence, and an antimuscarinic, solifenacin, for her symptoms of urgency. She has been started on laxatives for her constipation. For the management of her joint condition, a home exercise programme was developed by a physiotherapist to improve core stability, balance and muscle strength. She was also given advice on general fitness training to counter the effects of deconditioning. These measures should prevent future injury through dislocation and help to manage arthralgia.2
Discussion
The case highlights an unusual presentation of a condition that is highly prevalent but under-diagnosed.3 Stress incontinence in a nulliparous woman is an unusual complaint. Videourodynamics demonstrated bladder neck beaking, suggesting urethral hypermobility and the high flow rate is likely to be an accompaniment of this. Disorders of collagen can affect the tissues supporting the urethra, resulting in stress incontinence and the finding of a hypermobile urethra in videourodynamics.
In the evaluation of hypermobility, the differential diagnosis included BJHS, Ehlers Danlos syndrome, Marfan's syndrome and osteogenesis imperfecta.
There is limited information about urinary symptoms in Joint Hypermobility Syndrome. Some quantification of incontinence in the hypermobility syndrome population exists; studies by Arunkalaivanan et al.4 and Jha et al.5 found that urinary and faecal incontinence was significantly higher in people with the condition than controls. Uterine prolapse has also been correlated similarly, a finding in association with incontinence that has been found in related conditions such as Marfan's and umbrella Ehlers Danlos syndrome in general.6 However, there is little reported about bladder complaints being the presenting complaint of this condition, though this has recently begun to be recognized; especially that those with isolated stress incontinence without any obvious causative factors (i.e. child birth), may have BJHS.7,8
The management of stress incontinence in a person suffering from such a condition does not significantly differ from that provided for stress incontinence following child birth. Management is provided by a multidisciplinary team and involves physiotherapy and surgical options tailored to meet the patient's individual needs and requirements. However, management should first begin with conservative management then be escalated when needed.
In our patient, in addition to urinary incontinence, there were bowel complaints including faecal incontinence. Irritable bowel syndrome has also been associated with those with the condition.9
Physicians should enquire about joint hypermobility when faced with a young nulliparous woman presenting with stress incontinence. Similarly, specialists such as urologists and uro-gynaecologists should look for evidence for joint hypermobility in a patient with unexplained stress incontinence. Early diagnosis of the musculoskeletal condition expedites the management of symptoms associated with this condition such as pain, which can have drastic impact on quality of life. Likewise, an awareness of the condition allows patients to adopt measures to prevent soft tissue injuries.
Conclusion
Disorders of collagen can manifest in many ways, and suspicion of such a condition being responsible for symptoms in one area of the body should lead to investigation of gross collagen function, such as in the musculoskeletal system. Particularly in cases of stress incontinence in a nulliparous woman, practitioners may want to inquire about joint flexibility, as these easy to illicit signs may lead to expedited management for patients with unrecognized joint problems. As a cause of urinary symptoms, the diagnosis should remain one of exclusion when no other cause can be found.
DECLARATIONS
Competing interests
None declared
Funding
This work was undertaken at UCLH/UCL Institute of Neurology which received a proportion of funding from the Department of Health's NIHR Biomedical Research Centres funding scheme. MDS was attached to the department while receiving funding from a Wellcome Trust Elective Busary
Ethical approval
Written informed consent to publish was obtained from the patient or next of kin
Guarantor
MDS
Contributorship
The five authors are justifiably credited with authorship, according to authorship criteria. MDS, MH and JHS were involved in conception, acquisition of data, analysis and interpretation of data, and drafting of the manuscript; HK was involved in interpretation of data and critical revision of the manuscript; JNP was involved in conception, analysis and interpretation of data, and drafting of the manuscript
Acknowledgements
We would like to thank Barrie Lee for help in obtaining the video urodynamics image
Reviewer
Bruce Montgomery
References
- 1.Grahame R, Bird HA, Child A The revised (Brighton 1998) criteria for the diagnosis of benign joint hypermobility syndrome (BJHS). J Rheumatol 2000;27:1777–9 [PubMed] [Google Scholar]
- 2.Keer R, Grahame R Hypermobility Syndrome. Recognition and Management for Physiotherapists. Oxford, UK: Butterworth Heinemann, 2003 [Google Scholar]
- 3.Ross J, Grahame R Joint hypermobility syndrome. BMJ 2011;342:c7167. [DOI] [PubMed] [Google Scholar]
- 4.Arunkalaivanan AS, Morrison A, Jha S, Blann A Prevalence of urinary and faecal incontinence among female members of the Hypermobility Syndrome Association (HMSA). J Obstet Gynaecol 2009;29:126–8 [DOI] [PubMed] [Google Scholar]
- 5.Jha S, Arunkalaivanan AS, Situnayake RD Prevalence of incontinence in women with benign joint hypermobility syndrome . Int Urogynecol J Pelvic Floor Dysfunct 2007;18:61–4 [DOI] [PubMed] [Google Scholar]
- 6.Carley ME, Schaffer J Urinary incontinence and pelvic organ prolapse in women with Marfan or Ehlers Danlos syndrome. Am J Obstet Gynecol 2000;182:1021–3 [DOI] [PubMed] [Google Scholar]
- 7.Dickson MJ, Isdale M, Davies S Joint hypermobility syndrome. Urinary incontinence as presenting feature. BMJ 2011;342:d1002. [DOI] [PubMed] [Google Scholar]
- 8.Karan A, Isikoglu M, Aksac B, Attar E, Eskiyurt N, Yalcin O Hypermobility syndrome in 105 women with pure urinary stress incontinence and in 105 controls. Arch Gynecol Obstet 2004;269:89–90 [DOI] [PubMed] [Google Scholar]
- 9.Zarate N, Farmer AD, Grahame R, et al. Unexplained gastrointestinal symptoms and joint hypermobility: is connective tissue the missing link? Neurogastroenterol Motil 2010;22:252–62 [DOI] [PubMed] [Google Scholar]


