Abstract
Objectives
Foundation Year Ones (FY1s) are the most junior doctors in the UK who are often required to prescribe intravenous fluid to patients not under their regular care, during on-call or out-of-hours ward cover. This study aimed to investigate FY1s’ practice and decision-making process of intravenous fluid prescribing to these patients.
Design
Questionnaire survey.
Setting
Survey on Practices during on-calls and out-of-hours ward covers.
Participants
FY1s of five National Health Service (NHS) hospitals in England and Scotland.
Results
All 149 FY1s responded to survey. Eighty-six percent have been taught intravenous fluid prescribing during medical school, compared with only 48% in FY1 induction. More than half always/often checked the patient's urea and electrolytes (U&Es) (72%), read the fluid balance (58%) and observation charts (80%), discussed the case with nursing staff (75%), enquired about oral status (82%), identified the main diagnosis/operation (75%) and indication for intravenous fluid (72%) of the patient when prescribing intravenous fluid. However, less than half often/always read the medical notes (43%) or performed clinical examinations on patients (16%). Most FY1s (94%) always/often checked patient's U&Es when prescribing potassium.
Conclusions
The questionnaire study demonstrated variations among FY1s in the practice and decision-making process of intravenous fluid prescribing to patients unknown to them, during on-calls or out-of-hours ward covers. Such variations in practice should be addressed especially by medical and foundation schools, and NHS hospitals to improve patient care.
Background
Intravenous fluid therapy is an important and common component of medical and surgical care. Prescribing intravenous fluid to patients requires a good understanding of fluid and electrolyte balance in human body. The patient's condition, fluid and electrolytes balance, and dietary status are examples of important factors to be considered during decision-making when prescribing intravenous fluid. Studies showed that between 81% and 90% of intravenous fluid prescription on hospital wards were conducted by preregistration house officers (PRHOs) or Foundation Year Ones (FY1s) who were the most junior clinicians.1,2 FY1s, or previously known as PRHOs, are junior doctors in the first year of the Foundation Programme, which is a two-year training programme that forms the bridge between medical school and specialty or GP training in the UK.
Several studies have also reported that PRHOs/FY1s were often inadequately trained in fluid management, contributing to inappropriate intravenous fluid prescribing.2–5 Suboptimal intravenous fluid prescription may compromise patients’ safety and cause preventable iatrogenic complications including fluid overload, dehydration and imbalances of electrolytes such as sodium, potassium and chloride.3,4 Therefore, inappropriate intravenous fluid prescription increases morbidity and mortality among patients.3,4,6 A prospective study by Walsh and Walsh1 found that adverse outcomes directly related to incorrect intravenous fluid prescribing were mostly secondary to sodium and potassium overload. Another study has also demonstrated that there was poor correlation between serum electrolyte values and the amounts of electrolytes prescribed to postoperative patients in hospitals.7
FY1s are also often required to prescribe intravenous fluid to patients who are not under their regular care when they are on-call or on out-of-hours ward cover. This questionnaire survey aimed to investigate the FY1s’ practice and decision-making process of intravenous fluid prescribing to patients who were not under their regular care, during on-calls or out-of-hour ward covers in several hospitals in England and Scotland. Since potassium is not uncommonly included during intravenous fluid prescription, the study also specifically assessed the FY1s’ practice and decision-making process when prescribing potassium in the intravenous fluid.
Methods
A questionnaire survey (Figure 1) was handed out to FY1s of five National Health Service (NHS) hospitals in England (Colchester General Hospital and Homerton University Hospital) and Scotland (Glasgow Royal Infirmary, Stirling Royal Infirmary and Western Infirmary/Gartnavel General Hospital) in 2006/2007. The FY1s were identified from junior doctors lists obtained from postgraduate offices of the hospitals. Multiple choice questions were designed, based on several junior and senior clinicians’ opinions on what practices, attitudes and factors perceived to be important when making decision on intravenous fluid prescription to patients on general medical and surgical wards. Each question contained five choices of answers; ‘never’, ‘rarely’, ‘half the time’, ‘often’ and ‘always’. All FY1s were clearly informed that the questionnaire referred only to intravenous fluid prescribing to patients unknown to them and not under their routine care during on-calls or out-of-hours ward covers.
Figure 1.
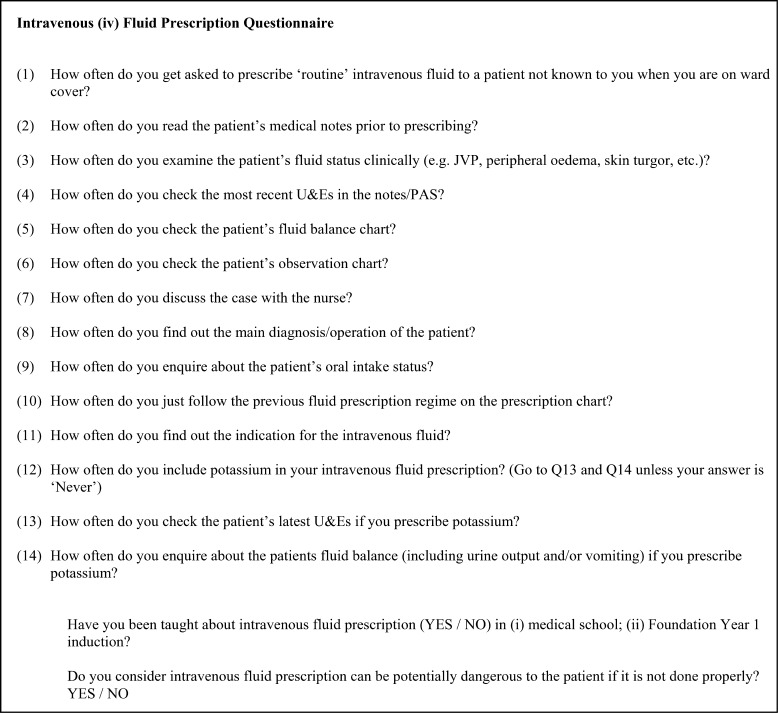
Intravenous fluid prescribing questionnaire used in this study. Choices of answer given for questions 1 to 14 were: Always; Often; Half the time; Rarely; or Never
Results
All FY1s identified at time of questionnaire in the five hospitals participated in the survey (n = 149). All FY1s surveyed have prescribed intravenous fluid to patients unknown to them during on-calls or out-of-hours ward covers. Ninety-five percent (142/149) of FY1s have often or always been asked to prescribe intravenous fluid to patients unknown to them. The majority of the FY1s (128/149 or 86%) have been taught intravenous fluid prescription in medical school, whereas only 71/149 (48%) FY1s were taught in their Foundation Programme induction. All but two FY1s (99%) considered intravenous fluid prescription to be potentially dangerous to patients if it was not done properly.
Majority of FY1s always (53/149 or 36%) or often (58/149 or 39%) found out the main diagnosis/operation of the patient when prescribing intravenous fluid. Only 28 (19%), 8 (5%) and one of the FY1s looked for the main diagnosis/operation half the time, rarely and never, respectively, when prescribing intravenous fluid. Similarly, many FY1s always (54/149 or 36%) or often (53/149 or 36%) identified the indication for intravenous fluid when prescribing. Only 37 (25%) and 5 (3%) of 149 FY1s looked for the indication for intravenous fluid half the time and rarely, respectively.
Less than half of FY1s often (15/149 or 10%) or always (49/149 or 33%) read patient's medical notes (the admission clerking and clinical progress documentation, with or without previous case-notes) when prescribing intravenous fluid. Two FY1s never read patient's medical notes while the rest of them only did it rarely (35/149 or 23%) or half the time (47/149 or 32%). Many FY1s rarely (67/149 or 45%) or never (9/149 or 6%) examined the patient when prescribing intravenous fluid. About a third (49/149 or 33%) of FY1s examined the patients half the time, while the rest performed it often (18/149 or 12%) or always (6/149 or 4%) when prescribing intravenous fluid.
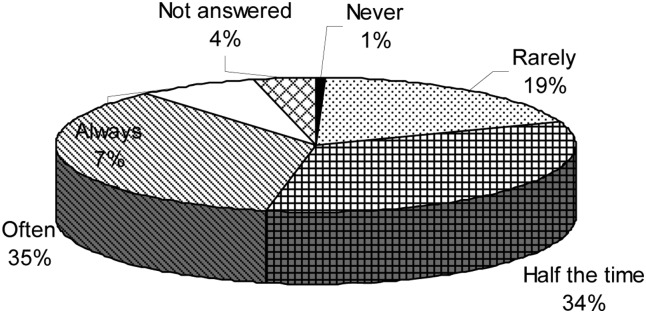
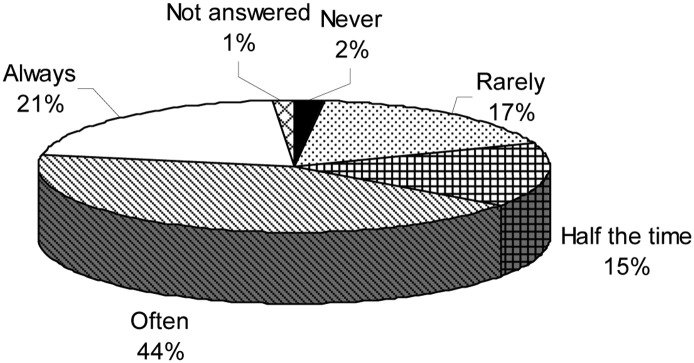
Majority of FY1s always (61/149 or 41%) or often (46/149 or 31%) checked patient's urea and electrolytes (U&E) before prescribing intravenous fluid. The rest of the FY1s only checked the U&E half the time (28/149 or 19%) or rarely (13/149 or 9%) (none never and one did not answer). Figures 2 and 3 summarized the percentages of FY1s who always/often/half the time/rarely/never checked patient's fluid balance and observation charts, respectively, when prescribing intravenous fluid.
Figure 2.
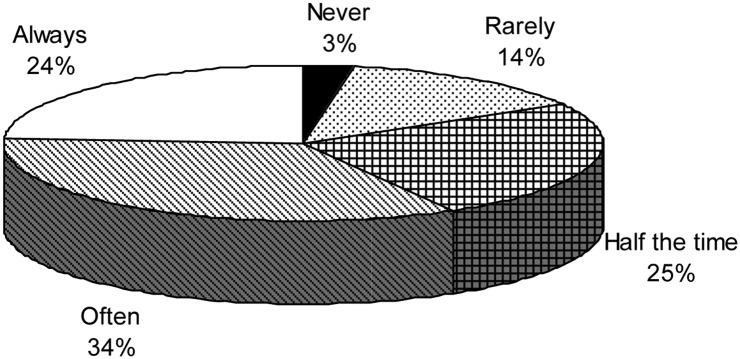
Percentages of Foundation Year Ones (FY1s) who checked the fluid balance chart before prescribing intravenous fluid to patients unknown to them and not under their care during on-calls or out-of-hours ward covers. How often do the FY1s check the patients's fluid balance chart?
Figure 3.
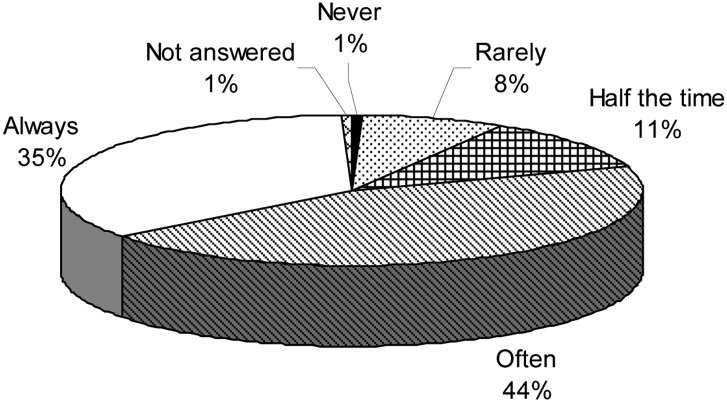
Percentages of Foundation Year Ones (FY1s) who checked the observation chart prior to intravenous fluid prescription to patients unknown to them and not under their care during on-calls or out-of-hours ward covers. How often do the FY1s check the patient's observation chart?
Most of the FY1s discussed the case with nursing staff when prescribing intravenous fluid with 52 (35%) always, 59 (40%) often, 21 (14%) half the time, 14 (9%) rarely and 2 (1%) never. Many FY1s always (53/149 or 36%) or often (69/149 or 46%) enquired about patient's oral intake when prescribing intravenous fluid. Meanwhile, only 21 (14%) and 4 (3%) of the FY1s enquired patient's oral intake half the time and rarely when prescribing intravenous fluid, respectively.
Although not many FY1s (5/149 or 3%) always just repeated the previous intravenous fluid prescription regimen on the chart, many of them did it half the time (51/149 or 34%) or often (57/149 or 38%). Meanwhile, 27 (18%) and 9 (6%) of them rarely and never, respectively, just followed the previous intravenous fluid prescription regimen.
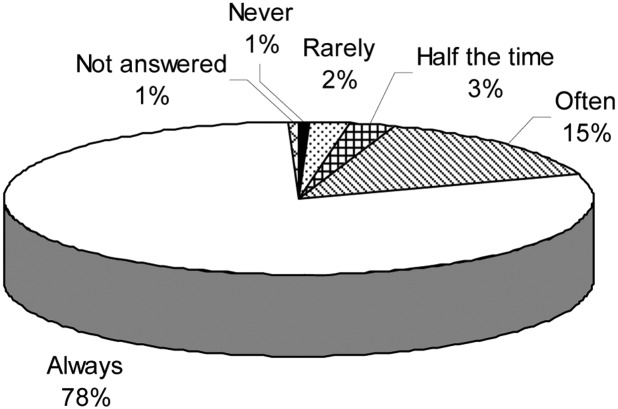
The practice of potassium prescribing in intravenous fluid by the FY1s is shown in Figures 4–6.
Figure 5.
Percentages of Foundation Year Ones (FY1s) who checked the latest urea and electrolytes (U&Es) results when prescribing potassium to patients unknown to them and not under their care during on-calls or out-of-hours ward covers. How often do the FY1s check the patient's latest U&Es when prescribing potassium?
Figure 4.
Percentages of Foundation Year Ones (FY1s) include potassium in intravenous fluid prescription to patients unknown to them and not under their care during on-calls or out-of-hours ward covers. How often do the FY1s include potassium in the iv fluid prescription?
Figure 6.
Percentages of Foundation Year Ones (FY1s) who enquired about fluid balance when prescribing potassium to patients unknown to them and not under their care during on-calls or out-of-hours ward covers. How often do the FY1s enquire about the patient's fluid balance (including urine output and/or vomiting) when prescribing potassium?
Discussion
Fluid management is a common and important part of clinical care of patients on medical and surgical wards.8 Inappropriate intravenous fluid management is common and known to contribute to a significant proportion of iatrogenic morbidities and mortalities.1,3,4,6,9 This is especially important in patients with reduced physiological reserves, including elderly patients and those with cardiac or renal failure.6,10–12 Despite the clear importance of appropriate intravenous fluid prescription, such practice is often left to be undertaken by the most junior doctors in the hospitals, such as the FY1s in the UK.1,2 This questionnaire survey found variations in the practice and decision-making process of intravenous fluid prescribing among the FY1s to patients unknown to them and not under their care during out-of-hours ward covers or on-calls. Overall, many FY1s assessed factors that were usually considered important when prescribing intravenous fluid to patients unknown to them during out-of-hours ward covers or on-calls. More than half of FY1s surveyed often, if not always, checked the patient's U&E, read the fluid balance and observation charts, discussed the case with nursing staff, identified the diagnosis/main operation and indication for the intravenous fluid, and enquired about the oral status of the patient when prescribing intravenous fluid. However, less than half of the FY1s surveyed often or always read the medical notes or performed clinical examinations on patients prior to intravenous fluid prescribing.
Potassium is not uncommonly prescribed with intravenous fluid on medical and surgical wards. Inappropriate intravenous potassium prescription is also known to contribute to significant mortality and morbidity in the hospital.1,5,13 For example, both hypokalaemia and hyperkalaemia can lead to serious cardiac arrythmias.14–16 In one audit that prospectively collected data regarding fluid and electrolyte prescription, fluid balance and intravenous fluid associated morbidity in an NHS hospital in England, it was found that seven of 71 (10%) patients developed tachyarrhythmia associated with the prescription of inadequate maintenance potassium.1 Another study observed that inappropriate fluid and electrolytes management, including potassium supplementation, was an important factor of iatrogenic hyperkalaemia even in hospitalized patients who were initially hypokalaemic, although other factors were also found to contribute.17 Previous studies have demonstrated variations in intravenous potassium prescription in hospitals, and recommended more consistency in the practice to improve safety.13 Many FY1s also not uncommonly prescribed potassium with intravenous fluid to patients unknown to them during out-of-hours ward covers or on-calls. In this study, the FY1s checked patients’ U&E more often when including potassium into intravenous fluid prescription than when not. This was not surprising since the complications from inappropriate prescription of potassium with intravenous fluid were commonly perceived to be more disastrous than when no potassium was included.
Previous studies have assessed the knowledge of FY1s or equivalent on fluid and electrolytes balance, content of various types of drips, and impact of medical teaching on intravenous fluid prescribing.2,18 Although these factors are often considered important to ensure appropriate intravenous fluid prescribing by FY1s, several other factors in practice are also relevant. In this study we investigated the way the FY1s assessed a patient's fluid and electrolytes status during intravenous fluid prescribing. We also specifically referred the practice to patients unknown to the FY1s during out-of-hours ward covers or on-calls because it was inevitable that FY1s would prescribe intravenous fluid to these group of patients, as demonstrated in this study. Furthermore, safe intravenous fluid prescribing to this group of patients would ideally require clinicians to find out as much detail about patient's condition, and fluid and electrolytes status as when prescribing to patients under their regular care.
The practices assessed in the study were generally considered important prior when prescribing intravenous fluid. Therefore, these practices should have been taught in the medical schools. As shown in this study, most FY1s have been taught intravenous fluid prescribing in medical school, and to a lesser extent in Foundation Programme induction. Despite this, variations still occurred among FY1s in intravenous fluid prescribing to patients unknown to them, with some of them rarely or never assessing certain factors which were generally considered important. Furthermore, almost all the FY1s surveyed (99%) were aware that inappropriate intravenous fluid prescribing could be potentially dangerous to patients. Therefore, besides education and awareness of the potential risks of inappropriate intravenous fluid prescription, other factors including time pressure and high workload during on-calls or out-of-hours ward covers, might contribute to such variations in practice and decision-making process.
One of the limitations of the study is that the number of FY1s interviewed may be relatively small. However, the FY1s involved in the study were from five different NHS hospitals in England and Scotland, and the majority of them graduated from several different medical schools in the UK, hence constitutes a reasonable representation of junior doctors in the country. Furthermore, even with 149 FY1s interviewed, it was clear that there were variations among FY1s in the practice and decision-making processes of intravenous fluid prescribing to patients unknown to them during on-calls or out-of-hours ward covers.
Conclusion
This questionnaire study concluded that there were variations among FY1s in the practice and decision-making processes of intravenous fluid prescribing to patients unknown to them during on-calls or out-of-hours ward covers. Further initiatives to educate and encourage all the FY1s to fully assess patients’ condition, and fluid and electrolytes status are important to ensure safe practice of intravenous fluid prescribing by junior doctors. These can take place as part of undergraduate medical school, Foundation Programme and local NHS hospital induction programme, thus reducing the variations observed in intravenous fluid prescribing among the FY1 doctors.
DECLARATION
Competing interests
None
Funding
None
Ethical approval
Ethical approval was not required for this study as it is a quality assurance/audit project that does not involve access to or collection of private, sensitive or health data
Guarantor
Chung Sim Lim
Contributorship
CTL and MD contributed equally
Acknowledgements
The authors thank all the FY1s of Colchester General Hospital, Homerton University Hospital, Glasgow Royal Infirmary, Stirling Royal Infirmary and Western Infirmary/Gartnavel General Hospital who took part in the questionnaire survey
Reviewer
Umar Saeed
References
- 1.Walsh SR, Walsh CJ Intravenous fluid-associated morbidity in postoperative patients. Ann R Coll Surg Engl 2005;87:126–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lobo DN, Dube MG, Neal KR, Simpson J, Rowlands BJ, Allison SP Problems with solutions: drowning in the brine of an inadequate knowledge base. Clin Nutr 2001;20:125–30 [DOI] [PubMed] [Google Scholar]
- 3.Lobo DN, Dube MG, Neal KR, Allison SP, Rowlands BJ Peri-operative fluid and electrolyte management: a survey of consultant surgeons in the UK. Ann R Coll Surg Engl 2002;84:156–60 [PMC free article] [PubMed] [Google Scholar]
- 4.Powell AG, Paterson-Brown S Safety through education. FY1 doctors still poor in prescribing intravenous fluids. BMJ 2011;342:d2741. [DOI] [PubMed] [Google Scholar]
- 5.Batra GS, Molyneux J, Scott NA Colorectal patients and cardiac arrhythmias detected on the surgical high dependency unit. Ann R Coll Surg Engl 2001;83:174–6 [PMC free article] [PubMed] [Google Scholar]
- 6.Walsh SR, Cook EJ, Bentley R, et al. Perioperative fluid management: prospective audit. Int J Clin Pract 2008;62:492–7 [DOI] [PubMed] [Google Scholar]
- 7.Stoneham MD, Hill EL Variability in post-operative fluid and electrolyte prescription. Br J Clin Pract 1997;51:82–4 [PubMed] [Google Scholar]
- 8.Lobo DN, Macafee DA, Allison SP How perioperative fluid balance influences postoperative outcomes. Best Pract Res Clin Anaesthesiol 2006;20:439–55 [DOI] [PubMed] [Google Scholar]
- 9.Mousavi M, Khalili H, Dashti-Khavidaki S Errors in fluid therapy in medical wards. Int J Clin Pharm 2012;34:374–81 [DOI] [PubMed] [Google Scholar]
- 10.Ferenczi E, Datta SS, Chopada A Intravenous fluid administration in elderly patients at a London hospital: a two-part audit encompassing ward-based fluid monitoring and prescribing practice by doctors. Int J Surg 2007;5:408–12 [DOI] [PubMed] [Google Scholar]
- 11.Luckey AE, Parsa CJ Fluid and electrolytes in the aged. Arch Surg 2003;138:1055–60 [DOI] [PubMed] [Google Scholar]
- 12.Friedman AL Management of the surgical patient with end-stage renal disease. Hemodial Int 2003;7:250–5 [DOI] [PubMed] [Google Scholar]
- 13.Van de Vreede MA, Wilson SG, Dooley MJ Intravenous potassium chloride prescribing and administration practices in Victoria: an observational study. Med J Aust 2008;189:575–7 [DOI] [PubMed] [Google Scholar]
- 14.Weiner ID, Wingo CS Hyperkalemia: a potential silent killer. J Am Soc Nephrol 1998;9:1535–43 [DOI] [PubMed] [Google Scholar]
- 15.Halperin ML, Kamel KS Potassium. Lancet 1998;352:135–40 [DOI] [PubMed] [Google Scholar]
- 16.Gennari FJ Hypokalemia. N Engl J Med 1998;339:451–8 [DOI] [PubMed] [Google Scholar]
- 17.Crop MJ, Hoorn EJ, Lindemans J, Zietse R Hypokalaemia and subsequent hyperkalaemia in hospitalized patients. Nephrol Dial Transplant 2007;22:3471–7 [DOI] [PubMed] [Google Scholar]
- 18.Allenby-Smith OC, Alexander RJ, Moffat CE, Carty NJ Back to basics: the impact of teaching on intravenous fluid prescribing. J Eval Clin Pract 2008;14:477–9 [DOI] [PubMed] [Google Scholar]


