Abstract
Purpose
To evaluate the long-term visual prognosis and complications of patients who received intravitreal Ozurdex injections for the treatment of macular edema (ME) due to retinal vein occlusion (RVO).
Methods
A total of 17 patients who received Ozurdex injections in our institution as part of the GENEVA study were recalled for examination. Recorded parameters included final visual acuity (VA), final retinal thickness by optical coherence tomography, persistence of ME, and the occurrence of any complications.
Results
Mean follow-up time was 50.5 months. Patients with branch RVO (BRVO) had a more favorable prognosis than central RVO (CRVO), and their mean VA had improved significantly, whereas the mean VA for the patients with CRVO did not improve significantly. Retinal thickness had reduced significantly in the whole group and in each subgroup separately. Complications included 10 patients with cataract progression, 1 with elevated intraocular pressure, and 1 with neovascularization and vitreous hemorrhage.
Conclusions
This is the first reported long-term evaluation of patients treated with Ozurdex. Our results indicate that it has favorable long-term safety profile, and may have a beneficial effect on the visual prognosis in BRVO even in the absence of continuous treatment. Further research is required to establish the optimal retreatment schedule for Ozurdex.
Keywords: Ozurdex, macular edema, retinal vein occlusion, long term, dexamethasone
Introduction
Retinal vein occlusion (RVO) is the second most common vascular retinopathy causing visual loss, surpassed only by diabetic retinopathy.1, 2, 3 The most common type is branch RVO (BRVO) with a prevalence of 0.6–1.1%, followed by central RVO (CRVO) with a prevalence of 0.1–0.4%.4, 5 Both RVO types are often associated with macular edema (ME) causing visual loss.6 The pathogenesis of ME in RVO is complex, and multiple factors have been implicated in it, including increased hydrostatic venous pressure, inflammation, endothelial dysfunction, and increased vascular permeability factors such as vascular endothelial growth factor (VEGF).2, 7
Treatment of ME in patients with RVO had been previously guided by the historical Branch Vein Occlusion Study and Central Vein Occlusion Study. According to the results of these trials, treatment included grid laser photocoagulation, if no spontaneous regression occurred 3 months after presentation for BRVO8, 9 and mere observation for CRVO.9, 10 However, significant advances in the management of ME in RVO have been made, and, currently, several effective treatment modalities are available. Intravitreal triamcinolone was demonstrated to be superior to observation for ME in CRVO,11, 12 and Ozurdex, an intravitreal dexamethasone implant (Allergan Inc., Irvine, CA, USA), has been approved for the treatment of ME in BRVO and CRVO.2, 13 Intravitreal ranibizumab (Lucentis; Genentech Inc., South San Francisco, CA, USA) has been shown to be an effective treatment for ME in both BRVO14 and CRVO.15 Bevacizumab (Avastin; Genentech Inc.) is also commonly used off-label for these indications.9
Ozurdex is a slow-release, intravitreal, biodegradable dexamethasone implant that is injected through the pars plana by a customized, single-used 22-gauge applicator.2 The active drug, dexamethasone, is a potent corticosteroid with anti-inflammatory and anti-VEGF effects, and its intravitreal administration bypasses the blood–retinal barrier, allowing high intraocular concentration with minimal systemic absorption.2, 16 The implant consists of a biodegradable copolymer matrix of lactic acid and glycolic acid, which enables the slow release of dexamethasone.2 It has been demonstrated that high concentrations of dexamethasone are sustained in the retina and vitreous during the first 2 months after the injection, and lower concentrations are sustained up to 6 months.17 Ozurdex has been proven effective, approved by the regulatory agencies in the United States and Europe, and is currently used in clinical practice for the treatment of ME associated with RVO and noninfectious posterior uveitis.2, 13, 18, 19 It has also been demonstrated to be effective for the treatment of diabetic ME in vitrectomized eyes.20
All published studies of Ozurdex focused on its short-term efficacy and safety, following patients for 6 or 12 months only.2, 13, 18, 19, 20 Information regarding the response to multiple treatments, the optimal retreatment interval, and long-term follow-up is lacking. The purpose of this study is to evaluate the long-term visual prognosis and complications of patients who received Ozurdex injections for the treatment of ME in RVO, as part of the GENEVA trial in our department.
Materials and methods
This observational study was approved by the Institutional Review Board of the Tel Aviv Medical Center, and all participants signed an informed consent before participation.
The study population included patients who were enrolled in our institution in the GENEVA study2 for the treatment of ME in RVO. As the study injections were masked, information regarding their content was requested from and provided by Allergan, Inc. Patients who received 700 or 350 μg Ozurdex injections at the masked initial phase or 700 μg Ozurdex injections at the open-label phase (after 180 days) were included, whereas patients who received only sham injections were excluded. The primary outcome was final visual acuity (VA), and secondary outcomes were final retinal thickness by optical coherence tomography (OCT), presence of ME, and the occurrence of any complications by the end of the follow-up period.
The study file for each included patient was reviewed for demographic information, background medical condition, diagnosis (BRVO or CRVO), VA, intraocular pressure (IOP), and retinal thickness by OCT throughout the study period, as well as lens status, additional retinal findings, and the occurrence of any complications during the study period. In addition, the patient charts were retrospectively reviewed from the time of study conclusion to the present, and information regarding additional treatments and complications was recorded. Finally, the patients were then summoned and underwent a complete ophthalmological examination, including best-corrected VA, applanation tonometry, anterior segment, lens status, and dilated fundus examination. Patients were questioned regarding the occurrence of any complications, use of any ocular medication, or need for any additional treatment or surgical procedure since the first Ozurdex injection. All the patients also underwent macular OCT imaging by Stratus OCT (Carl Zeiss Meditec AG, Jena, Germany) as performed in the GENVA study.2, 13 Comparisons of retinal thickness were performed for the central foveal location and the maximal macular thickness. The follow-up period was calculated from the time of the first Ozurdex injection.
For statistical analysis, all VA values were converted to the logMAR scale. According to Holladay21 and the University of Freiburg study group results,22 blindness was set at 0.00125/2.9 (decimal/logMAR), light perception at 0.0025/2.6, hand movements at 0.005/2.3, and counting fingers at 0.014/1.85.
Correlations between continuous variables were analyzed using Pearson's correlation coefficient, and t-test was used to analyze differences between groups. Because of small sample size, nonparametric analysis using the Mann–Whitney rank-sum test was performed. Data were analyzed using SPSS for windows version 17 (IBM, Chicago, IL, USA). A P-value of 0.05 was used to declare statistically significant difference between groups.
Results
A total of 28 patients were enrolled in the GENEVA study in our institution, 18 of whom received at least one Ozurdex injection and were eligible for this study. One patient was lost to follow-up, therefore our series consists of 17 patients. A summary of the patients' information is provided in Table 1.
Table 1. Summary of patient information (VA values are provided in logMAR units).
| Patient No. | Age at injection | Sex | Diagnosis | Number of Ozurdex injections | Initial VA | Final VA | VA change | Persistent ME | Cataract progression | Phaco (months) | Complications | Additional treatments administered during follow-up |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 52 | F | BRVO | 1 | 0.7 | 0.4 | 0.3 | No | No | No | None | None |
| 2 | 60 | F | BRVO | 2 | 0.6 | 0.477 | 0.123 | Yes | No | No | None | None |
| 3 | 61 | F | BRVO | 2 | 0.7 | 0.7 | 0 | Yes | No | No | None | Bevacizumab (X3), additional ozurdex injection |
| 4 | 62 | M | CRVO | 2 | 0.7 | 1.47 | −0.77 | Yes | Yes | Yes (25) | None | Argon laser photocoagulation, bevacizumab (X1) |
| 5 | 63 | M | BRVO | 1 | 1 | 0.151 | 0.849 | No | Yes | Yes (17) | None | Argon laser photocoagulation, bevacizumab (X5) |
| 6 | 64 | M | CRVO | 1 | 1 | 2.3 | −1.3 | N/A | Yes | Yes (64) | NV+VH | None |
| 7 | 65 | F | BRVO | 1 | 0.4 | 0.522 | −0.122 | Yes | No | No | Elevated IOP | Argon laser photocoagulation, bevacizumab (X2) |
| 8 | 67 | F | BRVO | 1 | 0.7 | 0.7 | 0 | No | Yes | No | None | None |
| 9 | 69 | F | BRVO | 2 | 0.6 | 0.3 | 0.3 | No | No | No | None | Argon laser photocoagulation, bevacizumab (X3) |
| 10 | 69 | M | BRVO | 1 | 1 | 0.7 | 0.3 | No | Yes | No | None | None |
| 11 | 69 | F | BRVO | 2 | 0.7 | 0.09 | 0.61 | No | No | No | None | Argon laser photocoagulation, bevacizumab (X8) |
| 12 | 70 | M | BRVO | 1 | 0.4 | 0.09 | 0.31 | No | No | No | None | None |
| 13 | 72 | F | BRVO | 1 | 0.4 | 0.3 | 0.1 | No | Yes | No | None | Bevacizumab (X2) |
| 14 | 76 | M | BRVO | 1 | 0.778 | 0.3 | 0.478 | No | Yes | Yes (29) | None | Additional ozurdex injection |
| 15 | 78 | F | CRVO | 2 | 0.7 | 0.522 | 0.178 | No | Yes | No | None | None |
| 16 | 82 | M | BRVO | 2 | 0.7 | 0.875 | −0.175 | No | Yes | Yes (25) | None | None |
| 17 | 83 | M | BRVO | 1 | 0.875 | 1 | −0.125 | No | Yes | Yes (10) | None | Argon laser photocoagulation |
Abbreviations: BRVO, branch retinal vein occlusion; CRVO, central retinal vein occlusion; F, female; IOP, intraocular pressure; M, male; ME, macular edema; N/A, not available; NV, neovascularization; phaco, phacoemulsification; VA, visual acuity; VH, vitreous hemorrhage.
The 17 patients in this study included 8 (47%) men and 9 (53%) women, with a mean age of 68.35±8.14 years (range 52–83) at the time of their first Ozurdex injection. In 14 (82.3%) of them, ME was secondary to BRVO, and in the remaining 3 (17.7%), ME was secondary to CRVO. At the time of the first injection, 3 (35.3%) patients were injected with 700 μg Ozurdex, 9 (53%) with 350 μg Ozurdex, and 2 (11.7%) received sham injections. Nine (53%) patients received a 700-μg Ozurdex injection at the open-label phase of the study. Overall, during the study period, 10 (58.8%) patients received one Ozurdex injection and 7 (41.2%) received two injections. The follow-up period from the first Ozurdex injection was 50.5±17.3 months (range 28–67 months).
Background medical conditions included hypertension (HTN) in 11 (64.7%) patients and diabetes mellitus (DM) in 5 (29.4%) of them. None of the patients received any treatment for ME before their enrollment in the study. After conclusion of the study, 9 (53%) of the patients received additional treatments for persisting ME. Additional treatments included grid laser photocoagulation in 6 (35.3%) patients, intravitreal bevacizumab injections in 7 (41.1%) patients, and an additional 700 μg Ozurdex injection in 2 (11.7%) patients. None were treated with intravitreal ranibizumab because of its significantly higher cost.
Analysis of the whole group of patients
When the whole group of patients was analyzed together, mean initial VA was 0.70±0.19 logMAR (approximately 20/100, range 0.40–1.00). Mean final VA was 0.64±0.55 logMAR (approximately 20/87, range 0.09–2.30). The mean change in VA at the end of the follow-up period was 0.06±0.50 logMAR, and thus, there was no statistically significant difference between the initial and final VA. VA had improved in 10 (58.8%) patients, remained the same in 2 (11.7%) of them, and deteriorated in the remaining 5 (29.4%). Six (35.2%) patients achieved final VA of 0.30 logMAR (20/40) or better, and only 2 (11.7%) patients had final VA worse than 1.00 logMAR (20/200) (Tables 1 and 2).
Table 2. Comparison between mean initial and final values of VA, IOP and retinal thickness (t-test).
| Parameter | VA (logMAR) | IOP (mm Hg) | Central foveal retinal thickness (μm) | Maximal macular retinal thickness (μm) |
|---|---|---|---|---|
| Initial | 0.70 | 15.5 | 496 | 573 |
| Final | 0.64 | 14.7 | 277 | 326 |
| P-value | >0.05 | >0.05 | <0.01 | <0.01 |
Abbreviations: IOP, intraocular pressure; VA, visual acuity.
Final VA and the change in VA did not correlate significantly with age, sex, presence of HTN or DM, number of Ozurdex injections, or administration of additional treatments during the follow-up period. A trend was noted between better initial VA and better final VA, but was not statistically significant (P=0.07).
At baseline, mean OCT retinal thickness was 496±162 μm at the center of the fovea and 573±119 μm at the macular area with maximal thickness. At the end of the follow-up period, only 4 (23.5%) of the patients still had persistent ME demonstrated by OCT or clinical examination. Retinal thickness had reduced significantly to 277±143 μm at the center of the fovea and 326±129 μm at the macular area with maximal thickness (P<0.01 for both locations). These values represent a mean reduction of 44.2% and 43.1% in retinal thickness, respectively (Table 2).
Analysis by initial diagnosis
Our series included 14 patients with BRVO and only 3 patients with CRVO, and patients with CRVO had a poorer visual prognosis than those with BRVO (Table 3). Two of these three patients with CRVO suffered further reduction in VA, one of them due to neovascularization complicated by vitreous hemorrhage (VH) and the other due to severe persistent ME, and none of them achieved final VA of 20/40 or better. A statistically significant lower mean final VA and VA change values were demonstrated for patients with CRVO compared with BRVO (P=0.023 and 0.045, respectively). Patients with BRVO had a mean initial VA of 0.68±0.19 logMAR (approximately 20/95, range 0.40–1.00) and a mean final VA of 0.47±0.28 logMAR (approximately 20/60, range 0.09–0.875). Mean change in VA was 0.21±0.29 logMAR, and represents a statistically significant improvement (P=0.03) of about two lines (Figure 1).
Table 3. Comparison of the visual prognosis between patients with BRVO and CRVO.
| Diagnosis | Number of patients | Mean initial VA (logMAR) | Mean final VA (logMAR) | Mean change in VA (logMAR) |
|---|---|---|---|---|
| BRVO | 14 | 0.68 | 0.47 | 0.21 |
| CRVO | 3 | 0.8 | 1.43 | −0.63 |
| P-value | 0.36 | 0.003 | 0.004 |
Abbreviations: BRVO, branch retinal vein occlusion; CRVO, central retinal vein occlusion; VA, visual acuity.
Figure 1.
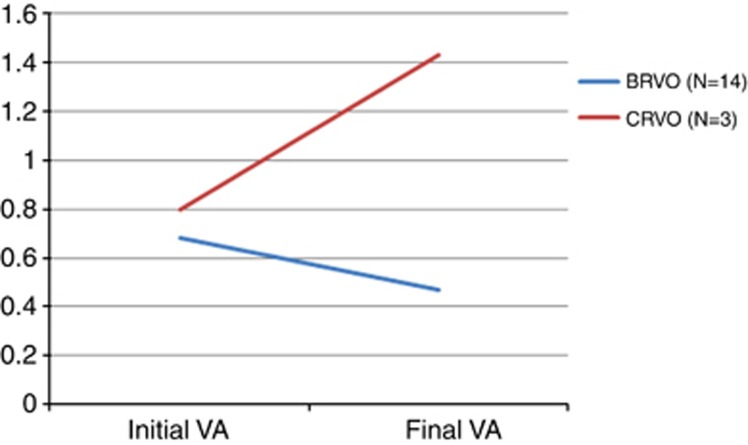
Comparison of initial and final VA between patients with BRVO and CRVO. Patients with BRVO enjoyed a statistically significant improvement by the end of the follow-up period (VA is presented in logMAR units.)
Reduction of retinal thickness at the center of the fovea and at the macular area with maximal thickness was significant for both patients with BRVO and CRVO when analyzed separately (P<0.01). Patients with BRVO had baseline mean OCT retinal thickness of 465±139 μm at the center of the fovea and 554±88 μm at the macular area with maximal thickness. Retinal thickness had reduced significantly to 238±50 μm at the center of the fovea and 291±53 μm at the macular area with maximal thickness (P<0.01 for both locations). These values represent a mean reduction of 48.9% and 47.5% in retinal thickness, respectively.
Complications
Mean initial IOP was 15.5±2.1 mm Hg and the mean final IOP was 14.7±2.3 mm Hg. There was no statistically significant difference between these values (Table 2). Only one (5.9%) patient had IOP elevation over 21 mm Hg throughout the follow-up period and was managed successfully by topical treatment.
All patients were phakic at the time of enrollment. During the follow-up period, 10 (58.8%) had cataract progression, which was documented in their retrospectively reviewed charts. Cataract progression was not graded according to any classification. Six patients (35.2%) had undergone phacoemulsification, and the mean period of time between the Ozurdex injection and the procedure was 28.3±18.7 months (range 10–64 months). Four of these patients received one Ozurdex injections and two received two injections.
One (5.9%) patient with CRVO developed retinal neovascularization and was further complicated by vitreous hemorrhage. At the examination performed for this study, VA was hand movement, and the patient was referred for vitrectomy. No neovascularization at the disc, retina, or iris was found in any of the other patients. No retinal detachment, endophthalmitis, or any other complication were encountered in this study. Remnants of the intravitreal implant were not observed in any of the patients.
Discussion
This is the first study evaluating the long-term prognosis after treatment with Ozurdex for ME in RVO. When the whole group of patients was analyzed together, VA did not change significantly over a mean follow-up period of over 4 years. However, patients with BRVO fared much better than those with CRVO (Figure 1), and in this subgroup, VA did improve in a statistically significant manner. This finding is not surprising in view of the better natural history and better response to various treatment modalities of BRVO as compared with CRVO.14, 15 Although VA improvement occurs frequently in BRVO even without any treatment, in the long-term, it rarely improves beyond 20/40.23 In our series, 6 out of 14 (42.8%) patients with BRVO achieved final VA of 20/40 or better. CRVO has been shown to have a worse natural history, with most cases suffering further VA loss.24 Treatment with Ozurdex has been demonstrated to be effective for ME associated with both BRVO and CRVO.2, 9, 13, 18 However, these studies focused on the short-term efficacy of this treatment (up to 12 months of follow-up), with a maximum number of two injections, given at a 6-month interval, a period which may be beyond the effect of the drug. Although 53% of the patients in this series received additional treatments for ME after conclusion of the GENEVA study protocol (Table 1), none were treated regularly after its conclusion. Therefore, despite the effect of the Ozurdex treatment, final VA also reflects considerably the natural history of the baseline diagnosis.
Treatment with a single Ozurdex injection has been demonstrated to reduce macular retinal thickness.2, 9, 13 This reduction was statistically significant after 90 days but not after 180 days.2 In our series, retinal thickness at the end of follow-up had significantly reduced by 44.2% at the center of the fovea and by 43.1% at the macular area with maximal thickness (Table 2). Persistent ME was demonstrated in 4 (23.5%) patients. This significant reduction in retinal thickness did not correlate with final VA. This may be explained that it results not only from resolution of the ME but also from retinal atrophy caused by the ME, especially in cases of CRVO.
Cataracts are a known complication of all types of steroid administration routes, and occur more commonly in patients with long-term steroid use.25, 26, 27, 28 Rate of cataract formation 12 months after Ozurdex injection had been previously reported to be as high as 29.8%, depending on the number and dosage of injections.13 Cataract advancement was documented in 10 (58.8%) patients in our series, and 6 (35.2%) of them had undergone phacoemulsification. Mean time between the Ozurdex injection and phacoemulsification was 28.3 months in our series, with only one patient who underwent the procedure within 1 year of the injection. Our results indicate that cataract formation may be a later complication of Ozurdex, occurring in higher rates after more than 12 months since the first injection. The safety profile in our series was very good. Ozurdex treatment did not cause a significant difference in IOP over the long follow-up period. Only one (5.9%) patient had elevated IOP and was managed successfully with topical treatment. Rates of IOP elevation were higher in the short term after intravitreal injection of both Ozurdex and triamcinolone.2, 11, 12, 13
One patient with CRVO suffered significant VA loss due to retinal neovascularization complicated by VH. The GENEVA study did not differentiate between ischemic and non-ischemic CRVO at baseline,2 but it has been established that approximately one-third of non-ischemic CRVO eyes convert to ischemic CRVO within 3 years, and more at significant risk of neovascular complications.24 Therefore, this unfavorable final VA may not be related to the Ozurdex treatment.
Limitations of this study include its small series size and, especially, the small number of patients with CRVO. In addition, 53% of the patients received additional treatments for their ME during the follow-up period, and their effects may confound that of the initial Ozurdex treatment. However, we note that except for one patient who was lost to follow-up, this was the maximum number of patients available for this study, and emphasize that additional treatments did not correlate with any of the parameters recorded. Another limitation is that the degree of cataract progression and cataract type were not graded and documented, and therefore, it is not possible to assess the significance of their effect on the final VA.
Despite the limitations, this study is of clinical importance because it is the first to investigate the long-term prognosis and complications in patients treated with Ozurdex for ME in RVO. Its short-term safety and efficacy have been established, and Ozurdex has rightfully earned its place in the arsenal of treatments for RVO that has grown over the recent years.2, 9, 13, 18, 29 Our results indicate that it is well tolerated with an excellent long-term safety profile, with cataract progression being the most common complication over time. Long-term efficacy was lower than that found in the short term. This is not surprising because no patient was treated on a regular repeated basis throughout the follow-up period, and the clinical course of the patients in this series undoubtedly reflects the natural history of RVO to some extent. However, it is important to note that even without regular and repeated treatments during the long-term follow-up period, patients with BRVO treated with Ozurdex had a better visual prognosis than that expected without any intervention.23
In conclusion, treatment with Ozurdex for ME in RVO has favorable long-term safety profile and a positive effect on the final visual prognosis in patients with BRVO. Most modalities in current clinical use for ME in RVO require repeated treatments.9, 10, 11, 12, 13, 29 Further studies are required to establish the optimal retreatment schedule for Ozurdex, but its long half-life may have a significant advantage over other options, allowing for a significantly longer interval between injections and improved patient compliance. Additional future research comparing the long-term safety and efficacy of Ozurdex with other treatment modalities is also required.
The authors declare no conflict of interest.
References
- Yau JW, Lee P, Wong TY, Best J, Jenkins A. Retinal vein occlusion: an approach to diagnosis, systemic risk factors and management. Intern Med J. 2008;38:904–910. doi: 10.1111/j.1445-5994.2008.01720.x. [DOI] [PubMed] [Google Scholar]
- Haller JA, Bandello F, Belfort R, Blumenkranz MS, Gillies M, Heier J, et al. Randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with macular edema due to retinal vein occlusion. Ophthalmology. 2010;117:1134–1146. doi: 10.1016/j.ophtha.2010.03.032. [DOI] [PubMed] [Google Scholar]
- Rogers S, McIntosh RL, Cheung N, Lim L, Wang JJ, Mitchell P, et al. The prevalence of retinal vein occlusion: pooled data from population studies from the United States, Europe, Asia and Australia. Ophthalmology. 2010;117:313–319. doi: 10.1016/j.ophtha.2009.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell P, Smith W, Chang A. Prevalence and associations of retinal vein occlusion in Australia: the blue mountains eye study. Arch Ophthalmol. 1996;114:1243–1247. doi: 10.1001/archopht.1996.01100140443012. [DOI] [PubMed] [Google Scholar]
- Klein R, Klein BE, Moss SE, Meuer SM. The epidemiology of retinal vein occlusion: the beaver dam eye study. Trans Am Ophthalmol Soc. 2000;98:133–143. [PMC free article] [PubMed] [Google Scholar]
- Rehak J, Rehak M. Branch retinal vein occlusion: pathogenesis, visual prognosis and treatment modalities. Curr Eye Res. 2008;33:111–131. doi: 10.1080/02713680701851902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campochiaro PA, Hafiz G, Shah M, Nguyen QD, Ying H, Do DV, et al. Ranibizumab for macular edema due to retinal vein occlusions: implication of VEGF as a critical stimulator. Mol Ther. 2008;16:791–799. doi: 10.1038/mt.2008.10. [DOI] [PubMed] [Google Scholar]
- The Branch Vein Occlusion Study Group Argon laser photocoagulation for macular edema in branch retinal vein occlusion. Am J Ophthalmol. 1984;98:271–282. doi: 10.1016/0002-9394(84)90316-7. [DOI] [PubMed] [Google Scholar]
- Chan A, Leung LS, Blumenkranz MS. Critical appraisal of the clinical utility of the dexamethasone intravitreal implant (Ozurdex) for the treatment of macular edema related to branch retinal vein occlusion or central retinal vein occlusion. Clin Ophthalmol. 2011;5:1043–1049. doi: 10.2147/OPTH.S13775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Central Vein Occlusion Study Group Evaluation of grid pattern photocoagulation for macular edema in central vein occlusion: the Central Vein Occlusion Study Group M report. Ophthalmology. 1995;102:1425–1433. doi: 10.1016/s0161-6420(95)30849-4. [DOI] [PubMed] [Google Scholar]
- Ip MS, Scott IU, Van Veldhuisen PC, Oden NL, Blodi BA, Fisher M, et al. A randomized trial comparing the efficacy and safety of intravitreal triamcinolone with observation to treat vision loss associated with macular edema secondary to central retinal vein occlusion: the standard care vs corticosteroid for retinal vein occlusion (SCORE) study report 5. Arch Ophthalmol. 2009;127:1101–1114. doi: 10.1001/archophthalmol.2009.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott IU, Ip MS, Van Veldhuisen PC, Oden NL, Blodi BA, Fisher M, et al. A randomized trial comparing the efficacy and safety of intravitreal triamcinolone with standard care to treat vision loss associated with macular edema secondary to branch retinal vein occlusion: the standard care vs corticosteroid for retinal vein occlusion (SCORE) study report 6. Arch Ophthalmol. 2009;127:1115–1128. doi: 10.1001/archophthalmol.2009.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haller JA, Bandello F, Belfort R, Blumenkranz MS, Gillies M, Heier J, et al. Dexamethasone intravitreal implant in patients with macular edema related to branch or central retinal vein occlusion. Ophthalmology. 2011;118:2453–2460. doi: 10.1016/j.ophtha.2011.05.014. [DOI] [PubMed] [Google Scholar]
- Campochiaro PA, Heier JS, Feiner L, Gray S, Saroj N, Rundle AC, et al. Ranibizumab for macular edema following branch retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology. 2010;117:1102–1112. doi: 10.1016/j.ophtha.2010.02.021. [DOI] [PubMed] [Google Scholar]
- Brown DM, Campochiaro PA, Singh RS, Li Z, Gray S, Saroj N, et al. Ranibizumab for macular edema following central retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology. 2010;117:1124–1133. doi: 10.1016/j.ophtha.2010.02.022. [DOI] [PubMed] [Google Scholar]
- Goldfien A.Adrenocorticosteroids and adrenocortical antagonistsIn: Katzung BG, (eds).Basic and Clinical Pharmacology6th ed.Prentice Hall International: London; 1995592–607. [Google Scholar]
- Chang-Lin JE, Attar M, Acheampong AA, Robinson MR, Whitcup SM, Kuppermann BD, et al. Pharmacokinetics and pharmacodynamics of a sustained-release dexamethasone intravitreal implant. Invest Ophthalmol Vis Sci. 2011;52:80–86. doi: 10.1167/iovs.10-5285. [DOI] [PubMed] [Google Scholar]
- Herrero-Vanrell R, Cardillo JA, Kuppermann BD. Clinical applications of the sustained-release dexamethasone implant for the treatment of macular edema. Clin Ophthalmol. 2011;5:139–146. doi: 10.2147/OPTH.S15783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowder C, Belfort R, Lightman S, Foster CS, Robinson MR, Schiffman RM, et al. Dexamethasone intravitreal implant for noninfectious intermediate or posterior uveitis. Arch Ophthalmol. 2011;129:545–553. doi: 10.1001/archophthalmol.2010.339. [DOI] [PubMed] [Google Scholar]
- Boyer DS, Faber D, Gupta S, Patel SS, Tabandeh H, Li XY, et al. Dexamethasone intravitreal implant for treatment of diabetic macular edema in vitrectomized patients. Retina. 2011;31:915–923. doi: 10.1097/IAE.0b013e318206d18c. [DOI] [PubMed] [Google Scholar]
- Holladay JT. Proper method for calculating average visual acuity. J Refract Cat Surg. 1997;13:388–391. doi: 10.3928/1081-597X-19970701-16. [DOI] [PubMed] [Google Scholar]
- Schulze-Bonsel K, Feltgen N, Burau H, Hansen L, Bach M. Visual acuities ‘hand motion' and ‘counting fingers' can be quantified with the freiburger visual acuity test. Invest Ophthalmol Vis Sci. 2006;47:1236–1240. doi: 10.1167/iovs.05-0981. [DOI] [PubMed] [Google Scholar]
- Rogers SL, McIntosh RL, Lim L, Mitchell P, Cheung N, Kowalski JW, et al. Natural history of branch retinal vein occlusion: an evidence-based systematic review. Ophthalmology. 2010;117:1094–1101. doi: 10.1016/j.ophtha.2010.01.058. [DOI] [PubMed] [Google Scholar]
- McIntosh RL, Rogers SL, Lim L, Cheung N, Wang JJ, Mitchell P, et al. Natural history of central retinal vein occlusion: an evidence-based systematic review. Ophthalmology. 2010;117:1113–1123. doi: 10.1016/j.ophtha.2010.01.060. [DOI] [PubMed] [Google Scholar]
- James ER. The etiology of steroid cataract. J Ocul Pharmacol Ther. 2007;23:403–423. doi: 10.1089/jop.2006.0067. [DOI] [PubMed] [Google Scholar]
- Van Kooij B, Rothova A, de Vries P. The pros and cons of intravitreal triamcinolone injections for uveitis and inflammatory cystoid macular edema. Ocul Immunol Inflamm. 2006;14:73–85. doi: 10.1080/09273940500545684. [DOI] [PubMed] [Google Scholar]
- Carnahan MC, Goldstein DA. Ocular complications of topical, peri-ocular, and systemic corticosteroids. Curr Opin Ophthalmol. 2000;11:478–483. doi: 10.1097/00055735-200012000-00016. [DOI] [PubMed] [Google Scholar]
- Renfro L, Snow JS. Ocular effects of topical and systemic steroids. Dermatol Clin. 1992;10:505–512. [PubMed] [Google Scholar]
- Bressler NM, Schachat AP. Management of macular edema from retinal vein occlusions: you can never have too many choices. Ophthalmology. 2010;117:1061–1063. doi: 10.1016/j.ophtha.2010.03.037. [DOI] [PubMed] [Google Scholar]


