Parents of pediatric oncology patients participated in a proactive risk assessment method, identifying processes that pose a risk for medication errors involving home oral chemotherapy.
Abstract
Purpose:
Observational studies describe high rates of errors in home oral chemotherapy use in children. In hospitals, proactive risk assessment methods help front-line health care workers develop error prevention strategies. Our objective was to engage parents of children with cancer in a multisite study using proactive risk assessment methods to identify how errors occur at home and propose risk reduction strategies.
Methods:
We recruited parents from three outpatient pediatric oncology clinics in the northeast and southeast United States to participate in failure mode and effects analyses (FMEA). An FMEA is a systematic team-based proactive risk assessment approach in understanding ways a process can fail and develop prevention strategies. Steps included diagram the process, brainstorm and prioritize failure modes (places where things go wrong), and propose risk reduction strategies. We focused on home oral chemotherapy administration after a change in dose because prior studies identified this area as high risk.
Results:
Parent teams consisted of four parents at two of the sites and 10 at the third. Parents developed a 13-step process map, with two to 19 failure modes per step. The highest priority failure modes included miscommunication when receiving instructions from the clinician (caused by conflicting instructions or parent lapses) and unsafe chemotherapy handling at home. Recommended risk assessment strategies included novel uses of technology to improve parent access to information, clinicians, and other parents while at home.
Conclusion:
Parents of pediatric oncology patients readily participated in a proactive risk assessment method, identifying processes that pose a risk for medication errors involving home oral chemotherapy.
Introduction
Oral chemotherapy is increasingly used in cancer care, but it poses novel patient safety risks.1–4 The use of oral chemotherapy at home can be highly complex, with error-prone processes, particularly among pediatric patients. This includes the need for different medications at various intervals, frequent adjustments in dosing, parents' understanding of dosing calculations, parent administration,1,5 use of liquid formulations6,7 and cutting or crushing chemotherapy tablets. Estimates of adherence to oral chemotherapy range from 20% to 100%.8,9,10 In a review of 1,379 medical records from outpatient visits to oncology clinics, we found that 19% of pediatric visits had a medication error compared with 7% in adults, a difference explained entirely by a high error rate in home medication administration.2 Because parents are in charge of the oral chemotherapy use process at home, their input is essential to develop effective interventions to prevent oral chemotherapy–related errors in this setting.
Proactive risk assessment techniques are used by hospitals and in other industries to understand highly complex, error-prone systems.11 The Joint Commission on Cancer requires hospitals to perform proactive risk assessments regularly.12 One type of proactive risk assessment technique is failure modes and effects analysis (FMEA). The FMEA method was developed in industry to engage front-line workers for the purposes of understanding the ways a process can fail and developing strategies to prevent such failures.13,14 In medicine, FMEA teams typically are multidisciplinary and include health care professionals and clerical personnel who have first-hand knowledge of how medical errors may occur and who then develop viable risk assessment strategies.15 To our knowledge, FMEAs have never been performed by teams that consist of patients or family members.
Our objective was to engage parents of children with cancer in FMEA teams, to identify how errors occur in home oral chemotherapy use, and to propose risk reduction strategies. Our FMEAs focused on the implementation of a dose change initiated by the patient's oncology clinician, because our prior research identified several serious errors when oral chemotherapy doses were changed.2 We performed this study for three reasons: to identify key vulnerabilities in home oral chemotherapy management in children with cancer, to develop potential strategies for reducing errors, and to test the feasibility of using FMEAs to partner with parents to prevent errors.
Methods
Setting
We selected three pediatric oncology clinics, all with academic affiliations, in different clinical settings in the northeast and southeast United States. Clinic volumes varied from 50 patients annually with five prescribers to 2,000 patients annually with 37 prescribers. All sites used an electronic health record for ordering medications and utilized both on- and off-site pharmacies. Two sites utilized paper medication calendars for parents to use at home; the third site used a paper home medication list. Two sites used visiting nurses to teach parents how to use medications at home. The study was approved by the institutional review boards at each site.
FMEA
Recruitment.
We recruited English-speaking parents of children (0 to 16 years) with cancer drawn from a pool of parents who participated in a prior observational study of home medication use (Walsh, submitted for publication) The population who participated in the observational study was 87% mothers and 83% with some college education; the population had an adequate level of health literacy (as assessed using the Short Test of Functional Health Literacy). We invited parents by phone to participate in a discussion about how medications are used at home in children with cancer and how to prevent errors in home medication use. The FMEAs were scheduled when convenient for interested parents. Parents were also compensated for their time.
Process.
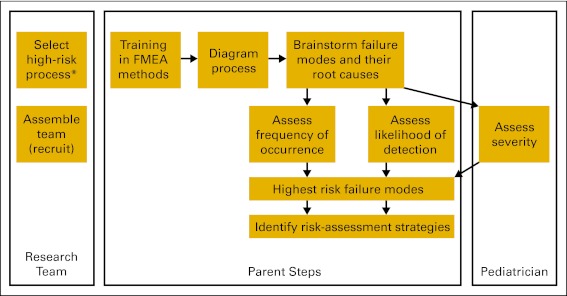
Any FMEA process is based on a target high-risk process (Figure 1). The study team selected parent administration of oral chemotherapy at home after a dose change as the target process. In our prior research, we found that a change in dosing was a common source of dangerous medical errors in outpatient cancer care. (Walsh, submitted for publication).
Figure 1.
Failure modes and effect analysis (FMEA) steps. Parents at each study site performed all parent steps. The second and third FMEA sites used the process diagram and failure modes from the first site as a starting point. (*) We chose to target the home use of a medication after a change in the dose of the medication, because our previous research identified changes in dose as an area at risk for common and dangerous medication errors.
The first FMEA was conducted at one institution over the course of three meetings. At the first meeting, parents were trained in the FMEA process, using a PowerPoint presentation and written materials at the eighth-grade literacy level. They then practiced the FMEA methods using an example from normal daily activities- the process of waking up in the morning to leave for work or to take children to school.16 Parents then worked together to map the steps involved in administering oral chemotherapy at home after a change has been made in the dose.
At the second meeting, parents brainstormed potential failure modes (ie, places on the process diagram where things could go wrong) and identified their root causes. For example, in the process of waking up to go to work, a failure mode might be the alarm not going off, and the root cause of that failure might be a power outage.
At the third meeting, parents prioritized failure modes according to established methods.17 On the basis of their personal experiences, parents assigned numbers to each failure mode on a 1 to 10 rating scale for likelihood of detection before reaching the patient (1 = highly likely; 10 = highly unlikely) and frequency of occurrence (1 = very infrequent; 10 = very frequent). Disagreements were resolved through discussion. The third rating, severity of potential harm (1 = no harm; 10 = terminal injury/death) was assigned by a clinician (K.E.W. or S.W.) for each site. Detectability, frequency of occurrence, and severity scores were multiplied to develop a risk priority number for each failure mode. For example, if a power outage caused someone to be late to work, it might score a 1 for frequency of occurrence, 8 for severity, and 8 for detectability. This would result in a risk priority number of 64 (8 × 1 × 8). This then produced a ranking of overall risk for each identified failure mode. The group brainstormed risk assessment strategies for the 10 failure modes with highest risk priority number. The group discussed the merits of each.
At the other two sites, because their FMEAs began with the process map and failure modes developed at the first site, the general approach and content of the three meetings was condensed into a single meeting. Parents used the process map and failure modes identified by the first group and adapted these materials based on local processes. Specifically, parents reviewed the process map from the first site's FMEA and added or removed steps based on their own environment and experiences. Similarly, they reviewed failure modes listed by the first site's FMEA and added additional items. Parents at each site prioritized failure modes by rating frequency of occurrence and detectability. Each FMEA concluded with a discussion of risk reduction strategies, targeting the 10 failure modes with the highest risk priority number.
Results
Parent Participants
At the first site, we approached 27 eligible parents, of whom 12 expressed interest, 10 were available on the scheduled date, and four participated (three attended meeting 1, and four attended meetings 2 and 3). At the second site we approached 18 eligible parents, of whom four expressed interest, four were available on the scheduled date, and four participated. At the third site, we approached 40 eligible parents, of whom 15 expressed interest, 12 were available on the scheduled date, and 10 participated. One participant was a father, the rest were mothers.
Home Oral Chemotherapy Administration
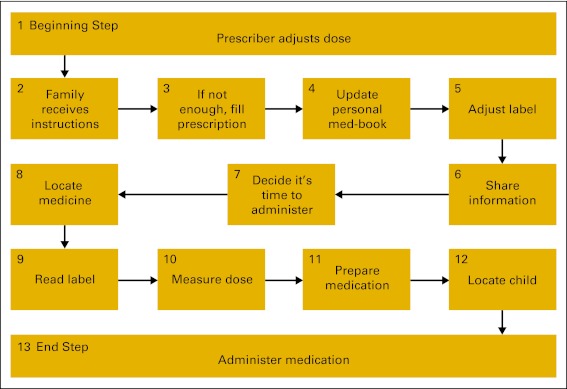
We began by having parents describe existing processes for home oral chemotherapy administration after the doctor changes the home medication dose. The first step (change in medication dose) and the last step (medication administration) were identified by the study team. At the first study site, parents developed a process map that included 12 steps. At the second site, parents agreed that they used the same process described by the first site. At the third site, parents added one additional step “locate medication” (Figure 2).
Figure 2.
Final process map. Steps 1 (beginning step) and 13 (end step) were identified by the study team.
Parents at all three sites reported using some form of a “personal medication book” (step 4), a paper binder used to keep track of their children's medications and any related changes. Although parents did not bring this book to clinic appointments, they updated it with any dosing adjustments on returning home and used it as reference when administering medications. About this personal medication book one parent said, “This is everything that could ever possibly happen to my son. It's always with me.” However, the type of book used (calendar versus binder) and content of the books varied between parents.
Some parents reported writing the new dose on the label of the bottle of chemotherapy they had at home, which they called “adjust label” (step 5). For example, if the child had been taking 6-mercaptopurine 50 mg daily and the dose was reduced to 25 mg, some parents would write the new dose on the bottle. The parent who went to the doctor's appointment where the dose was changed would communicate with other caregivers (eg, other parent, visiting nurse) about the change in the medication dose, so that the correct dose was administered at home (step 6, “share information”). In discussing “read the label” (step 9) one parent reported, “I don't know which directions to follow. One of our medications said not to take it with an antacid. My child is on Prilosec twice a day. I called the clinic and they said it was OK. Sometimes the directions conflict.”
For several of the major steps in the process map, minor steps were identified in a more granular analysis. (Appendix Table A1, online only) For example, for the major step 2, “family receives information,” two minor steps were identified: the clinicians provided the information and the family understood the information. Both of these minor steps had different potential errors.
Failure modes.
Parents identified 69 failure modes that could occur in the process of home use of oral chemotherapy after a change in medication dose. The step that had the most failure modes was step 3, “fill prescription.” This step was broken into three parts: prescribing problems (with one example failure mode: wrong dose on prescription), dispensing problems (with one example failure mode: wrong dose dispensed), and family problems (with one example failure mode: unable to pay copay). Dispensing problems had 10 failure modes, the most of any step. One failure mode involved forgetting to refill the prescription. One mother stated “They only give me a two week supply and I'm forever keeping track. There's a lot of these problems.” Another failure mode was confusion over generic and brand names. One parent commented “They have a generic of the pill. Then the next time you go to get it filled it's still a generic but a different generic.” Overall, 26% of failure modes were related to problems with communication. For example, a parent said “If you have a dose change, then you weren't home that night and he [child's father] didn't know about it,” then the incorrect dose was given.
There were three failure modes that were ranked high-risk at all three study sites. The first was misunderstanding physician instructions about changes in medication doses, either through misunderstanding on the part of the parent or conflicting instructions being received from different clinicians. The second was the unsafe handling of chemotherapy medications at home. Many parents reported that they were unaware that they were supposed to wear protective gear such as gloves when handling chemotherapy. Others reported problems with safely cutting chemotherapy tablets at home. One mother stated, “I asked the pharmacist to cut the chemotherapy and he said, ‘No way honey,’ so I had to go home and cut it myself in my kitchen.” The third failure mode highly ranked at all sites was the child refusing to take the medication or vomiting the medication for several days.
Strategies to reduce risk at home.
Parent recommendations for reducing the risk of highly ranked failure modes fell into three general categories: (1) streamlining processes, (2) eliciting information and support from clinicians, and (3) eliciting information and support from other parents (Table 1). Parents recommended streamlining processes that were already in place to improve their accuracy or consistency. For example, parents suggested that if they regularly received an updated home medication list or calendar, then this would reduce the risk of misunderstanding clinician instructions. In addition, it would reduce the risk of miscommunication between a parent who attended the clinic appointment and other caregivers at home. For several communication problems, parents recommended written materials to supplement verbal communication to reduce the risk of misunderstanding and facilitate transmittal of new dosing information to other caregivers at home. One parent said, “There is so much to communicate about during the clinic visit, about dose changes or whatever, besides the prescription. Is there not an opportunity for a recap, like a followup e-mail with a summary of the visit?” Parents suggested several possibilities, including after-visit summaries, Web-based information, an e-mail of the clinician's dictated note, or a nurse visit. Finally, parents were enthusiastic about the possibility of receiving additional support and information from other parents via an Internet chat room or listserve. Parents imagined a parent-led “WebMD” that is monitored by a clinician, to share information between parents about the home care of a child with cancer. One parent said, “There is no reason each parent should have to reinvent the wheel. You can't expect the doctor to communicate every trick that works because they are never at the houses.”
Table 1.
Highest Risk Failure Modes and Recommended Strategies to Reduce Risks
| Modes and Strategies |
| Highest risk failure modes |
| Miscommunication when the clinician instructs family to change the dose |
| Family misunderstands |
| Multiple conflicting instructions from different staff |
| Miscommunication when telling other caregivers at home about a change in medication dose |
| Confusion about timing with respect to food, bed time, other pills leads to a mistake |
| Person handling chemotherapy at home has not been told to wear gloves and does not do so |
| Child refuses to take or vomits medication for several days |
| Incorrrect dose measured because wrong equipment used |
| One home caregiver administers the medication when unaware that someone else has already given the medication |
| On admission, the hospital does not carry oral chemotherapy and the family did not bring theirs from home |
Recommended strategies to reduce risks
|
Discussion
To our knowledge, this is the first study to engage parents or patients in FMEA teams designed to reduce the risk of home chemotherapy administration errors. Parents quickly understood the method and enthusiastically participated. They identified key vulnerabilities in the process of managing a change in the dose of oral chemotherapy medication, an area prone to dangerous medical errors. These included several communication failures, parent failure to use proper chemotherapy handling technique, and a child's refusal or vomiting of medications. Parents recommended clinicians use written information and technology to improve parent access to information, clinicians, and other parents when and where they need it: in the home.
The proactive risk assessment methods we used successfully engaged parents in error-prevention research. These methods are designed to bring the care team together and place it in charge of the process. As key members of the outpatient health care team, and experts in home medication use, we found that parents quickly understood the methods and readily engaged in the process. Proactive risk assessment methods, such as an FMEA, may be a valuable tool in patient-centered error prevention research in the future.
Whereas previous studies of outpatient error have examined the impact of low health literacy on patient safety, parents in our study described conflicting messages and slips in communication, unrelated to parental knowledge, in the clinic and at home. This is consistent with observational studies from the inpatient and outpatient settings, where errors are often related to miscommunication.18 (Walsh, submitted for publication). Parents identified the reliance on verbal communication as the primary source of information about home medication use as a key vulnerability. In addition to addressing low health literacy, parents proposed using written materials to anchor verbal discussion about medication use and to avoid conflicting or incorrect verbal communication in the clinic or at home.
Several of the risk-assessment strategies parents suggested would involve health information technology to support home care. In adult patients with chronic conditions, interventions that make use of patient portals (Web-based access from home to the electronic medical records, with secure messaging to the health care team) have been shown to improve patient health.19,20 The use of health information technology has also been shown to support home care in children with chronic conditions.21 Health information technology may prevent many of the failures identified by parents in our study, by providing access to information and support from the health care team in the home when problems arise.
The process map that our parents developed did not include a mechanism for providing feedback to the prescriber about medication use at home. In the hospital, redundancy is a common strategy used to mitigate error. For example, nurses and pharmacists double-check physicians' medication orders. In prior studies, we and others have found little communication with clinicians about problems in home medication use.22,23,24 This communication failure perpetuates errors, rather than intercepting them in time to mitigate the duration or severity of injury. Future interventions should incorporate communication with the outpatient clinician regarding successes or failures in home medication use into routine processes of home care. In this way, the outpatient clinician becomes integrated into the home medication use process.
This study used proactive risk assessment methods to engage parents in research, but there are limitations to this approach. We performed this study in three diverse study sites, but these findings may not be generalizable beyond our participants and their health care systems. A single rater assigned severity scores in this FMEA. This study focused on changes in chemotherapy doses, which is common in outpatient pediatric cancer care protocols. Findings may not be generalizable to all children with cancer; as such, it may not be feasible for some institutions to implement some of the recommendations. Because of the significant time commitment of study participants at the first site, where we held three 2-hour meetings, participation rates were low. Most participants were mothers, all spoke English, and most had some college education; results may not be generalizable to all parents. This study is not meant to garner results on quantitative frequencies of errors, which are best obtained from observational research,2,25 but to harness parent experiences in processes of home medication use to develop future prospective studies of error prevention strategies.
In sum, parents of children with cancer can participate in proactive risk assessment teams that seek to improve medication safety in the home. As one parent commented, “We are doing a lot of care at home, and 90% of the time there is no one there [except the family]. It's a lot of hands off. There needs to be more support because there's a lot of assumptions about what's going on at home.” Parents represent an important untapped resource, providing information for improving the quality of cancer care that could not be obtained from observational research.
Acknowledgment
Supported by a Robert Wood Johnson Physician Faculty Scholar award (K.E.W.), by the Charles H. Hood Foundation, and by National Cancer Institute Grants No. 5 U19 CA79689-11 and 1P50CA137219-01.
Appendix
Table A1.
No. of Failure Modes Identified in Each Major and Minor Step in the Process Map for Home Administration of Oral Chemotherapy After the Prescriber Changed the Dose
| Major Step | Minor Step | No. of Failure Modes | Failure Modes per Major Step |
|---|---|---|---|
| Family receives instructions | Healthcare provider gives instructions | 7 | 11 |
| Family understands instructions | 4 | ||
| Not enough medication at home, fill prescription | Problem with prescribing | 4 | 19 |
| Problem with dispensing | 10 | ||
| Problem from family | 5 | ||
| Update personal medication book | None | 4 | 4 |
| Adjust label | None | 2 | 2 |
| Share information with other caregivers | Mistake giving information | 2 | 4 |
| Mistake receiving information | 2 | ||
| Decide it is time to administer | Remember to give | 4 | 6 |
| Consider whether ok to give | 2 | ||
| Locate medicine | None | 3 | 3 |
| Read label | Label wrong | 2 | 5 |
| Read wrong | 3 | ||
| Measure dose | None | 3 | 3 |
| Prepare medication | Equipment | 2 | 7 |
| Handling | 5 | ||
| Locate child and administer medication | Location/medication problem | 2 | 5 |
| Child problem with medication | 3 |
Authors' Disclosures of Potential Conflicts of Interest
The author(s) indicated no potential conflicts of interest.
Author Contributions
Conception and design: Kathleen E. Walsh, Kathleen M. Mazor, Douglas Roblin, Colleen Biggins, Justin W. Li, Jennifer Donovan, Abir Kanaan, Saul N. Weingart
Financial support: Kathleen E. Walsh
Administrative support: Kathleen E. Walsh, Joann L. Wagner, Justin W. Li
Provision of study materials or patients: Kathleen E. Walsh, Douglas Roblin, Kathleen Houlahan, Justin W. Li, Christopher Keuker, Karen Wasilewski-Masker, Saul N. Weingart
Collection and assembly of data: Kathleen E. Walsh, Colleen Biggins, Joann L. Wagner, Kathleen Houlahan, Justin W. Li, Saul N. Weingart
Data analysis and interpretation: Kathleen E. Walsh, Kathleen M. Mazor, Douglas Roblin, Colleen Biggins, Joann L. Wagner, Kathleen Houlahan, Justin W. Li, Jennifer Donovan, Abir Kanaan, Saul N. Weingart
Manuscript writing: Kathleen E. Walsh, Kathleen M. Mazor, Douglas Roblin, Kathleen Houlahan, Karen Wasilewski-Masker, Saul N. Weingart
Final approval of manuscript: All authors
References
- 1.Taylor JA, Winter L, Geyer LJ, et al. Oral outpatient chemotherapy medication errors in children with acute lymphoblastic leukemia. Cancer. 2006;107:1400–1406. doi: 10.1002/cncr.22131. [DOI] [PubMed] [Google Scholar]
- 2.Walsh KE, Dodd KS, Seetharaman K, et al. Medication errors among adults and children with cancer in the outpatient setting. J Clin Oncol. 2009;27:891–896. doi: 10.1200/JCO.2008.18.6072. [DOI] [PubMed] [Google Scholar]
- 3.Weingart S, Brown E, Bach P, et al. NCCN task force report: Oral chemotherapy. J Natl Compr Canc Netw. 2008;3(6 Suppl):S1–S14. [PubMed] [Google Scholar]
- 4.Fischer DS, Alfano S, Knobf MT, et al. Improving the cancer chemotherapy use process. J Clin Oncol. 1996;14:3148–3155. doi: 10.1200/JCO.1996.14.12.3148. [DOI] [PubMed] [Google Scholar]
- 5.Arnhold RG, Adebonojo FO, Callas ER, et al. Patients and prescriptions comprehension and compliance with medical instructions in a suburban pediatric practice. Clin Pediatr (Phila) 1970;9:648–651. doi: 10.1177/000992287000901107. [DOI] [PubMed] [Google Scholar]
- 6.Alldred DP, Standage C, Fletcher O, et al. The influence of formulation and medicine delivery system on medication administration errors in care homes for older people. BMJ Qual Saf. 2011;20:397–401. doi: 10.1136/bmjqs.2010.046318. [DOI] [PubMed] [Google Scholar]
- 7.Fernandez Landaluce A, Mintegi Raso S, Martinez Gonzalez MJ. [Paracetamol poisoning in infants aged less than six months: Dosage errors] Ann Pediatr (Barc) 2004;60:177–179. doi: 10.1016/s1695-4033(04)78241-7. [DOI] [PubMed] [Google Scholar]
- 8.Ruddy K, Mayer E, Partridge A. Patient adherence and persistence with oral anticancer treatment. CA Cancer J Clin. 2009;59:56–66. doi: 10.3322/caac.20004. [DOI] [PubMed] [Google Scholar]
- 9.Partridge AH, Avorn J, Wang PS, et al. Adherence to therapy with oral antineoplastic agents. J Natl Cancer Inst. 2002;94:652–661. doi: 10.1093/jnci/94.9.652. [DOI] [PubMed] [Google Scholar]
- 10.Kato PM, Cole SW, Bradlyn AS, et al. A video game improves behavioral outcomes in adolescents and young adults with cancer: A randomized trial. Pediatrics. 2008;122:e305–e317. doi: 10.1542/peds.2007-3134. [DOI] [PubMed] [Google Scholar]
- 11.Wreathall J, Nemeth C. Assessing risk: The role of probabilistic risk assessment (PRA) in patient safety improvement. Qual Saf Health Care. 2004;13:206–212. doi: 10.1136/qshc.2003.006056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marx DA, Slonim AD. Assessing patient safety risk before the injury occurs: An introduction to sociotechnical probabilistic risk modelling in health care. Qual Saf Health Care. 2003;12(suppl 2):ii33–8. doi: 10.1136/qhc.12.suppl_2.ii33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DeRosier J, Stalhandske E, Bagian JP, et al. Using health care failure mode and effect analysis: The VA National Center for Patient Safety's prospective risk analysis system. Jt Comm J Qual Patient Saf. 2002;28:248–263. doi: 10.1016/s1070-3241(02)28025-6. [DOI] [PubMed] [Google Scholar]
- 14.Rath F. Tools for developing a quality management program: Proactive tools (process mapping, value stream mapping, fault tree analysis, and failure mode and effects analysis) Int J Radiat Oncol Biol Phys. 2008;71:S187–S190. doi: 10.1016/j.ijrobp.2007.07.2385. [DOI] [PubMed] [Google Scholar]
- 15.Weingart SN, Spencer J, Buia S, et al. Medication safety of five oral chemotherapies: A proactive risk assessment. J Oncol Pract. 2011;7:2–6. doi: 10.1200/JOP.2010.000064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.VA National Center for Patient Safety. Process design and organizational change. http://www.patientsafety.gov.
- 17.Institute for Healthcare Improvement. Failure modes and effects analysis. 2004. www.IHI.org/ihi/workspace/tools/fmea/
- 18.AAP. Prevention of medication errors in the inpatient setting. Pediatrics. 2003;112:431–436. doi: 10.1542/peds.112.2.431. [DOI] [PubMed] [Google Scholar]
- 19.Green BB, Cook AJ, Ralston JD, et al. Effectiveness of home blood pressure monitoring, Web communication, and pharmacist care on hypertension control: A randomized controlled trial. JAMA. 2008;299:2857–2867. doi: 10.1001/jama.299.24.2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ralston JD, Hirsch IB, Hoath J, et al. Web-based collaborative care for type 2 diabetes: A pilot randomized trial. Diabetes Care. 2009;32:234–239. doi: 10.2337/dc08-1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Malasanos T. Analysis: Automated messaging system for diabetes: An ounce of prevention. Diabetes Technol Ther. 2005;7:719–720. doi: 10.1089/dia.2005.7.710. [DOI] [PubMed] [Google Scholar]
- 22.Walsh KE, Mazor KM, Stille CJ, et al. Medication errors in the homes of children with chronic conditions. Arch Dis Child. 2011;96:581–586. doi: 10.1136/adc.2010.204479. [DOI] [PubMed] [Google Scholar]
- 23.Weingart SN, Gandhi TK, Seger AC, et al. Patient-reported medication symptoms in primary care. Arch Intern Med. 2005;165:234–240. doi: 10.1001/archinte.165.2.234. [DOI] [PubMed] [Google Scholar]
- 24.Wilson IB, Schoen C, Neuman P, et al. Physician-patient communication about prescription medication nonadherance: A 50-state study of America's seniors. J Gen Intern Med. 2006;22:6–12. doi: 10.1007/s11606-006-0093-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gandhi TK, Bartel SB, Shulman LN, et al. Medication safety in the ambulatory chemotherapy setting. Cancer. 2005;104:2477–2483. doi: 10.1002/cncr.21442. [DOI] [PubMed] [Google Scholar]