Abstract
A 60-year-old man presented with pain on the left cheek and lateral nose. The patient had been diagnosed with facial herpes zoster in the left V2 area 6 months previously. Medical treatment was prescribed for 6 months but it had little effect. We blocked the left infraorbital nerve under ultrasound guidance, but pain relief was short term. Therefore, we performed pulsed radiofrequency treatment on the left infraorbital nerve under ultrasound guidance. Six months after the procedure, the reduction of pain was still maintained, and there was no need for further management.
Keywords: infraorbital nerve, radiofrequency, ultrasound
One of the most difficult pain syndromes to treat is postherpetic neuralgia (PHN), which occurs in about 10% of patients with acute herpes zoster. The reason why this painful condition occurs in some patients but not in others is unknown, but it occurs more frequently in older aged patients or those with acute herpes zoster of the trigeminal nerve (CN V) compared with that involving the thoracic dermatomes [1].
PHN of the trigeminal nerve is a neuropathic disorder characterized by constant dysesthetic facial pain, originating from the trigeminal nerve with superimposed sudden, sharp and shooting neuritic pain. Some patients may complain of burning pain [2].
Several treatments have been suggested for PHN, including medication, botulinum toxin injections, nerve blocks, peripheral nerve stimulation, surgical intervention, pulsed radiofrequency treatment (PRFT) [3], and radiofrequency ablation [4]. Infraorbital nerve block is widely used to treat postherpetic V2 (maxillary nerve) neuralgia. But, the landmark based approach can be challenging because identifying the foramen by palpation is difficult due to anatomical variations in the infraorbital foramen [5]. Thus, it is easier and safer if the infraorbital nerve block and PRFT are performed under ultrasound (US) guidance [5]. Here, we present a case of successful treatment of infraorbital PHN using US-guided (USG) PRFT.
CASE REPORT
A 60-year-old man visited our pain clinic with the chief complaint of left facial pain. The patient had been diagnosed with facial herpes zoster in the left V2 area 6 months previously. The left facial pain had continued for 6 months despite medical treatment. During this period, 150 mg pregabalin, 10 mg amitriptyline, 37.5 mg tramadol/375 mg acetaminophen combination tablet (Paramacet tab; Donga, Seoul, Korea) were administrated per os three times daily but had little effect. He had paroxysmal, sharp and shooting pain on his left cheek and lateral nose. The pain was aggravated by touching the left facial area, and palpation over the left infraorbital foramen reproduced the pain. Pain severity was 9-10/10 on the visual analogue scale (VAS).
Hence, we started pain intervention for trigeminal PHN in the left V2 area. We initially blocked the left infraorbital nerve under USG with a 10-12 MHz linear transducer (Vivid E, General Electronics, Fairfield, CT, USA) using a mixture of 2 ml 2% mepivacaine and 20 mg triamcinolone. This procedure decreased the pain immediately. When he returned to our pain clinic 1 month after the infraorbital nerve block, the patient stated that the VAS score had decreased from 9 to 4 for about 2 weeks following the infraorbital nerve block but then his symptoms returned to a previous state. Therefore, we tried the same additional USG left infraorbital nerve treatment, but the outcome was the same.
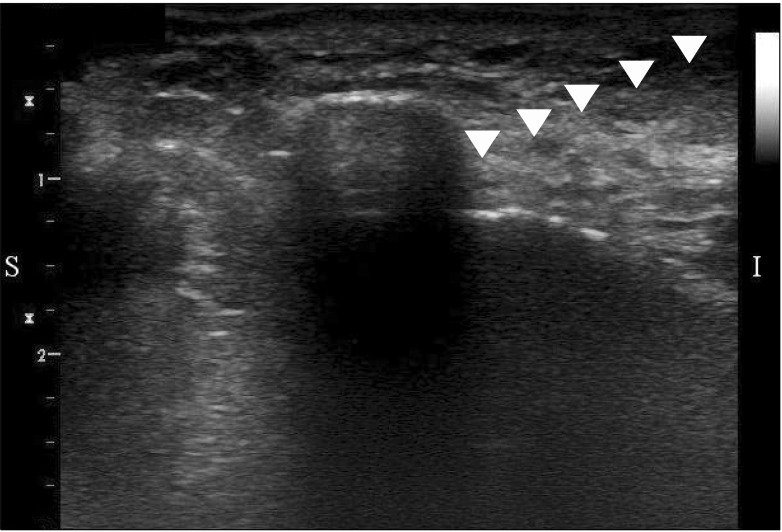
The USG infraorbital nerve blocks were effective but the effects were maintained for only 2 weeks, so we decided to perform PRFT. After explaining the procedure, efficacy, and possible side effects of PRFT, the patient was placed in a supine position. The skin was aseptically draped with betadine. The ultrasound was prepared with a sterile transparent sheath and aseptic ultrasound gel. The transducer was applied longitudinally to the lateral side of the nose and then rotated slightly clockwise to obtain an ideal longitudinal (long-axis) view of the infraorbital canal to find the left infraorbital foramen. We scanned his face from medial to lateral in the sagittal plane along the left lower orbital margin (Fig. 1). We easily identified the infraorbital foramen with a hyperechoic protuberance (Fig. 2).
Fig. 1.
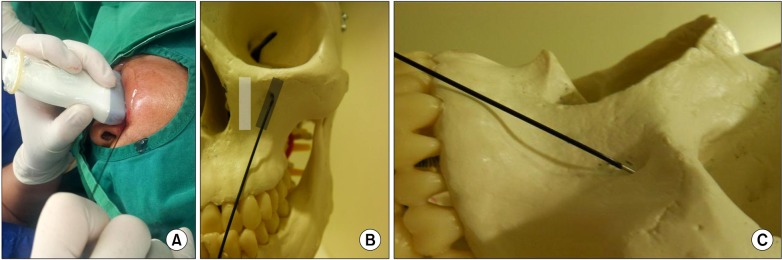
A photograph of the radiofrequency needle placement under ultrasound guidance (10-12 MHz linear transducer). (A) In the actual patient. (B) Anterior view in a human skull model, which is empirically depicted. (C) Lateral view in a human skull model, which is empirically depicted. The ultrasound transducer was initially applied longitudinally at the lateral side of the nose and rotated slightly clockwise. Then, the transducer was moved laterally until the left infraorbital foramen was identified.
Fig. 2.
An ultrasound image of the radiofrequency needle in the infraorbital foramen (10-12 MHz linear transducer, long-axis in-plane technique). The protuberance within the hyperechoic line indicates the infraorbital foramen. The radiofrequency needle through the infraorbital foramen is indicated with arrow heads.
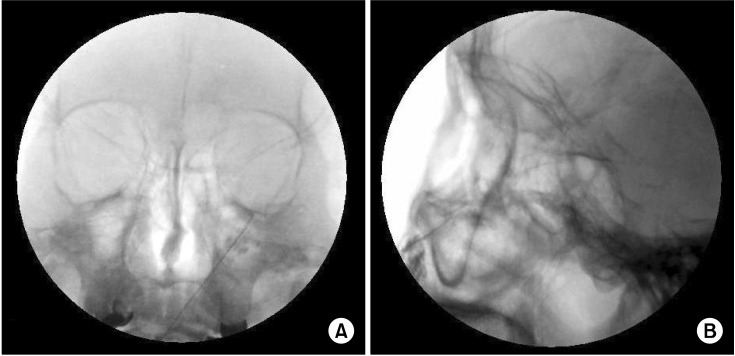
Radiofrequency needle (10 cm) insulated with a 5-mm active tip (22 G, SMK-C10; Radionics Inc, Burlington, MA, USA) was advanced slightly via the infraorbital foramen under USG (Fig. 2). Confirmation of the needle position inside the infraorbital foramen was achieved under fluoroscopy. Following negative aspiration, 0.5 ml of radio-contrast agent was injected to confirm no vascular uptake through the infraorbital artery (Fig. 3). Sensory stimulation using a 50 Hz, 0.3-0.5 V electrical current showed paresthesia over the left cheek and lateral nose. After confirming the needle position, we performed PRFT three times at 42℃ for 120 seconds. The patient did not show any problems throughout treatment.
Fig. 3.
Fluoroscope images during pulsed radiofrequency treatment of the left infraorbital nerve. (A) Anteroposterior view. (B) Lateral view. Fluoroscopic images show that the needle was in the infraorbital foramen and not in the orbital cavity. No vascular uptake of radio-contrast agent was observed.
One month after pulsed RF treatment, his pain severity was 1-2/10 on the VAS, and his pain relief scale was 80-90%. Because this pain relief was maintained continuously throughout the 2, 4, 6, and 12 month follow-ups after PRFT, no additional treatment including medication was provided.
DISCUSSION
Treatment of trigeminal PHN has been controversial; however, in our case, precisely performed USG infraorbital nerve PRFT resulted in an excellent outcome with no adverse effects. Furthermore, to the best of our knowledge, this is the first report of USG infraorbital nerve block and PRFT.
PHN pain is characterized as a constant, dysesthetic pain that can be exacerbated by movement or stimulation of the affected cutaneous regions. There may be sharp, shooting neuritic pain superimposed on constant dysesthetic symptoms. Some patients suffering from PHN will also complain of burning pain [6].
The infraorbital nerve is the terminal branch of the maxillary nerve (CN V2). The maxillary nerve begins at the middle of the trigeminal ganglion as a flattened plexiform band and passes horizontally forward. It leaves the skull through the foramen rotundum, where it becomes more cylindrical in form and firmer in texture. The maxillary nerve then crosses the pterygopalantine fossa, inclines laterally on the back of the maxillary, and enters the orbit through the inferior orbital fissure. It transverse the infraorbital groove and appears on the face at the infraorbital foramen. Here, it is referred to as the terminal branch of the infraorbital nerve. It supplies sensation to the cheek from the lower eyelid superiorly, to the upper lip inferiorly and from the nasal ala medially, and to the midzygoma region laterally.
Trigeminal PHN usually responds to pharmacotherapy, which should be employed before any intervention is attempted. Medical treatments results in good initial pain relief, but relief rates fall off dramatically over the long-term [7]. Cases refractory to medical management can be treated with minimally invasive procedures such as a nerve block. Nerve blocks with local anesthetics and steroids serving the painful area are a reasonable next step if pharmacological modalities fail to control the pain. The exact mechanism of pain relief from neural blockade during treatment of PHN is unknown, but it may be related to modulation of pain transmission [8].
Radiofrequency treatment for trigeminal PHN can also be considered. Heat radiofrequency lesioning (HRFL) has been effective for idiopathic trigeminal neuralgia, symptomatic facial pain, and herpes zoster of the fifth cranial nerve. HRFL is the recommended option for treating trigeminal pain in the elderly [4] and results in pain relief without medication in the relatively long term. But, it necessarily accompanies hypoesthesia or topoanesthesia. PRFT has gained interest because it seems to be a non-neuro-destructive method unlike conventional HRFL. The pulse output during PRFT is interrupted; thus, allowing sufficient time for the generated heat to be washed out. No reports have identified sensory or motor loss or complications related to PRFT [3].
The infraorbital nerve has a close anatomical relationship with the infraorbital foramen. Usually, we perform an infraorbital nerve block using the landmark-based approach and palpate the foramen. The infraorbital foramen can be palpated at 1-1.5 cm under the inferior edge of the orbit at the midpupillary line. It can occasionally be difficult to identify the infraorbital foramen by relying on palpation only, particularly in cases of anatomical variations in the infraorbital foramen [5]. Higher efficacy and a reduced risk of complications are realized using advanced imaging modalities including computed tomography or virtual reality techniques such as US or fluoroscopy [9]. Hence, US or fluoroscopy-guided infraorbital nerve PRFT can be a valuable treatment for trigeminal PHN.
US imaging is a safe, simple, and non-invasive modality through which soft tissues and nerve structures can be visualized and identified when combined with a thorough knowledge of regional anatomy. According to Koscielniak-Nielsen et al. [10], a USG peripheral nerve block significantly shortens performance time and reduces the number of needle passages to the target. The occurrence of paresthesia during block is also reduced but not the incidence of short-lasting post-operative neuropraxia. However, limited information is available on the use of US for identifying bony structures. Definitive identification of osseous landmarks may be important when the target nerve of the block is unidentifiable with US due to its small size and imaging artifacts. When we perform USG infraorbital nerve block, bone appears as a hyperechoic linear structure. Any disruption or protuberance within the hyperechoic line may indicate the infraorbital foramen (Fig. 2) [5]. Additionally, we confirmed arterial pulsation with Doppler. After we advanced the needle slightly into the infraorbital canal, we checked the needle position with fluoroscopy. Then we confirmed again that there was no vascular uptake through the infraorbital artery with radio-contrast agent (Fig. 3), which could help perform the procedure.
In summary, our patient had been treated medically for PHN. However, medication alone did not provide sufficient pain relief. USG infraorbital nerve block seemed to be effective for reducing the pain. But, its effect was insufficient. For these reasons, we finally decided to perform USG PRFT of the infraorbital nerve and gained excellent results. As with USG in our case, PRFT could be performed more precisely and efficiently. US provides insight into deeper structures under the skin and avoid the dangerous vessels with Doppler compared with the landmark approach. We could apply additional pulsed radiofrequency output to the infraorbital nerve compared to that of other nerves, because the infraorbital nerve is tight within infraorbital canal compared to other free-moving nerves during PRFT.
We have presented our experience of USG infraorbital nerve PRFT, which is safer and more effective than that of the landmark method. But, further randomized controlled studies will be needed to demonstrate the safety and efficacy of this treatment.
References
- 1.Hashizume K. Herpes zoster and post-herpetic neuralgia. Nihon Rinsho. 2001;59:1738–1742. [PubMed] [Google Scholar]
- 2.Fashner J, Bell AL. Herpes zoster and postherpetic neuralgia: prevention and management. Am Fam Physician. 2011;83:1432–1437. [PubMed] [Google Scholar]
- 3.Nguyen M, Wilkes D. Pulsed radiofrequency V2 treatment and intranasal sphenopalatine ganglion block: a combination therapy for atypical trigeminal neuralgia. Pain Pract. 2010;10:370–374. doi: 10.1111/j.1533-2500.2010.00382.x. [DOI] [PubMed] [Google Scholar]
- 4.Rahman M, Richter EO, Osawa S, Rhoton AL., Jr Anatomic study of the infraorbital foramen for radiofrequency neurotomy of the infraorbital nerve. Neurosurgery. 2009;64:423–427. doi: 10.1227/01.NEU.0000336327.10368.79. [DOI] [PubMed] [Google Scholar]
- 5.Tsui BC. Ultrasound imaging to localize foramina for superficial trigeminal nerve block. Can J Anaesth. 2009;56:704–706. doi: 10.1007/s12630-009-9129-3. [DOI] [PubMed] [Google Scholar]
- 6.Schmid T, Pautex S, Lang PO. Acute and postherpetic neuralgia in the elderly: analysis of evidence for therapeutic options. Rev Med Suisse. 2012;8:1374–1378. 1380–1382. [PubMed] [Google Scholar]
- 7.Haridas A, Mathewson C, Eljamel S. Long-term results of 405 refractory trigeminal neuralgia surgeries in 256 patients. Zentralbl Neurochir. 2008;69:170–174. doi: 10.1055/s-2008-1077076. [DOI] [PubMed] [Google Scholar]
- 8.Hall GC, Carroll D, McQuay HJ. Primary care incidence and treatment of four neuropathic pain conditions: a descriptive study, 2002-2005. BMC Fam Pract. 2008;9:26. doi: 10.1186/1471-2296-9-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bhaskar AK. Interventional management of cancer pain. Curr Opin Support Palliat Care. 2012;6:1–9. doi: 10.1097/SPC.0b013e32835017e7. [DOI] [PubMed] [Google Scholar]
- 10.Koscielniak-Nielsen ZJ. Ultrasound-guided peripheral nerve blocks: what are the benefits? Acta Anaesthesiol Scand. 2008;52:727–737. doi: 10.1111/j.1399-6576.2008.01666.x. [DOI] [PubMed] [Google Scholar]