Abstract
The decision to adopt the new WHO standard in the UK necessitated substantial changes to the neonatal section of the chart, including separation of the preterm UK birthweight reference from the WHO standard. The evidence-based design process has led to several novel features that could be generally applied in other chart designs, and revealed uncertainties leading to inconsistencies in charting. Failing to plot birthweight of term infants at age 0 can lead to spurious centile crossing in the early weeks of life, particularly among infants at the extreme of gestation. Users will need training to use the charts, but this should improve overall understanding and use of charts.
Introduction
In May 2009 new UK-WHO charts1 replaced those based on the British 1990 (UK90) reference2 for children 0-4 years of age. They incorporate World Health Organization (WHO) standards for weight, length (height from 2 years), body mass index and head circumference.3, 4 The WHO data were collected at six sites around the world, and all infants were exclusively or predominantly breastfed for the first 4-6 months of life in accordance with WHO infant feeding guidance at the time.5 All children included were born at term to healthy, socially privileged mothers who had not smoked. They thus portray how healthy children ought to grow and represent a growth standard rather than a reference.
In 2007 the UK Scientific Advisory Committee on Nutrition (SACN) reviewed applicability of the WHO standard to growth monitoring in the United Kingdom. It recommended that WHO data should be used from the age of 2 weeks, but that the UK90 birth data should be retained. This was partly because the WHO study excluded preterm infants but also because there were discrepancies between the UK90 and WHO datasets in birthweight at term.6 These may have reflected varying degrees of maternal restraint in the populations studied by WHO. SACN also recognised that the practice of smoothing centiles across the pre- and postnatal periods, as in previous UK charts, had introduced a bias in the depiction of weight gain during the first 2 weeks of life.7 It therefore recommended that the UK90 birth for gestation charts for 23-42 weeks should be separated from the WHO postnatal charts, and that the WHO centiles should be omitted during the first 2 weeks.
The Department of Health then commissioned the Royal College of Paediatrics and Child Health (RCPCH) to design the new charts and an expert group chaired by CMW undertook this work. The most significant design changes particularly affected the perinatal period and this paper explains the rationale behind the design. The final charts are described elsewhere1 and can be downloaded from www.growthcharts.rcpch.ac.uk .
Design issues
The starting point was SACN’s recommendation that the new chart should adopt the WHO growth standard from 2 weeks of age and “… take account of the differences in birthweight, gestational age and the adjustment in weight that often occurs in the first two weeks after birth”.6 Consequently the commissioning brief was to produce a composite A4 chart combining the UK90 birth reference data with the WHO growth standard data between 2 weeks and 4 years of age. Companion A5 charts were also required for the personal child health record (PCHR). Additionally it was decided that both sets of charts should be supported by newly written evidence-based instructions and training materials.
This design brief required clarity in the definition of age. The word “term” refers here to births between 37 and 42 completed weeks gestation, while “preterm” refers to births following shorter gestation. Postnatally, age is expressed here either as i) postnatal age (age since birth or simply age); ii) postmenstrual age (the sum of gestational and postnatal age), or iii) corrected age (postmenstrual age less 40 weeks). Thus for example 42 weeks postmenstrual age corresponds to age 2 weeks in infants born at 40 weeks gestation, or to age 7 weeks in infants born at 35 weeks gestation, or to corrected age 2 weeks in both.
The design specification therefore required an infancy chart starting at age 2 weeks, and a chart showing weight and size at birth for the range of gestational ages between 23 and 42 weeks. The intention was to plot preterm infants on the latter until they reached a postmenstrual age of 42 weeks, i.e. corrected age 2 weeks. These proposals raised further questions:
What form should the birth size for gestation chart take?
Should the birthweight of infants born at term (i.e. between 37 and 42 completed weeks of gestation) be adjusted for gestation?
How should weight be plotted in the first 2 weeks following birth at term?
How should the growth of preterm infants be plotted?
How the group worked
The expert group met regularly and, once a design specification had been developed, the detailed design work was undertaken collaboratively with a specialist chart printing firm (Harlow Printing, UK). A small group of neonatal specialists offered general advice on the presentation of the birth size for gestation charts. Two rounds of plotting workshops with health staff were then undertaken to test the proposed chart design. The first round evaluated the new design features and elicited views on the use of draft charts in clinical practice, while the second formally tested the final prototype. Staff were presented with clinical scenarios spanning the neonatal period and asked to plot and interpret measurements of term infants using both the old and the new charts. There was also a stakeholder consultation meeting at which many organizations provided comment.
What form should the birth for gestation chart take?
In order to construct the new charts the UK90 birth reference data were reanalysed to produce new centiles describing size at birth between 23 and 42 weeks of gestation. Additionally a pooled ‘term’ composite birthweight reference based on all births between 37 and 42 completed weeks of gestation was produced. The details of this process are described elsewhere.8
As only one in four preterm births (1.5% of all births) occurs before 32 weeks gestation a decision was made to include only birth data for 32-42 weeks gestation on the main 0-4 year charts. On the initial draft these were displayed in three small panels (weight, length and head circumference) to the left of the 0-1 year chart, but plotting trials revealed that practitioners found them difficult to use. Since length is rarely measured in healthy British newborns, and observation of clinical practice suggests that when it is, the measurements are often of doubtful accuracy, it was decided to enlarge the weight and head circumference panels, and replace the length chart with a text panel providing instructions. A separate chart including birth length for 26-42 weeks has been developed for monitoring of infants born from 23 weeks gestation. This “Neonatal and Infant Close Monitoring” (NICM) chart displays the recalculated UK90 reference between 23 and 42 weeks gestation. The infancy section of this chart also has an expanded measurement scale making it suitable for plotting all babies requiring continued close monitoring up to the age of two years.
Should the birthweight of infants born at term be adjusted for gestation?
The first round of plotting trials revealed that health staff inconsistently adjusted term births for gestation,9 and even within the expert group discussion revealed variation in practice. We therefore used longitudinal weight data from the Gateshead Millennium Study (GMS)10 to evaluate the consequences of gestational adjustment at term and to explore how the weight gain of term infants born at various gestational ages tracks centiles in early life. We specifically examined the implications of early life transition from the recalculated UK90 birth reference to the WHO postnatal standard after the age of 2 weeks.
The GMS is a prospective population-based cohort study with extensive routinely collected weight data in the early weeks. The numbers recruited at each week between 37 and 42 weeks of gestation were respectively 64, 124, 180, 296, 201 and 60 making a total of 925 infants. All GMS weight data were converted both to UK90 and UK-WHO SD scores and the two compared for groups of infants born at different gestations.
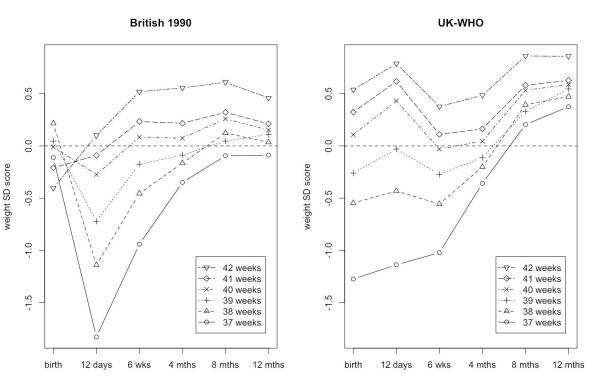
Figure 1 shows mean weight SD scores of the GMS cohort plotted two different ways. In the left panel, using the old UK90 reference, weight SD score has been adjusted for gestation at birth but no correction has been made thereafter. In consequence the weight of infants born at 37-38 weeks appears to falter dramatically between birth and 12 days of age. The mean weight SD scores at birth also fail to predict the ranking of the gestational age groups at later ages, with considerable crossover occurring in the first 12 days. This reflects two things: firstly there was a bias in the UK90 birthweight centiles attributable to the splining of birth and postnatal data; and secondly the UK90 data lacked measurements in the early days when weight gain is relatively slow.7
1.
Weight by age for 925 infants in the Gateshead Millennium Study, summarised as mean SD scores by gestation at six ages. The SD scores are based on the original UK90 charts (left) and new UK-WHO charts (right). Birthweight is adjusted for gestation (left) and unadjusted (right). See text for details.
In the right panel of Figure 1 the new UK-WHO composite reference for term infants has been applied at birth and subsequent data plotted against the WHO standard. Thus weight at birth has not been adjusted for gestation but is related to the mean weight of all infants born between 37 and 42 completed weeks of gestation. As might be expected infants born at 37-38 weeks gestation are relatively light at birth, and remain so later, but gain progressively. Both charts indicate completion of “catch up” by 8 months of age, but on the UK-WHO chart the appearance of weight faltering between birth and 12 days has been abolished. This is because the WHO standard incorporates data collected in the early days of life.
The plot also shows that the ranking of UK-WHO SD score for each gestational age group at birth corresponds well with the ranking of WHO SD score from 2 weeks onwards. The correlation between weight SD score at birth and at 8 months based on UK-WHO was 0.40 whether or not birthweight was adjusted for gestation, which suggests that gestational adjustment of birthweight does not improve prediction of relative weight at 8 months and later.
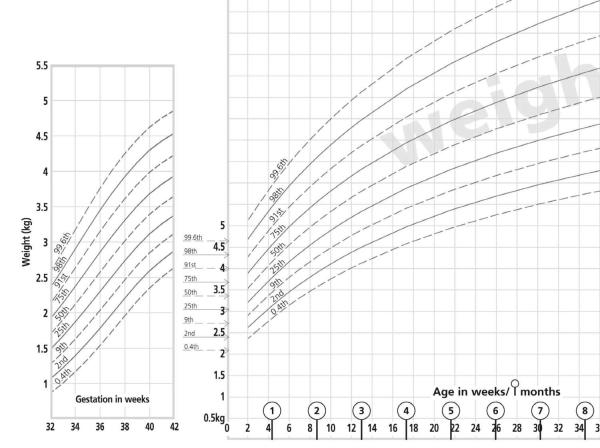
Given these findings, the expert group concluded that all term infants should be plotted against the composite term birth centiles at age 0 on the 0-1 year chart to pre-empt spurious centile crossing in the early weeks of life. The chart instructions now clearly state this. Figure 2, taken from the girls A4 chart, shows the weight by gestation chart together with the composite term centiles at age 0 on the 0-1 year chart, and the absence of WHO centiles before 2 weeks.
2.
UK-WHO A4 chart (detail) showing birth centiles for weight in UK girls from 32 to 42 weeks gestation, and at term.
How should weight be plotted in the first 2 weeks following birth at term?
The absence of centile lines from birth to 2 weeks was intended to stimulate practitioners to relate weights in this period to birthweight. It was recommended that weight loss of 10% or more should trigger closer assessment, particularly of feeding.1, 11 Initially an attempt was made to signal weight loss by differential scaling of the ordinate so that excess weight loss could be identified using a horizontal rule. However the plotting area was small and the first plotting workshops demonstrated considerable potential for reading error, so this feature was dropped. Instead users were instructed to calculate weight loss directly. The first round of trial plotting demonstrated widespread unfamiliarity with calculating percentage weight loss and some lack of concern about substantial (12.5%) weight loss.9 With clearer guidance performance improved somewhat in the second round, but this is an important training topic.9
How should the growth of preterm infants be plotted?
The plotting workshops demonstrated great confusion about gestational adjustment after preterm birth.9 After consultation, it was decided that birth data for infants born at 32-36 weeks gestation should be plotted at the appropriate gestational age on the preterm weight and head circumference panels, interpolating between whole weeks as necessary. Subsequent measurements should continue to be plotted in the preterm section until the attainment of 42 weeks postmenstrual age (i.e. 2 weeks corrected age). Later measurements should be plotted on the 0-1 year chart at postnatal age with an arrow drawn back to the corrected age, the length of the arrow being the difference between weeks of gestation and 40 weeks. In this way the arrowhead indicates clearly the gestationally corrected centile, confirms that correction for preterm birth has been made and reduces the risk of computation error. It was agreed that gestational correction for preterm infants of 32-36 weeks gestation could stop after 12 months corrected age, as by then the effect on centile position is very slight, but it should continue to 24 months corrected age for shorter gestations.
Conclusion
In retrospect when producing the original British 1990 charts2 it was unwise to smooth birth and postnatal data, as this biased the centiles at term and during the early postnatal weeks, ignoring the fact that the centiles during the two periods are not comparable.7 The clear separation of UK birth and WHO postnatal data on the new charts resolves this issue. This process has also clarified for the first time how birthweight at term should be plotted in relation to gestation. It was clear from the plotting exercises that practice in adjusting for gestation at term was highly variable, and that clear and unambiguous guidance on this was required. Not adjusting birthweight for gestation makes a considerable difference for less mature term infants; for example a 37-week gestation infant of median weight would plot at the 9th rather than the 50th centile. Yet the unadjusted centile is just as good as the adjusted centile for predicting relative weight at 8 months, and it avoids the spurious centile crossing in the early weeks associated with adjustment.
There are important lessons here also for other countries designing perinatal growth charts. We would suggest firstly that birth for gestation centiles should be kept separate from postnatal centiles, whether or not (as here) they are based on the same reference population. Secondly birthweight in term infants should not be adjusted for gestation, but plotted at age 0 on the postnatal chart. Finally there is a strong case for omitting centiles in the period immediately after birth so that practitioners are encouraged to calculate weight loss relative to birthweight and evaluate feeding practices when this exceeds 10%.
The UK-WHO charts now present birth and neonatal measurements in a different but better validated format. Training in the proper use of the charts is important but should result in better understanding and more consistent practice. Supporting educational materials were produced for the charts and are free to download at www.growthcharts.rcpch.ac.uk .
Acknowledgements
We are indebted to John Short, Diane Hall and Christine Charlton for their design work on the charts, to all the staff and parents who organized and took part in the various focus workshops and to Terence Stephenson, Linda Haines, and staff within the RCPCH Science and Research Department for their project management support.
Funding This UK-WHO early years growth chart project was funded by a grant from the English Department of Health to the RCPCH.
TJC is funded by Medical Research Council grant G0700961, based at GOSH/UCL Institute of Child Health which received a proportion of funding from the Department of Health’s NIHR Biomedical Research Centres funding scheme.
The Gateshead Millennium Baby Study was funded by grants from the Henry Smith Charity and SPARKS (Sport Aiding Research in Kids).
None of the funders had any influence on the writing of the paper.
Footnotes
Contributors All authors were members of the RCPCH Growth Chart Expert Group. All authors collaborated in writing this article. TJC drafted it, and the other authors commented on each draft. TJC will act as guarantor of the paper.
Copyright The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive licence (or non-exclusive for government employees) on a worldwide basis to the BMJ Publishing Group Ltd and its Licensees to permit this article (if accepted) to be published in Archives of Disease in Childhood and any other BMJPGL products to exploit all subsidiary rights, as set out in our licence (http://group.bmj.com/products/journals/instructions-for-authors/licence-forms).
Competing interests All authors were members of the Growth Chart Expert Group. TJC and CMW have acted as advisers on certain elements of the WHO Multicentre Growth Reference Study. TJC receives royalties from his LMSchartmaker software used to construct the UK birth for gestation charts.
Contributor Information
Tim J Cole, UCL Institute of Child Health, University College London.
Charlotte M Wright, Faculty of Medicine, University of Glasgow.
Anthony F Williams, St George’s, University of London RCPCH Growth Chart Expert Group, Royal College of Paediatrics and Child Health.
References
- 1.Wright CM, Williams AF, Elliman D, et al. Using the new UK-WHO growth charts. BMJ. 2010;340:c1140. doi: 10.1136/bmj.c1140. [DOI] [PubMed] [Google Scholar]
- 2.Freeman JV, Cole TJ, Chinn S, et al. Cross sectional stature and weight reference curves for the UK, 1990. Arch Dis Child. 1995;73:17–24. doi: 10.1136/adc.73.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO Multicentre Growth Reference Study Group WHO child growth standards based on length/height, weight and age. Acta Paediatr. 2006;(Suppl 450):76–85. doi: 10.1111/j.1651-2227.2006.tb02378.x. [DOI] [PubMed] [Google Scholar]
- 4.WHO . WHO child growth standards: methods and development. WHO; Geneva: 2006. [Google Scholar]
- 5.de Onis M, Garza C, Onyango AW, et al. WHO child growth standards. Acta Paediatr. 2006;95(Suppl 450):3–101. [Google Scholar]
- 6.SACN/RCPCH Expert Group [cited 31/8/2008];Application of WHO Growth Standards in the UK. 2007 Available from: http://www.sacn.gov.uk/pdfs/report_growth_standards_2007_08_10.pdf.
- 7.Wright CM, Parkinson KN. Postnatal weight loss in term infants: what is “normal” and do growth charts allow for it? Arch Dis Child. 2004;89:F254–F7. doi: 10.1136/adc.2003.026906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cole TJ, Williams AF, Wright CM. Revised birth centiles for weight, length and head circumference in the UK-WHO growth charts. Ann Hum Biol. 2011;38:7–11. doi: 10.3109/03014460.2011.544139. [DOI] [PubMed] [Google Scholar]
- 9.Wright CM, Sachs M, Short J, et al. Designing new UK-WHO growth charts: what do health staff understand about chart use and how accurately do they use them? MCN Journal. 2011 DOI: 10.1111/j.1740-8709.2010.00296.x. [Google Scholar]
- 10.Wright C, Lakshman R, Emmett P, et al. Implications of adopting the WHO 2006 Child Growth Standard in the UK: two prospective cohort studies. Arch Dis Child. 2008;93:566–9. doi: 10.1136/adc.2007.126854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Dommelen P, van Wouwe JP, Breuning-Boers JM, et al. Reference chart for relative weight change to detect hypernatraemic dehydration. Arch Dis Child. 2007;92:490–4. doi: 10.1136/adc.2006.104331. [DOI] [PMC free article] [PubMed] [Google Scholar]