Abstract
Background
On January 1, 2005, Medicare began covering a “Welcome to Medicare” visit (WMV) for new enrollees with fee-for-service (FFS) Medicare (Parts A and B). The new benefit was expected to increase demand for mammography and Pap tests among women transitioning onto Medicare. This study examined whether Medicare's coverage of a WMV influenced the use of mammography and Pap tests among women aged 65 and 66 years with FFS Medicare.
Methods
Medicare Current Beneficiary Survey (MCBS) data from 2001 to 2007 were linked with Medicare claims. Utilization rates for preventive visits, mammography, and Pap tests were measured among women entering Medicare. Multivariate logistic regressions were estimated to quantify the effects of the new Medicare benefit on the use of these screening tests, controlling for patient characteristics.
Results
Regression-adjusted mammography and Pap test rates did not increase after WMV coverage was introduced. The 2005 reform had nonsignificant trivial effects on the use of both tests, most likely because few of the women who were eligible for a WMV took advantage of it.
Conclusions
Medicare coverage of a WMV had no impact on mammography screenings or Pap tests among women who were eligible for the benefit.
Introduction
Effective January 1, 2005, Medicare began covering a one-time initial preventive visit, known as the “Welcome to Medicare” visit (WMV). This preventive visit was made available to new beneficiaries within 6 months of beginning their Part B coverage.1 In addition to measuring height, weight, and blood pressure, the WMV was to include education, counseling, and referrals for other preventive services already covered under Medicare, including breast and cervical cancer screening tests.2 It was believed that this initial visit would allow physicians and patients to spend time emphasizing prevention and cancer screening during a visit when patients were not preoccupied with symptoms or their treatment plans for other health problems. Medicare's regular cost-sharing provisions applied to the visit; that is, it was subject to the Medicare annual Part B deductible and a standard 20% Medicare copay above that amount.
Despite new screening modalities, mammography remains the main screening tool for breast cancer in the general population.3 Until recently, Pap smear cervical cytology was the only screening test available for cervical cancer. Pap smear tests and mammography screenings were first covered under Medicare Part B as preventive services for women in 1990 and 1991, respectively (Table 1). In 1998, Medicare waived its Part B deductible for Pap smears and mammography, but until 2011, a woman was still responsible for her standard Medicare copays. As a result of the 2010 Affordable Care Act (ACA), beginning January 1, 2011, Medicare waived its copays for mammography and Pap smears, thereby eliminating any out-of-pocket costs associated with these tests. A screening mammography may be billed to Medicare once a year, and a screening Pap smear may be billed once every 3 years. More frequent mammography screenings and Pap smears are covered by Medicare only if a woman is at higher risk for breast cancer and/or cervical or vaginal cancer. Nevertheless, although Medicare has provided more generous coverage for cancer screening over time, the US Preventive Services Task Force (USPSTF) has further specified its recommendations by age group, and in 2003, the USPSTF reinstated its upper age limit of 65 years for cervical cancer screening (Table 1). Thus, as of 2003, most age-eligible Medicare beneficiaries were no longer being recommended for cervical cancer screening under USPSTF guidelines.
Table 1.
Medicare Coverage of Breast and Cervical Cancer Screening and Wellness Visits
| |
|
|
USPSTF Recommendations |
|
|---|---|---|---|---|
| Date | Medicare coverage | Effective year | Breast | Cervical |
| January 1, 1990 | Pap smears first covered | 1989 | 1989—Mammogram every 1–2 years; ages 50–75 | 1989—Pap test every 1–3 years; up to age 65 |
| 1 test every 3 years | 1990 | |||
| 20% copayment; $100 deductible | ||||
| January 1, 1991 | Mammograms first covered | 1991 | ||
| 1 test between ages 35 and 39 years | 1992 | |||
| 1 test every 11 months for ages 40+ years | 1993 | |||
| 20% copayment; $100 deductible | 1994 | |||
| 1995 | ||||
| 1996 | 1996—Mammogram every 1–2 years; ages 50–69 | 1996—Pap test every 1–3 years; no upper age limit | ||
| 1997 | ||||
| January 1, 1998 | Mammograms | 1998 | ||
| Part B deductible waived; 20% copay still applies | 1999 | |||
| Pap smears | 2000 | |||
| Part B deductible waived; 20% copay still applies | ||||
| July 1, 2001 | Pap smears | 2001 | ||
| Biennial coverage | 2002 | 2002—Mammogram every 1–2 years; ages 40+ | ||
| 2003 | 2003—Pap test every 3 years; up to age 65 | |||
| 2004 | ||||
| January 1, 2005 | Welcome to Medicare first covered | 2005 | ||
| 1 visit within 6 months of Part B coverage | 2006 | |||
| 20% copayment; $100 deductible | 2007 | |||
| January 1, 2008 | Welcome to Medicare | 2008 | ||
| 1 visit within 12 months of Part B coverage | 2009 | 2009—Mammogram every 2 years; ages 50–74 | ||
| Part B deductible waived; 20% copay still applies | 2010 | |||
| January 1, 2011 | Wellness Visit first covered | 2011 | ||
| 1 visit every 12 months | ||||
| No cost to beneficiary | ||||
| Welcome to Medicare | ||||
| No cost to beneficiary | ||||
| Mammograms | ||||
| No cost to beneficiary | ||||
| Pap smears | ||||
| No cost to beneficiary | ||||
USPSTF, United States Preventive Services Task Force.
This article examines the effects of covering a WMV on the receipt of cancer screening among women who were newly enrolling in Medicare. Using data from the 2001–2007 Medicare Current Beneficiary Survey (MCBS), we evaluate whether offering coverage of a WMV influenced the receipt of mammography screenings and Pap tests among women aged 65 and 66 years with fee-for-service (FFS) Medicare.
Background
Prior to 2005, advocacy groups, including the American Cancer Society (ACS),2 had argued that allowing coverage for an initial preventive visit under Medicare would improve cancer screening rates and health outcomes among beneficiaries. The reasoning behind the WMV was to establish a source of primary care for new beneficiaries who may lack access to care and to provide a dedicated opportunity to emphasize health promotion and cancer screening among this group. Although Medicare had already been covering Pap tests and mammograms for some time (Table 1), it was believed that face-to-face visits focused on preventive care and good health habits were critical to attaining age-appropriate screening behaviors among older women.
Even though a woman could have obtained—and still can—screening mammograms without a referral or a prescription from her doctor,4 self-referral for mammography was the exception rather than the norm. Self-referrals comprise only about 6% of all mammograms.5 Most mammograms and Pap tests occur only after a woman receive a recommendation from a physician to get screened.5–8 In addition, approximately 80% of women who have not had a recent mammogram say it is because their physician did not suggest getting one.9,10 A lack of physician recommendation was also known to contribute to the underuse of Pap tests among older women.7,11,12
Physician referrals for cancer screening are much more likely to be given during office visits focused on preventive care than during office visits for acute or chronic health problems.13,14 Thus, there was evidence strongly suggesting that Medicare coverage for an initial preventive visit might increase cancer screening rates. We turn now to an empirical test of whether it actually did.
Materials and Methods
Data sources and sample
Data for this study come from the Medicare Current Beneficiary Survey (MCBS), an annual panel survey sponsored by the Centers for Medicare and Medicaid Services (CMS). Since 1991, the MCBS has been administered to a nationally representative sample of the Medicare population by a face-to-face interview in three waves, and it covers a host of topics, including health status, health insurance coverage and financing, access to care, knowledge and understanding of Medicare, and use and effectiveness of new program benefits and changes. The sampling scheme and methods for data collection in the MCBS have been described elsewhere in detail.15 The Institutional Review Board of the University of North Carolina at Chapel Hill approved all aspects of the study protocol.
Several prior studies have used the MCBS to examine cancer screening and use of other preventive services within the Medicare population.16–20 We used data from the 2001–2007 MCBS for our analysis, along with the annual outpatient and inpatient claims data for each respondent. At a beneficiary level, we linked the MCBS Cost and Use modules for each year to their respective annual Medicare claims and then pooled the data for years 2001–2007.
Our sample is restricted to female Medicare beneficiaries, aged 65–68 years, holding FFS Medicare (Parts A and B) rather than belonging to a Medicare health maintenance organization (HMO) plan and were not enrolled in Medicaid during the survey year. For purposes of analysis, we divide these women into two groups: a treatment group consisting of women aged 65 and 66 years and a comparison group consisting of women aged 67 and 68 years. The treatment group is limited to ages 65 and 66 because the WMV was only covered during a woman's first 6 months on Medicare, which would typically be during the 6 months following her 65th birthday. Women aged 66 years are included in the treatment group because some may have had a WMV but delayed their cancer screenings until they were due for the tests the following year. The comparison group includes women aged 67 and 68 years because these women were ineligible for a WMV, but in other respects, their Medicare coverage was the same. In both groups, we exclude women enrolled in Medicare HMOs because Medicare's coverage of a WMV did not apply to them, and we exclude women who also had Medicaid because in most states Medicaid already covered similar visits. We further exclude beneficiaries with any history of end-stage renal disease, breast cancer (for the mammography cohort), and cervical cancer (for the Pap smear cohort).
Measures of preventive visits and cancer screening
Our first outcome of interest was the percentage of women who had at least one preventive visit during the survey year. A binary variable was created from the Part B claims data using the Health Care Common Procedure Coding System (HCPCS). In addition to HCPCS codes associated with WMV claims (G0402 through G0405), we included HCPCS codes 99387 and 99397 for comprehensive preventive medicine evaluation and management visits for individuals aged ≥65. As providers are generally reluctant to change their billing practices and some may not have realized initially that the WMV has its own billing code, we took into consideration the possibility of coding the WMV as a 993×7 procedure. This approach made our estimated WMV utilization rate an upper-bound estimate.
For breast cancer screening, our outcome of interest was the percentage of eligible women who had at least one mammogram during the survey year. The codes used to identify a mammography screening were 76092, 77057, and G0202. For cervical cancer, our outcome was the percentage of women who received at least one Pap test during that year. To identify Pap smears, we used the following codes: G0123, G0124, G0141, G0143, G0144, G0145, G0147, G0148, P3000, P3001, and Q0091.
Medicare claims and survey data
We constructed a (0, 1) indicator of whether Medicare covered a WMV at the time of the survey, which equals 1 for years 2005–2007 and 0 for years 2001–2004. Another (0, 1) indicator was constructed to describe whether the respondent belongs to the treatment (1) vs. comparison (0) group. The key parameter of interest is the interaction term between the WMV flag and treatment/control flag. The MCBS data provide information on several other variables expected to influence the receipt of cancer screenings among women. Individual-level characteristics in each model include annual household income, educational attainment, whether the woman carries employer-sponsored health insurance in addition to Medicare, whether she holds a Medigap supplemental policy, marital status, self-rated overall health status (excellent, very good, good, fair, or poor), history of mental health problems, prior diagnoses of other nonskin cancers, smoking status, and race/ethnicity. The MCBS also captured whether the respondent resided in a metropolitan area and the Census region. Health Professional Shortage Area (HPSA) designation was obtained from the Area Resource File (ARF) and linked to MCBS respondents by ZIP code.21
Statistical analysis
We compared baseline characteristics of our treatment group, women newly enrolled in Medicare (aged 65–66 years), with those of the comparison group, women aged 67–68 years, using chi-square tests. We then estimated three difference-in-differences (DD) models22 to assess the impact of the WMV coverage on each of our three outcome variables. To estimate each DD model, the treatment and comparison groups were pooled, and a multivariate logistic regression was fit to determine if the introduction of Medicare coverage for a WMV increased the likelihood of that outcome. In all models, we controlled for the WMV flag, the treatment group flag, and the interaction of these two variables, in addition to other factors that may have influenced the receipt of such services. The three models describe having received a preventive visit, a screening mammography, and a Pap smear, respectively, during the past year. All analyses were conducted using SUDAAN statistical software (version 10) (RTI International, Research Triangle Park, NC) and included the complex survey sampling weights that produce nationally representative results.
Results
After pooling the 7 years in the observation period, a total of 1577 women newly enrolled in Medicare (aged 65–66 years) met the sample inclusion criteria (Table 2). The comparison group included 2126 women aged 67–68 years. Of new enrollees who did not report a history of breast cancer, 25% received a mammography screening during the observed year vs. 35% in the comparison group. Of new enrollees who did not report a history of cervical cancer, 11% received a Pap smear test in the treatment group and 14% in the comparison group. Only 3.4% of the treatment group had at least one claim for a preventive visit vs. 5% in the comparison group.
Table 2.
Sample Characteristics, Female Respondents from Medicare Current Beneficiary Survey Between 2001 and 2007
| Variable | Age group 65–66 years | Age group 67–68 years | p value |
|---|---|---|---|
| Mammography,a % | 25.3 | 35.2 | <0.01 |
| Pap smear,b % | 10.9 | 13.8 | 0.48 |
| Comprehensive preventive examination, % | 3.4 | 5.0 | 0.02 |
| Survey year ≥2005 (WMV introduction), % | 41.6 | 43.0 | 0.44 |
| Medicare supplemental coverage, % | |||
| Medigap, % | 7.3 | 10.5 | <0.01 |
| Employer-based, % | 40.8 | 40.1 | 0.59 |
| Census region, % | |||
| Northeast | 18.6 | 17.0 | 0.28 |
| Midwest | 22.6 | 23.2 | 0.70 |
| South | 39.0 | 39.6 | 0.74 |
| West | 19.8 | 20.2 | 0.79 |
| Race/ethnicity, % | |||
| White | 79.3 | 80.9 | 0.13 |
| Black | 7.2 | 6.7 | 0.53 |
| Hispanic | 6.9 | 7.2 | 0.62 |
| Married, % | 62.0 | 61.8 | 0.81 |
| Smoker, % | 15.1 | 13.5 | 0.19 |
| History of nonskin cancer, % | 13.2 | 14.9 | 0.06 |
| History of breast cancer, % | 5.4 | 6.1 | 0.26 |
| History of cervical cancer, % | 0.8 | 0.8 | 0.87 |
| History of mental health issues, % | 18.1 | 16.6 | 0.26 |
| General health status, % | |||
| Excellent | 22.6 | 19.6 | 0.06 |
| Very good | 30.2 | 33.8 | 0.02 |
| Good | 28.8 | 30.0 | 0.52 |
| Fair | 13.4 | 12.3 | 0.31 |
| Poor | 4.9 | 3.5 | 0.05 |
| Less than high school, % | 18.8 | 17.7 | 0.37 |
| Household income <$25,000, % | 51.2 | 44.9 | <0.01 |
| Residence in metropolitan area, % | 77.0 | 75.1 | 0.15 |
| Residence in HPSA, % | 17.5 | 20.4 | 0.06 |
| Mammography cohort size | 1,485 | 1,993 | |
| Pap smear cohort size | 1,561 | 2,104 | |
| Total number of respondents | 1,577 | 2,126 | |
| Weighted sample size | 10,581,445 | 10,685,374 | |
Among mammography cohort only (excludes breast cancer patients).
Among Pap smear cohort only (excludes cervical cancer patients).
HPSA, health professional service area; WMV, “Welcome to Medicare” visit.
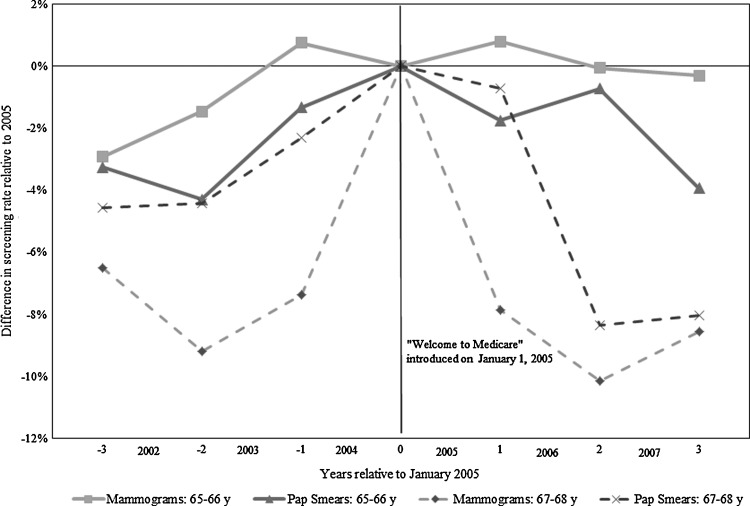
On estimating the models, we found no evidence of an increase in the likelihood of receiving preventive visits, mammography, or Pap smears among women after the introduction of coverage of the WMV. We examined regression-adjusted mean changes by year in the likelihood that a woman received a mammography screening, relative to the implementation of coverage for a WMV (Fig. 1). For the treatment group, the changes in rates of mammography from year to year were small (e.g., the largest annual change was+2.2% in 2003), and the change over the entire 2001–2007 period was only+1.4%. Similarly annual changes in Pap smear rates for the treatment group were small (largest was −3.1% in 2007), and the change over the entire observation period was +2.6%. Compared with 2004, Pap smear rates declined by 1.8%, 1.0%, and 3.2% in 2005, 2006, and 2007, respectively.
FIG. 1.
Adjusted change in the share of new Medicare enrollees (and compliance group) receiving mammograms and Pap smears, by year relative to January 2005 benefit change.
In the estimated logistic regressions (Table 3), the first column reports the odds ratios (ORs) associated with the likelihood of receiving a preventive visit. The interaction term between WMV coverage and age group is nonsignificant after adjusting for other covariates. In this model, having a history of mental problems was significantly associated with higher likelihood of receiving a preventive visit (OR 1.18), and reporting fair or poor health was significantly associated with lower likelihood of a visit (OR 0.35). Additional control variables were significant predictors of cancer screening use in the other two models, including having supplemental insurance coverage, being married, and being a smoker. However, both the mammography and Pap smear models yielded nonsignificant effects for the interaction term between WMV coverage and age group.
Table 3.
Multivariate Logit Models of Variables Associated with Receipt of Preventive Visits and Cancer Screening Among Female Respondents to Medicare Current Beneficiary Survey Between 2001 and 2007
| |
Preventive visit |
Mammogram |
Pap smear |
|||
|---|---|---|---|---|---|---|
| Characteristics | OR (95% CI) | p value | OR (95% CI) | p value | OR (95% CI) | p value |
| Age 65–66 (vs. 67–68) years | 0.58 (0.38-0.87) | 0.01 | 0.58 (0.47-0.71) | <0.01 | 0.90 (0.69-1.17) | 0.43 |
| Survey year ≥2005 (WMV available) | 0.71 (0.44-1.14) | 0.16 | 0.79 (0.63-0.98) | 0.04 | 0.78 (0.59-1.04) | 0.09 |
| (Age 65–66 years)×(year ≥2005) | 1.62 (0.76-3.44) | 0.21 | 1.34 (0.93-1.95) | 0.12 | 1.23 (0.77-1.97) | 0.38 |
| Medigap coverage | 1.50 (0.84-2.68) | 0.17 | 2.32 (1.66-3.23) | <0.01 | 1.79 (1.25-2.56) | <0.01 |
| Employer-based coverage | 1.28 (0.85-1.93) | 0.24 | 1.61 (1.29-2.00) | <0.01 | 1.47 (1.09-1.99) | 0.01 |
| Northeast | 1.51 (0.61-3.76) | 0.37 | 1.95 (1.33-2.87) | <0.01 | 1.60 (1.04-2.46) | 0.03 |
| Midwest | 2.80 (1.22-6.41) | 0.02 | 1.82 (1.30-2.54) | <0.01 | 1.94 (1.22-3.11) | <0.01 |
| South | 1.59 (0.76-3.30) | 0.21 | 1.80 (1.28-2.52) | <0.01 | 1.86 (1.28-2.69) | <0.01 |
| Black | 0.65 (0.28-1.49) | 0.31 | 0.82 (0.55-1.22) | 0.33 | 0.89 (0.53-1.49) | 0.66 |
| Hispanic | 0.32 (0.08-1.32) | 0.12 | 0.58 (0.36-0.93) | 0.02 | 0.84 (0.42-1.70) | 0.64 |
| Married | 1.08 (0.71-1.66) | 0.71 | 1.48 (1.19-1.84) | <0.01 | 1.38 (1.01-1.90) | 0.04 |
| Smoker | 0.85 (0.51-1.42) | 0.53 | 0.61 (0.44-0.85) | <0.01 | 0.65 (0.44-0.98) | 0.04 |
| History of nonskin cancer | 1.18 (0.73-1.93) | 0.50 | 1.20 (0.92-1.55) | 0.18 | 1.57 (1.12-2.19) | 0.01 |
| History of mental health issues | 1.54 (1.00-2.36) | 0.05 | 1.26 (0.99-1.59) | 0.06 | 1.30 (0.96-1.75) | 0.09 |
| Fair/poor health | 0.35 (0.17-0.73) | <0.01 | 0.91 (0.71-1.16) | 0.43 | 0.90 (0.61-1.33) | 0.58 |
| Less than high school | 0.66 (0.33-1.33) | 0.24 | 0.76 (0.58-1.00) | 0.05 | 0.74 (0.49-1.10) | 0.14 |
| Household income <$25,000 | 0.60 (0.36-1.01) | 0.06 | 0.79 (0.65-0.96) | 0.02 | 1.03 (0.80-1.33) | 0.82 |
| Residence in metropolitan area | 1.75 (0.91-3.38) | 0.09 | 0.73 (0.57-0.93) | 0.01 | 0.99 (0.71-1.38) | 0.94 |
| Residence in HPSA | 1.01 (0.54-1.89) | 0.98 | 0.83 (0.63-1.09) | 0.17 | 0.93 (0.69-1.26) | 0.65 |
| Cohort size | 3,703 | 3,478 | 3,665 | |||
| Weighted sample size | 21,266,819 | 20,036,343 | 21,091,963 | |||
CI, confidence interval; OR, odds ratio.
We also estimated the models a number of other ways to check the robustness of our findings (data not shown). Our substantive results remained unchanged. First, we reestimated both of the regressions in Table 3 excluding women aged 66 years, given the possibility that their inclusion in the sample might have diluted the estimated effect of coverage of a WMV. Even with this change in the sample, not much changed. The coefficients on the interaction term remained nonsignificant in these models. We then reestimated the models excluding women who had employer-sponsored health coverage in addition to Medicare, on the possibility that some of them may have already had coverage for a preventive visit through their employer plan, in which case Medicare's WMV benefit would have been duplicative coverage, not something new. We also considered a Pap smear model that excluded women who have had a hysterectomy (and thus do not require testing). The coefficients on the interaction term remained statistically nonsignificant in each of the alternative models.
Discussion
In 2006, approximately 1300 new enrollees in Medicare were surveyed as part of the MCBS's New Enrollee Supplement, a special survey administered in that year. Fewer than 3% of the beneficiaries who were eligible to receive a WMV said they took advantage of the benefit.23 According to those individuals surveyed, the main reason for not pursuing a WMV was that they did not know about the benefit. Of the respondents, 78% said they would have pursued it had they known about its availability. Our claims-based rates of preventive visits are consistent with these findings. Therefore, it comes as no surprise that the introduction of coverage for a WMV had no effects on cancer screening rates among women newly entering Medicare.
Currently, the WMV is reimbursed only once for Medicare beneficiaries and only during their first year after enrolling in Medicare Part B. When the program began in 2005, beneficiaries could take advantage of the visit only during their first 6 months in Part B. For some beneficiaries, it may have taken longer than 6 months to obtain an appointment for a visit.24 Providers may be less inclined to design a visit that provides a complex set of services described in the regulation if only a very small percentage of their patients is eligible for it each year. An important research area to investigate is the behavior of providers in response to these new benefits. It is possible that one visit is not enough to adequately address preventive care, which requires an ongoing relationship between the patient and provider. With the pressures of today's primary care environment, it may be difficult for a clinician to administer the screening questions and provide the necessary follow-up counseling in just one visit. It is also possible that some clinicians find reimbursement for the WMV (approximately $125)25 inadequate.
A few changes to the WMV benefit were made in 2008, under the Medicare Improvements for Patients and Providers Act. Most notably, Medicare began waiving its Part B deductible for the visit, and new enrollees were given 1 year instead of 6 months from their Medicare enrollment date to take advantage of the benefit. Beneficiaries were still liable for their Medicare copay for the visit (i.e., 20% of Medicare's approved amount, or approximately $25). The 2010 ACA eliminated the Medicare copay for this visit, effective January 1, 2011, so beneficiaries now pay nothing when they receive it, provided their doctors accept Medicare assignment (i.e., the doctor accepts the amount Medicare approves as payment in full). Follow-up analysis will be needed to determine if these changes resulted in increased use.
The ACA also includes several new preventive care benefits for Medicare beneficiaries. Among them is an annual wellness visit benefit, which is available to beneficiaries of all ages with FFS Medicare, not just new enrollees. The wellness visit is meant to be a visit during which the beneficiary and her physician develop or update a personalized prevention plan, including a schedule for receiving cancer screenings, such as a mammography screening and Pap smear. Like the WMV, the wellness visit will be fully covered, so beneficiaries pay nothing to receive it provided their doctors accept assignment.
Conclusions
Our findings in this article raise questions about the potential efficacy of the new wellness visit. Although it is intended to increase the use of preventive care and even though cost sharing is dropped from the new benefit and it is available to all FFS Medicare enrollees, our findings raise questions of whether it will have any effects at all. The reason is that the new benefit shares several of the characteristics of the WMV. In 2011, the first year the wellness visit was available, only 1.35 million (approximately 3%) Medicare beneficiaries received it.26 The motivation of providers to increase cancer screening rates among Medicare beneficiaries should be further examined.
A limitation of this study is that we were unable to track the healthcare utilization history of study subjects before their Medicare enrollment. In addition, screening rates in the MCBS are reported for the past year only, whereas screening recommendations for mammography and Pap smear call for longer time intervals between each test. Some women entering Medicare may have been screened for cancer before their enrollment in the program and, based on guideline recommendations, may not have required another screening until after their WMV eligibility period. Our finding that younger Medicare beneficiaries were less likely to receive preventive visits and mammograms relative to their older counterparts underscores that privately insured women may be getting these services before aging into Medicare. Further, it is difficult to accurately capture all preventive visits because providers may not be properly billing these services. Providers who did not bill for preventive visits as the primary visit type prior to 2005 would have been reluctant to bill for the WMV after it was introduced. Finally, this study examined whether the availability of a WMV benefit influenced cancer screening use. Because WMV utilization rates were so low, we were unable to determine if the lack of effect on screening rates was caused by the low uptake of these visits or by the ineffectiveness of WMVs when they occurred. Although introduction of the WMV did not have an impact on overall cancer screening rates, it may have been valuable for those women who actually used it. Unfortunately, because so few women in our sample actually had a WMV, we were unable to formally test that hypothesis.
In summary, we did not find an increase in cancer screening rates among women newly enrolled in Medicare after the introduction of the WMV benefit. These results are consistent with recent trends in mammography and Pap smear rates in the general population.27–29 Despite efforts by policymakers to improve cancer screening rates within the Medicare population, providers may lack the financial incentives to deliver preventive services,30 and their reimbursements may not be aligned with current evidence-based recommendations from the USPSTF.31 Improving the delivery of screening services to Medicare beneficiaries may require innovative payment reform for these services concordant with USPSTF recommendations.
Acknowledgments
R.G.S. is supported by the Cancer Care Quality Training Program of the National Cancer Institute, National Institutes of Health, under grant R25 CA116339.
Disclosure Statement
No competing financial interests exist.
References
- 1.Card RO. How to conduct a “Welcome to Medicare” visit. Fam Pract Manag. 2005;12:27–29. 31–32. [PubMed] [Google Scholar]
- 2.Dewilde LF. Russell C. The “Welcome to Medicare” physical: A great opportunity for our seniors. CA Cancer J Clin. 2004;54:292–294. doi: 10.3322/canjclin.54.6.292. [DOI] [PubMed] [Google Scholar]
- 3.Elmore JG. Armstrong K. Lehman CD. Fletcher SW. Screening for breast cancer. JAMA. 2005;293:1245–1256. doi: 10.1001/jama.293.10.1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Food and Drug Administration. Mammography Quality Standards Act and Program. MQSA national statistics. www.fda.gov/Radiation-EmittingProducts/MammographyQualityStandardsActandProgram/FacilityScorecard/ucm113858.htm. [Oct 20;2011 ]. www.fda.gov/Radiation-EmittingProducts/MammographyQualityStandardsActandProgram/FacilityScorecard/ucm113858.htm
- 5.Suter LG. Elmore JG. Self-referral for screening mammography. J Gen Intern Med. 1998;13:710–713. doi: 10.1046/j.1525-1497.1998.00209.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Romans MC. Marchant DJ. Pearse WH. Gravenstine JF. Sutton SM. Utilization of screening mammography–1990. Womens Health Issues. 1991;1:68–73. doi: 10.1016/s1049-3867(05)80018-0. [DOI] [PubMed] [Google Scholar]
- 7.Coughlin SS. Breslau ES. Thompson T. Benard VB. Physician recommendation for Papanicolaou testing among U.S. women, 2000. Cancer Epidemiol Biomarkers Prev. 2005;14:1143–1148. doi: 10.1158/1055-9965.EPI-04-0559. [DOI] [PubMed] [Google Scholar]
- 8.Hynes DM. Bastian LA. Rimer BK. Sloane R. Feussner JR. Predictors of mammography use among women veterans. J Womens Health. 1998;7:239–247. doi: 10.1089/jwh.1998.7.239. [DOI] [PubMed] [Google Scholar]
- 9.Schueler KM. Chu PW. Smith-Bindman R. Factors associated with mammography utilization: A systematic quantitative review of the literature. J Womens Health. 2008;17:1477–1498. doi: 10.1089/jwh.2007.0603. [DOI] [PubMed] [Google Scholar]
- 10.Meissner HI. Breen N. Taubman ML. Vernon SW. Graubard BI. Which women aren't getting mammograms and why? Cancer Causes Control. 2007;18:61–70. doi: 10.1007/s10552-006-0078-7. [DOI] [PubMed] [Google Scholar]
- 11.Gulitz E. Bustillo-Hernandez M. Kent EB. Missed cancer screening opportunities among older women: A provider survey. Cancer Pract. 1998;6:325–332. doi: 10.1046/j.1523-5394.1998.006006325.x. [DOI] [PubMed] [Google Scholar]
- 12.Juon HS. Seung-Lee C. Klassen AC. Predictors of regular Pap smears among Korean-American women. Prev Med. 2003;37:585–592. doi: 10.1016/j.ypmed.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 13.Jaen CR. Stange KC. Nutting PA. Competing demands of primary care: A model for the delivery of clinical preventive services. J Fam Pract. 1994;38:166–171. [PubMed] [Google Scholar]
- 14.Sabatino SA. Thompson T. Coughlin SS. Schappert SM. Predisposing, enabling, and reinforcing factors associated with mammography referrals in U.S. primary care practices. Open Health Serv Policy J. 2009;2:57–70. doi: 10.2174/1874924000902020057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adler GS. A profile of the Medicare current beneficiary survey. Health Care Financ Rev. 1994;15:153–163. [PMC free article] [PubMed] [Google Scholar]
- 16.Ozminkowski RJ. Goetzel RZ. Shechter D. Stapleton DC. Baser O. Lapin P. Predictors of preventive service use among medicare beneficiaries. Health Care Financ Rev. 2006;27:5–23. [PMC free article] [PubMed] [Google Scholar]
- 17.Doubeni CA. Laiyemo AO. Reed G. Field TS. Fletcher RH. Socioeconomic and racial patterns of colorectal cancer screening among medicare enrollees in 2000 to 2005. Cancer Epidemiol Biomarkers Prev. 2009;18:2170–2175. doi: 10.1158/1055-9965.EPI-09-0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Doubeni CA. Laiyemo AO. Young AC, et al. Primary care, economic barriers to health care, and use of colorectal cancer screening tests among Medicare enrollees over time. Ann Fam Med. 2010;8:299–307. doi: 10.1370/afm.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Doubeni CA. Laiyemo AO. Klabunde CN. Young AC. Field TS. Fletcher RH. Racial and ethnic trends of colorectal cancer screening among Medicare enrollees. Am J Prev Med. 2010;38:184–191. doi: 10.1016/j.amepre.2009.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schneider EC. Rosenthal M. Gatsonis CG. Zheng J. Epstein AM. Is the type of Medicare insurance associated with colorectal cancer screening prevalence and selection of screening strategy? Med Care. 2008;46:S84–90. doi: 10.1097/MLR.0b013e31817fdf80. [DOI] [PubMed] [Google Scholar]
- 21.Area Resource File (ARF) Rockville, MD: Bureau of Health Professions, U.S. Department of Health and Human Services; 2011. Office of research and planning. [Google Scholar]
- 22.Woolridge J. Introductory econometrics. 3rd. Mason, OH: South-Western Cengage Learning; 2009. [Google Scholar]
- 23.Petroski CA. Regan JF. Use and knowledge of the new enrollee “Welcome to Medicare” physical examination benefit. Health Care Financ Rev. 2009;30:71–76. [PMC free article] [PubMed] [Google Scholar]
- 24.Gold J. Physicians should make use of “Welcome to Medicare” visit. Wisconsin Med J. 2007;106:351. [PubMed] [Google Scholar]
- 25.Centers for Medicare & Medicaid Services. Physician fee schedule. www.cms.gov/apps/physician-fee-schedule. [Mar 27;2012 ]. www.cms.gov/apps/physician-fee-schedule
- 26.U.S. Department of Health & Human Services. More than 16 million people with Medicare get free preventive services in 2012. www.hhs.gov/news/press/2012pres/07/20120710a.html. [Aug 26;2012 ]. www.hhs.gov/news/press/2012pres/07/20120710a.html
- 27.Breen N. A Cronin K. Meissner HI, et al. Reported drop in mammography : Is this cause for concern? Cancer. 2007;109:2405–2409. doi: 10.1002/cncr.22723. [DOI] [PubMed] [Google Scholar]
- 28.Breen N. Cronin KA. Tiro JA, et al. Was the drop in mammography rates in 2005 associated with the drop in hormone therapy use? Cancer. 2011;117:5450–5460. doi: 10.1002/cncr.26218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Solomon D. Breen N. McNeel T. Cervical cancer screening rates in the United States and the potential impact of implementation of screening guidelines. CA Cancer J Clin. 2007;57:105–111. doi: 10.3322/canjclin.57.2.105. [DOI] [PubMed] [Google Scholar]
- 30.Lesser LI. Bazemore AW. Improving the delivery of preventive services to Medicare beneficiaries. JAMA. 2009;302:2699–2700. doi: 10.1001/jama.2009.1918. [DOI] [PubMed] [Google Scholar]
- 31.Woolf SH. A closer look at the economic argument for disease prevention. JAMA. 2009;301:536–538. doi: 10.1001/jama.2009.51. [DOI] [PubMed] [Google Scholar]