Abstract
Objectives
The female condom (FC), an effective barrier method for HIV/sexually transmitted infection (STI) prevention, continues to be absent from most community settings, including reproductive health and treatment clinics. Reducing or eliminating basic barriers, including lack of awareness, knowledge of proper use, and access to free samples, may significantly increase use among those who want or need them.
Methods
A prospective cohort of 461 women in Hartford, Connecticut (2005–2008), was interviewed at baseline, 1 month, and 10 months about FC use and other personal, partner, peer, and community factors. All participants received brief demonstration of FC use and four free FC1 at baseline. Pairwise longitudinal tests and structural equation modeling were used to test predictors of initial (1 month) and sustained (10 month) FC use.
Results
Although only 29% of the sample reported ever having used FC at baseline, 73% of never users (51% of the returned 1-month sample) had initiated FC use by 1 month after receiving the brief intervention. Additionally, 24% of the returned 10-month sample (30% of 10-month FC users) reported sustained use, measured as having used FC at baseline or 1 month and also in the prior 30 days. General latent variable modeling indicated that FC knowledge and attitudes predicted initiating FC use; male condom use, FC knowledge and attitudes, and network exposure to FC information predicted sustained use.
Conclusions
Findings indicated that many women will potentially initiate and continue using FC when basic barriers are removed. Brief FC education with free trial samples should be built into standard clinical practice and public health programs.
Introduction
Significant scientific efforts to develop an efficacious vaginal or oral microbicide to prevent HIV offer promise for new options to reduce infections in women. However, these efforts recently suffered a series of setbacks with the early discontinuation of efficacy trials of several microbicidal products,1–3 highlighting significant work still needed to achieve an effective microbicide.4,5 Women continue to lead in rates of new HIV infections around the globe.6 They need all available alternatives for the prevention of HIV and other sexually transmitted infections (STI) that can effectively prevent transmission.
The female condom (FC) is an effective and available barrier method, as efficacious as the male condom (MC) for the prevention of STI and unwanted pregnancy.7,8 FC also offers women an option they can initiate and possibly control. It is especially important for HIV/STI prevention among high-risk women who could benefit greatly from multiple and women-initiated prevention options. Innumerable studies of the FC conducted from the early 1990s to the present have shown its initial and short-term acceptability among women and men in a wide variety of ethnic populations, age groups, and risk groups across the United States and worldwide.9 These studies demonstrate that women can initiate FC use with their steady partners, including their husbands, as well as with casual or paying partners, even sometimes negotiating FC use if a partner refuses MC, or the reverse.10–12 Most reported user concerns about the FC diminish over time with repeated use, and in many studies, some women and men report liking it better than MC.9,13,14
Despite this strong body of research in support of FC, the device is often held up as a negative example—a failed method of limited or no value—because of its slow pace to take hold as a marketed product.15–19 FC continue to be absent from most community settings, including reproductive health and HIV/STI prevention and treatment clinics, and are not a part of common prevention practice, programming, or popular thinking about available effective options. One of the primary barriers to FC uptake for HIV/STI prevention or contraception appears to be healthcare providers and educators themselves, whose own skepticism about potential popular attitudes and use of the product keeps them from introducing it to their clients or patients and supporting its use and further promotion.13,19–21
Our own research with urban and high-risk women has indicated increasing need for more women-initiated prevention options but limited awareness of the FC, how to use it, and where it can be found locally.22–24 Based on this need and strong support in the literature for FC as an effective prevention option, we conducted a 4-year study (2005–2008) of FC use for HIV/STI prevention among women in Hartford, Connecticut. The study was designed to test whether women would use the product if basic barriers were removed. These barriers include lack of awareness of the product, poor basic knowledge and skills to insert and remove it properly and to troubleshoot common problems in use, and limited or no access to any FC in order to try them. We hypothesized that removal of these barriers would result in a significant increase in both initial trial (first time use) and sustained use of the product as a prevention option. The study was also designed to explore multilevel personal, relationship, and social factors affecting initial and sustained FC use and to examine patterns of use/nonuse in different contexts.22 We present here findings from the analysis of a cohort of women, their initial and sustained FC use over a 10-month period, and factors affecting their use of this product for HIV/STI prevention.
Materials and Methods
Study design, sample recruitment, and retention
We recruited 461 women into our prospective, longitudinal cohort study between October 2004 and November 2007. These women were interviewed at baseline and asked to return for 1-month and 10-month follow-up surveys. The sample was created through targeted street outreach recruitment, referrals from health and service organizations, and referral by other study participants. This adaptive sampling technique25 reached both a convenience sample of women distributed across the city representing the primary ethnic groups in Hartford and hidden subgroups of women at high risk, such as drug users, commercial sex workers, and women whose partners were HIV positive or illicit drug users. Participants received a $10 incentive if they referred another eligible woman to the survey, limited to two referrals per participant. Eligibility for the confidential baseline survey included being ≥16 years of age (based on proof of age), self-reported having had sex with a man within the prior 30 days, and residence in Hartford (to facilitate follow-up recruitment). Upon screening, women were asked to provide signed informed consent to participate in the study. All women who completed the 1-hour survey received a $25 incentive at each time point. All recruitment, screening, and other study protocols and all research measures received full review and approval by an Institutional Review Board.
With our adaptive sampling design, we could not document the rate of refusals of potential participants to enter the study. Of the 461 women recruited into the baseline survey, 390 (85%) returned for the 1-month survey, and 243 (53%) returned for the 10-month survey (15 of whom had missed the 1-month survey). All baseline and follow-up surveys were conducted in private rooms in our community-based research institute, located centrally in the city. Surveys were conducted face-to-face with a project interviewer, who completed the computer-assisted survey interview. The significantly different time gap between the first two measurements (1 month) and between the second two measurements (9 months) was designed to capture initiating FC use (1-month assessment) and sustained FC use (10-month assessment).
Brief female condom introduction
After completing the baseline survey, interviewers provided each woman a 10–15 minute demonstration of proper FC insertion and removal, using their hands as a model and a picture book as a visual aid. They explained common problems with FC use and possible solutions. Interviewers then gave each woman four free FC1 (the original polyurethane FC produced by the Female Health Company) along with MC, lubricant, and take-home instructions for use of both types of condom. After completing the 1-month survey, interviewers asked participants if they had questions about FC insertion or problems during use if they tried it and if they knew where to get more FC if they wanted them. Interviewers answered women's questions (e.g., regarding handling the slippery inner ring during insertion, ensuring its full placement around the cervix, using additional lubrication to reduce noise) and offered the same package of prevention materials to all who requested them. This support protocol was repeated after the 10-month follow-up assessment.
The study was not designed to test the efficacy of the brief FC demonstration. This session was provided to all participants in order to remove the barriers of limited awareness and insertion knowledge, need for troubleshooting support, and limited community availability of FC. We anticipated that the removal of these basic barriers would result in a significant upsurge in the number of women who initiated use. However, the brief intervention alone was not expected to induce sustained use. This we anticipated would vary by women's different personal and risk characteristics, social and peer circumstances, and sexual relationships.
Theoretical model and definition of measures
A social ecologic approach guided our research design and analysis of multilevel factors hypothesized to affect the primary outcomes of initial and sustained FC use.22,26–28 These included individual-level (demographic, risk), partner (types, gender power), peer (network), and environmental (community) factors and the relationships among these factors.
Measures of the individual-level factors included ethnicity, marital status, educational attainment, age, income, and homeless status. HIV/STI risk measures included prior 30-day alcohol use to intoxication, injection drug use or crack use, current HIV status (self-reported), past STI diagnosis and current symptoms, and experience of childhood and adulthood physical or sexual abuse. Partner variables included prior 30-day number of sex partners and types of partners (primary/intimate, casual, paying), MC and FC use with each type of sex partner, and unprotected sex by partner type. Environmental factors included sources of FC and MC and other prevention materials the participant accessed in the community.
In addition to measures of women's characteristics and sexual relationship contexts, we measured several cognitive factors. These included FC knowledge (proportion correct of 6 true–false items, e.g., FC are as effective as MC in protecting against HIV and other STIs. FC must be fitted by a healthcare provider. Range 0–1) and self-efficacy to use the FC with each type of sex partner (mean of two items: How sure are you that you could talk to a […] partner about using FC for vaginal sex? If you only had FC available, how sure are you that you could refuse vaginal sex with a […] partner who refused to use it? Range 1–4). We also measured internal STI locus of control (mean of two items: If I take care of myself, I can keep from getting an STI. If I take the right actions, I can keep from getting an STI. Range 1–4) and perceived relationship power with primary partners (15-item scale including questions about who has control over decisions, actions, and so on in the relationship. Range 1–4; α=0.887).29 FC attitudes were measured with a 26-item scale measuring responses to perceived FC characteristics (range 1–4, higher score is more positive attitudes; α=0.849).30 Subscales of attitudes measuring FC use for HIV/STI prevention (e.g., FC provides women another choice to protect against HIV and other STI.), comparison with MC (e.g., FC are stronger than MC.), insertion issues (e.g., I don't like having to use my finger to push the FC in.), effects on sexual pleasure (e.g., FC makes sex better for women.), and appearance (e.g., Having part of the FC hang out is gross.) were examined separately, but we report here only on total scale scores. Relationship power and FC attitude scales have been validated with similar low-income U.S. populations of women.29,30 Network exposure to FC information measured whether members of the woman's personal network ever talked to her about FC (1 item, yes–no). FC use behavioral outcome measures included ever having used FC, number of times ever used FC (none, once, 2–10 times, >10 times), and having used FC in the prior 30 days with any type of partner.
In conducting our analyses, we defined initial FC use at the 1-month survey as those reporting never having used the FC at baseline but having used it in the prior 30 days at 1 month. (The small number, n=9, who initiated use between the 1 month and 10-month surveys were not included in the analysis of FC initiated use.) We defined sustained FC use at the 10-month time point, including those who reported having used FC ever or in the prior 30 days at either baseline or 1-month surveys and also having used them in the prior 30 days at the 10-month survey.
In a prior analysis of the baseline data of this sample, we tested a multilevel model of stage of FC use (from never having thought about it through initial trial and ongoing regular use), which we report elsewhere.22 On the basis of that path analysis with multilevel factors, we hypothesized for the current analyses that both initial and sustained FC use would be predicted directly by higher baseline educational attainment, greater baseline FC knowledge, more positive FC attitudes, higher internal locus of control, peer influence, a history of childhood sexual or physical abuse, being HIV infected, and higher FC efficacy with primary partners.22
Statistical analyses
We began our analyses by describing and comparing the baseline sample with the subsamples of women who returned for the 1-month and 10-month surveys on all key variables. Comparisons were also made of those who reported ever having used FC and current FC users entering the study, those who initiated use at the 1-month survey, and those who ever used and sustained use by the 10-month survey with those who did not report each of these behaviors at the same time point. Then, we tested hypotheses about individual, cognitive, relationships, and contextual factors associated with use and predictors of use, including modeling the mediational effects of all these factors on initial and sustained FC use.
To address the problem of attrition, tests comparing baseline characteristics of retained participants with those lost to follow-up at 1 month and of 1-month characteristics of those retained and lost by 10 months, we assessed possible bias on analyses of change in FC use and attitudes over time. Multiple imputations of missing data performed in AMOS 16 on logistic models of initiation and then sustained use31 using the bayesian estimation algorithm were employed to impute likely initiation and sustained use among participants who dropped from the study to estimate potential attrition bias. In conducting comparisons between returning and dropout participants to assess the impact of attrition on all demographic, behavioral, and attitudinal measures, we used Pearson's chi-square tests for categorical measures and one-way analysis of variance (ANOVA) tests for continuous measures. The chi-square statistic was used to test the fit of the generalized latent variable models to the data.
To address the problem of nonindependence resulting from repeated measures, we used generalized latent variable modeling (GLVM),32 commonly known as structural equation modeling (SEM), to model the relationships among all predictor variables and FC use outcomes. SEM benefits from tremendous versatility in simultaneously estimating multiple linear regression equations and specifically modeling various cross-equations constraints, such as correlations between error variances across equations or across time, to model repeated measurements.33 We used GLVM with robust weighted least squares means and variance (WLSMV)-adjusted estimator with diagonal weight matrix34 for dichotomous endogenous variables, to test the predictors of initiated and sustained use; direct and indirect effects35 were estimated for the final causal models.
To model factors predicting FC initiation and sustained use with SEM, we tested three sets of GLVM models with robust estimator in Mplus 634 to arrive at the final models. For each of these outcomes, a first model included all relevant demographic, risk behavior, peer, partner, and attitudinal variables initially hypothesized to predict the final outcome. Predictors with significance levels p<0.2 were kept in a second round of testing, and models were reestimated. Then, longitudinal logistic models with direct and indirect effects on FC use initiation and FC sustained use were tested. Mediation effects were tested from each initial predictor through the consequent same-variable on the outcome.
Results
Sample characteristics and attrition
Table 1 describes the sample at baseline and those who returned for the 1-month and 10-month surveys. Participant ages ranged from 16 to 68 at baseline, with a mean age of 39.2 years. The majority indicated very low socioeconomic status. Many participants reported high risk for HIV through illicit drug or alcohol use, prior STI history or current STI symptoms, abuse histories, and multiple sex partners. Only around half the sample and returned subsamples, however, reported prior 30 day MC use.
Table 1.
Female Condom Study Sample Characteristics at Baseline, 1-Month, and 10-Month Surveys
| Total sample (% of baseline sample) | Baseline 461 | 1 Month 390 (84.6) | 10 Month 243 (52.7) |
|---|---|---|---|
| Ethnic group | |||
| Black/African American | 55.5 | 57.4 | 59.7 |
| Puerto Rican/other Latino | 30.4 | 28.7 | 29.2 |
| White/other groups | 14.1 | 13.8 | 11.1 |
| High school graduate | 49.9 | 50.3 | 52.3 |
| Marital status | |||
| Single | 56.4 | 65.4 | 61.7 |
| Married/living together | 25.2 | 19.5 | 23.5 |
| Divorced/separated/widowed | 17.6 | 14.9 | 14.0 |
| Homeless | 28.9 | 22.6* | 18.1 |
| Prior month income<$500 | 36.4 | 34.6 | 40.7 |
| Currently unemployed | 54.9 | 56.2 | 49.4 |
| Substance use in last 30 days | |||
| Alcohol use until drunk | 31.0 | 30.0 | 33.7 |
| Injection drug use | 7.6 | 4.9 | 4.9 |
| Crack use | 33.4 | 23.3* | 29.2 |
| Sexually transmitted infections | |||
| Past STI | 65.9 | 56.9 | 60.1 |
| Current STI symptoms | 10.8 | 4.1 | 4.1 |
| HIV-positive (self-report) | 10.8 | 11.8 | 13.2 |
| Any physical/sexual abuse history | 54.9 | 48.7 | 49.4 |
| Childhood abuse history | 45.3 | 40.3 | 42.8 |
| Adulthood abuse history | 48.4 | 46.2 | 47.7 |
| Current partner abuse | 6.5 | 4.9 | 2.9 |
| Multiple sex partners in last 30 days | 14.3 | 7.9* | 4.5 |
| Sex partner types in last 30 days | |||
| Primary male partner | 92.0 | 87.4 | 79.8 |
| Casual male partner(s) | 16.9 | 10.8* | 11.1 |
| Paying male partner(s) | 6.3 | 2.8* | 4.5 |
| Pregnant or trying | 4.3 | 5.9 | 5.3 |
| Used MC in last 30 days | 54.2 | 47.4 | 46.5 |
| Any unprotected sex in last 30 days | 63.6 | 53.6 | 51.4 |
| Network exposure to FC information | 64.4 | 71.1 | 69.5 |
| FC use | |||
| Ever used FC | 28.6 | 77.7 | 80.2 |
| Used FC in last 30 daysa | 28.0 | 67.7 | 34.4 |
| Total times used FC | |||
| Never | 71.4 | 22.3 | 19.8 |
| Once | 8.5 | 33.1 | 23.5 |
| 2–10 times | 14.3 | 37.7 | 41.6 |
| >10 times | 5.9 | 6.9 | 15.2 |
| Cognitive factors: | |||
| FC knowledge, mean (SD), range 0–1 | 0.75* (0.22) | 0.86 (0.16) | 0.85 (0.16) |
| FC attitudes, mean (SD), range 1–4 | 2.80 (0.29) | 2.82 (0.30) | 2.79 (0.30) |
| FC efficacy, mean (SD), range 1–4 | 2.14 (0.73) | 2.15 (0.66) | 2.16 (0.71) |
| Relationship power, mean (SD), range 1–4 | 2.90* (0.42) | 2.93 (0.36) | 2.93 (0.38) |
Significance reflects differences between participants who dropped out of and those who returned to the study for the subsequent assessment. Statistical tests reported for attrition analyses are Pearson chi-square test for categorical variables and one-way analysis of variance (ANOVA) tests for continuous measures.
Only participants who reported ever having used female condom (FC) at that time point are included in prior 30 day use (baseline n=132; 1-month n=303; 10-month n=195).
p<0.05.
MC, male condom; SD, standard deviation; STI, sexually transmitted infection.
We found that the potential effects of attrition on analysis of the returned subgroups of women who entered the study and their FC use were minimal. In comparing those who returned for the 1-month survey with those who did not (n=71), only FC knowledge and relationship power with primary partners were significantly different (p=0.01 and p=0.03, respectively), with dropouts reporting less knowledge and less relationship power at baseline. However, the 10-month sample included significantly fewer homeless, more crack users, fewer women with multiple sex partners, and more women with casual or paying partners than the 1-month sample, although the numbers in the last two groups were extremely small. Alternative estimates of percentages of FC initiators and sustained FC users were derived under no-attrition hypotheses. When we imputed who among the dropouts would have initiated or sustained FC use, our estimates based on returning participants only were similar to the imputed ones.
FC use over time
Reported FC use changed significantly from baseline to the 1-month and from the 1-month to the 10 month surveys (Table 1), with more than twice as many women reporting having used FC in the prior 30 days at 1-month (68% of women who reported ever having used FC by that time point, (n=303, confidence interval [CI] 63-72) compared to baseline (28% of FC ever users at intake, n=132, CI 20-36). However, this dropped to about half that at 10 months (34% of women who had ever used FC by the final survey, n=195, CI 28-41). (All CI are reported at the 95% level.) The overall number of times women reported ever using FC also changed dramatically, with never users dropping from 71% (CI 67-76) of the total sample at baseline to 22% (CI 18-26) of the total 1-month sample and 20% (CI 16-24) of the total 10-month survey participants. Further, the percent of women who reported lifetime use of FC 2–10 times more than doubled between baseline (14%, CI 11-17) and 1 month (38%, CI 33-42), and the percent who reported lifetime FC use >10 times doubled between 1 month (7%, CI 4-9) and 10 months (15%, CI 11-20).
Table 2 presents the characteristics of women who reported ever having used FC before entering the study and, among ever users, those who used FC in the prior 30 days at baseline. Women who reported ever having used FC at baseline were significantly more likely to be high school graduates, divorced/widowed, have multiple sex partners, have used MC in the prior 30 days, and have been exposed to FC information through someone in their network; they were less likely to be married/living with a partner, homeless, or injection drug users. Those ever users who reported having used FC in the prior 30 days at baseline were significantly less likely to have used alcohol to intoxication or have a casual sex partner than those who had not used FC recently. Both ever users and prior 30-day users were also significantly less likely to have had any unprotected sex in the prior 30 days. Further, both FC ever users and prior 30-day users had higher FC attitudes scores than did nonusers. Ever users also had higher FC knowledge and efficacy scores than never users, and prior 30-day users had higher relationship power scores than those who were not currently using FC.
Table 2.
Female Condom Users and Nonusers at Baseline (n=461)
| |
Ever used FC |
Used FC in last 30 Daysa |
||
|---|---|---|---|---|
| Baseline measures | Yes | No | Yes | No |
| Total % (n) | 28.6 (132) | 71.4 (329) | 28.0 (37) | 72.0 (95) |
| Ethnic group | ||||
| Black/African American | 58.3 | 54.4 | 56.8 | 58.9 |
| Puerto Rican/other Latino | 31.1 | 30.1 | 37.8 | 28.4 |
| White/other groups | 10.6 | 15.5 | 5.4 | 12.6 |
| High school graduate | 59.1b | 46.2 | 56.8 | 60.0 |
| Marital status | ||||
| Single | 57.6 | 55.9 | 54.1 | 58.9 |
| Married/living together | 18.2 | 28.0b | 13.5 | 20.0 |
| Divorced/widowed | 24.2b | 14.9 | 32.4 | 21.1 |
| Homeless | 25.0 | 30.4b | 18.9 | 27.4 |
| Substance use last 30 days | ||||
| Alcohol use until drunk | 34.8 | 29.5 | 21.6 | 40.0b |
| Injection drug use | 3.8 | 9.1b | 0 | 5.3 |
| Crack use | 34.1 | 33.1 | 32.4 | 34.7 |
| Past STI | 67.4 | 65.3 | 56.8 | 71.6 |
| HIV-positive (self-report) | 15.6 | 10.1 | 25.7 | 11.8 |
| Any physical/sexual abuse | 55.0 | 55.2 | 43.2 | 59.6 |
| Childhood abuse | 51.9 | 43.0 | 54.1 | 51.1 |
| Adulthood abuse | 49.6 | 48.2 | 37.8 | 54.3 |
| Multiple sex partners last 30 days | 21.7b | 12.5 | 10.8 | 26.1 |
| Sex partner types last 30 days | ||||
| Primary male partner | 94.7 | 90.9 | 94.6 | 94.7 |
| Casual male partner(s) | 18.9 | 16.1 | 8.1 | 23.2b |
| Paying male partners | 8.3 | 5.5 | 2.7 | 10.5 |
| Used MC last 30 days | 74.2b | 46.2 | 83.8 | 70.5 |
| Any unprotected sex last 30 days | 46.2 | 70.5b | 27.0 | 53.7b |
| Network exposure to FC information | 82.6b | 57.1 | 89.2 | 80.0 |
| Cognitive factors: | ||||
| FC knowledge, mean (SD), range 0–1 | 0.82b (0.18) | 0.72 (0.23) | 0.84 (0.18) | 0.81 (0.18) |
| FC attitudes, mean (SD), range 1–4 | 2.84b (0.33) | 2.78 (0.27) | 3.01b (0.27) | 2.77 (0.33) |
| FC efficacy, mean (SD), range 1–4 | 2.26b (0.69) | 2.09 (0.74) | 2.43 (0.62) | 2.19 (0.71) |
| Relationship power, mean (SD), range 1–4 | 2.95 (0.39) | 2.88 (0.43) | 3.11b (0.43) | 2.89 (0.35) |
Includes only participants who reported at baseline ever having used FC before entering the study (n=132).
Percentage or mean was significantly higher than the comparison group (p<0.05).
By the 1-month survey, after all women had received the baseline brief FC demonstration and four free FC1 samples, 200 women (i.e., 73% of the 275 women returning for the 1-month survey who had never used FC at baseline and could have initiated, CI 67-78) reported having used FC for the first time (Table 3). Significantly more FC initiators were injection drug users; they also had higher FC knowledge, attitudes, and efficacy scores than noninitiators.
Table 3.
Female Condom Initiators and Noninitiators at 1-month Survey (n=390)
| |
FC initiators at 1 month |
|
|---|---|---|
| 1-month measures | Yes | No |
| Total percent (n) of returned baseline FC never users | 72.7 (200) | 27.3 (75) |
| Ethnic group | ||
| Black/African American | 54.5 | 61.3 |
| Puerto Rican/other Latino | 31.0 | 24.0 |
| White/other groups | 14.5 | 14.7 |
| High school graduate | 48.5 | 40.0 |
| Marital status | ||
| Single | 62.5 | 74.7 |
| Married/living together | 24.0 | 16.0 |
| Divorced/widowed | 13.5 | 9.3 |
| Homeless | 22.0 | 32.0 |
| Substance use last 30 days | ||
| Alcohol use until drunk | 30.5 | 32.0 |
| Injection drug use | 8.0a | 1.3 |
| Crack use | 20.0 | 29.3 |
| Past STI | 57.3 | 59.5 |
| HIV-positive (self-report) | 12.1 | 8.6 |
| Any physical/sexual abuse | 50.0 | 48.6 |
| Childhood abuse | 38.6 | 32.9 |
| Adulthood abuse | 47.0 | 43.2 |
| Multiple sex partners last 30 days | 6.6 | 14.1 |
| Sex partner types last 30 days | ||
| Primary male partner | 94.3 | 88.5 |
| Casual male partner(s) | 10.0 | 13.3 |
| Paying male partners | 2.1 | 6.6 |
| Used MC last 30 days | 42.5 | 32.0 |
| Any unprotected sex last 30 days | 56.5 | 62.7 |
| Network exposure to FC information | 62.8 | 70.3 |
| Cognitive factors | ||
| FC knowledge, mean (SD), range 0–1 | 0.88a (0.15) | 0.79 (0.20) |
| FC attitudes, mean (SD), range 1–4 | 2.85a (0.29) | 2.70 (0.30) |
| FC efficacy, mean (SD), range 1–4 | 2.18a (0.62) | 1.96 (0.75) |
| Relationship power, mean (SD), range 1–4 | 2.94 (0.35) | 2.91 (0.32) |
Comparison of initiators/noninitiators includes only returning participants who reported never having used FC at baseline (n=275).
Percentage or mean was significantly higher than the comparison group (p<0.05).
By the 10-month survey, 80% of the returned sample reported ever having used FC (Table 4). Ever users at 10 months were significantly more likely than never users to be high school graduates and to report having experienced adult sexual or physical abuse. They were also significantly more likely to report MC use and less likely to have had any unprotected sex in the prior 30 days. Nearly a quarter of the total 10-month returning sample reported sustained FC use (24%, CI 18-29, 41% of those who used FC at baseline or 1 month, n=142, CI 33-49). Sustained users were more likely to have a primary partner, to have used MC in the prior 30 days, and to have been exposed to FC information in their networks; they were also less likely than nonsustained FC users to have had any unprotected sex in the prior 30 days at 10 months. Both 10-month ever users and sustained FC users reported higher FC knowledge and attitudes scores, and 10-month ever users had higher FC efficacy scores than never users.
Table 4.
Sustained Female Condom Users and Ever Users at 10-Month Survey (n=243)
| |
Total ever used FC at 10 monthsa |
Sustained FC use at 10 monthsb |
||
|---|---|---|---|---|
| 10-month measures | Yes | No | Yes | No |
| Total percent (n) | 79.6 (195) | 20.4 (48) | 40.8 (58) | 59.1 (84) |
| Ethnic group | ||||
| Black/African American | 56.9 | 70.8 | 51.7 | 53.6 |
| Puerto Rican/other Latino | 30.8 | 22.9 | 31.0 | 33.3 |
| White/other groups | 12.3 | 6.2 | 17.2 | 13.1 |
| High school graduate | 56.9c | 33.3 | 55.2 | 59.5 |
| Marital status | ||||
| Single | 60.5 | 66.7 | 58.6 | 52.4 |
| Married/living together | 23.1 | 25.0 | 25.9 | 29.8 |
| Divorced/widowed | 15.4 | 8.3 | 15.5 | 16.7 |
| Homeless | 16.4 | 25.0 | 12.1 | 11.9 |
| Substance use last 30 days | ||||
| Alcohol use until drunk | 32.8 | 37.5 | 25.9 | 38.1 |
| Injection drug use | 6.2 | 0 | 3.4 | 6.0 |
| Crack use | 27.2 | 37.5 | 20.7 | 29.8 |
| Past STI | 60.3 | 60.4 | 63.8 | 60.7 |
| HIV-positive (self-report) | 14.9 | 11.6 | 23.2 | 16.5 |
| Any physical/sexual abuse | 52.8 | 37.5 | 56.9 | 50.0 |
| Childhood abuse | 44.8 | 35.4 | 50.0 | 43.4 |
| Adulthood abuse | 51.5c | 33.3 | 56.9 | 47.0 |
| Multiple sex partners last 30 days | 6.3 | 7.1 | 2.0 | 6.8 |
| Sex partner types last 30 days | ||||
| Primary male partner | 92.6 | 88.9 | 94.8c | 94.0 |
| Casual male partner(s) | 10.3 | 14.6 | 8.6 | 7.1 |
| Paying male partners | 4.6 | 8.3 | 1.7 | 4.5 |
| Used MC last 30 days | 49.7c | 33.3 | 70.7c | 40.5 |
| Any unprotected sex last 30 days | 50.8 | 54.2c | 34.5 | 53.6c |
| Network exposure to FC information | 70.8 | 64.6 | 81.0c | 63.1 |
| Cognitive factors | ||||
| FC knowledge, score (SD), range 0–1 | 0.87c (0.15) | 0.81 (0.18) | 0.91c (0.13) | 0.85 (0.15) |
| FC attitudes, mean (SD), range 1–4 | 2.83c (0.29) | 2.61 (0.26) | 2.96c (0.28) | 2.77 (0.29) |
| FC efficacy, mean (SD), range 1–4 | 2.24c (0.65) | 1.86 (0.88) | 2.37 (0.59) | 2.16 (0.69) |
| Relationship power, mean (SD), range 1–4 | 2.95 (0.37) | 2.84 (0.42) | 3.01 (0.36) | 2.97 (0.38) |
Comparison of ever/never users includes the total 10-month survey sample (n=243).
Comparison of sustained/nonsustained users includes only participants who reported ever having used FC at either baseline or 1 month (n=142).
Percentage or mean was significantly higher than the comparison group (p<0.05).
We examined the significant association between FC use and MC use by comparing MC and FC users at each time point. We found that more women than expected were using both. This relationship held for women who reported unprotected sex as well as for those who had no unprotected sex. This is also indicated by the consistently higher use of MC among FC ever users (Tables 2, 3, and 4).
The cost of MC and moreso of FC can act as a barrier to using them. In our study, however, most women obtained most of their MC and FC free; 79%, 89%, and 87% had gotten MC free, and 90%, 96%, and 87% had gotten FC free at baseline, 1 month, and 10 months, respectively. Most women got FC from women's health clinics or community outreach programs.
Factors predicting initial and sustained FC use
Before testing models to identify factors that might predict initial and sustained FC use, we used bivariate analyses of factors associated with FC use outcomes and variation in samples returned for 1-month and 10-month surveys to assess the potential for attrition bias in our findings. Multiple imputations with bayesian estimation in AMOS 16 of logistic models predicting FC initiation from baseline variables that emerged as associated with initiation of FC use and of sustained use (namely, FC knowledge, attitudes and efficacy, relationship power with primary partner, injection drug use, MC use, and unprotected sex) indicated that of the 67 participants who did not return at 1 month and had not used FC at baseline, an average of 8 would have initiated use, resulting in an adjusted estimate of initiation of 61% (CI 56-66) rather than the 73% reported of the returned sample. Also, from similar imputations for sustained use, of the 37 participants who used FC at either baseline or 1 month and, therefore, might have become sustained users had they not dropped out at 10 months, an average of 7 are likely to have stayed FC users based on their other baseline characteristics that predicted sustained use. Thus, the 58 sustained users (from the sample of 243) (Table 4) would have changed to 65 (from a sample now of 177 potential sustained users), yielding an adjusted sustained use rate of 37% (CI 30-44) rather than the 41% reported in Table 4.
After assessing participant characteristics associated with FC use at each time point, we analyzed predictors of initial and sustained use over time. Based on ANOVA tests for comparisons of means, it appears that the main discriminating factors for both initiating and sustaining FC use are the FC cognitive measures (knowledge and attitudes) and FC efficacy for initiated use. Tables 3 and 4 illustrate these differences. Both women who initiated FC use (at 1 month) and sustained FC users had significantly higher average levels of FC knowledge and more positive FC attitudes than nonusers at each measurement point. FC initiators also reported higher levels of FC efficacy with primary partners. Sustained users also were more exposed to FC information from their networks and used more MC than those who did not sustain their FC use.
We tested these relationships with formal SEM models using the 1-month returned sample for initiated FC use and the 10-month returned sample for sustained FC use. In the first step, we tested as predictors age, education, homelessness, drug use, alcohol use, injection drug use, ever being abused, ever having an STI, having multiple sexual partners, MC use, power in the relationship, FC knowledge, FC attitudes, self-efficacy with FC, and network exposure to FC information. Predictors that were clearly not significant (p>0.2) were dropped, and models were reestimated. The final models retain the significant predictors, but we stopped excluding predictors when model fit indicated departure from the data. This led to keeping FC self-efficacy in both models. We then moved to testing longitudinal models, with autoregressive paths from prior-time predictors. This allowed us to test, for example, indirect effects of baseline FC attitudes on initiation through 1-month FC attitudes, as well as to specify an unexplained covariation between two 10-month predictors of sustained use.
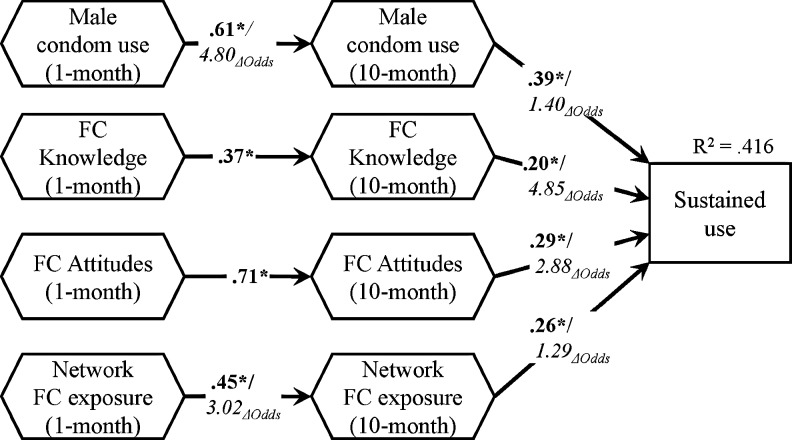
The final model for initiation of FC use (Fig. 1) had good fit (chi-square (11)=17.50, p=0.094) and showed significant direct effects from 1-month FC knowledge and 1-month FC attitudes to the outcome of initiated FC use at 1 month (odds ratio [OR] changes of 17.7 and 2.86, respectively, from the initial OR of FC initiation of 2.66—200 of 275). There were also significant indirect effects of baseline FC knowledge through 1-month knowledge and of baseline FC attitudes through 1-month attitudes; standardized effects β=0.18, p=0.007, OR change of 3.10, and β=0.19, p<0.001, OR change of 1.92, respectively (not shown). This suggests that higher baseline FC knowledge and attitudes indirectly impact the likelihood of initiation over and above the direct effects of the 1-month FC knowledge and attitudes.
FIG. 1.
Generalized linear model predicting initial female condom (FC) use 1 month after brief intervention. Bold numbers are standardized path coefficients; italics indicate odds changes caused by each predictor (n=266); initial odds of initiated FC use was 2.66; *p<0.05.
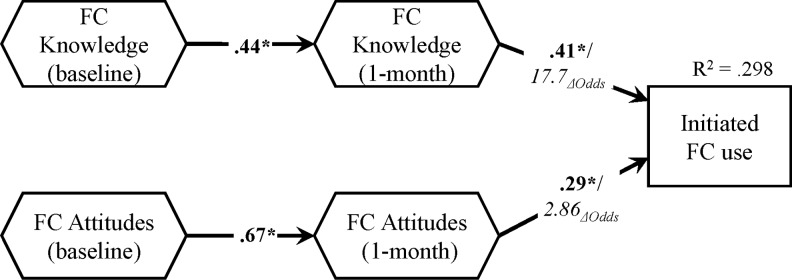
Figure 2 shows the final model of sustained FC use by 10 months after intervention. The main predictors were 10-month prior 30-day MC use, FC knowledge, FC attitudes, and network exposure to FC information (OR changes of 1.40, 4.85, 2.88, and 1.29, respectively, from the initial OR of sustained FC use of 0.69—58 of 142). The fit of the final model was chi-square (34)=51.26, p=0.03, WLSMV estimator. The only significant indirect effects were 1-month MC use through 10-month MC use (standardized effect estimate β=0.24, p=0.002, OR change of 1.71) and 1-month FC attitudes through 10-month FC attitudes (not shown). In both FC initiation and FC sustained use models, self-efficacy with primary partner at 10 months was also used as a predictor; however, its impact on either outcome was not significant.
FIG. 2.
Generalized linear model predicting sustained FC use 10 months after brief intervention. Bold numbers are standardized path coefficients; italics indicate odds changes caused by each predictor (n=134); * p<0.05; Δ Odds (change in odds)
Discussion
Despite ongoing efforts to find new effective approaches for prevention of sexually transmitted HIV and other STIs and the promise of early antiretroviral (ARV) treatment of HIV-infected individuals to prevent transmission to uninfected partners, consistent condom use and abstinence remain the most effective methods to prevent the spread of these infections. However, the MC requires full male cooperation, and very few women consider abstinence a viable option. One of the few effective and available options, the FC, remains severely underutilized and unsupported by healthcare and service providers, such as clinicians, nurses, and case managers, as well as prevention workers.9,16,36 Regardless of known, demonstrated FC acceptability among a wide variety of participants in numerous studies,9–11,13,14 few local communities nationally or internationally provide an environment that promotes the FC, including sufficient information, access, availability, and support for potential FC users.
Our study was designed to remove for all participants the most common barriers to FC use. Our 10–15-minute health education session feasibly could be incorporated into standard practice in clinical and health services settings, although it exceeds what is currently available in most such venues in our study city. Addition of known behavioral or social change intervention enhancements to this brief session might substantially increase FC adoption beyond what we achieved.37–41 Even without these enhancements, however, the brief session—for many women in the study, their first direct exposure to the FC—led over 43% of the baseline study sample to change from nonusers to initiated users, and at least 24% were still using FC 9 months after that.
It appears that first exposure to the product led to a dramatic increase in those reporting ever having used FC, as women tried it for the first time out of curiosity or because they saw immediate benefits. A combination of reduced interest, possible challenges with use, selection out by women who do not prefer the method (or whose partners reject it), and lack of availability in the community may have caused the notable reduction in continued use 9 months later. Further, the small number of women (n=9) who reported having initiated FC use between the 1-month and 10-month surveys suggests that trial use of the product is most likely to follow very soon after introduction to it. This is not unlike findings in several earlier studies in the United States and other countries demonstrating that a brief introduction of the product results in significant initial use, although longer-term continued use may be more moderate, and much use depends on available free samples.9,42–46 Nevertheless, introduction to the product with adequate information and supports, combined with ready availability, will likely make the FC a viable option to reduce overall unprotected sex even if it is not the preferred method and will certainly increase the number of users for whom it is the preferred or primary prevention option.
FC knowledge and attitudes proved to be common predictors of both initial and sustained use. Also, for FC use to be sustained, it appears that exposure to FC information from network members is beneficial, but sustained FC use also seems to be linked to consistent protective practices, as indicated by the effect of MC use. Furthermore, we found that prior knowledge and attitudes about FC indirectly predicted FC initiation, but only prior attitudes indirectly predicted sustained FC use. This suggests that interventions aiming to increase FC attitudes would provide added benefits in terms of both initiation and sustained FC use, and FC knowledge increases would particularly add to the impact on FC initiation.
FC attitudes were not extremely positive among users overall, although they were highest among current (prior 30 days) and sustained FC users. This suggests that small increases in positive attitudes about the FC might be sufficient for women to choose it as a prevention option. Negative attitudes toward MC among providers and users have not diminished the likelihood that widespread MC information and provision of free samples have prevented millions of infections worldwide. Similar support for the FC may have the same potential. However, negative provider views of FC as a failed product16–18 generate an ongoing barrier to its availability in the community for those who may wish to use it and benefit from its use and may even result in more negative attitudes among potential FC users.
Our initial hypothesis of predictors of initial and sustained FC use, based on previous multilevel analysis of factors predicting stage of FC use in the sample at baseline, was only partly supported by the analysis reported here. Educational attainment was associated with ever having used FC at both baseline and 10 months but did not predict either initial or sustained use. Likewise, childhood abuse history, HIV infection, and internal locus of control had no predictive value for either FC use pattern. No other demographic or risk characteristics remained significant in the final models, despite some indication that injection drug use and sex partner type were associated with initial and sustained use, respectively.
The significant association between MC use and FC use is not surprising. Negotiation of any type of condom with sex partners raises complex and multifaceted issues. These include partner trust, reproductive desires, religious values, gender power and roles, sexuality and sexual pleasure, and many other deep relationship, cultural, and social practices and beliefs.24 In this regard, MC and FC may not be largely different; thus, addressing and finding a comfortable solution to those issues with MC may facilitate the same with the FC. Nevertheless, initial and sustained FC users in this and other studies were not exclusively MC users, and FC use did not appear to replace MC use but rather to supplement it. This is suggested by the reduction in overall prior 30-day unprotected sex, along with a trend toward reduced MC use over time while FC use was increasing dramatically. This, too, has been found in other studies of FC introduction into populations in which some people were already using MC.22,47,48
Findings from this study indicate broad potential for uptake of the FC as a viable prevention option. This should encourage community healthcare and prevention service providers to create greater opportunity for FC use in order to expand women's ability to protect themselves from HIV and other STI. Evidence increasingly supports the development and testing of theoretically driven, multilevel interventions to increase community-wide availability, accessibility, and promotion of the FC.9,19,49,50 Undoubtedly, provision of free FC for some segment of the at-risk population is likely to be needed for sustained use because of the higher cost of this product, especially for low-income women and men. This seems reasonable and highly beneficial, however, given the high rate of free MC distribution that has occurred throughout the course of the worldwide HIV pandemic and the known value of that cost and effort.
This study has some limitations. The sampling method was designed to both reach a general population of urban women at elevated risk for HIV exposure because of high HIV prevalence rates in the study city and target women at high risk because of their own reported drug use, commercial sex work, or other HIV risks. Therefore, findings from this study might not be generalizable to some U.S. populations. Our FC use measures depended on self-report and could not be verified through other methods. However, women received no incentives to use FC and were provided additional FC at the follow-up surveys only if requested. Although we used multiple imputation methods to address the problem of missing data due to attrition, the counterfactual statement about how many would have initiated had they remained in the study is inherently of limited power, considering the limitation of having only baseline data to infer potential change due to an intervention. Finally, only FC1 were available at the time of this study, and outcomes might be different for other types of FC.
Since completion of our study, the FC2, a less expensive version of the FC1 made of synthetic latex instead of polyurethane, received U.S. Food and Drug Administration (FDA) approval and is being promoted in the United States and worldwide.51,52 Several other FC models are also in development, although more stringent regulations for FDA approval have hampered their availability.53,54 This continued evolution of the FC and other barrier methods that women can control has significant implications for the next generation of FC promotion and marketing to improve women's real access to these valuable options for protection. Unless substantial social and policy change accompanies the introduction of these and possibly other woman-initiate prevention options, such as microbicides, these products might face the same obstacles experienced to date with FC1, limiting their real potential to contribute to public health.
Acknowledgments
We greatly appreciate the tremendous effort of the field research team for their contributions to this study and this article, including Evelyn Baez, Mary Prince, Jennifer Salonia, and Michelle Garner. This project was funded by the National Institute of Mental Health (1R01MH069088). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health.
Disclosure Statement
The authors have no conflicts of interest to report.
References
- 1.Microbicide gel fails to work in large international trial. NAM Publications; [Google Scholar]
- 2.Pivotal HIV prevention trial for women in Africa finds that use of tenofovir gel does not prevent HIV: What does this mean for HIV prevention for women? www.global-campaign.org/clientfiles/GCM%20statement%20on%20the%20VOICE%20DSMB%20decision.pdf www.global-campaign.org/clientfiles/GCM%20statement%20on%20the%20VOICE%20DSMB%20decision.pdf
- 3.Global Campaign for Microbicides statement on the discontinuation of the FEM-PrEP trial. www.global-campaign.org/clientfiles/YH%20GCM%20Press%20Release%20FEM-PrEP%2019%20Apr%202011%20PROOFED%20FINAL.pdf www.global-campaign.org/clientfiles/YH%20GCM%20Press%20Release%20FEM-PrEP%2019%20Apr%202011%20PROOFED%20FINAL.pdf
- 4.Results of CAPRISA 004 a turning point for HIV prevention, say MTN researchers conducting VOICE. 2010. www.global-campaign.org/clientfiles/MTN_release_CAP004.pdf. [Jul 10;2011 ]. www.global-campaign.org/clientfiles/MTN_release_CAP004.pdf
- 5.CAPRISA 004: Tenofovir gel. 2010. www.global-campaign.org/CAPRISA004.htm. [Dec 8;2010 ]. www.global-campaign.org/CAPRISA004.htm
- 6.Report on the global AIDS epidemic. 2011. www.unaids.org/globalreport/documents/20101123_GlobalReport_full_en.pdf. [Jul 13;2011 ]. www.unaids.org/globalreport/documents/20101123_GlobalReport_full_en.pdf
- 7.French PP. Latka M. Gollub EL. Rogers C. Hoover DR. Stein ZA. Use-effectiveness of the female versus male condom in preventing sexually transmitted disease in women. Sex Transm Dis. 2003;30:433–439. doi: 10.1097/00007435-200305000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Galvao LW. Oliveira LC. Diaz J, et al. Effectiveness of female and male condoms in preventing exposure to semen during vaginal intercourse: A randomized trial. Contraception. 2005;71:130–136. doi: 10.1016/j.contraception.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 9.Vijayakumar G. Mabude Z. Smit J. Beksinska M. Lurie M. A review of female-condom effectiveness: Patterns of use and impact on protected sex acts and STI incidence. Int J STD AIDS. 2006;17:652–659. doi: 10.1258/095646206780071036. [DOI] [PubMed] [Google Scholar]
- 10.Busza J. Baker S. Protection and participation: An interactive programme introducing the female condom to migrant sex workers in Cambodia. AIDS Care. 2004;16:507–518. doi: 10.1080/09540120410001683457. [DOI] [PubMed] [Google Scholar]
- 11.Jivasak-Apimas S. Saba J. Chandeying V, et al. Acceptability of the female condom among sex workers in Thailand: Results from a prospective study. Sex Transm Dis. 2001;28:648–654. doi: 10.1097/00007435-200111000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Macaluso M. Wang X. Brill I, et al. Participation and retention in a study of female condom use among women at high STD risk. Ann Epidemiol. 2004;15:105–111. doi: 10.1016/j.annepidem.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 13.Witte SS. El-Bassel N. Gilbert L. Wu E. Chang M. Hill J. Promoting female condom use to heterosexual couples: Findings from a randomized clinical trial. Perspect Sex Reprod Health. 2006;38:148–154. doi: 10.1363/psrh.38.148.06. [DOI] [PubMed] [Google Scholar]
- 14.Napierala S. Kang MS. Chipato T. Padian N. Van der Straten A. Female condom uptake and acceptability in Zimbabwe. AIDS Educ Prev. 2008;20:121–134. doi: 10.1521/aeap.2008.20.2.121. [DOI] [PubMed] [Google Scholar]
- 15.Witte SS. Stefano K. Hawkins C. Can Medicaid reimbursement help give female condoms a second chance in the United States? Am J Public Health. 2010;100:1835–1840. doi: 10.2105/AJPH.2009.179598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peters A. Jansen W. van Driel F. The female condom: The international denial of a strong potential. Reprod Health Matters. 2010;18:119–128. doi: 10.1016/S0968-8080(10)35499-1. [DOI] [PubMed] [Google Scholar]
- 17.Hoffman S. Mantell J. Exner T. Stein Z. The future of the female condom. Int Fam Plann Perspect. 2004;30:139–145. doi: 10.1363/3013904. [DOI] [PubMed] [Google Scholar]
- 18.Mantell JE. Hoffman S. Exner TM. Stein ZA. Atkins K. Family planning providers' perspectives on dual protection. Perspect Sex Reprod Health. 2003;35:71–78. doi: 10.1363/3507103. [DOI] [PubMed] [Google Scholar]
- 19.Warren M. Philpott A. Expanding safer sex options: Introducing the female condom into national programmes. Reprod Health Matters. 2003;11:130–139. doi: 10.1016/s0968-8080(03)02178-5. [DOI] [PubMed] [Google Scholar]
- 20.Hoffman S. Smit JA. Adams-Skinner J. Exner T. Mandel J. Stein Z. Female condom promotion needed. Lancet Infect Dis. 2008;81:348. doi: 10.1016/S1473-3099(08)70109-9. [DOI] [PubMed] [Google Scholar]
- 21.Mantell JE. Hoffman JA. Weiss E, et al. The acceptability of the female condom: Perspective of family planning providers in New York City, South Africa, and Nigeria. J Urban Health. 2001;78:658–668. doi: 10.1093/jurban/78.4.658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weeks MR. Hilario H. Li J, et al. Multi-level social influences on female condom use and adoption among urban United States women. AIDS Patient Care STDs. 2010;24:297–309. doi: 10.1089/apc.2009.0312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weeks MR. Mosack K. Abbott M. Sylla LN. Valdes B. Prince M. Microbicide acceptability among high-risk urban U.S. women: Experiences and perceptions of sexually transmitted HIV prevention. Sex Transm Dis. 2004;31:682–690. doi: 10.1097/01.olq.0000143113.04524.a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Corbett M. Dickson-Gomez J. Hilario H. Weeks MR. A little thing called love: Condom use among high-risk primary heterosexual couples. Perspect Sex Reprod Health. 2009;41:218–224. doi: 10.1363/4121809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thompson SK. Adaptive sampling in behavioral surveys. NIDA Res Monogr. 1997;167:296–319. [PubMed] [Google Scholar]
- 26.Bronfenbrenner U. The ecology of human development. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- 27.McLeroy KR. Bibeau D. Steckler A. Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 28.Trickett EJ. Context, culture, and collaboration in AIDS interventions: Ecological ideas for enhancing community impact. J Primary Prev. 2002;23:157–174. [Google Scholar]
- 29.Pulerwitz J. Amaro H. DeJong W. Gortmaker SL. Rudd R. Relationship power, condom use and HIV risk among women in the USA. AIDS Care. 2002;14:789–800. doi: 10.1080/0954012021000031868. [DOI] [PubMed] [Google Scholar]
- 30.Neilands TB. Choi K. A validation and reduced form of the female condom attitudes scale. AIDS Educ Prev. 2002;14:158–171. doi: 10.1521/aeap.14.2.158.23903. [DOI] [PubMed] [Google Scholar]
- 31.Arbuckle J. Amos 16 user's guide. 16th. Chicago, IL: Marketing Department, SPSS Inc; 2007. [Google Scholar]
- 32.Skrondal A. Rabe-Hesketh S. Generalized latent variable modeling: Multilevel, longitudinal, and structural equation models. CRC Press; 2004. [Google Scholar]
- 33.Kline R. Principles and practice of structural equation modeling. 3rd. New York: Guilford Press; 2010. [Google Scholar]
- 34.Muthén LK. Muthén BO. Mplus user's guide. 6th. Los Angeles, CA: Muthén & Muthén; 1998–2010. [Google Scholar]
- 35.Judd C. Kenny D. Data analysis in social psychology: Recent and recurring issues. In: Fiske ST, editor; Gilbert DT, editor; Lindzey G, editor. Handbook of social psychology. Vol. 1. Hoboken, NJ: Wiley; 2009. pp. 113–137. [Google Scholar]
- 36.Mantell JE. Dworkin SL. Exner TM. Hoffman S. Smit JA. Susser I. The promises and limitations of female-initiated methods of HIV/STI protection. Soc Sci Med. 2006;63:1998–2009. doi: 10.1016/j.socscimed.2006.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fisher JD. Fisher WA. Bryan AD. Misovich SJ. Information-motivation-behavioral skills model-based HIV risk behavior change intervention for inner-city high school youth. Health Psychol. 2002;21:177–186. [PubMed] [Google Scholar]
- 38.Bandura A. Social cognitive theory and exercise of control over HIV infection. In: DiClemente RJ, editor; Peterson JL, editor. Preventing AIDS: Theories and methods of behavioral interventions. New York: Plenum Press; 1994. pp. 25–59. [Google Scholar]
- 39.Fogarty LA. Heilig CM. Armstrong K, et al. Long-term effectiveness of a peer-based intervention to promote condom and contraceptive use among HIV-positive and at-risk women. Public Health Rep. 2001;116:103–119. doi: 10.1093/phr/116.S1.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kelly JA. St Lawrence JS. Stevenson LY, et al. Community AIDS/HIV risk reduction: The effects of endorsements by popular people in three cities. Am J Public Health. 1992;82:1483–1489. doi: 10.2105/ajph.82.11.1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Weeks MR. Convey M. Dickson-Gomez J, et al. Changing drug users' risk environments: Peer health advocates as multi-level community change agents. Am J Community Psychol. 2009;43:330–344. doi: 10.1007/s10464-009-9234-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Telles Dias PR. Souto K. Page-Shafer K. Long-term female condom use among vulnerable populations in Brazil. AIDS Behav. 2006;10:S67–75. doi: 10.1007/s10461-006-9139-x. [DOI] [PubMed] [Google Scholar]
- 43.Artz L. Macaluso M. Brill I, et al. Effectiveness of an intervention promoting the female condom to patients at sexually transmitted disease clinics. Am J Public Health. 2000;90:237–244. doi: 10.2105/ajph.90.2.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Choi KH. Gregorich SE. Anderson K. Grinstead O. Gomez CA. Patterns and predictors of female condom use among ethnically diverse women attending family planning clinics. Sex Transm Dis. 2003;30:91–98. doi: 10.1097/00007435-200301000-00018. [DOI] [PubMed] [Google Scholar]
- 45.Hoffman S. Exner TM. Leu CS. Ehrhardt AA. Stein Z. Female-condom use in a gender-specific family planning clinic trial. Am J Public Health. 2003;93:1897–1903. doi: 10.2105/ajph.93.11.1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Van Devanter N. Gonzales V. Merzel C. Parikh NS. Celantano D. Greenberg J. Effect of an STD/HIV behavioral intervention on women's use of the female condom. Am J Public Health. 2002;92:109–115. doi: 10.2105/ajph.92.1.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fontanet AL. Saba J. Chandelying V, et al. Protection against sexually transmitted diseases by granting sex workers in Thailand the choice of using the male or female condom: Results from a randomized controlled trial. AIDS. 1998;12:1851–1859. doi: 10.1097/00002030-199814000-00017. [DOI] [PubMed] [Google Scholar]
- 48.Liao SS. Weeks MR. Wang Y, et al. Inclusion of the female condom in a male condom-only intervention in the sex industry in China: A cross-sectional analysis of pre- and post-intervention surveys in three study sites. Public Health. 2011;125:283–292. doi: 10.1016/j.puhe.2011.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Manhart LE. Holmes KK. Randomized controlled trials of individual-level, population-level, and multilevel interventions for preventing sexually transmitted infections: What has worked? J Infect Dis. 2005;191:1. doi: 10.1086/425275. [DOI] [PubMed] [Google Scholar]
- 50.Kaler A. The future of female-controlled barrier methods for HIV prevention: Female condoms and lessons learned. Culture Health Sex. 2004;6:501–516. [Google Scholar]
- 51.Food and Drug Administration notifications: FC2 female condom receives FDA approval. AIDS Alert. 2009;24:58–59. [PubMed] [Google Scholar]
- 52.Callahan B. Media release: Chicago AIDS advocates launch female condom campaign. Chicago: Female Health Company; 2010. [Google Scholar]
- 53.Beksinska M. Smit J. Joanis C. Usher-Patel M. Potter W. Female condom technology: New products and regulatory issues. Contraception. 2011;83:316–321. doi: 10.1016/j.contraception.2010.07.022. [DOI] [PubMed] [Google Scholar]
- 54.PATH. Woman's condom. Seattle, WA: The Program for Appropriate Technology in Health; 2009. [Google Scholar]