SUMMARY
Free flaps, with their very high rates of success and low donor site morbidity, are considered the gold standard in head and neck reconstruction, allowing the transfer of ideal tissues for head and neck reconstruction. Nonetheless, under certain circumstances they may be contraindicated or cannot be utilized. We describe four subjects in which delayed locoregional flaps were used to reconstruct head and neck defects after a previous flap failure. Due to adverse anatomic and systemic conditions these patients were not suitable for a free flap, and thus one delayed prelaminated temporalis fasciocutaneous flap placement and three delayed supraclavicular flap (one of which was prelaminated) placements to reconstruct large defects of the cheek and commissural region needed to be performed. All flaps and grafts were viable. All patients in this case series had acceptable functional and aesthetic outcomes. Donor-site morbidity was negligible. Delayed locoregional flap placement required a total of three surgical sessions. Although limited, our experience suggests that in cases in which a free flap is contraindicated or not ideal, locoregional flaps may be a valid and safe alternative. Limitations of these procedures include increased duration of hospitalization and, foremost, the need for three-step surgery.
KEY WORDS: Delayed flap, Locoregional flap, Free flap failure
RIASSUNTO
I lembi microvascolari rappresentano il gold standard nelle ricostruzioni cervico-cefaliche essendo affidabili e consentendo il trasferimento con tessuti ideali, pur mantenendo ridotti livelli di morbidità del sito donatore. Nel presente lavoro vengono descritti 4 casi di ricostruzioni cervico-cefaliche con lembi locoregionali autonomizzati dopo fallimento di precedenti lembi ricostruttivi. In questi pazienti l'uso di lembi liberi non era possibile per controindicazioni locali o sistemiche. La casistica consiste di un lembo prelaminato fasciocutaneo temporale e tre lembi autonomizzati sopraclavicolari (uno di questi era prelaminato) per ricostruire deficit maggiori cervico-facciali. Tutti i lembi e gli innesti sopravvivevano interamente. Risultati morfo-funzionali accettabili venivano raggiunti in tutti i pazienti della casistica. La morbidità dei siti donatori era trascurabile. L'esecuzione dei lembi locoregionali autonomizzati richiedeva un totale di 3 interventi chirurgici. La nostra esperienza suggerisce che nei rari casi in cui i lembi liberi siano controindicati o non ideali, i lembi locoregionali possono ancora rappresentare una alternativa valida e sicura. L'aumento dei tempi di degenza e la necessità di tre tempi chirurgici rappresentano la maggiore limitazione di queste procedure.
Introduction
Free flaps, combining a high success rate with low donorsite morbidity, are considered the gold standard for the reconstruction of tissues lost during oncologic surgery 1-5. In addition, they enable the reconstruction of different tissues lost during radical surgery. However, there are conditions that do not allow free flaps as the first choice, typically when the surgeon has no experience with microvascular surgery or when a patient is in poor general health with vascular depletion, or has had previous free flap failure, even though this latter issue is controversial. These cases are best managed with delayed placement of a locoregional flap. In addition, locoregional flaps are also suitable for use in combination with free flaps in extended reconstruction. In the present paper, our experience with the use of locoregional flaps in reconstructive procedures after the failure of locoregional or free flaps, and in a case where a free flap could not be performed, is presented.
Between 2008 and 2010, four delayed locoregional flap procedures were performed at the Division of Maxillofacial Surgery, San Paolo Hospital, Milan, Italy. One prelaminated temporalis fasciocutaneous flap was used to reconstruct a large defect of the cheek and commissural region after partial necrosis of a cervicofacial rotation flap for a skin squamous cell carcinoma. One prelaminated supraclavicular flap was used to reconstruct a full-thickness defect of the cheek after necrosis of a cervicofacial rotation flap and of the skin paddle of a fibular free flap for oral squamous cell carcinoma. One supraclavicular flap was used to reconstruct a cervicomandibular defect after necrosis of the skin paddle of a fibular free flap in a patient presenting with local recurrence of an oral squamous cell carcinoma who had received surgical and radiotherapy elsewhere. Finally, one supraclavicular flap was used to close a pharyngocutaneous fistula in a patient who had previously received total laryngectomy and radiotherapy for laryngeal cancer. In the first two patients, the delayed procedure was performed with a skin graft on the inner face of the flap. The wounds of all patients were infected at the time of the delayed procedure. All these patients had undergone functional neck dissection. Additionally, the third and fourth patients had previously received radiation therapy.
Case series
In the first case, a 75-year-old male (Figs. 1-4), heavy smoker and affected by severe chronic ischaemic heart disease was treated with bilateral functional neck dissection, full thickness resection of the right cheek, and reconstruction with a cervicofacial myocutaneous rotation flap for a cheek squamous cell carcinoma with nodal disease. The skin flap suffered from venous congestion and could not be salvaged. After removal of the necrotic tissues, a wide heavily infected wound resulted. In the same surgical session we performed the first reconstructive phase by partially sculpting (delay procedure) and covering the inner surface of a temporalis fasciocutaneous flap with a partial thickness skin graft from the thigh. Two weeks later, we rotated the flap to cover the defect of the cheek and commissure. The temporalis donor site was covered with a partial-thickness dermo-epidermal graft taken from the thigh. The patient was discharged 4 days later and, after another 2 weeks, the flap pedicle was divided under local anaesthesia.
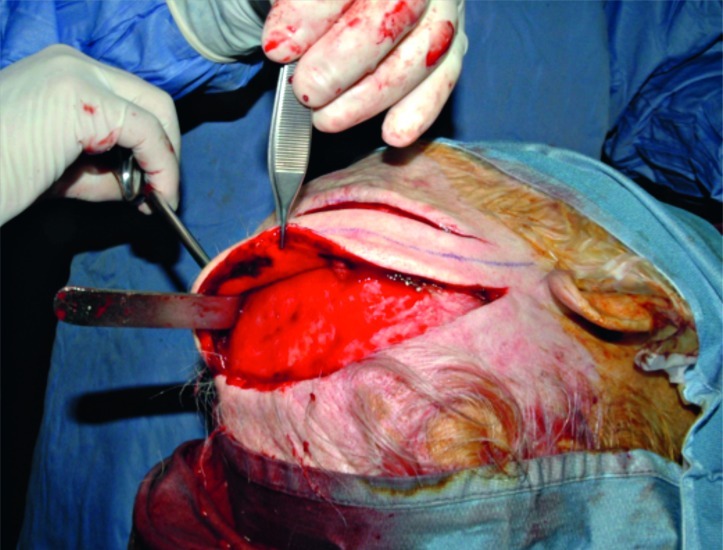
Fig. 1.
Case 1. A 75-year-old man with squamous cell carcinoma of the cheek with intraoral extension, treated with bilateral functional neck dissection, right cheek resection and reconstruction with a cervicofacial myocutaneous flap. The picture shows the lost tissue area after partial necrosis of the cervicofacial flap due to venous congestion.
Fig. 4.
The picture shows good aesthetic and functional outcomes of the procedure.
Fig. 2.
Delayed placement of a locoregional temporal fasciocutaneous flap with pedicle on the right superficial temporal vessels was performed. The distal flap portion was lined with a partial-thickness dermo-epidermal graft harvested from the thigh.
Fig. 3.
Flap rotation was performed to cover the defect of the cheek and commissure. The temporal donor site was covered with a partial-thickness dermo-epidermal graft harvested from the thigh.
The second patient, a 60-year-old male, heavy smoker and suffering from hypertension, underwent right neck dissection, a right hemimandibulectomy with wide excision of the right cheek and lower lip skin owing to squamous cell carcinoma of the right mandibular gum. Reconstruction was performed using a fibula free flap and a right cervicofacial myocutaneous flap. Within a few days after surgery, venous congestion developed in the cervicofacial flap that led to necrosis of the distal 6 cm of the flap. At the same time, the skin paddle of the fibula suffered from arterial ischaemia and had to be removed. No clear causes for the failure of the fibula flap skin paddle were apparent. After removal of nonviable tissue, a wide infected through and through wound resulted. In the same operation, under local anaesthesia, we sculpted (delay procedure) a supraclavicular flap and covered the inner flap surface with a splitthickness dermal-epidermal graft taken from the thigh. After 10 days, we rotated the flap in the right cheek under general anaesthesia to cover the defect. After another 15 days, the flap pedicle was divided under local anaesthesia. A third patient (Figs. 5-8), a 60-year-old female, heavy smoker with a history of alcoholism, was previously treated with mandibular resection, neck dissection and 60 Gy postoperative radiotherapy elsewhere for a squamous cell carcinoma of the oral mucosa. Owing to locoregional recurrence, we performed a mandibular and cheek resection and a reconstruction with a fibula osteocutaneous free flap. However, after 9 days the flap suffered from arterial ischaemia and complete thrombosis of the peroneal artery was noted: revision of the anastomosis could not save the flap. This was then removed and the wound closed primarily. In the following days, a complete wound breakdown developed, leaving the patient with a wide, infected defect of the cheek and mandibular region. We then sculpted partially (delay procedure) a supraclavicular flap under local anaesthesia. After 15 days, the flap was rotated to cover the cheek– cervical defect. Thirty days later, the flap pedicle was divided under local anaesthesia.
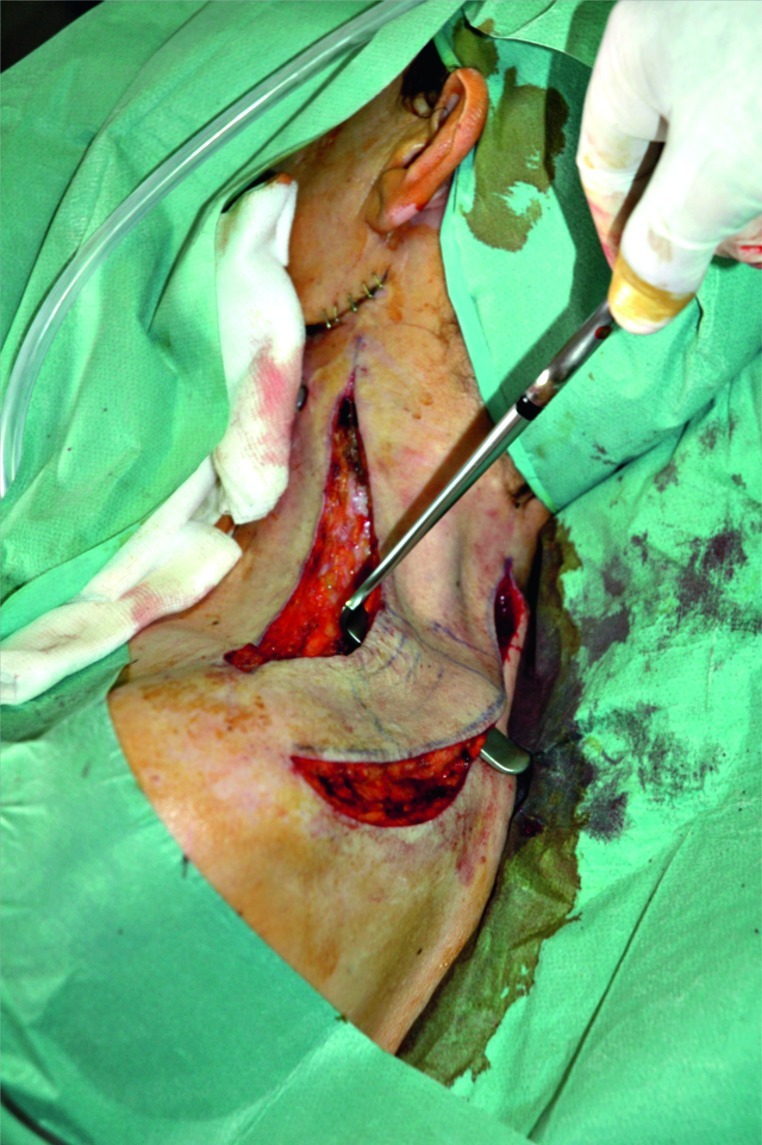
Fig. 5.
Case 2. A 60-year-old woman affected by a recurrent squamous cell carcinoma of the left mandible involving bone and surrounding soft tissues. She had undergone a left hemimandibulectomy with extensive soft tissues sacrifice and reconstruction with a microvascular fibula free flap with skin paddle. The picture shows complete wound dehiscence causing an 8 × 6 cm through-and-through defect.
Fig. 8.
The final result appears satisfactory.
Fig. 6.
A delayed supraclavicular flap procedure was performed under local anaesthesia.
Fig. 7.
Flap rotation was performed to cover the cheek–cervical defect.
A fourth patient, a 73-year-old male, heavy smoker with chronic heart failure had a pharyngocutaneous fistula after he underwent permanent tracheostomy, laryngectomy, and bilateral selective neck dissection (levels II–V) along with 60Gy postoperative radiotherapy for laryngeal cancer elsewhere. Under local anaesthesia, a delayed supraclavicular flap was sculpted. After 21 days, under general anaesthesia, a Wookey flap was used to close the inner surface of the fistula, and the supraclavicular flap was rotated over the latter to reconstruct the outer surface. After 60 days, the flap pedicle was divided under local anaesthesia.
Discussion
The use of free flaps for the reconstruction of large defects in head and neck surgery is today considered the gold standard with a success rate of nearly 95% 6. Very good morphological reconstruction can be obtained . With the aid of some conservative accesses to the condyle 7 8, mandibular reconstruction with free flaps can even be performed intraorally with only a small incision for anastomosis. For these reasons, free flaps are ideally suited for reconstruction after removal of benign tumours 9. Moreover, with some elegant techniques, donor site morbidity can be considered to be very low 10.
However, even if such high success rates are reported, free flaps can fail and several issues need to be addressed in such cases. Conservative management of a partial flap loss, with attention to potential infectious complications and possible exposure of delicate anatomic structures 11, is by and large the accepted procedure.
However, in cases of complete free flap loss, the nonviable tissue has to be removed with careful consideration for the best reconstructive option. Placement of a new free flap may be the first choice, unless prevented by local or systemic adverse conditions 12. Indeed, local infection and the unavailability of virgin vessels for anastomosis may severely contraindicate the placement of a second free flap, with a success rate reduced to 53% 13. All these factors indicate the importance of selecting the procedure used for locoregional flaps. Even primary reconstructions are better managed without free flaps under certain conditions, as diffuse atherosclerosis in both donor and recipient vessels, which increase significantly the difficulties and risks of anastomosis. Additionally, adverse systemic factors, such as ischaemic heart disease with a reduced ejection fraction or poorly controlled diabetes mellitus, may exclude some patients from free flap surgery, in consideration of the typically long microvascular surgical sessions. For such patients, locoregional flaps for reconstruction of the surgical defect is still the best management option.
Locoregional flaps have several advantages compared to free flaps, which include a reduced vulnerability to infection, thrombosis and other complications 14. Furthermore, considering that the procedure for locoregional flaps is easier and can be performed quicker15 than free flaps, they are also feasible also in centres where no microsurgical team is available. The most frequently used locoregional flaps for head and neck reconstruction are pectoralis myofasciocutaneous flaps 16 (first proposed by Ariyan 17 in 1979), supraclavicular flaps (Lamberty 18 1979), cervicofacial flaps (Crow 19 1976), cervicopectoral flaps (Becker 20 1978), deltopectoralis flaps (Conley 21 1953), scalp flap (Arena 22 1977), pedicled latissimus dorsi flap (Quillen 23 1978) and the temporalis flap (Dunham 24 1893). Some authors have proposed the use of a free flap in combination with a locoregional flap for reconstruction of larger surgical defects 25. This avoids the need to place multiple free flaps, which would increase operative time. The use of selected locoregional flaps to reconstruct the outer lining (facial skin) may also lead to better results in terms of colour and texture matching 25. Finally, cost remains an open issue; some authors 26 have argued that free flaps require more resources than locoregional flaps but enable better functional outcomes and are associated with fewer complications, thereby lowering the overall economic burden thus justifying their use. However, these aspects remain controversial.
In the present case series, one temporalis fasciocutaneous flap and three supraclavicular fasciocutaneous flaps were used in salvage procedures. The temporalis fascial flap was used as a pedicled flap based on the superficial temporal artery 27. The pedicle is usually located with a Doppler probe, and the flap is designed accordingly. According to the literature, this flap can be harvested as an island flap or pedicled flap 28. Its advantages include the good length of the pedicle and the choice of raising it as a composite flap. This procedure is usually performed in one session, but we preferred to raise the flap in a delayed procedure 28 in order to increase the chance of success. Complications specific to this flap are alopecia, donor-site hollowing and injury to the frontal branch of the facial nerve with eyebrow ptosis 29. This flap is very versatile and has various applications in the reconstruction of a variety of head and neck defects 28. We found it particularly well suited to the reconstruction of the upper half of the cheek and oral commissure. Colour and texture matching, although not ideal, are acceptable.
The trapezius-deltoid fasciocutaneous flap, or supraclavicular flap, is based on the supraclavicular artery, a branch of the transverse cervical artery. The typical size of the flap is 21 × 11 cm. If a flap with a width of < 10 cm is raised, the donor site can be closed primarily 30. Pallua 31 and Abe 32 have extensively studied the vascular anatomy of this flap. It can be raised as a pedicled, island or free flap. The advantages of this flap are minimal donor-site morbidity and acceptable colour and texture matching to facial and cervical skin. Its disadvantages are the shortness of the pedicle (1-7 cm) and anatomical variability in the supraclavicular artery 33. This flap is indicated for the reconstruction of the cervical region or lower third of the face 34. We have raised such flaps in delayed procedures in two patients without grafting the inner surface of the flap. In one patient, we reconstructed the inner lining of the cheek (oral mucosa) due to a through-and-through defect, which required the prelamination of the flap with a partial-thickness skin graft.
We decided to use these flaps for the following reasons. The failure of a free flap reduces the success rate of a second free flap, as mentioned above. Local infections subsequent to flap necrosis, the worsening of the patient's general condition, and the patient's refusal for the procedure can prevent the placement of a new free flap 35. Moreover, microvascular anastomosis is less favourable in an anatomical site previously subjected to surgery or radiation therapy. Some authors 25 consider the use of locoregional scalp or pectoralis flaps to be safer for head and neck reconstructions under certain circumstances. In three of the four cases described in our study, we chose to use a supraclavicular flap because of the location of the defect (the lower third of the face in two patients, a pharyngocutaneous fistula in one patient), the safety of this solution, especially as a delayed procedure and negligible donorsite morbidity (primary closure was performed in all three cases). The delayed placement of a supraclavicular flap was preferred over more routinely used locoregional flaps, such as the pectoralis flap, because we required a thin pliable flap in all cases, and routine musculocutaneous flaps are always bulky. Furthermore, a pectoralis flap is not ideal for use in women. In one case, we decided to use a fasciocutaneous temporalis flap because of the size and location of the defect (upper half of the cheek and oral commissure). All the flaps in the present case series could have been performed as a one stage procedure with the supraclavicular flaps raised as island flaps. However, the use of a delayed procedure for a locoregional flap may offer several advantages. The procedure is safer than immediate placement because it allows progressive autonomization of the vascular pedicle. This is especially true for the distal portion of the flap, which is almost always the most useful portion, but at the same time is most at risk for vascular compromise. In the case series reported here, we observed no minimal necrosis of the distal flap portions. This factor can be critically important in patients undergoing reconstruction after the failure of a previous flap and for whom no alternative is available.
The substantial disadvantage of a delayed procedure is that 7-15 days must pass before the flap can be placed safely. However, this time was required in all of our patients to eliminate necrosis and infection in the wound. No surgical procedure could have been performed earlier in these compromised sites.
Another disadvantage of a delayed locoregional interpolated flap placement is the necessity of three surgical sessions. Autonomization (and prelamination if necessary) is performed in the first session, flap rotation is performed in the second and pedicle division is performed in the third session. However, in all cases described here, autonomization and pedicle division were performed under local anaesthesia, and pedicle division was performed as an outpatient procedure, which reduced the economic burden of the entire procedure.
Conclusions
Free flaps represent the gold standard in head and neck reconstructive surgery. When a free flap is contraindicated or not ideal, locoregional flaps represent a valid alternative. The use of such flaps is also indicated when partial or total necrosis develops in previously placed locoregional or free flaps, which requires a salvage procedure. Local infections, adverse local conditions related to previous surgery or radiotherapy, and the patient's poor general condition may be contraindications for the placement of a second free flap. The delayed procedure guarantees greater safety of the flap and allows the prelamination of the inner flap surface in the correction of a through-and-through defect. Donor-site morbidity and aesthetic and functional outcomes appear to be acceptable. The increased duration of hospitalization and the need for three-step surgery represent the greatest limitations of these procedures, which are nonetheless invaluable under certain circumstances.
References
- 1.Giordano L, Bondi S, Ferrario F, et al. Radial forearm free flap surgery: a modified skin-closure technique improving donor-site aesthetic appearance. Acta Otorhinolaryngol Ital. 2012;32:158–163. [PMC free article] [PubMed] [Google Scholar]
- 2.Mura F, Bertino G, Occhini A, et al. Advanced carcinoma of the hypopharynx: functional results after circumferential pharyngolaryngectomy with flap reconstruction. Acta Otorhinolaryngol Ital. 2012;32:154–157. [PMC free article] [PubMed] [Google Scholar]
- 3.Baj A, Youssef DA, Monteverdi R, et al. Reconstruction of partial maxillary defects with the double-barrel fibula free flap. Acta Otorhinolaryngol Ital. 2010;30:299–302. [PMC free article] [PubMed] [Google Scholar]
- 4.Baj A, Bellocchio G, Marelli S, et al. Reconstruction of the anterior floor of the mouth using a peroneal perforator free flap. A case report. Acta Otorhinolaryngol Ital. 2010;30:47–51. [PMC free article] [PubMed] [Google Scholar]
- 5.Autelitano L, Colletti G, Bazzacchi R, et al. Ossification of vascular pedicle in fibular free flaps: a report of four cases. Int J Oral Maxillofac Surg. 2008;37:669–671. doi: 10.1016/j.ijom.2008.01.023. [DOI] [PubMed] [Google Scholar]
- 6.Gusenoff JA, Vega SJ, Jiang S, et al. Free tissue transfer: comparison of outcomes between university hospitals and community hospitals. Plast Reconstr Surg. 2006;118:671–675. doi: 10.1097/01.prs.0000233203.84078.6b. [DOI] [PubMed] [Google Scholar]
- 7.Biglioli F, Colletti G, et al. Mini-retromandibular approach to condylar fractures. J Craniomaxillofac Surg. 2008;36:378–383. doi: 10.1016/j.jcms.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 8.Biglioli F, Colletti G. Transmasseter approach to condylar fractures by mini-retromandibular access. J Oral Maxillofac Surg. 2009;67:2418–2424. doi: 10.1016/j.joms.2009.04.066. [DOI] [PubMed] [Google Scholar]
- 9.Biglioli F, Pedrazzoli M, Autelitano L, et al. The free fibula flap for treating benign mandibular lesions. Minerva Stomatol. 2007;56:349–358. [PubMed] [Google Scholar]
- 10.Squadrelli-Saraceno M, Compan A, Bimbi G, et al. Autonomous reparative unit (ARU): a new concept of repairing free flap donor site with local full-thickness skin graft. Acta Otorhinolaryngol Ital. 2010;30:40–46. [PMC free article] [PubMed] [Google Scholar]
- 11.Novakovic D, Patel RS, Goldstein DP, et al. Salvage of failed free flaps used in head and neck reconstruction. Head Neck Oncol. 2009;1:33–33. doi: 10.1186/1758-3284-1-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Okazaki M, Asato H, Takushima A, et al. Analysis of salvage treatments following the failure of free flap transfer caused by vascular thrombosis in reconstruction for head and neck cancer. Plast Reconstr Surg. 2007;119:1223–1232. doi: 10.1097/01.prs.0000254400.29522.1c. [DOI] [PubMed] [Google Scholar]
- 13.Bozikov K, Arnez ZM, et al. Factors predicting free flap complications in head and neck reconstruction. J Plast Reconstr Aesthet Surg. 2006;59:737–742. doi: 10.1016/j.bjps.2005.11.013. [DOI] [PubMed] [Google Scholar]
- 14.Genden E, Rinaldo A, Suarez C, et al. Complications of free flap transfers for head and neck reconstruction following cancer resection. Oral Oncol. 2004;40:979–984. doi: 10.1016/j.oraloncology.2004.01.012. [DOI] [PubMed] [Google Scholar]
- 15.Bhaya MH, Harel G. Resident training in head and neck flap reconstruction in U.S. academic otolaryngology programs. J Laryngol Otol. 2001;115:119–121. doi: 10.1258/0022215011907712. [DOI] [PubMed] [Google Scholar]
- 16.Montemari G, Rocco A, Galla S, et al. Hypopharynx reconstruction with pectoralis major myofascial flap: our experience in 45 cases. Acta Otorhinolaryngol Ital. 2012;32:93–97. [PMC free article] [PubMed] [Google Scholar]
- 17.Ariyan S. The pectoralis major myocutaneous flap: a versatile flap for reconstruction in the head and neck. Plast Reconstr Surg. 1979;63:73–81. doi: 10.1097/00006534-197901000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Lamberty BG. The supra-clavicular axial patterned flap. Br J Plast Surg. 1979;32:207–212. doi: 10.1016/s0007-1226(79)90033-x. [DOI] [PubMed] [Google Scholar]
- 19.Crow ML, Crow FJ. Resurfacing large cheek defects with rotation flaps from the neck. Plast Reconstr Surg. 1976;58:196–200. doi: 10.1097/00006534-197608000-00010. [DOI] [PubMed] [Google Scholar]
- 20.Becker DW. A cervicopectoral rotation flap for cheek coverage. Plast Reconstr Surg. 1978;61:868–870. [PubMed] [Google Scholar]
- 21.Conley JJ. The prevention of carotid artery hemorrhage by the use of rotating tissue flap. Surgery. 1953;34:186–194. [PubMed] [Google Scholar]
- 22.Arena S. The posterior scalping flap. Laryngoscope. 1977;87:98–104. doi: 10.1288/00005537-197701000-00012. [DOI] [PubMed] [Google Scholar]
- 23.Quillen CG, Shearin JC, Georgiade NG. Use of the latissimus dorsi myocutaneous island flap for reconstruction in the head and neck area: case report. Plast Reconstr Surg. 1978;62:113–117. doi: 10.1097/00006534-197807000-00028. [DOI] [PubMed] [Google Scholar]
- 24.Dunham T. A method for obtaining a skin-flap from the scalp and a permanent buried vascular pedicle for covering defects of the face. Ann Surg. 1893;17:677–679. [PMC free article] [PubMed] [Google Scholar]
- 25.Bianchi B, Ferri A, Ferrari S, et al. Free and locoregional flap associations in the reconstruction of extensive head and neck defects. Int J Oral Maxillofac Surg. 2008;37:723–729. doi: 10.1016/j.ijom.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 26.Tsue TT, Desyatnikova SS, Deleyiannis FWB, et al. Comparison of cost and function in reconstruction of the posterior oral cavity and oropharynx free vs pedicled soft tissue transfer. Arch Otolaryngol Head Neck Surg. 1997;123:731–737. doi: 10.1001/archotol.1997.01900070075012. [DOI] [PubMed] [Google Scholar]
- 27.Chen T-H, Chen C-H, Shyu J-F, et al. Distribution of the superficial temporal artery in the Chinese adult. Plast Reconstr Surg. 1999;104:1276–1276. doi: 10.1097/00006534-199910000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Tan O, Atik B, Ergen D. Temporal flap variations for craniofacial reconstruction plast. Reconstr Surg. 2007;119:152e–163e. doi: 10.1097/01.prs.0000261038.49905.b6. [DOI] [PubMed] [Google Scholar]
- 29.Ozdemir R, Sungur N, Sensöz O, et al. Reconstruction of facial defects with superficial temporal artery island flaps: a donor site with various alternatives. Plast Reconstr Surg. 2002;109:1528–1535. doi: 10.1097/00006534-200204150-00007. [DOI] [PubMed] [Google Scholar]
- 30.Vinh VQ, Anh T, Ogawa R, et al. Anatomical and clinical studies of the supraclavicular flap: analysis of 103 flaps used to reconstruct neck scar contractures. Plast Reconstr Surg. 2009;123:1471–1471. doi: 10.1097/PRS.0b013e3181a205ba. [DOI] [PubMed] [Google Scholar]
- 31.Pallua N, Magnus Noah E. The tunneled supraclavicular island flap: an optimized technique for head and neck reconstruction. Plast Reconstr Surg. 2000;105:842–851. doi: 10.1097/00006534-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 32.Abe M, Murakami G, Abe S, et al. Supraclavicular artery in Japanese: an anatomical basis for the flap using a pedicle containing a cervical, nonperforating cutaneous branch of the superficial cervical artery. Okajimas Folia Anat Jpn. 2000;77:149–154. doi: 10.2535/ofaj1936.77.5_149. [DOI] [PubMed] [Google Scholar]
- 33.Liu PH, Chiu ES. Supraclavicular artery flap: a new option for pharyngeal reconstruction. Ann Plast Surg. 2009;62:497–501. doi: 10.1097/SAP.0b013e31818c9d7d. [DOI] [PubMed] [Google Scholar]
- 34.Chiu ES, Liu PH, Friedlander PL. Supraclavicular artery island flap for head and neck oncologic reconstruction: indications, complications, and outcomes. Plast Reconstr Surg. 2009;124:115–123. doi: 10.1097/PRS.0b013e3181aa0e5d. [DOI] [PubMed] [Google Scholar]
- 35.Wei FC, Demirkan F, Chen HC, et al. The outcome of failed free flaps in head and neck and extremity reconstruction: what is next in the reconstructive ladder? Plast Reconstr Surg. 2001;108:1154–1160. doi: 10.1097/00006534-200110000-00007. [DOI] [PubMed] [Google Scholar]