SUMMARY
The present retrospective analysis evaluated the outcomes of different flap reconstructions for several hypopharyngeal defects in 136 patients who underwent hypopharyngeal reconstruction with a free or pedicled flap after excision of pharyngeal or laryngeal carcinoma.
Functional and oncological outcome were the main measures. Nine patients had a type I-a hypopharyngeal defect (partial with larynx preserved), 33 type I-b (partial without larynx preserved), 85 type II (circumferential), 5 type III (extensive superior) and 4 vertical hemipharyngolaryngectomy. The flaps used to reconstruct these defects were pectoralis major (n = 34), free radial forearm (n = 25), jejunum (n = 72), pedicled latissimus dorsi (n = 2), sternocleidomastoid (n = 1), lateral thigh (n = 1) and deltopectoral (n = 1). Twelve defects (9%) needed a secondary flap reconstruction. Surgical and medical complications were seen in 29% and 8% of patients, respectively; 18% of patients developed a fistula. No difference in complication rate or admission days was found for pre-operative versus no previous radiotherapy, type of defect or free versus pedicled flap. After 12 months follow-up, 38% of patients had a tracheo-oesophageal voice prosthesis, in 82% a fully oral diet was obtained and the average body weight gain was 0.9 kg. Five-year overall and disease-specific survival rates were 35% and 49%, respectively, while local and regional control rates were 65% and 91%, respectively. Considering these results, a defect orientated approach may be helpful for deciding which flap should be used for reconstruction of the hypopharynx. An algorithm is proposed with similar functional and oncological outcomes for the different groups. The choice of flap should be based on expected morbidity and functional outcome.
KEY WORDS: Hypopharynx, Free flap, Myocutaneous flap, Reconstruction, Laryngopharyngectomy, Squamous cell carcinoma
RIASSUNTO
Questo studio si pone come obiettivo la valutazione dei risultati di diverse tipologie di ricostruzione chirurgica dell'ipofaringe. A tale scopo è stata condotta un'analisi retrospettiva su 136 pazienti sottoposti a ricostruzione ipofaringea mediante lembo libero o peduncolato in seguito ad asportazione di carcinoma squamoso del faringe o della laringe. Nella casistica esaminata, 9 pazienti hanno riportato un deficit tissutale ipofaringeo di tipo I-a (difetto parziale dell'ipofaringe con preservazione laringea), in 33 pazienti il deficit è stato di tipo I-b (parziale, senza preservazione laringea), in 85 di tipo II (difetto circonferenziale), 5 pazienti hanno presentato un difetto di tipo III (superiore esteso) ed infine in altri 4 pazienti è stata praticata un'emifaringolaringectomia verticale. Nell'approccio ricostruttivo si è fatto uso di lembi di grande pettorale (n = 34), radiale libero (n = 25), digiunale (n = 72), grande dorsale peduncolato (n = 2), sternocleidomastoideo (n = 1), laterale di coscia (n = 1) e deltoideo pettorale (n = 1). In 12 casi (9%) si è reso necessario un secondo intervento ricostruttivo. Nel 29% dei casi trattati si sono presentate complicanze di tipo chirurgico e in circa l'8% complicanze di tipo medico. La presentazione di una fistola è stata riscontrata nel 18% dei pazienti trattati. Per quanto riguarda il rischio di complicanze e la durata della degenza ospedaliera, non sono state osservate significative differenze tra i pazienti sulla base della tipologia di difetto ipofaringeo, tipologia di trattamento ricostruttivo impiegato (mediante lembi liberi o peduncolati) o in relazione al fatto che fossero stati impiegati protocolli di trattamento radioterapico pre-operatoria. A distanza di 12 mesi dal trattamento, il 38% dei pazienti era portatore di protesi tracheo-esofagea, l'82% era in grado di alimentarsi per os e l'incremento ponderale medio è risultato essere pari a 0,9Kg. A cinque anni i tassi di sopravvivenza globale e specifica per malattia erano del 35% e del 49% e le percentuali di controllo locale e regionale di malattia sono risultate essere il 65% e 91% rispettivamente. In accordo con quanto osservato, sembra che un approccio chirurgico orientato sulla base del tipo di difetto ipofaringeo sia utile alla scelta del lembo da utilizzare nella ricostruzione ipofaringea. Viene quindi proposto un algoritmo in grado di offrire risultati funzionali ed oncologici simili per i diversi gruppi di pazienti. La scelta del lembo dovrebbe essere basata infatti sulla morbidità e sui risultati funzionali attesi.
Introduction
The treatment of advanced squamous cell carcinoma of the hypopharynx is challenging in terms of disease outcome and optimal reconstruction after surgical ablation. When hypopharyngectomy is undertaken, either alone or in combination with laryngectomy, reconstructive surgeons are faced with the challenge of minimizing morbidity in a high-risk population while achieving adequate functional results with regard to swallowing and voice restoration. The hypopharynx moves the food bolus by a series of coordinated muscular contractions, while distension and vibration of the pharyngeal wall are responsible for phonation 1. Several reconstructive methods and flaps have been developed. The preferred reconstruction should minimize early post-operative complications that could prolong hospitalization and become life-threatening, maintain post-operative functions and decrease the degree of surgical invasiveness and donorsite morbidity.
The purpose of the current study is to evaluate the outcome of different flap reconstructions for several hypopharyngeal defects.
Materials and methods
Patients
A retrospective analysis was performed on all 136 patients who underwent hypopharyngeal reconstruction with a free or pedicled flap for squamous cell carcinoma of the hypopharynx or larynx in two university hospitals in Europe between 1990 and 2004. Details of patient and tumour characteristics are shown in Table I. In 97 patients, surgery was the primary treatment (86 primary and 11 second primary tumours), while in 39 patients salvage surgery was performed (2 residual and 37 recurrent tumours). Carcinomas were located in the piriform sinus (60%), posterior pharyngeal wall (15%), postcricoid region (10%), supraglottic (2%), glottic (1%) and neopharynx (12%). Two patients with piriform sinus carcinoma had a synchronous tumour (T1 oral cavity and T2 posterior pharyngeal wall carcinoma). The pathological post-operative TNM-stage for primary or second primary tumours is shown. Most of patients with recurrent, residual or second primary tumours had undergone previous radiotherapy (47/50 patients), which in 15 patients was combined with chemotherapy. To better characterize the preoperative physical condition of patients, the ASA score (American Society of Anesthesiologists) was retrospectively determined.
Table I.
Characteristics of 136 patients with hypopharynx reconstruction concerning: patient, previous tumour and treatment, and postoperative outcome details.
| Variables | No. of patients | % of patients | No. or percentage |
|---|---|---|---|
| Tumour site • Piriform sinus • Posterior pharyngeal wall • Postcricoid • Supraglottic • Glottic • Neopharynx |
82 21 14 2 1 16 |
60 15 10 2 1 12 |
|
| T classification; primary and second primary tumours, n = 95 • T1 • T2 • T3 • T4 |
1 11 41 42 |
1 12 43 44 |
|
| N classification; primary and second primary tumours, n = 95 • N0 • N1 • N2a • N2b • N2c • N3 |
24 9 5 37 18 2 |
25 10 5 39 19 2 |
|
| Tumour • Primary surgery – Primary tumour – Second primary tumour • Salvage surgery – Residual tumour – Recurrent tumour |
97 86 11 39 2 37 |
71 63 8 29 2 27 |
|
| Previous treatment • Radiotherapy • Chemoradiotherapy |
42 15 |
31 11 |
|
| ASA score • ASA 1 • ASA 2 • ASA 3 |
35 68 33 |
26 50 24 |
|
| Postoperative • Peri-operative mortality • Length of hospital stay (median) |
4 |
3 |
26 days (range 9-137) |
| Complications • Surgical – Fistula – Haemorrhage – Necrosis flap – Stenosis – Wound dehiscence – Abdominocele • Medical – Cardiovascular – Oedema brain – Mediastinitis – MOF – Hypotension |
40 24 10 4 3 2 1 11 7 1 1 1 1 |
29 18 7 3 2 2 1 8 5 1 1 1 1 |
|
| Postoperative chemo/radiotherapy • Radiotherapy • Chemotherapy |
79 9 |
58 7 |
|
| Oncological outcome (5-year) • LCR • RCR • OS • DSS |
65 % 91 % 35 % 49 % |
||
| Functional outcome • Weight (median) – Pre-operative – Discharge – 12 months • Diet (12 months); n = 85 – Fully oral – Gastric tube • Voice prosthesis (12 months); n = 106 |
70 15 40 |
82 18 38 |
66.1 kg 63.6 kg 67.0 kg |
MOF multi-organ failure; LRC local control rate; RCR regional control rate; OS overall survival; DSS disease specific survival
Retrospectively, the type of diet at discharge, at 6 and at 12 months after surgery was scored as normal, soft, fluid or tube feeding. For each patient, the worst type was taken into evaluation. Weight was determined at admission and discharge, and at 6 and 12 months thereafter. The number of patients with a voice prosthesis was determined to evaluate voice quality. Oncological outcome was evaluated by survival analysis. Treatment factors, e.g. postoperative complications and length of hospital stay were also scored.
Classification
Hypopharyngeal defects were classified as one of five types (Table II). Type I-a defects were partial defects with the larynx preserved, as with a partial pharyngectomy or a posterior pharyngeal wall defect. Type I-b defects also consisted of partial defects, but without the larynx preserved, as in a total laryngectomy with a partial pharyngectomy. Type II defects were total circumferential defects (total laryngectomy with total pharyngectomy) without resection of the base of the tongue. In type III defects, with extensive superior defects, total laryngopharyngectomy was extended with resection of the base of the tongue. A different type of defect was vertical hemipharyngolaryngectomy.
Table II.
Classification of defects and preferred flap reconstruction.
| Classification | Defect | Larynx preserved | Resection base of tongue | Preferred flap reconstruction |
|---|---|---|---|---|
| Ia | Partial | Larynx preserved | FRF | |
| Ib | Partial | Larynx not preserved | PM | |
| II | Total circumferential | Without base of tongue | Jejunum, FRF | |
| III | Extensive | With base of tongue | Jejunum, Myocutaneous | |
| Vertical hemilaryngopharyngectomy | FRF |
Definitions
For all oncological results (survival and disease control), the date of the first flap reconstruction was used as the starting point. If a flap was substituted by a second flap, the functional results were determined with the second flap in situ.
Surgical complications concerned only complications for which re-operation was required, while medical complications concerned only complications that required admission at an intensive care unit or that led to death.
Statistics
Descriptive statistics were used to evaluate patient and surgical characteristics, functional results (diet, weight and voice) and complications. Statistical differences between two independent groups were calculated by the chisquare test. The Trend test was used where appropriate. Oncological outcome was evaluated with Kaplan Meier survival analysis. Log rank was employed for comparison among different groups.
Results
Defects and reconstruction
Nine patients had a type I-a hypopharyngeal defect (partial with preserved larynx), 33 type I-b defect (partial without larynx preserved), 85 type II defect (circumferential), 5 type III defect (extensive superior) and 4 vertical hemipharyngolaryngectomy defect.
Flaps used to reconstruct these defects were pedicled pectoralis major (PM; n = 34), free radial forearm (FRF; n = 25), free jejunum (n = 72), pedicled latissimus dorsi (LD; n = 2), pedicled sternocleidomastoid (SCM; n = 1), free anterolateral thigh (ALT; n = 1) and pedicled deltopectoral (DP; n = 1).
A type I-a defect was mainly reconstructed by FRF (n = 7, 78%), while a type I-b defect was in most cases restored with PM (n = 24, 73%) or jejunum flap (n = 6, 18%). A type II defect was reconstructed with jejunum in 62 (73%) patients and with FRF in 12 (14%) patients. A type III defect was reconstructed with jejunum (n = 3, 60%), PM (n = 1, 20%) or LD flap (n = 1, 20%). All vertical hemipharyngolaryngectomies were reconstructed with FRF (Table III).
Table III.
Type of flap reconstructions according to type of defect.
| Type I-a partial with larynx preservation | Type I-b partial without larynx preservation | Type II total/circular | Type III extensive superior | Vertical hemipharyngolaryngectomy | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | n | % | |
| PM | 1 | 11.1 | 24 | 72.7 | 8 | 9.4 | 1 | 20 | 0 | 34 | 25 | |
| FRF | 7 | 77.8 | 2 | 6.1 | 12 | 14.1 | 0 | 4 | 100 | 25 | 18.4 | |
| Jejunum | 1 | 11.1 | 6 | 18.2 | 62 | 72.9 | 3 | 60 | 0 | 72 | 52.9 | |
| LD | 0 | 0 | 1 | 1.2 | 1 | 20 | 0 | 2 | 1.5 | |||
| SCM | 0 | 1 | 0 | 0 | 0 | 1 | 0.7 | |||||
| ALT | 0 | 0 | 1 | 1.2 | 0 | 0 | 1 | 0.7 | ||||
| DP | 0 | 0 | 1 | 1.2 | 0 | 0 | 1 | 0.7 | ||||
| Total | 9 | 100 | 33 | 100 | 85 | 100 | 5 | 100 | 4 | 100 | 136 | 100 |
PM: pectoralis major; FRF: free radial forearm; LD: latissimus dorsi; SCM: sternocleidomastoid; ALT: anterolateral thigh; DP: deltopectoralis
Twelve defects (9%) needed a secondary flap reconstruction. Flaps used for secondary reconstruction were PM (n = 5), jejunum (n = 5), LD (n = 1) and free lateral upperarm flap (n = 1).
For functional outcome, 42 patients with pedicled flap reconstruction and 94 patients with free flap reconstruction were evaluated.
Peri-operative mortality and morbidity
Four patients died within the first month after surgery (perioperative mortality 3%). The median length of hospital stay was 26 days (range 9-137 days). Forty patients (29%) experienced one or more post-operative surgical complication. Eleven patients (8%) experienced one or more post-operative medical complication. Considering all complications (more than 1 complication per patient possible), fistula was most frequently reported (24 patients, 18%). There were a total of 47 (35%) occurrences of fistulae (conservative and surgical management). Other surgical complications that required surgical intervention were bleeding in 10 patients (7%), necrosis of the flap in 4 patients (3%), stenosis in 3 patients (2%), wound dehiscence in 2 patients (1%) and abdominocele after harvesting of the jejunum transplant in 1 patient (1%). Medical complications were mainly cardiovascular (5%). Other medical complications that required admission at intensive care unit were oedema of the brain (n = 1, 1%), mediastinitis (n = 1, 1%), multi-organ failure (n = 1, 1%) and severe hypotension (n = 1, 1%) (Table I).
Subanalyses were performed among the following groups previous versus no previous radiotherapy, pedicled versus free flap reconstruction and with type I-b defect versus type II defect. To compare the complications per type of defect, we analyzed the two largest groups, partial pharyngectomy with a total laryngectomy (type I-b) and the total/circular defect (type II). No differences in the median length of hospital stay, or in surgical or medical complications, were found between subgroups. Type II defects seemed to have more surgical (29% versus 27%) and medical (11% versus 3%) complications, but this was not statistically significant.
Post-operative radiotherapy and/or chemotherapy
Seventy-nine (58%) patients received post-operative radiotherapy with curative intent (median total dose of 62.5 Gy), and 9 patients (7%) received post-operative chemotherapy.
Oncological outcome
The median follow-up period was 19 months (range 0.1- 143 months). Sixty-one patients (45%) developed a recurrence during follow-up. Five-year survival analysis showed a local control rate of 65%, regional control rate of 91%, overall survival of 35% and disease specific survival of 49% (Figs. 1, 2).
Fig. 1.
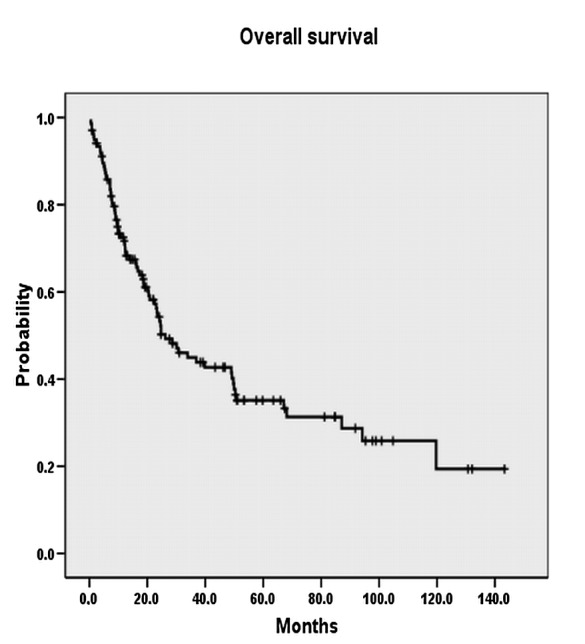
Overall survival (5-year 35%).
Fig. 2.
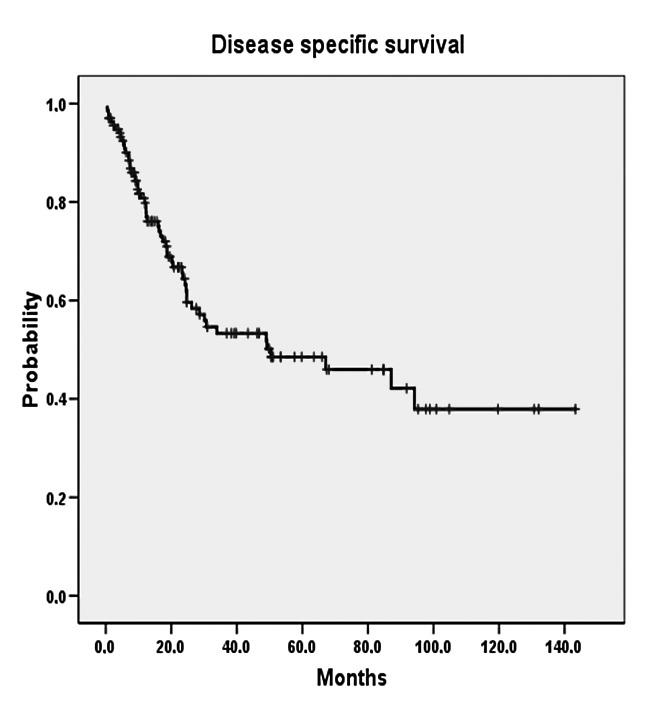
Disease specific survival (5-year 49%).
None of these survival analyses showed a statistically significant difference for the type of defect, previous radiotherapy, type of flap used for reconstruction or between primary tumour and salvage surgery (Fig. 3). Except for the disease control rate, where the group with a circumferential defect had significantly less recurrences than the group with a partial pharyngeal defect (type I-b) (Fig. 4; logrank: p = 0.04).
Fig. 3.
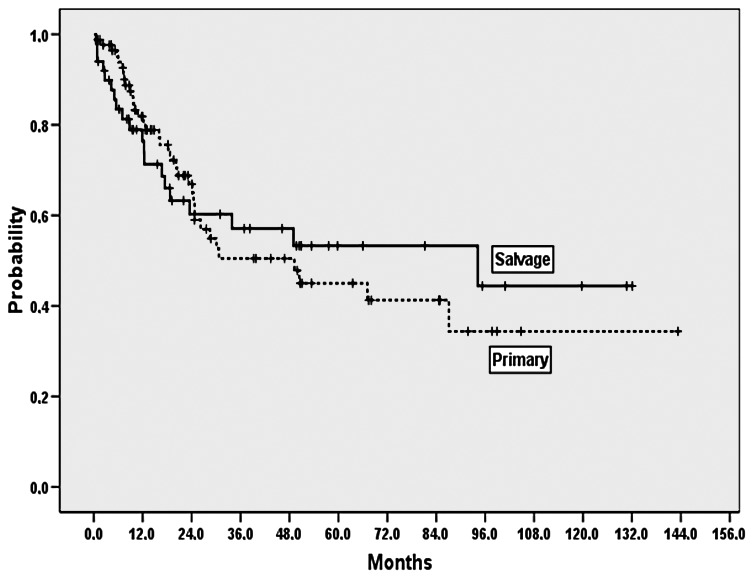
Overall survival. Primary versus salvage surgery (p = 0.42).
Fig. 4.
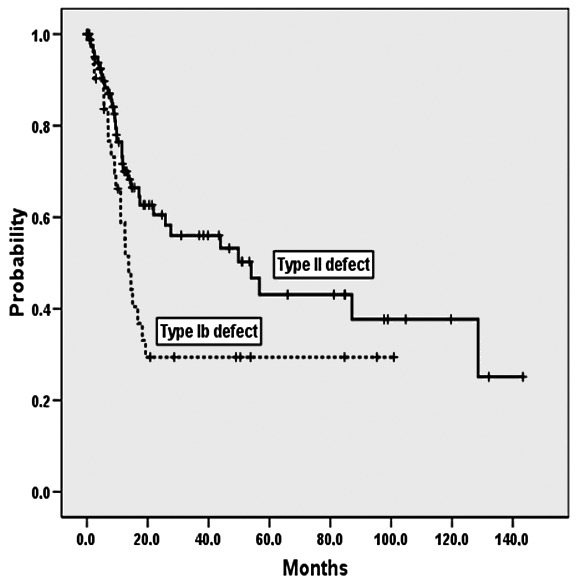
Disease free survival. Type I-b versus type II defect (p = 0.04).
Functional outcome
The mean weight of 66.1 kg decreased to 63.6 kg at discharge, and subsequently increased to a mean weight of 67 kg at 12 months after intervention. Patients were classified in quartiles according to preoperative weight (40- 56 kg, 56-63 kg, 64-74 kg and 75-106 kg). Subsequently, the percentage of weight loss or gain 6 months after operation was measured for each group (Fig. 5). Group 1 (with the lowest pre-operative weight) gained most, while group 4 (with the highest preoperative weight) lost most. The median of group 1 reached 100% recovery and thus returned to preoperative weight. The medians of the other groups did not (yet) recover to their preoperative weight.
Fig. 5.
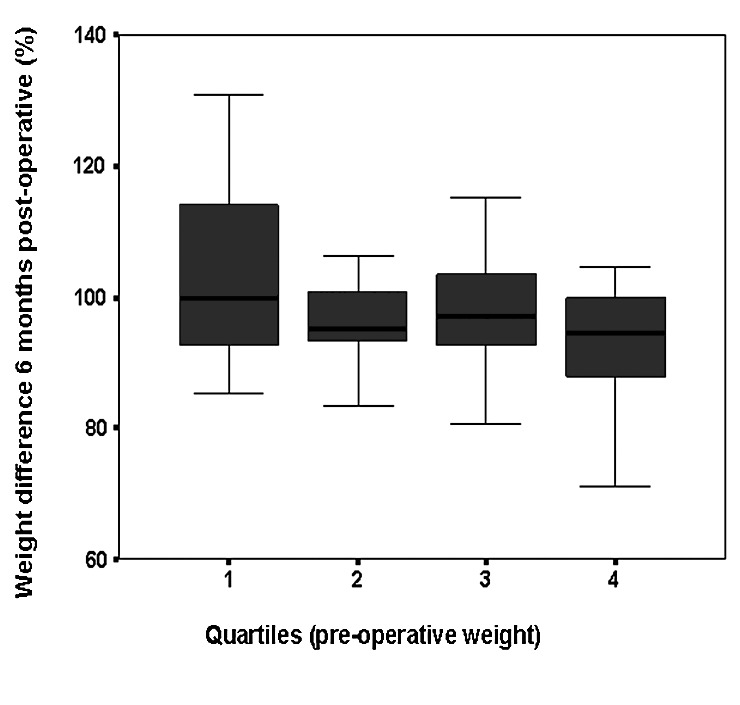
Percentage of weight gain or loss at 6 months post-operative for each quartile (weight pre-operative). Pre-operative median weight: quartile 1: 53 kg, quartile 2: 60 kg, quartile 3: 70 kg, quartile 4: 83 kg.
We also wanted to compare weight gain or loss between patients with free or pedicled flaps, with or without preoperative radiotherapy and with type Ib or II reconstructions. Therefore, we divided patients in the following post-operative groups (6 and 12 months): weight less than 90% of pre-operative weight, between 90% and 95% of pre-operative weight, between 95% and 100% of pre-operative weight and more than 100% of pre-operative weight. For both 6 months and 12 months after intervention, no statistically significant difference was found between the aforementioned groups. After 6 and 12 months, respectively, 61% and 68% of patients had a weight of 95% or more of pre-operative weight.
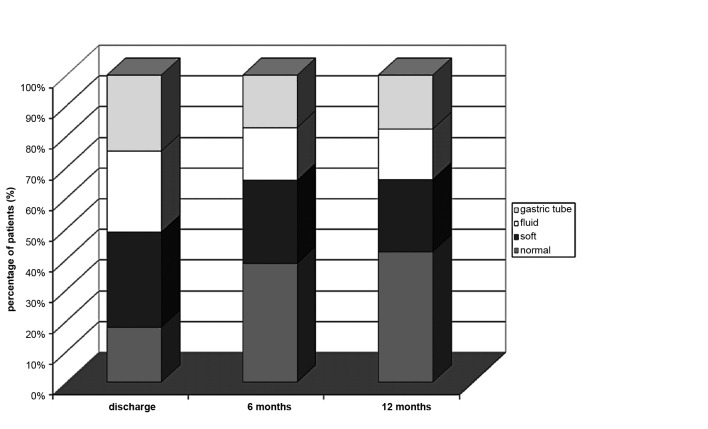
As with weight, diet subsequently improved from discharge to 12 months after intervention. At one year after intervention, 82% of patients had a fully oral diet. Nonetheless, 18% used a gastric tube for either total or supplemental nutrition (Fig. 6). The type of nutrition (representing swallowing function) was compared between groups: a) with versus without pre-operative radiotherapy, b) with versus without post-operative radiotherapy, c) classification Ib (partial defect without larynx preserved) versus II (total circumferential defect, without resection of base of tongue), d) pedicled versus free flap reconstruction and e) primary versus salvage surgery. The only statistically significant difference found was the type of nutrition at discharge between patients with a type Ib and those with a type II defect. Patients with a type Ib defect had a more normalized diet at discharge, but at 6 and 12 months post-operative this difference had disappeared.
Fig. 6.
Post-operative course of diet.
Of the patients with a laryngectomy who were still alive at one year after the operation, 38% had a voice prosthesis in situ. A significantly greater percentage of patients with a pedicled flap had a voice prosthesis compared to those with a free flap (51% versus 29%, p = 0.023). Circumferential defects were mainly reconstructed with free flaps, and were less accessible for voice prosthesis.
Discussion
When pharyngeal resection is required, special attention must be given to closure of the pharynx. If less than one-third of the circumference of the pharynx is resected, primary closure of the surgical defects is the method of choice for restoration of the continuity of the alimentary tract. When one-third to three-quarters of the pharyngeal circumference has been resected, satisfactory reconstruction is performed by utilizing pedicled flaps, (e.g. pectoralis major myocutaneous flap) or free vascularized flaps, (e.g. free radial forearm flap). If less than one-quarter is preserved, it is advocated to proceed with a circumferential pharyngectomy. When the circumferential pharyngeal defect extends to include the cervical and thoracic oesophagus, then gastric pull-up is the optimal choice of reconstruction. Microvascular methods to replace the pharyngo-oesophagus are the jejunum graft and tubed fasciocutaneous flaps, such as the radial forearm or the anterolateral thigh flap 2-4. After pharyngectomy with preservation of the larynx, non-bulky tissue, e.g. free fasciocutaneous flap, is needed. Reconstruction of the posterior pharyngeal wall poses a problem, since this area is vital in swallowing and a flap that is too bulky can easily induce untreatable aspiration and a poor quality of life 5.
Comparisons with other studies
Several classifications of defects of several sites have been proposed. Kimata et al. 6 distinguished defects after partial glossectomy, hemiglossectomy and (sub)total glossectomy. Urken et al. 7 described a classification scheme for composite defects of the oral cavity involving bone, soft tissue and neurologic defects. Disa et al. 8 developed a scheme for classification of hypopharyngeal defects. Type I defects were partial, involving less than 50% of the circumference. Type II defects were considered to be circumferential or involving greater than 50% of the circumference of the hypopharynx. Type III defects were extensive, non-circumferential deficiencies involving multiple anatomic levels including the nasopharynx, oropharynx, floor of mouth and mandible to varying degrees. In the present study, this classification scheme is modified, because of the following reasons. In partial defects, no distinction was made between larynx preservation or laryngectomy. Furthermore, the Disa classification considered a defect of more than 50% of the circumference to be circumferential. We did not consider a defect where a mucosal strip of one quarter of the circumference is left circumferential, since a patch can often still be used for reconstruction.
The peri-operative mortality of 2.9% was comparable with 0-3.3% found in other studies on hypopharyngeal reconstruction 8-10. In the present study, surgical and medical complications were seen in 29% and 8% of cases, respectively. Other studies on hypopharyngeal flap reconstruction have reported overall complication rates of 20-70% 8 9 11-19. The most frequently reported complication was fistula, in agreement with other studies 8-10. In the present analysis, no difference in morbidity or length of hospital stay was found between patients with or without previous irradiation, between patients with partial or circumferential pharyngeal defects or between patients with pedicled or free flap reconstruction. These findings are in contrast to other studies reporting that patients undergoing laryngectomy after previous irradiation, circumferential reconstruction or reconstruction with a pedicled flap have more complications 8 9 12 20-22.
The survival rates found in the present study (local control and overall survival rates of 65% and 35%, respectively) were comparable to the findings of Clarke et al. 9 23. The disease-free survival for patients with a circumferential defect was better than for patients with a partial pharyngeal defect. This difference is difficult to explain. On one hand, tumours that require circumferential pharyngeal resection may be more advanced than tumours which are resected by partial pharyngeal resection. On the other hand, circumferential defects may be a result of a resection with wider surgical margins compared to partial pharyngeal defects. Since no difference in duration of hospital stay and morbidity (complications) was found, wide surgical excisions are advocated in hypopharyngeal cancer treatment.
Herein, rough assessments for speech and swallowing functions were used. Voice restoration using tracheooesophageal voice prosthesis was performed in 38% of patients surviving hypopharyngectomy at least one year. This is similar to the 44-60% reported in other studies 9 10 24. We found a significant difference in the use of voice prosthesis between patients with a free flap (29%) and a pedicled flap reconstruction (51%). This may be caused by the fact that more free flaps are used for circumferential reconstruction compared to pedicled flaps.
A fully oral diet was obtained in 82% of patients, and about half of these had a normal diet. Twelve months after reconstruction 18% used a gastric tube for either total or supplemental nutrition. These results are comparable to the findings in other studies, which reported that about half of patients had an unrestricted oral diet, and 4-16% remained dependent on a gastric feeding tube 8-10 24.
We found an average body weight gain of 0.9 kg after 12 months compared to pre-operative average body weight. This is comparable with the results of Puttawibul et al. 25 on gastric pull-up for pharyngolaryngeo-oesophagectomy, who reported an average body weight gain of 0.3 kg after 6 months and 0.83 kg in total after 12 months. As for Bertino et al. 12, we found no statistically significant difference in mean body weight between patients with a free flap and those with a pedicled flap reconstruction.
To compare functional outcomes reliably, more extensive and detailed quality of life measurements are required. Speech outcome can be assessed by using indicators of speech production, speech perception (intelligibility and acceptability) and self-reported speech adequacy in every- day-life situations (questionnaires). Various methods are used to evaluate swallowing function including clinical evaluation, objective evaluation and questionnaires on swallowing problems. The type of reconstructive procedure used should be based on outcome data examining speech and swallowing function; however, there is a paucity of such information. Moreover, due to differences in methodology, the results as reported in the limited literature are difficult to compare.
Clinical applicability of the study
Since this is a descriptive study, a reconstructive algorithm, based on our findings, is difficult to design. To obtain this, a randomized clinical trial for each type of defect is warranted, but would probably be difficult to conduct. The choice of flap should be driven by donor site factors and functional outcome. Reconstructive aims need to be individualized based on predicted morbidity, expected disease outcomes, performance status and patient and surgeon preferences 9. Since the complication rates and functional outcome between patients with smaller and patients with larger or more complex defects were similar, it can be anticipated that the flaps used for reconstruction for the different defects were chosen well. Therefore, a defect oriented approach for reconstruction can be advocated.
For type I-a defects (partial defects with the larynx preserved), as after partial pharyngectomy, a free fasciocutaneous flap is preferred over a bulky flap. The same is true for defects after vertical hemipharyngolaryngectomy.
In type I-b defects, following total laryngectomy with partial pharyngectomy, bulk is not contraindicated. The pectoralis major flap has been extensively used for partial pharyngeal reconstructions with satisfactory outcome. This flap is reliable and easily to harvest. A type II defect (circumferential) needs to be reconstructed with a tubed structure. The free jejunum graft is naturally tubed through which one less suture line is needed. The jejunal free flap 26 can provide lubrication that keeps patients from being dry after irradiation. The free jejunal flap has a reliable vascular pedicle, and matches as a visceral flap the characteristics of the hypopharyngeal mucosa most closely: it is pliable and has some isoperistaltic motility. However, the donor site morbidity associated with abdominal surgery can be substantial. In addition, the voice has a "wet" quality and patients offer suffer intermittent dysphagia from uncoordinated peristalsis during deglutition. Fasciocutaneous flaps can easily be tubed. However, the vertical suture made to close the cylinder can add another point of potential weakness and dehiscence. Only in selected cases can a myocutaneous flap (with limited subcutaneous fat) be tubed and used to reconstruct a circumferential defect.
In type III defects with involvement of the base of tongue, depending on its extension, reconstruction may need some bulk. Therefore, in addition to tubed fasciocutaneous and enteric flaps, myocutaneous flaps, e.g. rectus abdominis, latissimus dorsi and pectoralis major flaps, may be useful to reconstruct this type of defect 8.
Conclusions
In conclusion, a defect orientated approach may be helpful in choosing the flap used for reconstruction of the hypopharynx. The choice of flap should to be based on expected morbidity and functional outcome. More extensive functional measurements are warranted to facilitate this decision. Since for the different hypopharyngeal defect groups outcome is generally similar, the algorithm presented seems suitable. The difference in survival for partial and circumferential defects indicates the need for wide resections in hypopharyngeal cancer.
References
- 1.Benazzo M, Bertino G, Lanza L, et al. Voice restoration after circumferential pharyngolaryngectomy with free jejunum repair. Eur Arch Otorhinolaryngol. 2001;258:173–176. doi: 10.1007/s004050100324. [DOI] [PubMed] [Google Scholar]
- 2.Baek CH, Kim BS, Son YI, et al. Pharyngoesophageal reconstruction with lateral thigh free flap. Head Neck. 2002;24:975–981. doi: 10.1002/hed.10144. [DOI] [PubMed] [Google Scholar]
- 3.Cho BC, Kim M, Lee JH, et al. Pharyngoesophageal reconstruction with a tubed free radial forearm flap. J Reconstr Microsurg. 1998;14:535–540. doi: 10.1055/s-2008-1040771. [DOI] [PubMed] [Google Scholar]
- 4.Hoorweg JJ, Rauwerda JA, Croll GA, et al. Free vascularized jejunum interposition for pharyngoesophageal reconstruction after total laryngopharyngectomy. Clin Otolaryngol Allied Sci. 1994;19:496–501. doi: 10.1111/j.1365-2273.1994.tb01276.x. [DOI] [PubMed] [Google Scholar]
- 5.Jol JK, Quak JJ, Bree R, et al. Larynx preservation surgery for advanced posterior pharyngeal wall carcinoma with free flap reconstruction: a critical appraisal. Oral Oncol. 2003;39:552–558. doi: 10.1016/s1368-8375(03)00037-x. [DOI] [PubMed] [Google Scholar]
- 6.Kimata Y, Sakuraba M, Namba Y, et al. Functional reconstruction with free flaps following ablation of oropharyngeal cancer. Int J Clin Oncol. 2005;10:229–233. doi: 10.1007/s10147-005-0500-2. [DOI] [PubMed] [Google Scholar]
- 7.Urken ML, Weinberg H, Vickery C, et al. Oromandibular reconstruction using microvascular composite free flaps. Report of 71 cases and a new classification scheme for bony, soft-tissue, and neurologic defects. Arch Otolaryngol Head Neck Surg. 1991;117:733–744. doi: 10.1001/archotol.1991.01870190045010. [DOI] [PubMed] [Google Scholar]
- 8.Disa JJ, Pusic AL, Hidalgo DA, et al. Microvascular reconstruction of the hypopharynx: defect classification, treatment algorithm, and functional outcome based on 165 consecutive cases. Plast Reconstr Surg. 2003;111:652–660. doi: 10.1097/01.PRS.0000041987.53831.23. [DOI] [PubMed] [Google Scholar]
- 9.Clark JR, Gilbert R, Irish J, et al. Morbidity after flap reconstruction of hypopharyngeal defects. Laryngoscope. 2006;116:173–181. doi: 10.1097/01.mlg.0000191459.40059.fd. [DOI] [PubMed] [Google Scholar]
- 10.Scharpf J, Esclamado RM. Reconstruction with radial forearm flaps after ablative surgery for hypopharyngeal cancer. Head Neck. 2003;25:261–266. doi: 10.1002/hed.10197. [DOI] [PubMed] [Google Scholar]
- 11.Azizzadeh B, Yafai S, Rawnsley JD, et al. Radial forearm free flap pharyngoesophageal reconstruction. Laryngoscope. 2001;111:807–810. doi: 10.1097/00005537-200105000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Bertino G, Spasiano R, Mazzola I, et al. The use of pedicled and free flaps in laryngeal cancer recurrences: postoperative considerations and functional results. Ann Plast Surg. 2005;55:384–388. doi: 10.1097/01.sap.0000178814.73683.30. [DOI] [PubMed] [Google Scholar]
- 13.Biel MA, Maisel RH. Free jejunal autograft reconstruction of the pharyngoesophagus: review of a 10-year experience. Otolaryngol Head Neck Surg. 1987;97:369–375. doi: 10.1177/019459988709700405. [DOI] [PubMed] [Google Scholar]
- 14.Bottger T, Bumb P, Dutkowski P, et al. Carcinoma of the hypopharynx and the cervical oesophagus: a surgical challenge. Eur J Surg. 1999;165:940–946. doi: 10.1080/110241599750008044. [DOI] [PubMed] [Google Scholar]
- 15.Bradford CR, Esclamado RM, Carroll WR, et al. Analysis of recurrence, complications, and functional results with free jejunal flaps. Head Neck. 1994;16:149–154. doi: 10.1002/hed.2880160208. [DOI] [PubMed] [Google Scholar]
- 16.Oniscu GC, Walker WS, Sanderson R. Functional results following pharyngolaryngooesophagectomy with free jejunal graft reconstruction. Eur J Cardiothorac Surg. 2001;19:406–410. doi: 10.1016/s1010-7940(01)00618-2. [DOI] [PubMed] [Google Scholar]
- 17.Stark B, Nathanson A. The free radical forearm flap: a reliable method for reconstruction of the laryngohypopharynx after in-continuity resection. Acta Otolaryngol. 1998;118:419–422. doi: 10.1080/00016489850183548. [DOI] [PubMed] [Google Scholar]
- 18.Teknos TN, Myers LL, Bradford CR, et al. Free tissue reconstruction of the hypopharynx after organ preservation therapy: analysis of wound complications. Laryngoscope. 2001;111:1192–1196. doi: 10.1097/00005537-200107000-00011. [DOI] [PubMed] [Google Scholar]
- 19.Triboulet JP, Mariette C, Chevalier D, et al. Surgical management of carcinoma of the hypopharynx and cervical esophagus: analysis of 209 cases. Arch Surg. 2001;136:1164–1170. doi: 10.1001/archsurg.136.10.1164. [DOI] [PubMed] [Google Scholar]
- 20.Chepeha DB, Annich G, Pynnonen MA, et al. Pectoralis major myocutaneous flap vs revascularized free tissue transfer: complications, gastrostomy tube dependence, and hospitalization. Arch Otolaryngol Head Neck Surg. 2004;130:181–186. doi: 10.1001/archotol.130.2.181. [DOI] [PubMed] [Google Scholar]
- 21.Ganly I, Patel S, Matsuo J, et al. Postoperative complications of salvage total laryngectomy. Cancer. 2005;103:2073–2081. doi: 10.1002/cncr.20974. [DOI] [PubMed] [Google Scholar]
- 22.Clark JR, McCluskey SA, Hall F, et al. Predictors of morbidity following free flap reconstruction for cancer of the head and neck. Head Neck. 2007;29:1090–1101. doi: 10.1002/hed.20639. [DOI] [PubMed] [Google Scholar]
- 23.Clark JR, Almeida J, Gilbert R, et al. Primary and salvage (hypo)pharyngectomy: Analysis and outcome. Head Neck. 2006;28:671–677. doi: 10.1002/hed.20428. [DOI] [PubMed] [Google Scholar]
- 24.Murray DJ, Novak CB, Neligan PC. Fasciocutaneous free flaps in pharyngolaryngo-oesophageal reconstruction: a critical review of the literature. J Plast Reconstr Aesthet Surg. 2008;61:1148–1156. doi: 10.1016/j.bjps.2007.09.030. [DOI] [PubMed] [Google Scholar]
- 25.Puttawibul P, Pornpatanarak C, Sangthong B, et al. Results of gastric pull-up reconstruction for pharyngolaryngooesophagectomy in advanced head and neck cancer and cervical oesophageal squamous cell carcinoma. Asian J Surg. 2004;27:180–185. doi: 10.1016/S1015-9584(09)60029-4. [DOI] [PubMed] [Google Scholar]
- 26.Giovanoli P, Frey M, Schmid S, et al. Free jejunum transfers for functional reconstruction after tumour resections in the oral cavity and the pharynx: changes of morphology and function. Microsurgery. 1996;17:535–544. doi: 10.1002/(SICI)1098-2752(1996)17:10<535::AID-MICR2>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]