SUMMARY
The objective of the present study was to compare the efficacy of functional endoscopic dilatation sinus surgery (FEDS) with functional endoscopic sinus surgery (FESS) in treatment of chronic rhinosinusitis in patients who failed medical therapy. We enrolled 24 patients suffering with chronic rhinosinusitis, who failed medical treatment and were proceeding to surgery, in a prospective, randomized controlled pilot study carried out between January and December 2008 following ethical committee approval. All patients completed sino-nasal outcome test (SNOT)-20 questionnaires and underwent saccharine test preoperatively and 24 weeks post operatively. Only trained surgeons performed surgery. The SNOT-20 questionnaire and saccharine clearance time (SCT) were used to measure outcomes. The SNOT-20 scores for both patient groups showed similar, consistent symptomatic improvement compared with baseline measures. SCT was reduced in both groups. No significant post-operative complications were recorded in either group. No patient in the FEDS group had any bleeding, and all were ready for discharge within hours of the procedure. Thus, FEDS is as effective as FESS in treatment of chronic rhinosinusitis. It is can be considered an additional tool in endoscopic surgery and has the potential to be undertaken as a day procedure.
KEY WORDS: Balloon sinuplasty, Chronic rhinosinusitis, FESS
RIASSUNTO
Obiettivo del nostro studio è stato paragonare l'efficacia della chirurgia endoscopica dilatativa funzionale (FEDS) con quella funzionale dei seni paranasali (FESS) in pazienti con rinosinusite cronica resistente a terapia medica. Il nostro è uno studio pilota prospettico, casocontrollo randomizzato. In questo studio (previa approvazione del comitato etico) sono stati arruolati, dal gennaio al dicembre 2008, 24 pazienti affetti da rinosinusite cronica resistente a terapia medica, con indicazione alla terapia chirurgica. Tutti i pazienti hanno compilato il questionario SNOT-20 e si sono sottoposti al test alla saccarina pre-operatoriamente e 24 settimane dopo l'intervento. Solo chirurghi esperti hanno eseguito l'intervento. I risulatati ottenuti con il questionario SNOT-20 erano simili nei due gruppi di studio e hanno messo in evidenza un importante miglioramento della sintomatologia rispetto ai valori di partenza. Il tempo di clearance muco ciliare con saccarina era ridotto in entrambi i gruppi. Non ci sono state complicanze post operatorie in nessun paziente e nessuno dei pazienti sottoposti a FEDS ha presentato sanguinamenti, è stato infatti possibile dimetterli tutti entro poche ore. Concludendo nella nostra casistica con la chirurgica dilatativa sinusale (FEDS) abbiamo ottenuto la stessa efficacia che con la FESS, nel trattamento della rinosinusite cronica. Inoltre tale metodica può essere considerata un valido strumento aggiuntivo nell'ambito della chirurgia endoscopica, con il vantaggio di poter essere effettuata in regime di day-surgery.
Introduction
Chronic rhinosinusitis (CRS) is a common condition; its precise incidence is difficult to estimate due to discrepancies in its definition. It is generally defined as the presence of two or more sino-nasal symptoms, one of which includes nasal obstruction, nasal blockage, congestion or nasal discharge with or without facial pain, facial pressure and reduction of smell or loss of smell 1 for a period of over 12 weeks. Endoscopic evidence of pus and/or oedema and CT scan findings of blocked osteomeatal patency helps in confirming diagnosis. The normal physiologic functioning of the sinuses depends on patency of the osteomeatal unit, normal mucociliary transport and normal quantity and quality of secretions. A popular hypothesis for the development of chronic rhinosinusitis is environmental factors, such as allergens; infectious agents including viruses, bacteria or fungi; or air pollutants, all of which stimulate the epithelium to induce local inflammation of the sinus mucosa 2. The resulting mucosal oedema leads to ostial obstruction and retention of secretions followed by bacterial proliferation. In response to inflammation, the lining epithelium may become metaplastic and ciliary dysfunction ensues, perpetuating the condition. Medical therapy is the primary treatment modality for patients with chronic rhinosinusitis in the form of antibiotics and topical nasal steroids. Over the past two decades, the surgical management of rhinosinusitis has entirely changed due to technical advances in endoscopic systems and the recognition of the importance of mucociliary flow and ventilation through the anatomical ostia for normal sinus function. Functional endoscopic sinus surgery (FESS) is a set of minimally invasive techniques in which sinus air cells and ostia are opened under direct visualisation. The goal of this procedure is to restore sinus ventilation and normal function.
The relative risks of sinus surgery have been the subject of controversy for many years. Several large series report a very low complication rate suggesting that this procedure can be done safely. FESS has now become well established for the treatment of chronic rhinosinusitis that is refractory to medical treatment. There is, however, a conspicuous lack of good scientific evidence of the comparative efficacy of this intervention.
Functional endoscopic dilatation of the sinuses (FEDS) is a new technique of sinus ostial balloon dilatation and is specifically aimed at restoring the patency of sinuses without removing any tissue thereby decreasing morbidity. Cadaver studies confirm the potential use of this method in rhinosinusitis 3. Clinical trials in the USA have also shown the safety and effectiveness in selected patients with rhinosinusitis 4. Some studies anecdotally reported that FEDS effectively relieves sinus ostial obstruction with less post-operative pain, scarring and bleeding than typically seen with traditional instruments 4.
Materials and methods
Patients
Patients (n = 24) with CRS who failed medical treatment and proceeding to surgery were randomly allocated to undergo either FESS or FEDS at Departments of Otolaryngology in Wigan and Leigh (Wrightington, Wigan and Leigh NHS Trust). These patients presented with a combination of 2 or more of the following symptoms including nasal obstruction/blockage, reduced sense of smell, excessive nasal catarrh, postnasal drip, headaches and facial pressure. Pre-operative CT scans of these patients showed blockage of osteomeatal complex, involving uni/bilateral frontal, ethmoidal and/or maxillary sinuses. The sphenoid sinus was clear in all patients. Only the blocked sinuses were opened with either traditional FESS or balloon dilatation, and sinuses were lavaged with saline intra-operatively. Patients in both treatment arms were encouraged to re-establish their routine activities as early as possible. Postoperatively, all patients were treated with Stérimar (saline spray) for 6 weeks, flixonase nasules (fluticasone propionate drops) for 4 weeks followed by flixonase/ nasonex (mometasone furoate monohydrate) nasal spray for 6 weeks. All patients were offered analgesics on an as required basis. They were all followed up at 6, 12 and 24 weeks after intervention.
Randomization
The R&D coordinator and trust statistician drew up a block randomisation list and enclosed the treatment allocations in consecutively numbered, sealed, opaque envelopes. The envelopes were stored securely in the clinic cupboard locker. They were accessed by senior sister in charge once the patient was recruited, and opened before allocating patients to either Group A (FEDS/study group) or Group B (FESS/control group).
Eligibility and exclusion criteria
Patients above 18 years of age suffering with chronic rhinosinusitis (diagnosis as per EPOS guidelines 1), not responding to medical treatment (in the form of topical steroids for 12 weeks with or without antibiotics) and willing to proceed for endoscopic sinus surgery were eligible for inclusion.
Patients with extensive sinonasal polyps, previous sinonasal surgery or trauma involving sinonasal complex, Sampter's Triad (aspirin sensitivity, asthma, sinonasal polyposis), sinonasal tumours or obstructive lesions, known ciliary dysfunction or cystic fibrosis, and pregnancy were excluded.
Design and ethics
This was an open, randomized controlled, pilot study; hence, both patients and researchers knew the full details of treatment. There is a challenge for bias, as we cannot use a placebo effect. Null Hypothesis: there is no difference between the two interventions FEDS (Group A) or FESS (Group B). Ethical committee approval was acquired from Northwest 6 Research Ethics Committee GM South. Funding for this study was obtained from Research & Development (R&D) department, Wrightington, Wigan & Leigh NHS Trust.
Outcome measures
Sinonasal outcome test (SNOT – 20) questionnaire; saccharine clearance time (SCT) preoperative and 6 months postoperative. Saccharine clearance time: In this test, we placed one saccharine pellet (5 mm diameter) in the floor of nasal cavity adjacent to anterior end of inferior turbinate. We then recorded the time when patients reported the sensation of tasting saccharine at back of mouth. This time interval was interpreted as the muco-ciliary clearance time.
Surgery
All procedures were done under general anaesthesia. Topical anaesthesia (5% cocaine in 1:1000 adrenaline) was used to prepare the nose before the procedure.
FEDS: To gain initial sinus access, the sinus guide catheter is introduced into the target sinus under endoscopic visualization. A flexible sinus guide wire is introduced through the sinus guide catheter and gently advanced into the target sinus. The sinus balloon catheter tracks smoothly over the sinus guide wire and positioned across the blocked ostium. The position of the sinus balloon catheter is confirmed using fluoroscopic guidance. It is gradually inflated to gently restructure the blocked ostium. The balloon sinuplasty system is removed, leaving the ostium open and allowing the return of normal sinus drainage and function. There is little to no disruption to mucosal lining. FESS: Uncinectomy, middle meatal antrostomy, opening of frontal recess and ethmoidectomy was done with specially designed instruments, mainly sickle knife, Freer's elevator, upturned Blakesley, backbiting forceps, trucut forceps and occasionally microdebrider. The instruments sharply cut small, precise pieces of tissue away, while any normal tissue is preserved and remains lining the sinuses. None of our participants needed a postoperative nasal pack, and bleeding was minimal in both groups. Both surgeries were performed only by trained surgeons, competent in performing endoscopic sinus surgery and additionally, attended cadaveric dissection courses for performing FEDS.
Results
Twenty four patients (Tab. I) were included in the study; 12 in the FESS group and 12 in the FEDS group. All patients in both groups were followed up to 6 months, and there were no dropouts. The mean Lund-Mackay score of CT scans 7.92 and 8.25 in the FEDS and FESS groups, respectively. The FEDS group of patients underwent mainly frontal dilatation in 17 sinuses and maxillary dilatation in 18 sinuses. One patient also had microdebrider polypectomy for grade 2 polyposis. The uncinate process was preserved in this case and the maxillary sinus was dilated with the balloon bilaterally. One patient had additional bilateral reduction of the concha bullosa. All FEDS patients underwent balloon dilatation under fluoroscopic guidance; the mean fluoroscopy exposure time was less than a minute. The FESS group of patients mainly underwent middle meatal antrostomy in 18 sinuses, anterior ethmoidectomy in 16 and opening of frontal recess in 14 sinuses. None of the patients in either treatment group had posterior ethmoidectomy or sphenoidotomy.
Table I.
Patient characteristics and CT Lund Mackay scores.
| FEDS Group | FESS Group | ||||||
|---|---|---|---|---|---|---|---|
| Case (Age, sex) |
Pre-op SNOT-20 | Pre-op SCT | CT sinus Lund Mackay score |
Case (Age, sex) |
Pre-op SNOT-20 | Pre-op SCT | CT sinus Lund Mackay score |
| 64, M | 78 | 12 | 5 | 44, F | 34 | 12 | 4 |
| 30, F | 84 | 30 | 6 | 36, F | 40 | 15 | 6 |
| 30, F | 85 | 15 | 4 | 51, F | 68 | 15 | 7 |
| 30, F | 47 | 12 | 6 | 46, F | 45 | 8.4 | 8 |
| 33, F | 79 | 16 | 4 | 39, F | 39 | 20 | 14 |
| 49, M | 51 | 15 | 6 | 39, F | 44 | 16 | 14 |
| 41, M | 58 | 15 | 8 | 43, F | 92 | 16 | 4 |
| 33, F | 56 | 12 | 16 | 33, F | 71 | 10 | 14 |
| 52, F | 68 | 14 | 16 | 36, F | 61 | 11 | 10 |
| 30, F | 51 | 10 | 8 | 48, M | 44 | 14 | 8 |
| 40, F | 64 | 12 | 12 | 29, M | 34 | 16 | 4 |
| 35, F | 43 | 20 | 4 | 52, F | 48 | 12 | 6 |
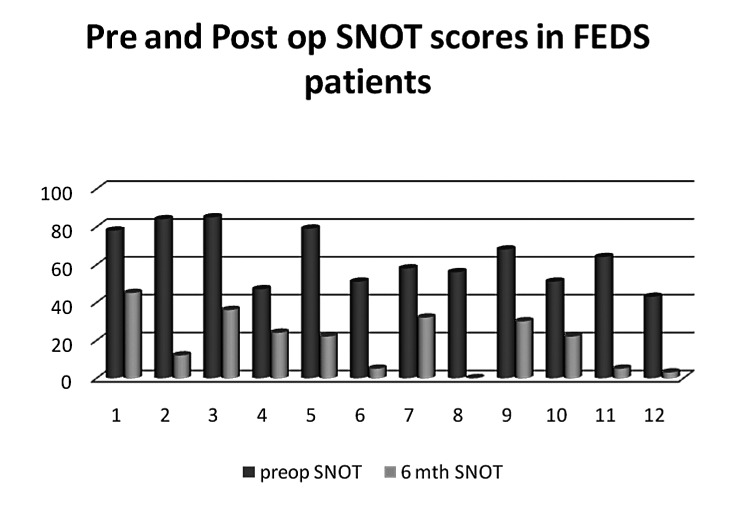
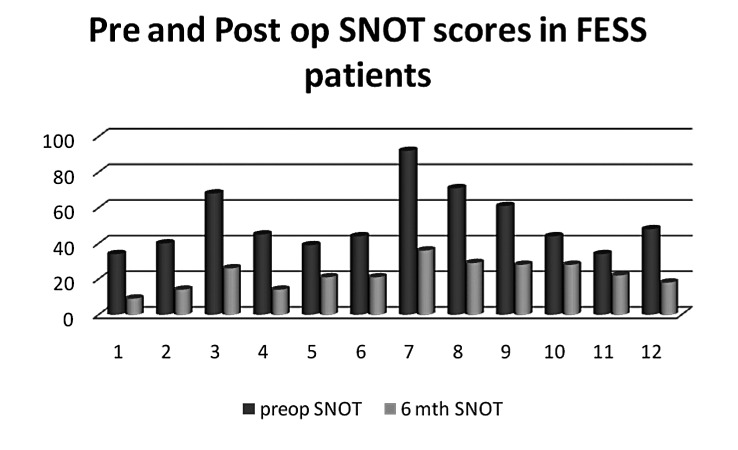
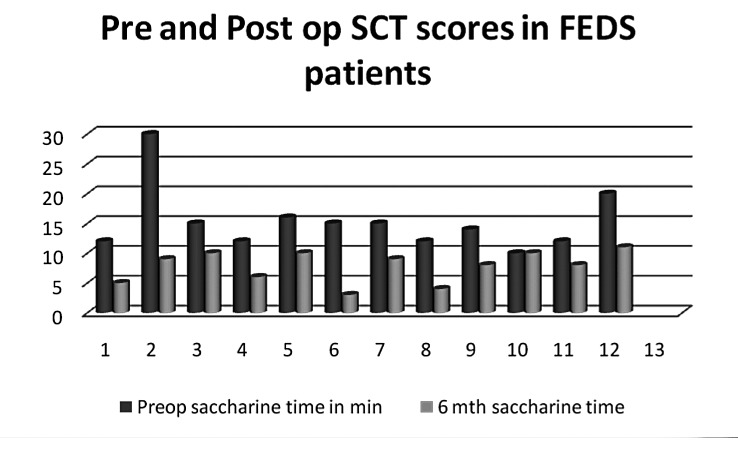
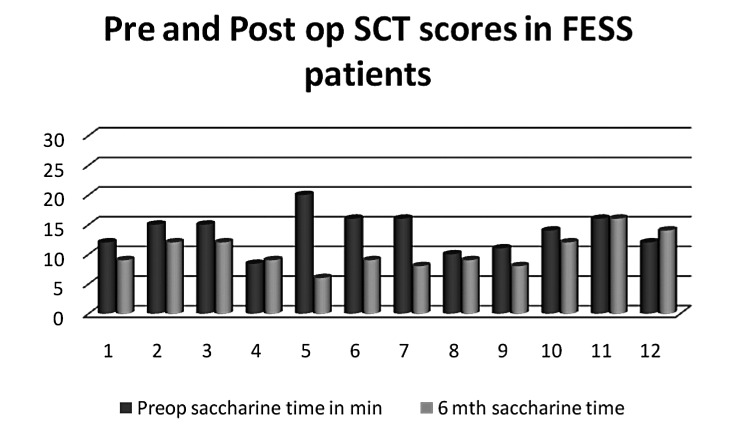
The mean postoperative recovery period (time required to get back to routine activities) in the FEDS group was 2.2 days, and in the FESS group was 5 days. The mean difference in SNOT-20 score in the FEDS group (Fig. 1) was 43.83, with a standard deviation of 15.17 and standard error of 4.38. The mean difference in SNOT-20 score in the FESS group (Fig. 2) was 29.66 with a standard deviation of 12.33 and standard error of 3.56. We used a Mann Whitney test to compare the two groups, (p = 0.026), which suggested better improvement in SNOT-20 scores in the FEDS group. The FEDS group (Fig. 3) had a mean difference in SCT of 7.5 (SD = 5.13, SE = 1.48), while the FESS group (Fig. 4) showed a mean difference in SCT of 3.5 (SD = 4.34, SE = 1.25). The mean difference in saccharine clearance time between the two groups was significant (p=0.03), suggesting better improvement in SCT with FEDS than FESS. However, this was a noninferiority trial. The p value comparing both SNOT-20 and SCT in two groups was significant, thus showing that FEDS is equivalent to FESS in subjective improvement of symptoms.
Fig. 1.
SNOT-20 scores pre-operatively and at 6 months post-operatively in the FEDS group of patients.
Fig. 2.
SNOT-20 scores pre-operatively and at 6 months post-operatively in the FESS group of patients.
Fig. 3.
Saccharine clearance time in minutes; pre-operative and 6 months post operative in the FEDS group.
Fig. 4.
Saccharine clearance time in minutes; pre-operative and 6 months post operative in the FESS group.
Discussion
The tissue preservation technique used by balloon sinuplasty offers sinus ostial dilatation with the added advantage of avoiding destructive procedures for access like septoplasty and medialisation of middle turbinate. This technique was first assessed in cadavers in achieving patent sinus ostia and published in 2006 3. Since then, there have been many other series including multi-centre studies showing similar safety and effectiveness in live patients 4 6 including children 7. Our pilot study is the first randomized controlled trial comparing the safety and effectiveness of the technique compared to classic FESS. This was a non-inferiority trial, and our aim was solely to recognize this additional tool in sinus surgery.
The role of surgery in management of chronic rhinosinusitis is limited. There have been many studies examining the correlation between nitric oxide levels within the nose/sinuses and various sinus pathologies. The role of lower nitric oxide levels within the sinus in sinonasal disease is being increasingly appreciated 8 9. A recent systematic review 10 shows some evidence that sinus surgery lowers levels of nasal nitric oxide. Preservation of the uncinate process in balloon sinuplasty may be helpful in maintaining nitric oxide levels within the sinus, and maintaining the physiology of the sinuses. This is an area that needs further study.
In our patients, we did not treat the ethmoid group of sinuses in the FEDS group of patients. Ethmoid air cells provide multiple and having variable openings to these sinuses, and it is difficult to perform balloon sinuplasty for these sinuses. Spontaneous resolution of ethmoid sinus disease following clearance of adjoining (maxillary and frontal) sinus disease has been hypothesized. Kutluhan A et al. 6 described their technique of ethmoid sinus dilatation, mainly by perforating the bulla for the anterior ethmoid cells and the basal lamella for the posterior group of ethmoid cells. This technique, however, contradicts the principle of tissue preservation in balloon sinuplasty, since it involves removal of part of the antero-inferior wall of bulla and basal lamella to enter the ethmoidal air cells instead of dilatation of the normal sinus ostia.
FESS is now a well established procedure, and a success rate of 80-90% has been reported for FESS in treatment of chronic rhinosinusitis 11 12 in studies following patients for an average of 18 months. Levine et al 13 reported a success rate of over 95% in patients undergoing dilatation sinus surgery when followed up at 18 months with 1.3% needing revision surgery, while Kutluhan et al. 6 reported the need for revision in 6.7% of their cases. Over the last couple of decades, the morbidity of FESS has decreased significantly, with major complications like CSF leak, orbital complications and major bleeding being less than 1%. Although there are not many complications reported for balloon sinuplasty, Tomazic et al. 14 recently reported a case of ethmoid roof CSF leak and small iatrogenic encephalocoele 3 weeks post-balloon dilation of frontal sinus, which needed repair with endoscopic duraplasty.
Use of a c-arm for fluoroscopic guidance of catheter position is now being replaced by use of the Translumina system, eliminating the risk of radiation exposure. In our study, we initiated the trial using fluoroscopic guidance, and all 12 patients underwent FEDS with the use of a c-arm; our longest fluoroscopy time was 53 seconds in one patient and least was 16 seconds. The total fluoroscopy time per procedure showed a decreasing trend with increasing surgeon experience. A study on radiation exposure to surgeons performing balloon sinuplasty under fluoroscopic guidance showed the average radiation dose to be within the recommended annual maximum for occupational radiation exposure 15.
In our study, we also used SCT as one of our outcome measures. This test is a semi-objective measure to determine the function of the mucociliary component of the sino-nasal tract. An improvement in the SCT seen in both group of patients signifies the return of physiological functioning of the ciliary movement, and thus good movement of sino-nasal mucosal secretions. This further demonstrates the efficacy of balloon sinuplasty as noninferior to FESS in treatment of rhinosinusitis.
This was a descriptive, pilot study and not adequately powered. A power calculation suggested the requirement of at least 30 participants in each group, based on minimal clinically important difference of 16 (0.8 on a 0-5 scale) and standard deviation of change in SNOT-20 scores of 22(1.1) at 6 months. Due to funding restrictions and other technical difficulties, we could not proceed with further recruitment for the study. Our preliminary results can be used for as a prelude for a larger randomised controlled trial with adequate power calculation.
This study was open to both patients and investigators. Hence, there can be an element of bias in reporting of symptoms, more so with the use of a subjective outcome measure like SNOT 20. We did not include patients with severe polyposis, cystic fibrosis or history of nasal trauma or previous sino-nasal surgery. These patients certainly have benefits with endoscopic sinus surgery, and the role of sinus ostial dilatation alone in such complex cases is limited. Two of our FEDS patients underwent hybrid treatment, which could bias the result in view of a very small patient group. Follow-up was only for 6 months, and we cannot comment on the long-term benefits of surgery in these patients.
The role of FEDS in simple chronic rhinosinusitis can be likened to the effect achieved with FESS. However, careful selection of patients is important in order to avoid overt misuse of this expensive tool. Apart from chronic rhinosinusitis, FEDS may also be of benefit as an outpatient or day procedure in treatment of acute sinusitis, helping physiological drainage of the sinus along with good irrigation of the sinus similar to the type of antral washouts that used to be done in a non-physiological manner in the past.
Conclusions
Our preliminary results suggest that functional endoscopic dilatation sinus surgery is as effective as functional endoscopic sinus surgery in the treatment of chronic rhinosinusitis, and that it is a useful addition to the armamentarium of tools for endoscopic sinus surgery. The added advantage for FEDS is the potential for day surgery and earlier return to normal activities. The authors propose further studies with a larger randomized controlled trial, with adequate power, longer follow-up and use of less strict inclusion and exclusion criteria. Evidence from long-term follow-up (18 to 24 months) of these patients in the literature substantiates the safety and feasibility of this tool 13 16. The role of preservation of the uncinate process in balloon sinuplasty in maintenance of sinus nitric oxide levels is an area for further research.
References
- 1.Fokkens W, Lund V, Mullol J, et al. European Position Paper on Nasal Polyps. Rhinology. 2007;45(suppl. 20):1–139. [PubMed] [Google Scholar]
- 2.Benninger MS, Ferguson BJ, Hadley JA, et al. Adult chronic rhinosinusitis: definitions, diagnosis, epidemiology, and pathophysiology. Otolaryngol Head Neck Surg. 2003;129:S1–S32. doi: 10.1016/s0194-5998(03)01397-4. [DOI] [PubMed] [Google Scholar]
- 3.Bolger WE, Vaughan WC. Catheter-based dilation of the sinus ostia: initial safety and feasibiliiy analysis in a cadaver mode. Am J Rhinol. 2006;20:290–294. doi: 10.2500/ajr.2006.20.2868. [DOI] [PubMed] [Google Scholar]
- 4.Bolger WE, Brown CL, Church CA, et al. Safety and outcomes of balloon catheter sinusotomy: a Multicenter 24-week analysis in 115 patients. Otolaryngol Head Neck Surg. 2007;137:10–20. doi: 10.1016/j.otohns.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 5.Brown CL, Bolger WE. Safety and feasibility of balloon catheter dilation of paranasal sinus ostia: a preliminary investigation. Ann Otol Rhinol Laryngol. 2006;115:293–301. doi: 10.1177/000348940611500407. [DOI] [PubMed] [Google Scholar]
- 6.Kutluhan A, Bozdemir K, Çetin H, et al. Endoscopic balloon dilation sinuplasty including ethmoidal air cells in chronic rhinosinusitis. Ann Otol Rhinol Laryngol. 2009;118:881–886. doi: 10.1177/000348940911801209. [DOI] [PubMed] [Google Scholar]
- 7.Ramadan HH. Safety and feasibility of Balloon sinuplasty for treatment of chronic rhinosinusitis in children. Ann Otol Rhinol Laryngol. 2009;118:161–165. doi: 10.1177/000348940911800301. [DOI] [PubMed] [Google Scholar]
- 8.Bommarito L, Guida G, Heffler G, et al. Nasal nitric oxide concentration in suspected chronic rhinosinusitis. Ann Allergy Asthma Immunol. 2008;101:358–362. doi: 10.1016/S1081-1206(10)60310-9. [DOI] [PubMed] [Google Scholar]
- 9.Kirihene RK, Rees G, Wormald P-J, et al. The influence of the size of the maxillary sinus ostium on the nasal and sinus nitric oxide levels. Am J Rhinol. 2002;16:261–264. [PubMed] [Google Scholar]
- 10.Phillips PS, Sacks R, Marcells GN, et al. Nasal nitric oxide and sinonasal disease: a systematic review of published evidence. Otolaryngol Head Neck Surg. 2011;144:159–169. doi: 10.1177/0194599810392667. [DOI] [PubMed] [Google Scholar]
- 11.Levine HL. Functional endoscopic sinus surgery: evaluation, surgery, and follow-up of 250 patients. Laryngoscope. 1990;100:79–84. doi: 10.1288/00005537-199001000-00016. [DOI] [PubMed] [Google Scholar]
- 12.Matthews BL, Smith LE, Jones R, et al. Endoscopic sinus surgery: outcome in 155 cases. Otolaryngol Head Neck Surg. 1991;104:244–246. doi: 10.1177/019459989110400214. [DOI] [PubMed] [Google Scholar]
- 13.Levine HL, Sertich AP, Hoisington DR, et al. PatiENT Registry Study Group. Multicenter registry of balloon catheter sinusotomy outcomes for 1036 patients. Ann Otol Rhinol Laryngol. 2008;117:263–270. doi: 10.1177/000348940811700405. [DOI] [PubMed] [Google Scholar]
- 14.Tomazic PV, Stammberger H, Koele W, et al. Ethmoid roof CSF-leak following frontal sinus balloon sinuplasty. Rhinology. 2010;48:247–250. doi: 10.4193/Rhin09.129. [DOI] [PubMed] [Google Scholar]
- 15.Albritton FD, Levine HL, Smith JL, et al. Surgeon radiation exposure in ESS with balloon catheters. Otolaryngol Head Neck Surgery. 2009;140:834–840. doi: 10.1016/j.otohns.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 16.Levine H, Rabago D. Balloon sinuplasty: a minimally invasive option for patients with chronic rhinosinusitis. Postgrad Med. 2011;123:112–118. doi: 10.3810/pgm.2011.03.2269. [DOI] [PubMed] [Google Scholar]