Abstract
Aim of the study: To investigate the comorbidity of Alzheimer’s/dementia, epilepsy, multiple sclerosis and Parkinson’s with depression.
Methods: 42,914 patients who were newly diagnosed with the four comorbid diseases were included in the study. We analyzed how many of these patients developed depression within five years.
Results: Between 21% (males with epilepsy) and 39% (women with Parkinson’s)/44% (Alzheimer’s patients under 60 years) developed depression within five years.
Conclusion: We recommend routine checks for depression in patients diagnosed with one of these diseases, especially in the most comorbid ones.
Keywords: comorbidity, depression, dementia, epilepsy, multiple sclerosis, Parkinson’s
Abstract
Zweck der Untersuchung: Ermittlung der Häufigkeit des Auftretens von Depressionen im Gefolge von neurologischen Erkrankungen (M. Alzheimer, Demenz, Epilepsie, multiple Sklerose, M. Parkinson).
Methodik: Wir beobachteten den Krankheitsverlauf von 42.914 Patienten, bei denen die genannten neurologischen Erkrankungen erstmals auftraten, über fünf Jahre, im Hinblick auf das Auftreten einer Depression.
Ergebnisse: Bei 21% (männliche Patienten mit Epilepsie) bis 39% (weibliche Parkinson-Patientinnen) bzw. 44% (beide Geschlechter, Patienten unter 60 Jahren mit Alzheimer-Diagnose) der Patientinnen und Patienten wurde innerhalb von fünf Jahren zusätzlich eine Depression diagnostiziert.
Schlussfolgerung: Wir empfehlen, alle Patientinnen und Patienten mit einer der genannten Erkrankungen, v. a. den besonders komorbiden, auf Depression zu untersuchen.
Introduction
Depression is among the most common diseases. Although it is the third most common today, experts predict it will be the second most common in 2020 [2]. Current lifetime prevalence is about 16–26%, with a 2:1 ratio between females and males [30]. One-year prevalences for major depression have been estimated at 6.4% in the US [22], 5.8% in Europe [6], and 8.3% in Germany [39].
Literature typically finds increasing prevalence over time, i.e. persons born later face a higher risk of suffering from depression, at the same age, than persons born earlier [32], although this has been debated [38]. It is also unclear whether age in itself increases the risk of depression [37].
Many psychic and somatic diseases have been found to be associated with depression – e.g., anxiety [33], cardiovascular diseases [3], dementia [14], Parkinson’s disease [8], stroke [20], and combinations of diseases such as Parkinson’s and dementia [28]. For many other diseases it is assumed that there is a correlation with depression, e.g., diabetes, cancer, and others; in most cases, the etiology of comorbidity is not yet known [24].
Literature findings are difficult to compare across comorbid diseases, as most studies analyze the comorbidity of depression with only one other disease. Furthermore, the study design, inclusion criteria and other influencing factors are different from study to study. In addition, studies are typically based on comorbidities at a certain point in time. Thus, we studied this risk for approximately 40,000 patients with four different neurological diseases over five years.
Methods
Database
This study is based on data from the IMS Disease Analyzer database.
This database collates drug prescriptions, diagnoses, and basic medical and demographic data directly obtained from the practice computer systems of general practitioners and specialists throughout Germany [23]. Diagnoses (ICD-10), prescriptions (Anatomical Therapeutic Chemical [ATC] Classification System) and the quality of reported data are continuously monitored by IMS based on a number of quality criteria (e.g. completeness of documentation, linkage of diagnoses and prescriptions). The data are generated directly from the computers in the physicians’ practices via standardized interfaces and provide daily routine information on patients’ diseases and therapies. A practice transmits patient data stored in the physician’s computer to IMS on a monthly basis. Before transmission, the data are encrypted for data protection and contain in similar scope and detail the information in the files of patients in the doctor’s practice. In total, the database contains data from around 3,000 practices and approximately 20 million patients in Germany in the last 10 years. The validity of Disease Analyzer data was researched and described [4].
Study population
Overall, the data used for this study included 1,109 GPs in 882 general practices continuously reporting to IMS HEALTH during the study period between January 2000 and April 2012. Firstly, all subjects initially diagnosed with Alzheimer’s/dementia (ICD codes G30, F01, and F03), epilepsy (G40), multiple sclerosis (ICD code G35) or Parkinson’s (G20, G21) between January 2002 and December 2006 (index date) were identified. We included patients only if:
(1) they had seen the same physician at least once yearly two years before and more than five years after the index date, (2) they did not suffer from any of these diseases nor depression before the index date and (3) they did not suffer from cancer throughout the observation period.
A total of 13,652 patients with Alzheimer’s disease or dementia, 15,722 with epilepsy, 5,137 with multiple sclerosis and 8,403 with Parkinson’s disease were available for analysis. For comparison purposes, we also investigated the percentage of all patients in our database who developed depression and met criteria (1) to (3), not only those with Alzheimer’s/dementia, epilepsy, etc.
Study outcome
The main outcome measure was the first diagnosis of depression (ICD 10: F32, F33) within five years after the index date. Moreover, the differences between the incidence of depression in male and female patients and in patients younger and older than 60 years were investigated.
Statistical analysis
The analyses were conducted using SAS version 9.2 (SAS Institute, Cary, NC, USA). For age, the mean value and standard deviation were calculated. The incidence of depression with 95% confidence intervals was estimated.
Results
Study population
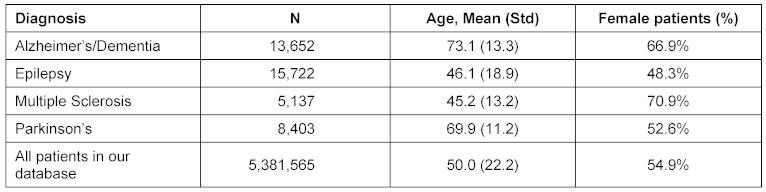
42,914 patients were included in the study. The mean age of patients at the time of inclusion was between 45 years for multiple sclerosis and 73 years for Alzheimer’s/dementia, at the index date. For multiple sclerosis and Alzheimer’s/dementia, women represented 71% and 67% of patients, respectively (see Table 1 (Tab. 1) for details).
Table 1. Age and sex of study patients.
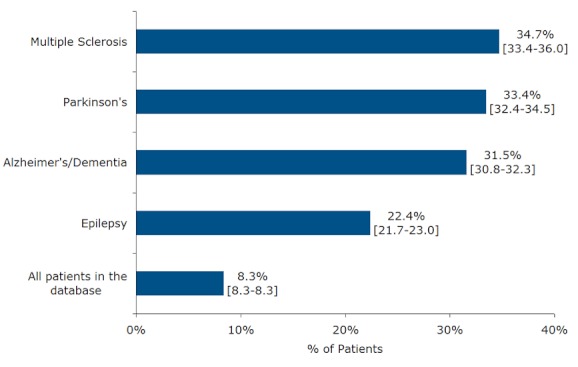
All the diseases studied increased the risk of developing depression after the index date. The risk ranged from 22% for epilepsy to 35% for multiple sclerosis (see Figure 1 (Fig. 1)). Alzheimer’s/dementia, multiple sclerosis, and Parkinson’s are more risky than epilepsy in terms of the likelihood of the development of depression. Only 8% of all the patients in the database developed depression.
Figure 1. Proportion of patients with first depression diagnosis within 5 years after index date.
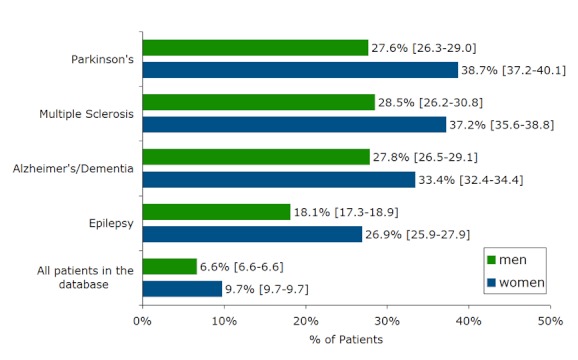
In all the diseases studied, women were more likely to develop depression (Figure 2 (Fig. 2)); their risk ranged from 27% for epilepsy to 39% for Parkinson’s patients.
Figure 2. Proportion of patients with first depression diagnosis withing 5 years after index date, for female and male patients.
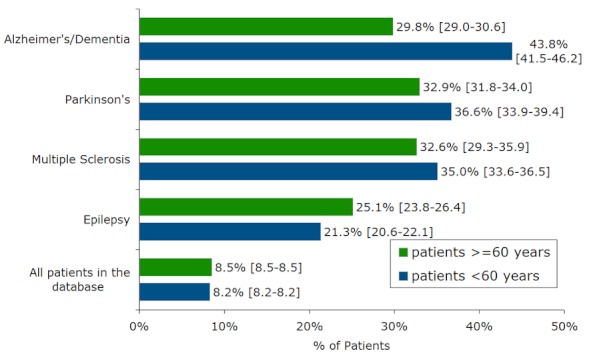
In terms of Alzheimer’s/dementia only, patients under 60 years had a higher risk of developing depression. For the other diseases, and in the total database population, the risks were about the same below and above 60 years (Figure 3 (Fig. 3)).
Figure 3. Proportion of patients with first depression diagnosis within 5 years after index date, in patients <60 and ≥60 years.
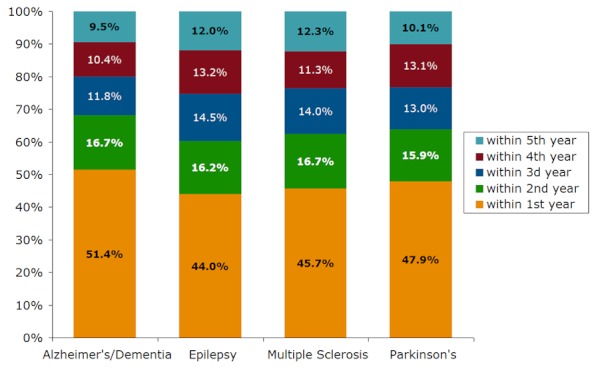
We also studied the timeframe for the onset of depression. In all diseases, about half of the patients developed depression in the first year after the index date; the other half did in the years two to five (Figure 4 (Fig. 4)).
Figure 4. Proportion of depression patients with first depression diagnosis within 1st, 2nd, 3rd, 4th and 5th year after index date.
Finally, we studied how many depression patients received antidepressant medication. The percentages were 56.6% for epilepsy patients, 63.9% for Alzheimer’s/dementia, 66.8% for Parkinson’s, and 67.0% for multiple sclerosis.
Discussion
Overall, 8.3% of all the patients in our database who met inclusion criteria (1) to (3) were diagnosed with depression in the five-year period after the index date. This is in line with earlier findings on incidence: current lifetime prevalence is about 16–26% [30]; one-year prevalences for major depression have been estimated at 6.4% in the US [22], 5.8% in Europe [6], and 8.3% in Germany [39]. Compared to the latter figure, our five-year prevalence is at the lower end of what was expected. There are several reasons that could be responsible for this finding:
Firstly, we excluded patients with cancer from the study group, thus patients who developed depression because of a malign disease are not included in our 8.3%. Secondly, there is a debate about the question of whether ambulatory care physicians tend to underdiagnose and undertreat patients with depression [12], [25], [36], [40]. Thus it could be that some patients in our study population did suffer from depression but weren’t diagnosed as such. On the other hand, our population is based on patients who visited a doctor; there might be a difference in prevalence in our population as compared to the total population. Finally, we used the ICD code to identify patients with depression, and not other criteria like specific tests for depression. Therefore, our study uses the same methodology to detect depression as for all predecessor diseases, thus it allows us to estimate their relative risk. This would not be the case if different techniques for diagnosing depression were used.
At first glance the number of depression patients treated with antidepressant medication, which ranges from 57% to 67%, seems rather low, but is in line with the literature [36], [39], [40].
The most striking result of our study is the high risk of developing depression as a consequence of other neurological diseases. Between 21% (males with epilepsy) and 39% (women with Parkinson’s)/44% (Alzheimer’s patients under 60 years) developed depression within five years.
For Alzheimer’s/dementia, about 30% of our population developed depression; more specifically, younger patients had the highest risk of all our subpopulations. It is well known that Alzheimer’s/dementia is comorbid with depression. This relationship works in both directions. Thus, depression also increases the risk of developing dementia around more than twofold, although the amount of relative risk is debated [7], [21]. In terms of Alzheimer’s/dementia patients, the comorbidity of depression is estimated at 16–87%, measured on different scales [11], [35] again with the amount of comorbidity debated [19]. Although there have been different mechanisms proposed that could explain comorbidity, such as psychological factors – for instance, a patient noticing that he/she is developing dementia might become depressive – or biological explanations – “vascular depression” – the reason for comorbidity is not well understood [9]. Our finding that most instances of depression are diagnosed in the year after Alzheimer’s/dementia is in line with the literature [26]. Finally, we cannot exclude the fact that patients who suffer from Alzheimer’s/dementia will be treated by specialized physicians who may be more likely to diagnose depression; but we do not have any specific data on this.
This scenario of comorbidity in itself being well known, but that the instances and underlying reasons are not well understood, holds true for the other diseases studied here.
About 22% of our epilepsy patients developed depression within five years. This is still a significant number, but is much lower than for the three other diseases studied here. It is well known that epilepsy is comorbid with depression, as well as the fact that several antiepileptics can cause depression (e.g., hydantoins, succinimides, clonazepam, phenytoin) [16], [29]. Some antiepileptics, on the other hand, can support antidepressant treatment (“mood stabilizers”, e.g., carbamazepine, valproate, lamotrigine) [31].
It is not known exactly how epilepsy and depression influence each other. Common pathogenetic mechanisms are discussed [17], [18].
In our patients with multiple sclerosis, 35% developed depression. Earlier estimates found a risk of up to 50–56%; and that the risk was higher in younger, single, better educated, and unemployed patients [1], [10]. It is not yet clear whether the depression is pathophysiological or reactive in nature [13], [34].
33% of our Parkinson’s patients developed depression. This is in line with the 25–72% range found in the literature [8], [15], [27]. Several Parkinson’s drugs are suspected to cause depression: L-dopa, amantadine, Baclofen, and bromocriptine [29]. However, other authors find that some of them may also augment antidepressants [5].
Again, several mechanisms of comorbidity are discussed but not yet fully understood [8].
There are some limitations in our findings which need to be discussed. Firstly, we have studied patients in an out-patient setting only; we did not have access to hospital data for these patients. Secondly, we had to rely on the validity of diagnoses as coded by physicians; thus we did not have any data on depression-specific tests (nor on the tests specific for the other diseases). Finally, we could not control for potential distortions due to the diagnosis process; e.g., it might have been that patients with neurological symptoms were seen by a specialist who put more emphasis on diagnosing depressive disorders.
To the best of our knowledge, this is the first time that for a sample of approximately 40,000 patients, the longitudinal risk of developing depression in patients with neurological diseases has been estimated. In addition, it is the first time that the same estimation method has been used for all these diseases, thereby allowing for comparison of their relative risks in terms of developing depression. Based on our results, we conclude that Alzheimer’s/dementia, epilepsy, multiple sclerosis and Parkinson’s disease patients should be monitored routinely for depression, with a specific emphasis to the highest-risk groups (females diagnosed with multiple sclerosis, younger patients confronted with dementia).
Notes
Contributorship statement
All persons designated as authors qualify for authorship, and all those who qualify are listed.
All authors contributed 1) substantially to conception and design of the paper, acquisition of data, and analysis and interpretation of data; 2) to drafting the article and revising it critically for important intellectual content; and 3) to final approval of the version to be published.
Each author participated sufficiently in the work to take public responsibility for appropriate portions of the content.
In terms of planning, K. Kostev and C. Thielscher took the lead; in conduct, C. and S. Thielscher focused on the medical part of the paper as well as the literature review, whereas K. Kostev focused on the data extraction. In the discussion, all authors contributed.
C. Thielscher is the sole guarantor and takes responsibility for the overall content.
Acknowledgements
The authors would like to thank Ms. Elaine Last, manager, editorial publications, IMS Health, Cambridge, UK, for proofreading and editing the paper.
Funding statement
We did not receive funding for our study.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Alajbegovic A, Loga N, Tiro N, Alajbegovic S, Todorovic L, Jasminika-Djelilovic Depression in multiple sclerosis patients. Med Arh. 2011;65(2):115–118. [PubMed] [Google Scholar]
- 2.Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. 2004 Nov-Dec;66(6):802–813. doi: 10.1097/01.psy.0000146332.53619.b2. Available from: http://dx.doi.org/10.1097/01.psy.0000146332.53619.b2. [DOI] [PubMed] [Google Scholar]
- 3.Barth S. Major Depression, somatische Komorbidität und psychosoziales Wohlbefinden im mittleren und höheren Lebensalter: Ergebnisse der Interdisziplinären Längsschnittstudie des Erwachsenenalters [Dissertation] Heidelberg: Ruprecht-Karls-Universität; 2004. p. 12. Available from: http://archiv.ub.uni-heidelberg.de/volltextserver/5195/ [Google Scholar]
- 4.Becher H, Kostev K, Schröder-Bernhardi D. Validity and representativeness of the "Disease Analyzer" patient database for use in pharmacoepidemiological and pharmacoeconomic studies. Int J Clin Pharmacol Ther. 2009 Oct;47(10):617–626. doi: 10.5414/cpp47617. [DOI] [PubMed] [Google Scholar]
- 5.Benkert O, Hippius H. Kompendium der psychiatrischen Pharmakotherapie. Heidelberg: Springer; 2011. pp. 74–75. Available from: http://dx.doi.org/10.1007/978-3-642-13044-1. [DOI] [Google Scholar]
- 6.Bijl RV, Ravelli A, van Zessen G. Prevalence of psychiatric disorder in the general population: results of The Netherlands Mental Health Survey and Incidence Study (NEMESIS) Soc Psychiatry Psychiatr Epidemiol. 1998 Dec;33(12):587–595. doi: 10.1007/s001270050098. Available from: http://dx.doi.org/10.1007/s001270050098. [DOI] [PubMed] [Google Scholar]
- 7.Byers AL, Yaffe K. Depression and risk of developing dementia. Nat Rev Neurol. 2011 May 3;7(6):323–331. doi: 10.1038/nrneurol.2011.60. Available from: http://dx.doi.org/10.1038/nrneurol.2011.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dissanayaka NN, Sellbach A, Silburn PA, O'Sullivan JD, Marsh R, Mellick GD. Factors associated with depression in Parkinson's disease. J Affect Disord. 2011 Jul;132(1-2):82–88. doi: 10.1016/j.jad.2011.01.021. Available from: http://dx.doi.org/10.1016/j.jad.2011.01.021. [DOI] [PubMed] [Google Scholar]
- 9.Enache D, Winblad B, Aarsland D. Depression in dementia: epidemiology, mechanisms, and treatment. Curr Opin Psychiatry. 2011 Nov;24(6):461–472. doi: 10.1097/YCO.0b013e32834bb9d4. [DOI] [PubMed] [Google Scholar]
- 10.Feinstein A. Multiple sclerosis and depression. Mult Scler. 2011 Nov;17(11):1276–1281. doi: 10.1177/1352458511417835. Available from: http://dx.doi.org/10.1177/1352458511417835. [DOI] [PubMed] [Google Scholar]
- 11.Fritze F, Ehrt U, Sønnesyn H, Kurz M, Hortobágyi T, Nore SP, Ballard C, Aarsland D. Depression in mild dementia: associations with diagnosis, APOE genotype and clinical features. Int J Geriatr Psychiatry. 2011 Oct;26(10):1054–1061. doi: 10.1002/gps.2643. Available from: http://dx.doi.org/10.1002/gps.2643. [DOI] [PubMed] [Google Scholar]
- 12.Hensler S, Wiesemann A. Diskreditierende Versorgungsstudien in deutschen Hausarztpraxen. Z Allg Med. 2003;79:579–585. [Google Scholar]
- 13.Holden K, Isaac CL. Depression in multiple sclerosis: reactive or endogenous? Clin Neuropsychol. 2011 May;25(4):624–639. doi: 10.1080/13854046.2011.564208. Available from: http://dx.doi.org/10.1080/13854046.2011.564208. [DOI] [PubMed] [Google Scholar]
- 14.Hummel J, Weisbrod C, Bösch L, Himpler K, Böhm G, Diener S, Gaebel A, Dipper L, Zieschang T, Oster P, Kopf D. Komorbidität von Depression und Demenz bei geriatrischen Patienten mit akuter körperlicher Erkrankung: AIDE-cog-Studie. [Acute illness and depression in the elderly and the influence of cognitive impairment: AIDE-cog trial]. Z Gerontol Geriatr. 2012 Jan;45(1):34–39. doi: 10.1007/s00391-011-0271-5. (Ger). Available from: http://dx.doi.org/10.1007/s00391-011-0271-5. [DOI] [PubMed] [Google Scholar]
- 15.Jasinska-Myga B, Putzke JD, Wider C, Wszolek ZK, Uitti RJ. Depression in Parkinson's disease. Can J Neurol Sci. 2010 Jan;37(1):61–66. doi: 10.1017/s0317167100009665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kanner AM. Depression and epilepsy: a review of multiple facets of their close relation. Neurol Clin. 2009 Nov;27(4):865–880. doi: 10.1016/j.ncl.2009.08.002. Available from: http://dx.doi.org/10.1016/j.ncl.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 17.Kanner AM. Depression in epilepsy: a complex relation with unexpected consequences. Curr Opin Neurol. 2008 Apr;21(2):190–194. doi: 10.1097/WCO.0b013e3282f4e978. Available from: http://dx.doi.org/10.1097/WCO.0b013e3282f4e978. [DOI] [PubMed] [Google Scholar]
- 18.Kanner AM, Schachter SC, Barry JJ, Hersdorffer DC, Mula M, Trimble M, Hermann B, Ettinger AE, Dunn D, Caplan R, Ryvlin P, Gilliam F. Depression and epilepsy: epidemiologic and neurobiologic perspectives that may explain their high comorbid occurrence. Epilepsy Behav. 2012 Jun;24(2):156–168. doi: 10.1016/j.yebeh.2012.01.007. Available from: http://dx.doi.org/10.1016/j.yebeh.2012.01.007. [DOI] [PubMed] [Google Scholar]
- 19.Korczyn AD, Halperin I. Depression and dementia. J Neurol Sci. 2009 Aug 15;283(1-2):139–142. doi: 10.1016/j.jns.2009.02.346. Available from: http://dx.doi.org/10.1016/j.jns.2009.02.346. [DOI] [PubMed] [Google Scholar]
- 20.Kouwenhoven SE, Kirkevold M, Engedal K, Kim HS. Depression in acute stroke: prevalence, dominant symptoms and associated factors. A systematic literature review. Disabil Rehabil. 2011;33(7):539–556. doi: 10.3109/09638288.2010.505997. Available from: http://dx.doi.org/10.3109/09638288.2010.505997. [DOI] [PubMed] [Google Scholar]
- 21.Li G, Wang LY, Shofer JB, Thompson ML, Peskind ER, McCormick W, Bowen JD, Crane PK, Larson EB. Temporal relationship between depression and dementia: findings from a large community-based 15-year follow-up study. Arch Gen Psychiatry. 2011 Sep;68(9):970–977. doi: 10.1001/archgenpsychiatry.2011.86. Available from: http://dx.doi.org/10.1001/archgenpsychiatry.2011.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Narrow WE, Rae DS, Robins LN, Regier DA. Revised prevalence estimates of mental disorders in the United States: using a clinical significance criterion to reconcile 2 surveys' estimates. Arch Gen Psychiatry. 2002 Feb;59(2):115–123. doi: 10.1001/archpsyc.59.2.115. Available from: http://dx.doi.org/10.1001/archpsyc.59.2.115. [DOI] [PubMed] [Google Scholar]
- 23.Ogdie A, Langan SM, Parkinson J, et al. Medical Record Databases. In: Strom BL, Kimmel S, Hennessy S, editors. Pharmacoepidemiology. 5th ed. Philadelphia, PA: University of Pennsylvania; 2012. [Google Scholar]
- 24.Pieper L, Schulz H, Klotsche J, Eichler T, Wittchen HU. Depression als komorbide Störung in der primärärztlichen Versorgung. [Depression as a comorbid disorder in primary care]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2008 Apr;51(4):411–421. doi: 10.1007/s00103-008-0509-6.. (Ger). Available from: http://dx.doi.org/10.1007/s00103-008-0509-6. [DOI] [PubMed] [Google Scholar]
- 25.Pilars de Pilar M, Abholz HH, Becker N, Sielk M. Was erzählen Hausärzte über ihre Patienten, bei denen sie eine vorliegende Depression nicht diagnostiziert haben? [How do general practitioners deal with patients they do not consider to be depressed but who are classified as such according the PHQ-9?]. Psychiatr Prax. 2012 Mar;39(2):71–78. doi: 10.1055/s-0031-1276897.. (Ger). Available from: http://dx.doi.org/10.1055/s-0031-1276897. [DOI] [PubMed] [Google Scholar]
- 26.Preuss UW, Siafarikas N, Petrucci M, Wong WM. Depressive Störungen bei Demenzen und milder kognitiver Beeinträchtigung: Komorbidität, Ursache oder Risikofaktor? [Depressive disorders in dementia and mild cognitive impairments: is comorbidity a cause or a risk factor?]. Fortschr Neurol Psychiatr. 2009 Jul;77(7):399–406. doi: 10.1055/s-0028-1109454. (Ger). Available from: http://dx.doi.org/10.1055/s-0028-1109454. [DOI] [PubMed] [Google Scholar]
- 27.Riedel O, Heuser I, Klotsche J, Dodel R, Wittchen HU GEPAD Study Group. Occurrence risk and structure of depression in Parkinson disease with and without dementia: results from the GEPAD Study. J Geriatr Psychiatry Neurol. 2010 Mar;23(1):27–34. doi: 10.1177/0891988709351833. Available from: http://dx.doi.org/10.1177/0891988709351833. [DOI] [PubMed] [Google Scholar]
- 28.Riedel O, Klotsche J, Spottke A, Deuschl G, Förstl H, Henn F, Heuser I, Oertel W, Reichmann H, Riederer P, Trenkwalder C, Dodel R, Wittchen HU. Frequency of dementia, depression, and other neuropsychiatric symptoms in 1,449 outpatients with Parkinson's disease. J Neurol. 2010 Jul;257(7):1073–1082. doi: 10.1007/s00415-010-5465-z. Available from: http://dx.doi.org/10.1007/s00415-010-5465-z. [DOI] [PubMed] [Google Scholar]
- 29.Schmauß M, Messer, T . Therapieresistenz in der Behandlung unipolarer Depressionen. In: Schmauß T, Messer M, editors. Therapieresistenz bei psychischen Erkrankungen. München: Elsevier, Urban & Fischer; 2009. p. 4. [Google Scholar]
- 30.Schmauß M, Schramm E, Berger M. Unipolare Depression – Pharmakotherapie und Psychotherapie (ICD-10: F3) In: Voderholzer U, Hohagen, F, editors. Therapie psychischer Erkrankungen. München: Elsevier, Urban & Fischer; 2012. p. 132. [Google Scholar]
- 31.Schramm E, et al. Chronische und therapieresistente Depressionen. In: Voderholzer U, Hohagen F, editors. Therapie psychischer Erkrankungen. München: Elsevier GmbH; 2012. p. 183. [Google Scholar]
- 32.Simon GE, VonKorff M, Ustun TB, Gater R, Gureje O, Sartorius N. Is the lifetime risk of depression actually increasing? J Clin Epidemiol. 1995 Sep;48(9):1109–1118. doi: 10.1016/0895-4356(95)00010-2. Available from: http://dx.doi.org/10.1016/0895-4356(95)00010-2. [DOI] [PubMed] [Google Scholar]
- 33.Üstün TB, Sartorius N, editors. Mental illness in general health care. Chichester: John Wiley & Sons; 1995. [Google Scholar]
- 34.Vattakatuchery JJ, Rickards H, Cavanna AE. Pathogenic mechanisms of depression in multiple sclerosis. J Neuropsychiatry Clin Neurosci. 2011 Summer;23(3):261–276. doi: 10.1176/appi.neuropsych.23.3.261. Available from: http://dx.doi.org/10.1176/appi.neuropsych.23.3.261. [DOI] [PubMed] [Google Scholar]
- 35.Winter Y, Korchounov A, Zhukova TV, Bertschi NE. Depression in elderly patients with Alzheimer dementia or vascular dementia and its influence on their quality of life. J Neurosci Rural Pract. 2011 Jan;2(1):27–32. doi: 10.4103/0976-3147.80087. Available from: http://dx.doi.org/10.4103/0976-3147.80087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wittchen HU, Höfler M, Meister W. Prevalence and recognition of depressive syndromes in German primary care settings: poorly recognized and treated? Int Clin Psychopharmacol. 2001 May;16(3):121–135. doi: 10.1097/00004850-200105000-00001. Available from: http://dx.doi.org/10.1097/00004850-200105000-00001. [DOI] [PubMed] [Google Scholar]
- 37.Wittchen HU, Jacobi F, Klose M, Ryl L. Depressive Erkrankungen. Berlin: Robert-Koch-Institut; 2010. (Gesundheitsberichterstattung des Bundes; 51). [Google Scholar]
- 38.Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jönsson B, Olesen J, Allgulander C, Alonso J, Faravelli C, Fratiglioni L, Jennum P, Lieb R, Maercker A, van Os J, Preisig M, Salvador-Carulla L, Simon R, Steinhausen HC. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011 Sep;21(9):655–679. doi: 10.1016/j.euroneuro.2011.07.018. Available from: http://dx.doi.org/10.1016/j.euroneuro.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 39.Wittchen HU, Müller N, Schmidtkunz B, Winter S, Pfister H. Erscheinungsformen, Häufigkeit und Versorgung von Depressionen. Ergebnisse des bundesweiten Gesundheitssurveys Psychische Störungen". Fortschr Med. 2000;118(S1):4–10. [Google Scholar]
- 40.Wittchen HU, Pittrow D. Prevalence, recognition and management of depression in primary care in Germany: the Depression 2000 study. Hum Psychopharmacol. 2002 Jun;17 Suppl 1:S1–11. doi: 10.1002/hup.398. Available from: http://dx.doi.org/10.1002/hup.398. [DOI] [PubMed] [Google Scholar]