Abstract
Research demonstrates substantial comorbidity between PTSD and alcohol use disorders. Evidence for functional relationships between PTSD and problematic alcohol use has not always been consistent, and there have been few investigations with adolescent samples. Further, research has not consistently controlled for cumulative potentially traumatic event (PTE) exposure when examining prospective relationships between PTSD and problematic alcohol use (i.e., binge drinking). This study examines the prospective relationships between PTSD symptoms, problematic alcohol use, and cumulative PTE exposure measured at three time points over approximately three years among a nationally representative sample of adolescents exposed to at least one PTE (N = 2399 and age range = 12–17 at wave 1). Results from parallel process latent growth curve models demonstrated that increases in cumulative PTE exposure over time positively predicted increases in both PTSD symptoms and binge drinking, whereas increases in PTSD symptoms and increases in binge drinking were not related when controlling for the effect of cumulative PTE exposure. Further analyses suggested that these relationships are specific to assaultive PTEs and are not found with non-assaultive PTEs. Theoretical implications are discussed.
Keywords: PTSD, trauma, assault, binge drinking, adolescents
Exposure to potentially traumatic events (PTE) is common, with a prevalence of approximately 65% in the general population (Kessler, 2000; Kilpatrick et al., 2003; Resnick et al., 1993). Some individuals develop Posttraumatic Stress Disorder (PTSD) following PTE exposure, which is characterized by intrusive re-experiencing of a traumatic event, avoidance of trauma-related cues, and physiological hyperarousal symptoms (American Psychological Association [APA], 2000). PTSD is associated with significant psychosocial impairment (Amaya-Jackson et al., 1999; Breslau, 2001; Kessler, 2000) and lower quality of life relative to other anxiety disorders (Olatunji, Cisler, & Tolin, 2007). In contrast to overall PTE prevalence, PTSD has an estimated prevalence of 8% (APA, 2000; Breslau, Davis, Andreski, & Peterson, 1991; Kessler et al., 2005; Kilpatrick et al., 2003; Resnick et al., 1993). Given the prevalence and negative impact of PTSD, researchers have become increasingly interested in delineating mechanisms contributing to the development and maintenance of PTSD.
Systematically examining comorbid conditions is one approach that may shed light on these mechanisms of PTSD. Such research has shown that PTSD is often comorbid with substance use disorders (Chilcoat & Breslau, 1998; Breslau et al., 2003; McFarlane, 1998; Stewart, 1996; Stewart et al., 1998), particularly alcohol use disorders (AUDs; Mills et al., 2006; Stewart, 1996). For example, 52% of males and 30% of females diagnosed with PTSD are also diagnosed with an AUD (Kessler et al., 1995). This relationship is also found among young adults and adolescents (Kilpatrick et al., 2003; Reed et al., 2007). For example, Kilpatrick and colleagues (2003) found that 30% of adolescent males and 24% of adolescent females diagnosed with PTSD were also diagnosed with a substance use disorder. The high prevalence of AUD and other substance use disorders among individuals with PTSD can be compared to the lower prevalence rates of 5% and 1% for AUDs and other substance use disorders, respectively, in the general population (Compton, Thomas, Stinson, & Grant, 2007; Hasin, Stinson, Ogburn, & Grant, 2007).
Given the robustness of these comorbidity patterns, there has been much speculation as to why PTSD is so frequently comorbid with AUDs and other substance use disorders. The explanation that has received the most empirical attention is the self-medication hypothesis (Khantzian, 1985). This hypothesis has two main predictions: 1) alcohol intoxication should at least temporarily reduce anxiety, which provides a mechanism for negative reinforcement via escape or avoidance of PTSD symptoms, and 2) PTSD development should precede the development of AUD. Research over the last two decades has yielded mixed results in support of the self-medication hypothesis. First, research has not consistently demonstrated that alcohol intoxication reliably causes straightforward reductions in anxiety during a stressor (Abrams & Wilson, 1979; Carrigan & Randall, 2003; Himle et al., 1999; Kushner et al., 2000; Kusnher et al., 1996; Morris, Stewart, & Ham, 2005). Instead, whether alcohol intoxication leads to reductions in anxiety depends on the type of stressor (e.g., carbon dioxide challenge versus public speech challenge; Himle et al., 1999; Kushner et al., 1996), whether drinking occurs before or after learning about the upcoming stressor (e.g., appraisal disruption hypothesis; Sayette, 1993), whether there is a family history of alcoholism or anxiety disorders (Sinha et al., 1998), and also on one’s alcohol expectancies (Abrams et al., 2004). This research suggests that alcohol only offers escape or avoidance of anxiety symptoms under certain conditions, which calls into question the power of the self-medication hypothesis’ first prediction. Second, the prediction that PTSD precedes the development of AUD also has inconsistent support. Several studies have found that PTSD prospectively predicts AUD onset (Breslau et al., 1997; Chilcoat & Breslau, 1998; McFarlane, 1998; Reed, Anthony, & Breslau, 2007), while other prospective studies either suggest no relationship between PTSD and AUD (Breslau, Davis, & Shultz, 2003; Shipherd et al., 2005) or show the opposite temporal pattern (Cottler et al., 1992). This research further questions the accuracy of the self-medication hypothesis.
A second explanation for the robust relationship between AUDs and PTSD is that AUDs increase vulnerability towards the development of PTSD (Kushner et al., 2000; Stewart et al., 1998). One central mechanism in this explanation is that AUDs are associated with anxiogenic withdrawal symptoms, and these anxiogenic withdrawal symptoms increase PTSD symptoms following PTE exposure (Kushner et al., 2000). Another mechanism posited in this explanation is that behavior during alcohol intoxication may increase the likelihood of PTE exposure, thus also increasing likelihood of PTSD development (Jacobsen et al., 2001; Stewart et al., 1998). The hypothesis that AUDs may increase vulnerability to PTSD, regardless of the mediating mechanism, predicts that AUD onset should temporally precede the development of PTSD. However, this prediction has also not been consistently supported. Whereas some studies support this temporal relationship (Cottler et al., 1992), as noted above, several studies find the opposite temporal pattern (Breslau et al., 1997; Chilcoat & Breslau, 1998; McFarlane, 1998; Reed, Anthony, & Breslau, 2007).
A third hypothesis explaining the robust relationship between PTSD and AUDs posits that the relationship may be due to a shared third variable (Kushner et al., 2000; Stewart et al., 1998). While focus commonly has been on shared genetic influences as the third variable explaining the relationship between PTSD and AUD (cf., Kushner et al., 2000), another possibility that has not received thorough empirical testing is that cumulative PTE exposure may account for vulnerability towards both outcomes (cf., Brady & Sinha, 2005). Previous research has yielded mixed results regarding whether PTE exposure alone (i.e., independent of PTSD) increases risk for AUDs, with some studies yielding a null effect (e.g., Breslau et al., 2003; Chilcoat & Breslau, 1998; Reed et al., 2007) and others yielding a positive effect (e.g., Kilpatrick et al., 1997; 2000; Stewart et al., 1996). One possible explanation for the inconsistent results is that studies often collapse the count of PTE exposure into a dichotomous variable of ‘any exposure’ versus ‘no exposure.’ PTE exposure may have a cumulative allostatic effect (Kollassa et al., 2010; McEwen, 2004; Neuner et al., 2004; Steel et al., 2009; but also see Breslau, Peterson, & Schultz, 2008), and dichotomization may fail to capture this effect. Additionally, different PTEs may have different effects on mental health outcomes. For example, assaultive (e.g., rape, physical assault) PTEs are associated with higher rates of PTSD compared to non-assaultive PTEs (Kessler et al., 1995; Resnick et al., 1993). Studies that only examine ‘any PTE exposure’ versus ‘no PTE exposure’ necessarily collapse across types of PTEs, which could further obscure any clear independent effects of PTE exposure. No previous epidemiological study has examined the relationship between PTSD symptoms and drinking behavior when accounting for this effect of cumulative PTE.
A major limitation of the available studies examining relationships between PTEs, PTSD, and alcohol use is that they are almost exclusively limited to adult samples. There is a general lack of prospective studies examining these relationships among adolescents, and cross-sectional studies provide conflicting findings regarding functional relations (Danielson et al., 2010; DeMilio, 1989; Lopez, Turner, & Saavedra, 2005). Examining these relationships among adolescents specifically is important for two reasons. First, children and adolescents may be more sensitive to the effects of PTE exposure. Evidence for this hypothesis comes from studies demonstrating that age of PTSD onset among children and adolescents positively correlates with brain volume (De Bellis et al., 1999) and that stress has a stronger negative biological impact during adolescence compared to adulthood (McCormick et al., 2010; McCormick & Mathews, 2007). If adolescence is a developmental period marked by sensitivity to stress, then different relations might therefore be expected between cumulative PTE exposure, PTSD symptoms, and problematic drinking behavior. Second, drinking behavior during adolescence, particularly binge drinking, is strongly predictive of future AUD development (Bonomo et al., 2004; Hingson et al., 2006; Viner & Taylor, 2007). Accordingly, understanding the factors influencing adolescent drinking behavior may facilitate understanding of both adolescent and future drinking behavior.
The present study provides a unique opportunity to empirically examine the three competing explanations of the relation between PTSD and problematic alcohol use among a nationally representative sample of adolescents, and also to test whether these relationships differ as a function of type of traumatic event exposure (i.e., assaultive versus non-assaultive; cf., Resnick et al., 1993). Problematic alcohol use was indexed with binge drinking frequency. Binge drinking frequency during adolescence is strongly predictive of subsequent AUD (Bonomo et al., 2004; Viner & Taylor, 2007); thus, binge drink frequency is a useful measure of problematic alcohol use, even when there is no indication of impairment.
Method
Participants
The National Survey of Adolescents-Replication (NSA-R) is a longitudinal epidemiological study of youth aged 12–17 (n=3,614 at Wave 1) residing in the U.S, aimed at determining the prevalence and correlates of adolescents’ exposure to PTEs. The sampling and methodological procedures used in the NSA-R have been reported in detail elsewhere (see Wolitzky-Taylor et al., 2009) and are briefly summarized here. The full sample included a national household probability sample as well as an oversample of urban-dwelling adolescents. Analyses here were constricted to individuals endorsing at least one PTE at Wave 1 (i.e., individuals with no PTE exposure cannot by definition have any PTSD symptoms to measure over time), resulting in 2,399 adolescents (1,174 female). Mean age was 14.82 (SD = 1.64), 62% were Caucasian, 18% were African-American, 12% were Hispanic, 3% were Native American, 2% were Asian, 1% were Pacific Islander, and 2% described their racial/ethnic status as ‘other.’.
Measures
Cumulative PTE history
Cumulative PTE history was assessed by asking the adolescents to endorse behaviorally specific events. Participants answered with a ‘yes’ or ‘no’ response. Participants were asked about the following events: 1) sexual assault (i.e., anal penetration, vaginal penetration, oral sex on the perpetrator, oral sex from the perpetrator, digital penetration, fondling of the adolescent, forced fondling of the perpetrator, or drug or alcohol facilitated sexual assault) using questions such as “Has a man or boy ever put his private sexual part (inside your private sexual part), inside your rear end, or inside your mouth when you didn’t want him to?”, 2) physical assault (i.e., attack with a weapon, attacked with a stick, club, or bottle, attacked without a weapon, threatened with a weapon, attacked with fists) with questions such as “Has anyone – including family members, dating partners, or friends – ever attacked you with a gun, knife, or some other weapon, regardless of when it happened or whether you ever reported it to the police?”, 3) abuse from a caregiver (i.e., spanked, slapped, pushed, locked in a closet, thrown against a hard surface, beaten up with fists or kicked, choked, burned on purpose, cut with sharp object, or threatened with a weapon) utilizing questions such as “Has a parent or other adult in charge of you ever spanked or slapped you so hard it caused bad bruises, cuts, or welts on you?”, 4) witnessed community violence (i.e., witnessed shooting, witnessed stabbing, witnessed sexual assault, witnessed robbery, witnessed threatening with a weapon, witnessed hitting or kicking) assessed with questions such as “Have you ever seen someone actually shoot someone else with a gun?”, 5) witnessed domestic violence (i.e., witnessing pushing or shoving, punching or hitting, choking, hitting with objects, or threatening with weapon) using questions such as “Have you ever seen or heard one of your parents push, shove, or slap the other in anger?”, and 6) other traumatic events (i.e., motor vehicle accidents, other accidents, fires, natural disasters, bitten by dog) with questions such as “Have you ever been in a serious motor vehicle accident in a car, truck, or motorcycle?” For specific details of this methodology, see (Kilpatrick et al., 2000; 2003). Consistent with the recently proposed criteria for DSM-V (http://www.dsm5.org/), a PTE was considered endorsement of any of the events regardless of whether the individual experienced fear, helplessness, or horror.
At Wave 1, participants indicating ‘yes’ were then asked how many times the event had ever happened to them. At Waves 2 and 3, participants indicating ‘yes’ were then asked how many times since the last interview the event had happened to them. Three PTE variables were created: 1) cumulative assaultive PTE history (sum of sexual assault, physical assault, caregiver abuse, witnessed community violence, and witnessed domestic violence), 2) cumulative non-assaultive PTE history (sum of the ‘other’ PTEs [e.g., accidents, natural disasters]), and 3) cumulative total PTE history (sum of all PTEs). These variables were computed separately for Waves 1, 2, and 3.
One limitation of prospectively measuring cumulative PTE exposure is that there will necessarily be dependency between the variables at the different time points (i.e., total PTEs to which an adolescent was exposed at Wave 2 is dependent on the number of PTEs to which the adolescent was exposed at Wave 1). Dependency between variables measured prospectively is common and one means of statistically addressing this issue is by allowing the residuals of the observed variables (e.g., cumulative PTE exposure) to covary (Byrne & Crombie, 2003; Kline, 2005). As will be described in the results section, this was not necessary for the individual and combined models to provide good fits to the data, which provides strong evidence that the dependency between variables was not problematic (Byrne & Crombie, 2003).
PTSD symptoms
Current PTSD symptoms were assessed using the PTSD module of the NSA survey (Kilpatrick et al., 2000) and National Women Survey (Resnick et al., 1993), a structured diagnostic interview that assessed each DSM-IV symptom with a yes/no response indicating the presence of a symptom during the last 6 months. Symptoms endorsed were added to create a total sum of PTSD symptoms. The symptoms were not anchored to any specific index traumatic event. This measure demonstrates good concurrent validity and several forms of reliability (e.g., temporal stability, internal consistency, diagnostic reliability; Resnick et al., 1993; Ruggiero et al., 2006). The measure was validated against the PTSD module of the Structured Clinical Interview for the DSM (SCID; Spitzer, Williams, & Gibbon, 1987) administered by mental health professionals (Kilpatrick et al, 1998). The inter-rater kappa coefficient was 0.85 for the diagnosis of PTSD, and comparisons between the PTSD module used here and SCID yielded a kappa coefficient of 0.77.
Binge Drinking Frequency
Problematic alcohol use frequency was assessed by asking the adolescents how many days in the past 12 months they had consumed 5 or more alcoholic drinks (i.e., binge drink frequency; Courtney & Polich, 2009). Binge drinking was categorized as five or more drinks per drinking day following the Center for Disease Control Behavioral Risk Factor Surveillance System standard question/definition (see Stahre, Naimi, Brewer, & Holt, 2006). Further, this is the most commonly used definition in population-based research (e.g., Monitoring the Future, National College Health Risk Behavior Survey, Core Alcohol and Drug Survey, National Household Survey of Drug Abuse) allowing for comparability across studies (McCauley et al., 2009; Wechsler & Nelson, 2001).
Procedure
Participants were selected using a multi-stage, stratified, random-digit dial procedure within each region of the country. The highly structured interview was administered by trained interviewers at a survey research firm with significant experience managing survey studies (Shulman, Ronca, and Bucuvalas, Inc.). A computer-assisted telephone interview system aided this process by prompting interviewers with each question consecutively on a computer screen, and supervisors conducted random checks of data entry accuracy and interviewers’ adherence to assessment procedures. Interviews began with parental consent and a brief parent interview consisting primarily of demographic questions. The majority of the interview was conducted with the adolescent.
Mean number of months between Wave 1 and Wave 2 assessment among PTE exposed adolescents was 15.45 (SD = 4.76), and mean number of months between Wave 2 and Wave 3 assessment was 14.61 (SD = 2.79). Missing data for any variable among completers never exceeded 2.3%.
Attrition
Of the 2399 PTE-exposed adolescents that completed the Wave 1 assessment, 1638 completed Wave 2 assessment and 1051 completed Wave 3 assessment. Individuals who did not complete each time point assessment had a greater Wave 1 cumulative PTE exposure history (M=3.70, SD=2.79) compared to completers (M=3.16, SD=2.50), F(1, 2398) = 24.09, p<.001, ηp2=.01. Although non-completers had higher initial PTSD symptoms (M=1.98, SD=2.85) and binge frequency (log transformed M=.15, SD=.37) relative to completers (M=1.88, SD=2.86, and log transformed M=.13, SD=.36, respectively), these differences were not significant (Fs<1.5, ps>.23). Completers did not differ from non-completers in gender, χ2(1)=.02, p>.05, but participants belonging to a minority race or ethnicity were more likely to not complete all three waves, χ2(1)=56.7, p<.01. Missing values of the primary variables entered in the primary analyses were estimated using maximum likelihood (ML) in Amos 18, and previous research demonstrates that ML is an appropriate imputation method when large amounts of data are missing not at random (Newman, 2003). Further, analyses were repeated when restricting the sample to only participants who completed each measurement point (n=1051). Results were essentially the same and did not change interpretation; thus, we chose to report results from the full sample.
Analytic Approach
Parallel process latent growth curve modeling (LGM), an application of structural equation modeling for longitudinal designs, was employed. Intra-individual patterns of change are represented by an intercept latent factor and slope latent factor(s). The intercept latent factor represents the initial level of the variable being measured when the first measurement point is coded as 0 in the shape factors, as was done in the present model (Biesanz, Deeb-Sossa, Papadikis, Bollen, & Curran, 2004; Duncan et al., 2006). The slope latent factor(s) represent the shape of the change (i.e., growth) in the measured variable over the measurement period. Shape of growth is measured with a linear slope latent factor, in which the paths from the linear slope factor to the measured variables are fixed to increase (or decrease, depending on the direction of growth) at a linear rate (e.g., 0, 1, 2, etc.). However, non-linear patterns of growth can also be modeled, and one means of modeling non-linear growth is by allowing the final regression path on the slope factor to be freely estimated in a three-wave longitudinal design.
Parallel process LGM (Cheong et al., 2003) allows a researcher to examine how the parameters of one individual LGM predict the parameters of one or more other individual LGMs, and is becoming increasingly used to examine complex multivariate hypotheses in longitudinal data (e.g., Littlefield et al., 2010). In the present context, parallel process LGM allows for simultaneous modeling of 1) the relationships between PTE Intercept and Slope and Binge Intercept and Slope, 2) the relationships between PTE Intercept and Slope and PTSD Intercept and Slope, and 3) the relationships between PTSD Intercept and Slope and Binge Intercept and Slope. The simultaneous modeling of the relevant paths is important, as it allows for examining each path when controlling for variance explained by the other paths (i.e., unique and non-spurious variance explained by the path).
Fit indices to test the LGM were the χ2 test, comparative fit index (CFI), and root mean square error of approximation (RMSEA). CFI values above .95 suggest good fit (Hu & Bentler, 1999), RMSEA values below .08 suggest adequate fit, and values below .06 suggest good fit (Brown & Cudek, 1993; Hu & Bentler, 1999). It is important to note that interpretation of these fit indices is based on recommended criteria (Hu & Bentler, 1999) and that clear cut-offs for appropriate fit do not exist. LGM was conducted in the present study using AMOS 18.0 software (Arbuckle, 2007) with maximum likelihood estimation. To account for multiple comparisons, alpha was set at p < .01 for all path coefficients.
Results
Preliminary Analyses
Multivariate Normality
PTE count and PTSD symptoms at each wave demonstrated acceptable levels of skewness (< 2.1) and kurtosis (< 5.5; cf. Kline, 2005). However, binge frequency was significantly skewed (> 8.7) and kurtotic (> 104). Accordingly, binge frequency was log transformed, which improved both skewness (< 3.1) and kurtosis (<9.4).
PTE prevalence
Among this trauma-exposed sample, the prevalence of assaultive PTEs and non-assaultive PTEs was 75.2% and 66.9%, respectively, at Wave 1, 75.7% and 69.9% at Wave 2, and 75.9% and 71.4% at Wave 3. The prevalence of new assaultive PTEs and non-assaultive PTEs was 30% and 16%, respectively, at Wave 2, and 22% and 7% at Wave 3. Cumulative assaultive PTEs and non-assaultive PTEs were significantly, but weakly, correlated at Wave 1 (r=.09, p<.001) and Wave 2 (r=.18, p<.001), but not correlated at Wave 3 (r=.04, p=.19). Table 1 displays the mean number of exposures to assaultive, non-assaultive, and any PTE at Waves 1, 2, and 3.
Table 1.
Descriptive statistics of relevant study variables of those who completed each wave.
| Wave 1 | Wave 2 | Wave 3 | |
|---|---|---|---|
| Binge frequency | 2.27 (12.73) | 3.34 (16.11) | 5.48 (21.75) |
| PTSD symptoms | 1.97 (2.89) | 2.18 (3.28) | 1.94 (3.29) |
| Total PTE | 3.46 (2.68) | 4.11 (3.33) | 4.35 (3.68) |
| Assaultive PTE | 2.14 (2.17) | 2.58 (2.68) | 2.78 (3.02) |
| Non-assaultive PTE | 1.33 (1.38) | 1.53 (1.64) | 1.57 (1.73) |
Note. Values in parenthesis indicate SDs.
Binge drinking prevalence
Mean days in the past 12 months binge drinking for Waves 1, 2, and 3 are displayed in Table 1. Regarding the general frequency of binge drinking behavior, at Wave 1, 82% of adolescents reported 0 days binge drinking, 51% reported 0 days binge drinking at Wave 2, and 29% 0 days binge drinking at Wave 3. Age was significantly correlated with binge drinking (r = .31, .29, and .32 at Waves 1, 2, and 3, all ps < .001), so the frequency of any binge drinking was examined as a function of age. Adolescents aged 12–15 at Wave 1 were less likely to have engaged in binge drinking in the past 12 months at Wave 1 (91.2% reported 0 days in the past 12 months), Wave 2 (58% reported 0 days in past 12 months), and Wave 3 (35% reported 0 days in the past 12 months) relative to adolescents aged 16–17 at Wave 1, with Wave 1, 2, and 3 frequencies of 0 binge drinking in past 12 months of 67%, 40%, and 20%, respectively.
Individual LGMs
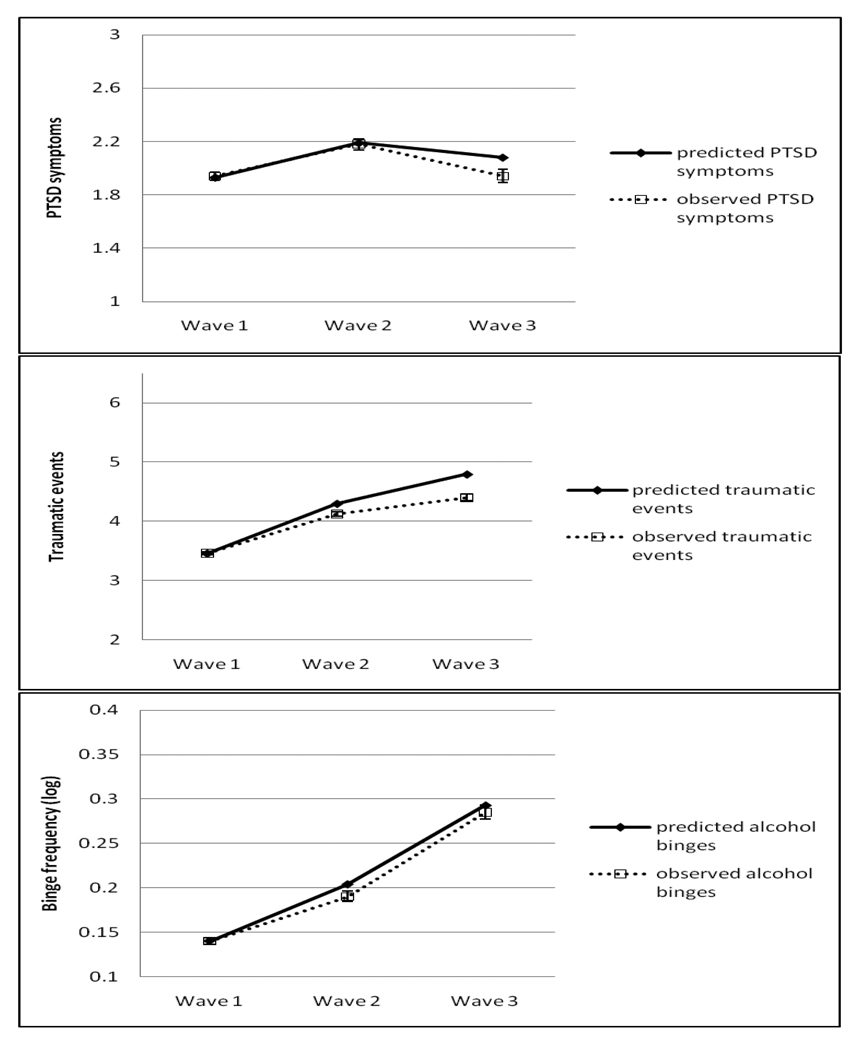
For each variable of interest, an individual LGM was tested in order to establish appropriate fit and whether the modeled slope trajectory was appropriate. All final models for the individual LGMs demonstrated good fit to the data (all CFIs over .982, all RMSEAs less than .061). For each individual LGM, a non-linear slope provided better fit than a linear slope. For the PTSD LGM, best fit was provided by constraining the error variances of Wave 1 and Wave 2 to be equal, and best fit was provided in the PTE and Binge models by constraining error variances at all three Waves to be equal. Further, as shown in Figure 1, the values predicted by the LGMs correspond closely to the observed values, which demonstrate that the individual LGMs correctly modeled the growth processes of interest. The individual LGMs were then combined to test a measurement model for the parallel process LGM, in which all latent variables were allowed to freely covary. Gender and age were also included in the model as covariates and allowed to covary with all latent variables. This model provided a good fit to the data: χ2(27)=122.47, p<.001, CFI=.990, RMSEA=.038 (90% CI=.032–.045). The variances of all latent intercept and slope variables were significant (all ps < .001), which provides support for specifying regression paths between the latent variables in the parallel process LGM to explain this variability.
Figure 1.
Observed means (and standard error bars) and means predicted by the individual LGM across the waves. Top figure = PTSD symptoms; middle figure = PTE exposure; bottom figure = binge drinking frequency.
Parallel Process LGMs
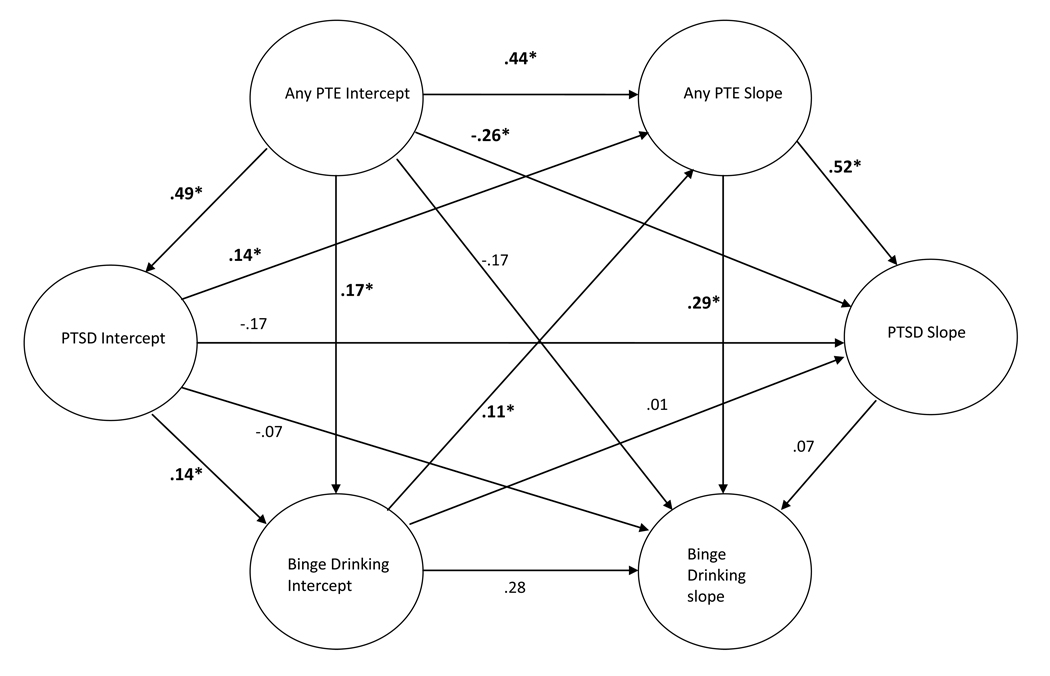
Cumulative Total PTE, PTSD symptoms, and Binge Drinking
This analysis used the full sample of PTE-exposed adolescents at Wave 1 (n=2399). Gender (1=male, 2=female) and age were also included as observed variable covariates and were specified as a predictor of each parameter of each individual LGM. This model used the cumulative total PTE variable and demonstrated a good fit to the data: χ2(27)=122.47, p<.001, CFI=.990, RMSEA=.038 (90% CI=.032–.045), AIC = 222.47. All regression paths for this model are displayed in Figure 2. As can be seen, PTE Slope was significantly positively related to Binge Slope (β=.29, p=.002), whereas PTSD slope was not significantly related to the Binge Slope (β=.07, p=.48). These results suggest that increased exposure to PTEs over the three year period (i.e., increases in the PTE Slope variable) predict increases in binge drinking over the three year period (i.e., increases in the Binge Slope variable), whereas this pattern is not found for the relationship between PTSD symptoms and Binge drinking frequency.
Figure 2.
Standardized path coefficients for the omnibus parallel process LGM (n=2399). Significant paths are indicated by bold font and an asterisk. Gender and age were included as covariates in the model, but are not in the figure to ease interpretability.
These data demonstrate that PTE Slope and not PTSD Slope predicts Binge Slope, but in order to demonstrate that cumulative PTE explains the prospective relationship between PTSD symptoms and binge frequency, it must also be demonstrated that PTSD Slope predicts Binge Slope when not controlling for the relationship between cumulative PTE exposure and binge frequency. Accordingly, another model was tested in which only the path from PTE Slope to Binge Slope was removed. Importantly, PTSD Slope was a robust and significant positive predictor of Binge Slope (β=.44, p< .001) when not considering the relation between PTE Slope and Binge Slope.
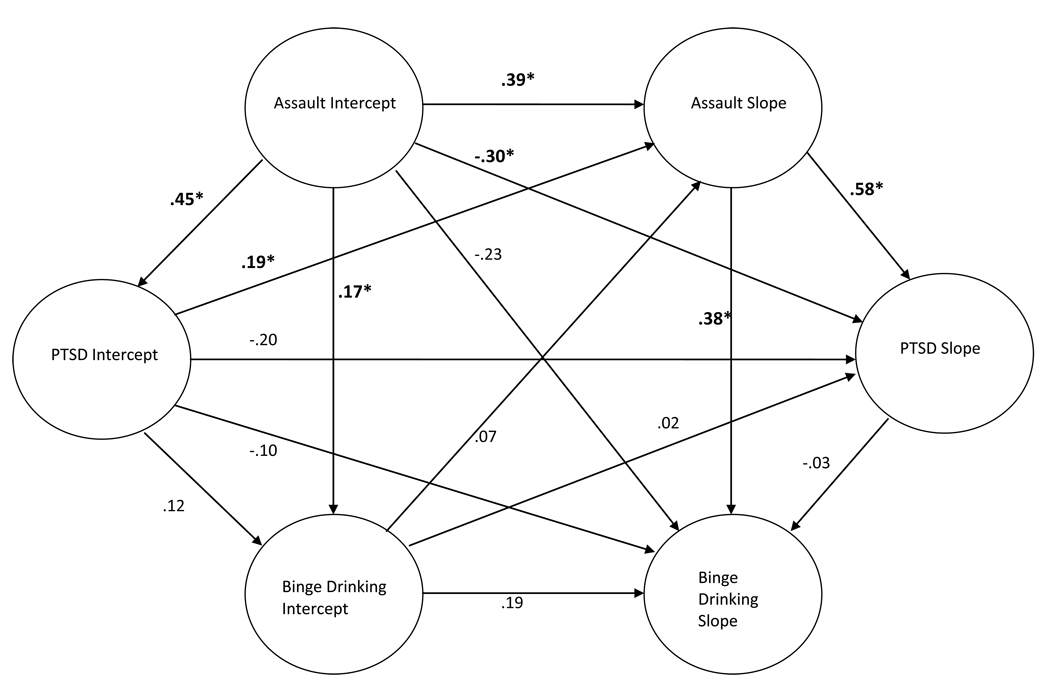
Cumulative Assaultive PTE, PTSD symptoms, and Binge Drinking
To examine the specific effect of assaultive PTE exposure, another model was tested using the cumulative assaultive PTE variable in the parallel process LGM using the subsample of adolescents exposed to an assaultive PTE at Wave 1 (n=1799). This model revealed a good fit to the data: χ2(27)=110.57, p< .001, CFI=.987, RMSEA=.042 (90% CI=.034–.050), AIC = 210.57. As with the first model, Assaultive PTE Slope was significantly positively related to Binge Slope (β=.38, p< .001), whereas PTSD Slope was not related to the Binge Slope (β=−.03, p =.83; see Figure 3). When removing the path from PTE Slope to Binge Slope, the path from PTSD slope to Binge Slope became significant (β=.46, p<.001). As with the above cumulative total PTE results, these results suggest that increased expose to assaultive PTEs specifically over the three year period predict increases in binge drinking over the three year period, whereas this pattern is again not found for the relationship between PTSD symptoms and Binge drinking frequency.
Figure 3.
Standardized path coefficients for the assaultive PTE parallel process LGM (n=1799). Significant paths are indicated by bold font and an asterisk. Gender and age were included as covariates in the model, but are not in the figure to ease interpretability.
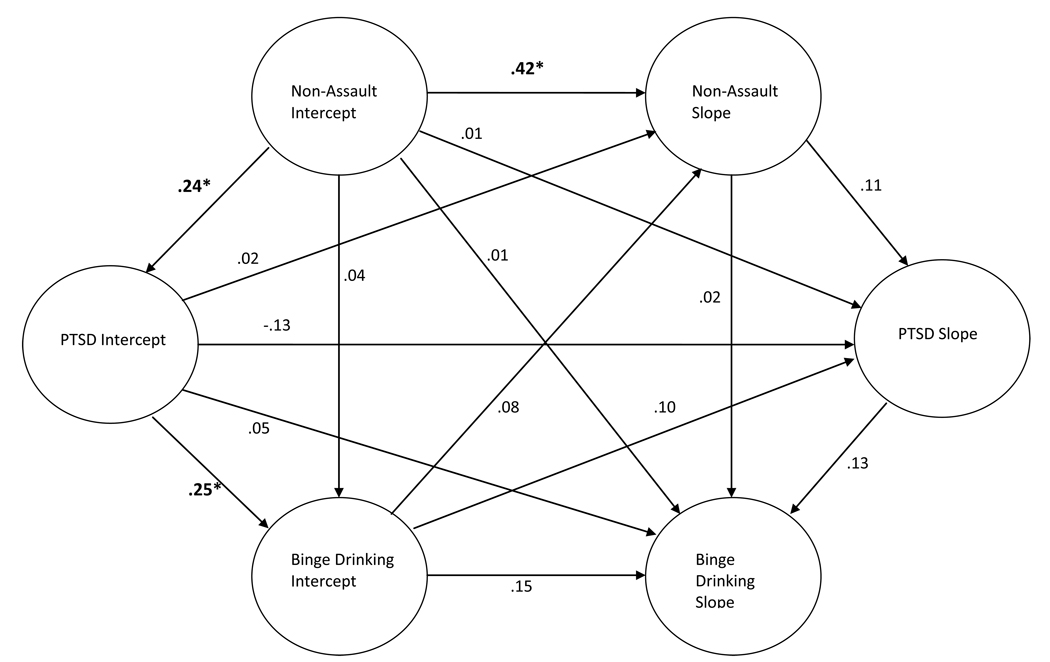
Cumulative Non-Assaultive PTE, PTSD symptoms, and Binge Drinking
Using the cumulative non-assaultive PTE variable within the subsample of adolescents exposed to at least one such event at Wave 1 (n=1600), another parallel process LGM was tested (see Figure 4). This model revealed a good fit to the data: χ2(27)=61.28, p <.001, CFI=.994, RMSEA=.028 (90% CI=.019–.038), AIC = 161.28. In contrast to the first two models, neither PTE Slope (β=.02 p=.81) nor PTSD Slope (β=.13, p=.30) were significantly related to Binge Slope. Further, PTE slope was not significantly related to PTSD Slope in this model (β=.11, p=.11). Finally, the unstandardized path coefficient for the Non-Assaultive PTE to Binge Slope path (B = .003, 95% CI:−.022 – .028) was significantly less than (p < .05) the unstandardized path coefficient for the Assaultive PTE to Binge Slope path (B = .06, 95% CI: .024 – .086) using the method described by Cummings and Finch (2005). Results from these analyses suggest that increased exposure to non-assaultive PTEs over the three year period are not significantly predictive of changes in binge drinking frequency or PTSD symptoms over the three year period. Further, the magnitude of the relation between increases in non-assaultive PTEs and changes in binge drinking is significantly weaker than the magnitude of the relation between increases in assaultive PTEs and changes in binge drinking frequency. 1, 2, 3
Figure 4.
Standardized path coefficients for the non-assaultive PTE parallel process LGM (n=1600). Significant paths are indicated by bold font and an asterisk. Gender and age were included as covariates in the model, but are not in the figure to ease interpretability.
Discussion
The present study examined the prospective relationships between PTSD symptoms, cumulative PTE exposure, and binge drinking in a nationally representative sample of adolescents. While initial levels (i.e., the intercepts) of PTE exposure, PTSD symptoms, and binge drinking were all related, the prospective relationships (i.e., the intercepts and slopes) suggested a specific pattern of functional relationships. The results demonstrate that increases in cumulative total PTE exposure and cumulative assaultive PTE exposure predict increases in both PTSD symptoms and binge drinking. By contrast, increases in PTSD symptoms and increases in binge drinking, regardless of modeled direction of causality, were only significantly related when not considering the significant effect of cumulative PTE exposure. These results can be discussed in the context of hypotheses explaining the robust relationship between PTSD and AUD.
First, the self-medication hypothesis (Khantzian, 1985) would predict that PTSD symptoms mediate the relationship between PTE exposure and increased drinking. The present results demonstrate that PTSD symptoms do not explain variability in binge drinking above and beyond cumulative PTE exposure; thus, attempts to dampen or avoid PTSD symptoms following PTE exposure does not seem a viable explanation of binge drinking in the present sample of adolescents. However, drinking to cope motives (cf., Littlefield et al., 2010) were not assessed in the present study and it remains possible that, specifically among individuals who drink to cope, PTSD symptoms would predict binge drinking above and beyond PTE exposure. Second, the data were not consistent with the hypothesis that alcohol use increases vulnerability to PTSD through either increased PTE exposure (initial binge drinking did not predict increases in cumulative PTE over time) or anxiogenic withdrawal symptoms (neither initial binge drinking nor increases in binge drinking over time predicted increases in PTSD symptoms). Further, increases in binge drinking did not predict increases in PTSD symptoms even when removing the effect of cumulative PTE exposure on increases in binge drinking. However, the design of the present study was not optimal for testing the hypothesis that alcohol-related anxiogenic withdrawal symptoms increase PTSD symptoms over time because there was no assessment of withdrawal. Thus, it remains possible that binge drinking would predict increases in PTSD symptoms among those adolescents whose drinking is severe enough to produce anxiogenic withdrawal symptoms.
The results do provide support for the hypothesis that PTSD and problematic alcohol use are related through a common third variable(s). In this study, the relationship appears to be explained by cumulative PTE exposure. While some prior studies have not revealed a unique effect of PTE exposure on drinking behavior (Breslau et al., 2003; Chilcoat & Breslau, 1998; Reed et al., 2007), the present results differ from previous studies in two important ways. First, the present results were found among an adolescent sample. The strong effects of PTE exposure may be consistent with observations that adolescent brains are particularly sensitive to the effects of stress (McCormick & Mathews, 2007). Alternatively, the lack of incremental effect of PTSD symptoms on binge drinking may be due to less developed beliefs about the stress dampening effects of alcohol (e.g., drinking to cope motives) among adolescents relative to adults. Second, the present study accounted for cumulative PTE exposure, which highlights the importance of investigating the number of PTE exposures, rather than using a dichotomous ‘exposed’ versus ‘non-exposed’ variable.
PTE exposure is not expected to fully explain either PTSD or binge drinking; instead, it may be the case that cumulative PTE exposure affects the functioning of neurobiological mechanisms that mediate vulnerability for both PTSD and AUDs. For example, chronic stress has been found to increase dendritic branching in the amygdala and increase reactivity towards motivationally salient cues (e.g., threat cues and drug cues), decrease dendritic spine density and length in key structures of the prefrontal cortex necessary for cognitive, emotional, and behavioral control, and alter dopamine transmission and reward areas of the brain (Arnsten, 2009; Izquierdo et al., 2006; Liston et al., 2006; Mitra et al., 2005; Pacak et al. 2002; Radley et al., 2006; Saal et al., 2003; Vyas et al., 2002; 2004). However, results from the present study cannot directly speak to the mechanisms by which cumulative PTE exposure increases vulnerability for PTSD and AUD. Nonetheless, the results do support previous speculation that PTSD and AUD may be linked through common stress-related pathways (cf. Brady & Sinha, 2005).
The present results demonstrate that the effect of cumulative PTE exposure on PTSD symptoms and binge drinking is specific to assaultive, and not non-assaultive, PTE exposure. These findings are in line with previous research demonstrating that assaultive (vs. non-assaultive) PTEs are a more “potent” risk factor for mental health outcomes (Kessler et al., 1995; Resnick et al., 1993). The present results extend this literature by also demonstrating that PTSD symptoms related to assaultive PTEs predict exposure to new assaults, but PTSD symptoms related to non-assaultive PTEs do not predict increases in new exposure to non-assaultive PTEs. These results suggest a ‘vicious cycle’ between assaultive PTE exposure and PTSD symptoms: assaultive PTE exposure predicts PTSD symptoms, which predict increased PTE exposure, which predicts greater PTSD symptoms. The mechanisms by which PTSD symptoms lead to increased exposures to new assaults are unclear (cf. Cougle et al., 2009) and future research is necessary to clarify this relationship.
The present results suggest other relevant prospective relationships. First, the results suggest a nuanced description of the longitudinal course of PTSD symptoms. Initial PTE exposure has a negative relationship with growth in PTSD symptoms. Given that initial PTE exposure had a positive relationship with initial PTSD symptoms, which suggests that PTSD severity at one time point increases as a function of greater cumulative PTE exposure, the negative relationship between initial PTE and change in PTSD symptoms over time may reflect that PTSD symptoms tend to decrease as time since PTE exposure increases (Goenjian et al., 2005; Steel et al., 2009). This suggests that greater initial cumulative PTE exposure does not directly predict a more chronic longitudinal course of PTSD symptoms. Instead, initial PTE exposure may predict greater initial PTSD symptoms, which predicts greater increases in cumulative PTE exposure, which in turn predicts greater increases in PTSD symptoms. This ‘vicious cycle’ echos other research demonstrating that PTSD remission may be hampered by exposure to new PTEs (Perkonigg et al., 2005) and suggests that the relationship between initial PTSD symptoms and PTSD chronicity is mediated by the effect of initial PTSD symptoms on exposure to new PTEs, particularly assaultive PTEs.
Second, the results also shed light on the longitudinal course of PTE exposure. The intercept of these variables were each positively related to their respective slope parameters. The finding that the slope of PTE exposure depends on initial PTE exposure, above and beyond the influence of initial PTSD symptoms, may be due to alterations in neurobiological mechanisms impairing self-control and decision making processes (e.g., putting oneself in riskier and riskier situations). Alternatively, this relationship could be due to static environmental variables (e.g., poverty, caregiver abuse from a caregiver who remains in the home) that continue to confer vulnerability for PTE exposure after the first exposure. Future research will benefit from examining the mechanisms by which initial PTE exposure confers vulnerability for additional PTE exposure.
The present results must be considered in the context of the following limitations. First, the results are specific to problematic alcohol use, and it is important to note that different substances have different pharmacological effects that may moderate their association with PTSD. Future research is necessary to test for specific relationships with specific substances. Second, PTSD symptoms and problematic alcohol use frequency were analyzed continuously and it is possible that using a PTSD or AUD diagnosis would yield different results. Third, a true test of the present hypotheses about why cumulative PTE increased vulnerability for both PTSD and binge drinking would involve direct measures of neurobiological functioning, which were not obtained in this epidemiological sample. Future laboratory-based research is needed to more clearly test these hypotheses. Fourth, attrition was high and did not occur at random. It remains possible that different results would have been obtained if more of the adolescents had been retained across the assessment waves and future research is necessary to replicate these results among a longitudinal sample where attrition is not as large or biased. Similarly, participants belonging to a minority race or ethnicity were less likely to complete the study; thus, future research should pay particular attention to this important demographic variable in future research. Fifth, the results are limited to self-report indices, and adolescents may not have accurately reported their PTE exposure history. Sixth, there are numerous other third variables, in addition to PTE exposure, that could explain the observed relations, including delinquency, family characteristics, peer groups, socioeconomic status, etc. Future research will be needed to rule out these alternative influences. Seventh, PTSD symptom assessment was not tied to any particular PTE, which raises the possibility that the identified PTSD symptoms were not necessarily tied to any of the indicated PTEs. Finally, the observed relations only indicate correlations and causality cannot be established in these data, as there were no experimental manipulations.
Despite the limitations of the present study, the results highlight the importance of thoroughly assessing trauma history in order to fully estimate the risk of future mental health outcomes. Further, given the positive relationship between initial PTE exposure and increases in PTE exposure, and that increases in PTE exposure predict increases in PTSD symptoms and binge drinking, targeting PTE exposure per se through risk reduction strategies may be a powerful means of preventing negative future mental health outcomes. Demonstrating the viability of such risk reduction protocols, Orchowski and colleagues (2008) recently found that a risk reduction protocol among college women reduced the incidence of rape relative to a control group. The field is currently moving toward the development and evaluation of integrated protocols that incorporate risk reduction techniques into treatment of victimization among adolescents, with treatments such as Risk Reduction through Family Therapy (RRFT; Danielson, 2006) and Seeking Safety (Najavits, Gallop, & Weiss, 1996). Further evaluation and efforts to incorporate these protocols into existing PTSD treatments may be a useful area of future research.
Research Highlights.
-
-
Posttraumatic Stress Disorder (PTSD), assaultive violence exposure, and problematic drinking frequently co-occur
-
-
Increases in assaultive violence exposure over a three year period positively correlated with increases in both PTSD symptoms and binge drinking frequency.
-
-
Increases in PTSD symptoms and binge drinking frequency over the three year period were unrelated after controlling for increases in assaultive violence exposure.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
It was also tested whether the different symptom clusters of PTSD differentially affected the results for each of the three parallel process LGM models. Results were essentially the same in all models.
Given that analyses were restricted to adolescents who had experienced a PTE at wave 1, it remains possible that different results would be obtained among adolescents exposed to their first PTE. To rule out this alternative hypothesis, two multiple regression analyses were conducted among adolescents who reported 0 PTE exposures at wave 1 and at least 1 PTE exposure at either wave 2 or 3 (n = 192, 105 females). The first analysis entered wave 1, 2, and 3 binge drinking, wave 2 and 3 cumulative PTE exposure, and wave 2 PTSD symptoms as predictors of wave 3 PTSD symptoms. When controlling for wave 1 and 2 covariates, wave 3 PTE exposure predicted increased wave 3 PTSD symptoms (t = 3.66, p < .001, partial r = .30), but wave 3 binge drinking did not (partial r = .11, p = .19). A parallel analysis with wave 3 binge drinking as the dependent measure demonstrated that wave 3 PTE exposure predicted greater wave 3 binge drinking (t = 3.35, p = .001, partial r = .28), but wave 3 PTSD symptoms did not (partial r = .11, p = .19). These results replicate the more nuanced analyses among trauma exposed adolescents.
Other researchers (Kolassa et al., 2010; Neuner et al., 2004) advocate for defining cumulative PTE exposure as the total different types of PTEs to which the individual was exposed, as opposed to the total number of traumatic events as defined here. Accordingly, it was also tested whether results were the same with this other definition of cumulative PTE exposure. The total cumulative PTE, cumulative assaultive PTE, and cumulative non-assaultive PTE models all demonstrated good fit to the data (CFIs over .987, RMSEAs below .049). The same pattern of major results emerged in these other analyses: 1) cumulative total and cumulative assaultive PTE slope predicted increased binge slope and PTSD slope, 2) PTSD slope only predicted binge slope when removing the effect of PTE slope, 3) PTSD intercept predicted increased PTE slope for total and assaultive PTEs, and 4) binge intercept did not predict either PTSD slope or PTE slope. Given that results were the same regardless of how cumulative PTE exposure was defined, we chose to use the definition based on the total number of times an individual was exposed to a traumatic event, as opposed to the different types of traumatic events, because this definition is less dependent on the number of different types of traumatic events assessed.
References
- Abrams DB, Wilson GT. Effects of alcohol on social anxiety in women: cognitive versus physiological processes. Journal of Abnormal Psychology. 1979;88:161–173. doi: 10.1037//0021-843x.88.2.161. [DOI] [PubMed] [Google Scholar]
- Abrams K, Kushner M, Medina KL, Voight A. The pharmacologic and expectancy effects of alcohol on social anxiety in individuals with social phobia. Drug and Alcohol Dependence. 2004;64:219–231. doi: 10.1016/s0376-8716(01)00125-9. [DOI] [PubMed] [Google Scholar]
- Amaya-Jackson L, Davidson JR, Hughes DC, Swartz M, Reynolds V, George LK, et al. Functional impairment and utilization of services associated with posttraumatic stess disorder in the community. Journal of Traumatic Stress. 1999;12:709–724. doi: 10.1023/A:1024781504756. [DOI] [PubMed] [Google Scholar]
- Arnsten AF. Stress signalling pathways that impair prefrontal cortex structure and function. Nature Reviews Neuroscience. 2009;10:410–422. doi: 10.1038/nrn2648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baler RD, Volkow ND. Drug addiction: the neurobiology of disrupted self-control. Trends in Molecular Medicine. 2006;12:559–566. doi: 10.1016/j.molmed.2006.10.005. [DOI] [PubMed] [Google Scholar]
- Biesanz JC, Deeb-Sossa N, Papadikis AA, Bollen KA, Curran PJ. The role of coding time in estimating and interpreting growth curve models. Psychological Methods. 2004;9:30–52. doi: 10.1037/1082-989X.9.1.30. [DOI] [PubMed] [Google Scholar]
- Brady KT, Sinha R. Co-occurring mental and substance use disorders: the neurobiological effects of chronic stress. American Journal of Psychiatry. 2005;162:1483–1493. doi: 10.1176/appi.ajp.162.8.1483. [DOI] [PubMed] [Google Scholar]
- Breslau N. Outcomes of posttraumatic stress disorder. Journal of Clinical Psychiatry. 2001;62(supplement 17):55–59. [PubMed] [Google Scholar]
- Breslau N, Davis GC, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Archives of General Psychiatry. 1991;48:216–222. doi: 10.1001/archpsyc.1991.01810270028003. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Schultz LR. Posttraumatic stress disorder and the incidence of nicotine, alcohol, and other drug disorders in persons who have experienced trauma. Archives of General Psychiatry. 2003;60:289–294. doi: 10.1001/archpsyc.60.3.289. [DOI] [PubMed] [Google Scholar]
- Breslau N, Peterson EL, Schultz LR. A second look at prior trauma and the posttraumatic stress disorder effects of subsequent trauma: a prospective epidemiological study. Archives of General Psychiatry. 2008;65:431–437. doi: 10.1001/archpsyc.65.4.431. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing Structural Equation Models. Newbury Park, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- Byrne BM, Crombie G. Modeling and testing change: an introduction to the latent growth curve model. Understanding Statistics. 2003;2:177–203. [Google Scholar]
- Carrigan MH, Randall CL. Self-medication in social phobia: a review of the alcohol literature. Addictive Behaviors. 2003;28:269–284. doi: 10.1016/s0306-4603(01)00235-0. [DOI] [PubMed] [Google Scholar]
- Cheong J, MacKinnon DP, Khoo ST. Investigation of meditational processes using parallel process latent growth curve modeling. Structural Equation Modeling. 2003;10:238–262. doi: 10.1207/S15328007SEM1002_5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chilcoat HD, Breslau N. Posttraumatic stress disorder and drug disorders: testing causal pathways. Archives of General Psychiatry. 1998;55:913–917. doi: 10.1001/archpsyc.55.10.913. [DOI] [PubMed] [Google Scholar]
- Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry. 2007;64:566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- Cottler LB, Compton WM, Mager D, Spitznagel EL, Janca A. Posttraumatic stress disorder among substance users from the general population. American Journal of Psychiatry. 1992;149:664–670. doi: 10.1176/ajp.149.5.664. [DOI] [PubMed] [Google Scholar]
- Cougle JR, Resnick H, Kilpatrick DG. A prospective examination of PTSD symptoms as risk factors for subsequent exposure to potentially traumatic events among women. Journal of Abnormal Psychology. 2009;118:405–411. doi: 10.1037/a0015370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danielson CK, McCart M, de Arellano MA, Macdonald A, Silcott L, Resnick H. Risk reduction for substance use and trauma-related psychopathology in adolescent sexual assault victims: Findings from an open trial. Child Maltreatment. doi: 10.1177/1077559510367939. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeMilio L. Psychiatric syndromes in adolescent substance abusers. American Journal of Psychiatry. 1989;146:1212–1214. doi: 10.1176/ajp.146.9.1212. [DOI] [PubMed] [Google Scholar]
- Duncan TE, Duncan SC, Strycker LA. An introduction to latent variable growth curve modeling. Mahwah, NJ: Lawrence Erlbaum Associates; 2006. [Google Scholar]
- Goenjian AK, Walling D, Steinberg AM, Karayan I, Najarian LM, Pynoos R. A prospective study of posttraumatic stress and depressive reactions among treated and untreated adolescents 5 years after a catastrophic disaster. American Journal of Psychiatry. 2005;162:2302–2308. doi: 10.1176/appi.ajp.162.12.2302. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Himle JA, Abelson JL, Haghightgou H, Hill EM, Nesse RM, Curtis GC. Effect of alcohol on social phobic anxiety. American Journal of Psychiatry. 1999;156:1237–1243. doi: 10.1176/ajp.156.8.1237. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Izquierdo A, Wellman CL, Holmes A. Brief uncontrollable stress causes dendritic retraction in infralimbic cortex and resistance to fear extinction in mice. Journal of Neuroscience. 2006;26:5733–5738. doi: 10.1523/JNEUROSCI.0474-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liston C, Miller MM, Goldwater DS, Radley JJ, Rocher AB, Hof PR, et al. Stress-induced alterations in prefrontal cortical dendritic morphology predict selective impairments in perceptual attentional set-shifting. Journal of Neuroscience. 2006;26:7870–7874. doi: 10.1523/JNEUROSCI.1184-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littlefield AK, Sher KJ, Wood PK. Do changes in drinking motives mediate the relation between personality change and “maturing out” of problem drinking? Journal of Abnormal Psychology. 2010;119:93–105. doi: 10.1037/a0017512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez B, Turner RJ, Saavedra LM. Anxiety and risk for substance dependence among late adolescents/young adults. Journal of Anxiety Disorders. 2005;19:275–294. doi: 10.1016/j.janxdis.2004.03.001. [DOI] [PubMed] [Google Scholar]
- Kessler RC. Posttraumatic stress disorder: the burden to the individual and to society. Journal of Clinical Psychiatry. 2000;61(supplement 5):4–12. [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikanga KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ. The self-medication hypothesis of addictive disorders: focus on heroin and cocaine dependence. American Journal of Psychiatry. 1985;142:1259–1264. doi: 10.1176/ajp.142.11.1259. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Acierno R, Resnick HS, Saunders BE, Best CL. A 2-year longitudinal analysis of the relationships between violent assault and substance use in women. Journal of Consulting and Clinical Psychology. 1997;65:834–847. doi: 10.1037//0022-006x.65.5.834. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Acierno R, Saunders B, Resnick HS, Best CL, Schnurr PP. Risk factors for adolescent substance abuse and dependence: data from a national sample. Journal of Consulting and Clinical Psychology. 2000;68:19–30. doi: 10.1037//0022-006x.68.1.19. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Saunders BE, Best CL. Rape, other violence against women, and posttraumatic stress disorder. In: Dohrenwend BP, editor. Adversity, stress, and psychopathology. New York: Oxford University Press; 1998. pp. 161–176. [Google Scholar]
- Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, Best CL. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: results from the National Survey of Adolescents. Journal of Consulting and Clinical Psychology. 2003;71:692–700. doi: 10.1037/0022-006x.71.4.692. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and Practice of Structural Equation Modeling. 2nd Edition. New York: Guilford Press; 2005. [Google Scholar]
- Kolassa IT, Kolassa S, Ertl V, Papassotiropoulos A, De Quervain DJ. The risk of posttraumatic stress disorder after trauma depends on traumatic load and the catecho-methyltransferase Val(158)Met polymorphism. Biological Psychiatry. 2010;67:304–308. doi: 10.1016/j.biopsych.2009.10.009. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Abrams K, Borchardt C. The relationship between anxiety disorders and alcohol use disorders: a review of major perspectives and findings. Clinical Psychology Review. 2000;20:149–171. doi: 10.1016/s0272-7358(99)00027-6. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Mackenzie TB, Fiszdon J, Valentiner DP, Foa E, Anderson N, et al. The effects of alcohol consumption on laboratory-induced panic and state anxiety. Archives of General Psychiatry. 1996;53:264–270. doi: 10.1001/archpsyc.1996.01830030086013. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Protection and damage from acute and chronic stress: allostasis and allostatic overload and relevance to the pathophysiology of psychiatric disorders. Annals of the New York Academy of Sciences. 2004;1032:1–7. doi: 10.1196/annals.1314.001. [DOI] [PubMed] [Google Scholar]
- McFarlane AC. Epidemiological evidence about the relationship between PTSD and alcohol abuse: the nature of the association. Addictive Behaviors. 1998;23:813–825. doi: 10.1016/s0306-4603(98)00098-7. [DOI] [PubMed] [Google Scholar]
- Mills KL, Teesson M, Ross J, Peters L. Trauma, PTSD, and substance use disorders: findings from the Australian National Survey of Mental Health and Well-Being. American Journal of Psychiatry. 2006;163:652–658. doi: 10.1176/ajp.2006.163.4.652. [DOI] [PubMed] [Google Scholar]
- Mitra R, Jadhav S, McEwen BS, Vyas A, Chattarji S. Stress duration modulates the spatiotemporal patterns of spine formation in the basolateral amygdala. Proceedings of the National Academy of Sciences. 2005;102:9371–9376. doi: 10.1073/pnas.0504011102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris EP, Stewart SH, Ham LS. The relationship between social anxiety disorder and alcohol use disorders: a critical review. Clinical Psychology Review. 2005;25:734–760. doi: 10.1016/j.cpr.2005.05.004. [DOI] [PubMed] [Google Scholar]
- Najavits LM, Gallop RJ, Weiss RD. Seeking safety therapy for adolescent girls with PTSD and substance use disorder: A randomized controlled trial. The Journal of Behavioral Health Services and Research. 2006;33:453–463. doi: 10.1007/s11414-006-9034-2. [DOI] [PubMed] [Google Scholar]
- Neuner F, Schauer M, Karunakara U, Klaschik C, Robert C, Elbert T. Psychological trauma and evidence for enhance vulnerability for posttraumatic stress disorder through previous trauma among West Nile refugees. BMC Psychiatry. 2004;4:34. doi: 10.1186/1471-244X-4-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olatunji BO, Cisler JM, Tolin DF. Quality of life in the anxiety disorders: a meta-analytic review. Clinical Psychology Review. 2007;27:572–581. doi: 10.1016/j.cpr.2007.01.015. [DOI] [PubMed] [Google Scholar]
- Orchowski LM, Gidycz CA, Raffle H. Evaluation of a sexual assault risk reduction and self-defense program: a prospective analysis of a revised protocol. Psychology of Women Quarterly. 2008;32:204–218. [Google Scholar]
- Pacak K, Tjurmina O, Palkovits M, Goldstein DS, Koch CA, Hoff T, et al. Chronic hypercortisolemia inhibits dopamine synthesis and turnover in the nucleus accumbens: an in vivo microdialysis study. Neuroendocrinology. 2002;76:148–157. doi: 10.1159/000064522. [DOI] [PubMed] [Google Scholar]
- Perkonigg A, Pfister H, Stein MB, Hofler M, Lieb R, Maercker A, Wittchen HU. Longitudinal course of posttraumatic stress disorder and posttraumatic stress disorder symptoms in a community sample of adolescents and young adults. American Journal of Psychiatry. 2005;162:1320–1327. doi: 10.1176/appi.ajp.162.7.1320. [DOI] [PubMed] [Google Scholar]
- Radley JJ, Rocher AB, Miller M, Janssen WG, Liston C, Hof PR, et al. Repeated stress induces dendritic spine loss in the rat medial prefrontal cortex. Cerebral Cortex. 2006;16:313–320. doi: 10.1093/cercor/bhi104. [DOI] [PubMed] [Google Scholar]
- Reed PL, Anthony JC, Breslau N. Incidence of drug problems in young adults exposed to trauma and posttraumatic stress disorder: do early life experiences and predispositions matter? Archives of General Psychiatry. 2007;64:1435–1442. doi: 10.1001/archpsyc.64.12.1435. [DOI] [PubMed] [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting and Clinical Psychology. 1993;61:984–991. doi: 10.1037//0022-006x.61.6.984. [DOI] [PubMed] [Google Scholar]
- Ruggiero KJ, Rheingold AA, Resnick HS, Kilpatrick DG, Galea S. Comparison of two widely used PTSD-screening instruments: implications for public mental health planning. Journal of Traumatic Stress. 2006;19:699–707. doi: 10.1002/jts.20141. [DOI] [PubMed] [Google Scholar]
- Saal D, Dong Y, Bonci A, Malenka RC. Drugs of abuse and stress trigger a common synaptic adaptation in dopamine neurons. Neuron. 2003;37:577–582. doi: 10.1016/s0896-6273(03)00021-7. [DOI] [PubMed] [Google Scholar]
- Sayette MA. An appraisal-disruption model of alcohol’s effects on stress responses in social drinkers. Psychological Bulletin. 1993;114:459–476. doi: 10.1037/0033-2909.114.3.459. [DOI] [PubMed] [Google Scholar]
- Shipherd JC, Stafford J, Tanner LR. Predicting alcohol and drug abuse in Persian Gulf War veterans: what role do PTSD symptoms play? Addictive Behaviors. 2005;30:595–599. doi: 10.1016/j.addbeh.2004.07.004. [DOI] [PubMed] [Google Scholar]
- Sinha R, Robinson J, O’Malley S. Stress response dampening: effects of gender and family history of alcoholism and anxiety disorders. Psychopharmacology. 1998;137:311–320. doi: 10.1007/s002130050624. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M. Structured Clinical Interview for DSM-III-R. New York: New York State Psychiatric Institute, Biometrics Research Department; 1987. [Google Scholar]
- Stahre M, Naimi T, Brewer R, Holt J. Measuring average alcohol consumption: the impact of including binge drinks in quantity-frequency calculations. Addiction. 2006;101:1711–1718. doi: 10.1111/j.1360-0443.2006.01615.x. [DOI] [PubMed] [Google Scholar]
- Steel Z, Chey T, Silove D, Marnane C, Bryant RA, van Ommeren M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. Journal of the American Medical Association. 2009;302:537–549. doi: 10.1001/jama.2009.1132. [DOI] [PubMed] [Google Scholar]
- Stewart SH. Alcohol abuse in individuals exposed to trauma: a critical review. Psychological Bulletin. 1996;120:83–112. doi: 10.1037/0033-2909.120.1.83. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Pihl RO, Conrad PJ, Dongier M. Functional associations among trauma, PTSD, and substance-related disorders. Addictive Behaviors. 1998;23:797–812. doi: 10.1016/s0306-4603(98)00070-7. [DOI] [PubMed] [Google Scholar]
- Ullman SE, Filipas HH, Townsend SM, Starzynski LL. Trauma exposure, posttraumatic stress disorder and problem drinking in sexual assault survivors. Journal of Studies on Alcohol. 2005;66:610–619. doi: 10.15288/jsa.2005.66.610. [DOI] [PubMed] [Google Scholar]
- Vyas A, Chattarji S. Modulation of different states of anxiety-like behavior by chronic stress. Behavioral Neuroscience. 2004;118:1450–1454. doi: 10.1037/0735-7044.118.6.1450. [DOI] [PubMed] [Google Scholar]
- Vyas A, Mitra R, Shankaranarayana Rao BS, Chattarji S. Chronic stress induces contrasting patterns of dendritic remodeling in hippocampal and amygdaloid neurons. Journal of Neuroscience. 2002;22:6810–6818. doi: 10.1523/JNEUROSCI.22-15-06810.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vyas A, Pillai AG, Chattarji S. Recovery after chronic stress fails to reverse amygdaloid neuronal hypertrophy and enhanced anxiety-like behavior. Neuroscience. 2004;128:667–673. doi: 10.1016/j.neuroscience.2004.07.013. [DOI] [PubMed] [Google Scholar]
- Wechsler H, Nelson TF. Binge drinking in the American college student: What’s five drinks? Psychology of Addictive Behaviors. 2001;15:287–291. doi: 10.1037//0893-164x.15.4.287. [DOI] [PubMed] [Google Scholar]