Abstract
Considering the fact that a key factor in tumor development is the evasion of immune detection, the search for natural products, which have reduced toxicity towards normal tissues as well as immunostimulatory capabilities has received growing interest. One attractive source of antitumor products is the Ganoderma lucidum mushroom, which has been used for centuries as an herbal medicine for the prevention and treatment of a variety of diseases, including cancer, and has been shown to improve immune function. Interestingly, its methanol soluble triterpenoid extracts, namely Ganoderic Acids (GAs), have been the subject of several recent investigations on their chemotherapeutic effects. While current research has revealed GAs’ role in inducing apoptosis of cancer cells with a much lower toxicity to healthy cells, little information is available on their in vitro and/or in vivo immune activities. In this review, we aim to discuss the current knowledge on GAs, and their potential as apoptosis inducing as well as immune activating molecules that could be a potential alternative approach for designing novel chemoimmunotherapeutics against malignant diseases. We also discuss other new approaches for exploiting the advantages of using a nanoparticle polymer-GA conjugate as a tool for a sustained and targeted delivery of drug in vivo.
Keywords: Ganoderma lucidum, Ganoderic acids, Cancer, Apoptosis, Cytokines, Immune regulation, Nanoparticles
Introduction
Cancer is one of the world’s leading causes of death and arises when the homeostatic balance between cell growth and death is disturbed [1,2]. Recent reports estimate the total worldwide economic burden associated with cancer therapy to be several hundred billions of US$ [3]. Consequently, advances in cancer therapy will have economic as well as public health implications. As more evidence highlights the toxic side effects of traditional chemotherapies, there is a growing interest for alternative medicines to improve the function of the immune system in order to target late stage metastatic tumors. Natural extracts from fungi have been the focus of recent investigation, particularly those with reduced cellular toxicity to healthy tissue. When considering any new therapy, both efficacy and cost-effectiveness of the cancer treatment strategy are the two main players that decide the healthcare costs associated with cancer management. Advances in technology have allowed for widespread screening of natural products to identify those with anticarcinogenic and immunostimulatory potential. This has led to a renewed investigation into the anecdotal evidence of health benefits associated with folk medicine, with the goal of identifying the active components which could be used as alternative or complementary treatment for cancer. This may be of particular importance to societies and countries where modern medicine is scarce, expensive to buy, or simply unavailable.
Ganoderic acids (GAs), the triterpenoid extracts of Ganoderma lucidum mushroom (Figure 1) are potential low-cost candidates with interesting therapeutic properties. The mushroom itself has long been used in Eastern herbal medicine and is thought to increase vitality, immune function and life expectancy. Several recent studies have shown them to possess antitumor and anti-metastatic properties in a range of cancer cell types [4–6]. More than 130 GAs and related derivatives have been isolated and identified from the spores, fruiting bodies and cultured mycelia of the Ganoderma spp. in the past two decades [7–9]. GAs and derivatives have received interest due to their substantial pharmacological activities. Interestingly, a number of GAs including GA-A, GA-B, GA-H and GA-C1 showed anti-HIV-1 activity [10,11]. Other possible reported activities include: antihistamine [12], antinociceptive [13], antihypercholesterolemic [14], antiangiotensin [15] and antitumor effects [16]. This review aims to discuss the current knowledge of antitumor activities associated with G. lucidum crude extracts with particular emphasis on the anticancer apoptotic and immune restoration activities of purified GAs. Also, we will discuss our development of a novel treatment-delivery approach of GAs via nanoparticles, termed GAIN “Ganoderic Acid-Infused Nanoparticle” complex, that were particularly designed to target the malignant cells with reduced bystander effects. GAIN could also be enrobed with cancer-targeting ligands to allow more of the incorporated compound to reach the target tissue. This article will thus further highlight both chemo- and immunotherapeutic potentials of GAs in addition to the use of nanotechnology to develop antitumor treatment.
Figure 1.
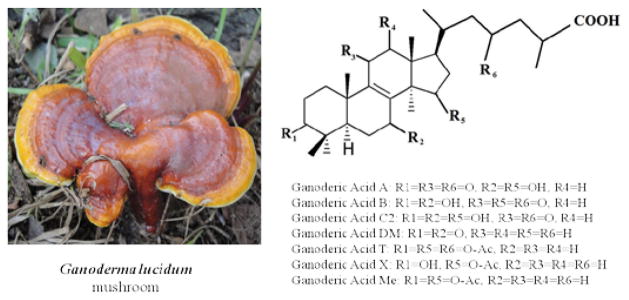
Ganoderma lucidum mushroom and the chemical structures of some well characterized Ganoderic Acids (right).
G. lucidum as a Natural Anticancer Drug Source
Ganoderma, a genus of polypore mushrooms that grows on wood, includes about 80 species, and is distributed in many tropical regions [17]. Ganoderma’s economic importance was gained as several species of the mushroom were extensively used in traditional Asian medicines due to its potential bioremediation. One species, however, G. lucidum (known as Lingzhi in China and Reishi in Japan) (Figure 1) has become one of the natural sources of numerous efficacious medicines, and is now being used to complement or sometimes substitute modern medicine in remote places of the world. In fact, the popularity of using alternative medicines has increased steadily as their prevention activity has been proven. The curative use of mushrooms has a very long tradition in the Asian countries, whereas their use in the Western hemisphere has considerably increased since the last decade [18]. Many agents derived from medicinal mushroom fruiting bodies, cultured mycelium, and/or culture filtrates exert a wide range of beneficial biological effects when tested in vitro or in vivo in animal models. Lingzhi has gained its popularity as a therapeutic mushroom and named king of herbs in China since ancient times for improving longevity, health promotion and its marked immune-modulating effects as demonstrated by an increase in T lymphocytes [19,20]. Many further investigations into the anticancer activity of G. lucidum have been carried out both in vitro and in vivo, which support its application for cancer treatment and prevention [21–23]. Although anticancer activities of G. lucidum extracts have prompted the usage of the mushroom by cancer patients, its medicinal/therapeutic value remains debatable. So far, there has been no report of human trials using G. lucidum or its extracts as anticancer agents. Thus studies focused on cytotoxic, apoptotic, antiangiogenic, and immunogenic mechanisms of crude preparation of G. lucidum and its purified GAs should be encouraged.
Recent clinical studies in cancer patients have shown that a crude G. lucidum water extract (i.e. Ganopoly) can enhance host immune function with increased activity of T cells, macrophages, and natural killer cells, although remarkable antitumor responses were not observed [24–27]. Other study, however, suggests that the cancer preventive and tumoricidal properties of G. lucidum could be ascribed to its ability to enhance the host’s immune functions, antioxidative and radical-scavenging effects, inhibition of metabolic activation and enhanced detoxification of carcinogens, and their cytotoxicity to cancer cells [28]. The major active constituents from G. lucidum extract (including polysaccharides and triterpenoinds) were also found to exert chemopreventive and tumoricidal effects through a possible modulation of signaling molecules and induction of cell-cycle arrest and apoptosis [29–32]. Other mechanisms, such as antiangiogenesis, antipromotion, and antiprogression activities were also assumed to play a role, and will be discussed in this review.
G. lucidum Bioactive Extracts
Investigations on biologically active components of the carpophores and the cultured mycelia of G. lucidum have shown that this mushroom is rich in various natural metabolites that have demonstrated both antitumor and immunomodulatory activities [33,34]. Among the most medically important constituents of the mushroom are its polysaccharides and alcohol soluble triterpenoids that also include GAs [22,35,36]. Polysaccharides represent the major water extract fraction of G. lucidum that exhibits significant antitumor effects in several tumor-bearing animals, mainly through their immuno-enhancing activity [34,37]. They are mostly high molecular weight glucans that vary in their water solubility and nature of their side chains. Researchers have found that polysaccharide-rich fractions exhibit antitumor properties in rodents mainly through the induction of cytokines such as IL-1, IL-6, IL-12, IFN-γ, TNF-α, GM-CSF, G-CSF, and M-CSF in monocytes/macrophages and T lymphocytes [34,37–39]. G. lucidum triterpenes are considered to be potential anticancer agents due to cytotoxicity against growing tumors, although much of the credit of enhancing the immune system was given to the polysaccharide-rich extract. The crude triterpenoid extracts of Ganoderma have been reported in numerous publications to significantly induce cytotoxicity and to reduce tumor growth [40–42]. Purified triterpenoids have also been shown to possess anti-invasive properties through inhibition of matrix metalloproteinase-9 (MMP-9), and reduction of NF-κB/AP-1 DNA-binding activities in PMA-induced HepG2 cells [43]. Also the inhibition of AP-1 and NF-κB was documented in highly invasive human breast cancer cells, which coincided with downregulation of Cdk4 expression and reduced secretion of uPA [44]. The anti-inflammatory and antitumor properties of purified triterpene acids and sterols were also reported by other groups [45,46], encouraging the potential use of GAs in combination therapy against inflammation and cancer.
The main focus of this review is the methanol soluble fraction of G. lucidum extract, predominantly GAs, a family of compounds that possesses a molecular structure similar to steroid hormones [46] (Figure 1). Studies suggest that GAs possess antitumor properties that seem to be related to a cytotoxic activity against cancer cells [5,47,48]. Both the antitumor and immuno-modulatory properties of G. lucidum extract, along with its low cytotoxicity, increase the possibility that it could be very effective in a complementary treatment for cancer patients receiving conventional chemotherapy and/or radiation treatment.
The potential clinical value and wide acceptability of G. lucidum extracts as alternative anticancer medication have attracted intense interest in the search for their molecular mechanisms. Studies have reported that G. lucidum extracts combine both polysaccharides and triterpenoids that collectively possess aspects of immuno-modulatory and antitumor effects [5,41] (Table 1). Yet, little work has been done on identifying the antitumor activity and immune regulation mediated by purified triterpenes in vivo. Understanding the mechanisms by which purified triterpenes exert their antitumor and immune stimulation effects would contribute to the design of alternative strategies for cancer treatment.
Table 1.
Some recent applications, observed activities and suggested mechanisms of actions for Ganoderma lucidum raw extracts (I), and its purified Ganoderic acids (II) on several types of cancer cells.
| I-Ganoderma extracts | Applications | Observed Activities | Suggested Mechanism(s) | Refs |
|---|---|---|---|---|
| Dried powder of G. lucidum (dissolved in boiled water) | Highly invasive breast cancer (MDAMB-231) and prostate cancer (PC-3) cell lines. | Downregulates transcription factors AP-1 and NF-κB in breast and prostate cancer cells. | Inhibition of uPA and uPAR reduces cell motility. | [65] |
| Dried powder of G. lucidum (13.5% polysaccharides & 6% triterpenes) | Human prostate cancer cells (PC-3), and human aortic endothelial cells (HAECs) | Inhibits early events in angiogenesis & capillary morphogenesis of HAECs, and modulates the phosphorylation of Erk1/2 & Akt kinases in PC-3 cells, potentially decreasing the activity of AP-1. | Inhibition of AP-1 down-regulates the secretion of VEGF and TGF-β1 from PC-3 cells. Suppression of angiogenesis by modulating MAPK and Akt signaling. | [66] |
| Ethanol and water extract of G. lucidum | Human urothelial cells (HUC, bladder cancer ) consisting of two cell lines (HUC-PC cells and MTC-11 cells). | Ethanol extracts show a stronger growth inhibition than those of water extracts. Induces growth arrest and reduces cell migration in vitro. | Increased actin polymerization inhibits carcinogen 4-aminobiphenyl-induced cellular migration. | [67] |
| Methanolic G. lucidum extract | 26 types of human cancer cell lines including 16 hematological cell lines (lymphomas & multiple myelomas), and 10 other solid tumor cell lines. | Exhibits cytotoxicity to HL-60 (ED50 ≥26 μg/ml), U937 (ED50 ≥63μg/ml), K562 (ED50 ≥50μg/ml), Blin-1 (ED50 ≥38μg/ml), Nalm-6 (ED50 ≥30 μg/ml) and RPMI8226 (ED50 ≥40 μg/ml). | Induction of cell cycle arrest, mitochondrial dysfunction, and upregulation of p21/p27. | [68] |
| G. lucidum polysaccharide extract | In vivo treatment of ovarian cancer in rodents. | Reduces MDA adducts by increasing activity of serum antioxidant enzymes [superoxide dismutase (SOD), catalase (CAT), glutathione peroxidase (GSH-Px)]. | Reduction of malignant growth by modulation of serum antioxidant enzymes. | [69] |
| Hot water G. lucidum extract | Drug-sensitive (H69) and multi-drug resistant (VPA) human SCLC cells. VPA was derived from H69 cells selected in etoposide. | Exhibits cytotoxicity and induces apoptosis in both drug-sensitive and drug-resistant cells. | Induction of apoptosis similar to the conventional chemotherapeutics (etoposide and doxorubicin) via DNA fragmentation and caspase activation. | [70] |
| Semi-purified G. lucidum (methanol extract) | Human leukemic cell line NB4. | Induces apoptosis in NB4 cells. | Reduction and modulation of Bcl2/Bax, p53, Akt, Erk; Inhibition of NF-κB. | [71] |
| Ethanol extract of G. lucidum (GLe) | Pre-cancerous human uroepithelial cell line (HUC-PC). | Induces apoptosis and upregulates IL-2, IL-6, and IL-8 in HUC-PC cells in a dose-dependent manner. | Enhancement of cytokine expression by p50/p65 NF-κB activity. Migration of neutrophils via upregulation of IL-8. | [72] |
| II-Ganoderic acid subtypes | Applications | Observed Activities | Suggested Mechanism(s) | Refs |
| Ganoderic acid X (GA-X) | Hepatoma cells (HuH-7), colorectal carcinoma (HCT-116), Burkitt’s lymphoma (Raji cells), acute promyelocyte leukemia (HL-60). | Inhibits topoisomerases I and IIa in vitro, resulting in immediate inhibition of DNA synthesis as well as activation of ERK and JNK mitogen-activated protein kinases. | Induction of apoptosis with degradation of chromosomal DNA; decreased levels of Bcl-xL, disruption of mitochondrial membrane, release of cytochrome c and activation of caspase-3. | [73] |
| Ganoderic acid T (GA-T) | Human metastatic lung tumor (95-D), liver tumor (SMMC7721), epidermal cancer (KB-A-1&KB-3-1), cervical cancer (HeLa), melanoma (A375), normal lung (HLF), embryonic liver (L-02), kidney (HEK293), and colon carcinoma (Ls174t) cell lines. | Induces cytotoxicity to cancer cells, but less toxic to normal cells. Induces cell cycle arrest at G1 phase. Suppresses MMP-2 and MMP-9 gene expression through the inhibition of NF-κB activation. | Reduction of mitochondrial membrane potential (Δψm), release of cytochrome c and apoptotic activity in lung cancer cells. Induction of p53 and Bax, which stimulates the activity of caspase-3 but not caspase-8. | [50, 74] |
| Ganoderic acid ME (GA-Me) | In vivo Lewis lung carcinoma in C57BL/6 mice, human colon carcinoma cells (HCT-116), MDR human colorectal carcinoma cell lines, and metastatic lung carcinoma (95-D), p53-null lung cancer (H1299), HCT-116 p53+/+ and HCT-116 p53 −/− colon cancer cells. | Inhibits tumor growth and lung metastasis in rodents (28 mg/kg i.p.), increases NK activity with upregulation of NF-κB. Kills cancer cells via p53 and mitochondria-mediated apoptosis. Reverses multidrug resistance of HCT-116 cells enhancing chemosensitivity to anticancer agents. | Induction of cell cycle arrest. Induction of apoptosis in MDR cells via upregulation of p-p53, p53, Bax, caspases-3/9 with downregulation of Bcl-2. Upregulation of IL-2 and IFN-γ in vivo. | [54, 55, 75, 76] |
GAs in Apoptosis and Immune Activation
GAs have shown a wide range of medicinal benefits, most notably their potent toxicity to tumor cells with a comparatively limited toxicity to bystander cells (Table 1). It has been reported that GA-X inhibits topoisomerases and sensitizes the cancer cells toward apoptosis [49]. The in vitro treatment of human hepatoma HuH-7 cells causes immediate inhibition of DNA synthesis as well as activation of ERK and JNK, and induction of apoptosis. The observed molecular events include: degradation of chromosomal DNA, decreased levels of Bcl-xL, disruption of mitochondrial membrane potential, cytosolic release of cytochrome c and activation of caspase-3. The involvement of mitochondrial dysfunction was also supported by a later work [50], in which GA-T induced apoptosis of metastatic lung tumor cells through the intrinsic pathway mediated via the mitochondria-dependent caspase pathway and p53 expression. This study also detected the exposure of p53 and Bax proteins in 95-D cells, while the expression of Bcl-2 was not significantly changed. In vivo study also showed that GA-T suppressed the growth of human solid tumors in athymic mice. In addition to its antiproliferative effects, recent studies have found that GA-T effectively inhibits cancer cell invasion and metastasis both in vitro and in vivo [51]. This study also showed that GA-T promoted aggregation and simultaneously inhibited adhesion to the extracellular matrix, thus impairing the migration of colon (HCT-116) and lung (95-D) cancer cells in a dose- and time-dependent manner. Strikingly, GA-T treatment inhibits the nuclear translocation of NF-κB and the degradation of inhibitor of κB-α (IκB-α), which ultimately led to a decrease of MMP-9, inducible nitric oxide synthase (iNOS), and urokinase-type plasminogen activator (uPA). Furthermore, in vivo administration demonstrated that GA-T suppresses tumor growth and metastasis, and down-regulates MMP-2 and MMP-9 mRNA expression in a Lewis Lung Carcinoma (LLC) model in vivo.
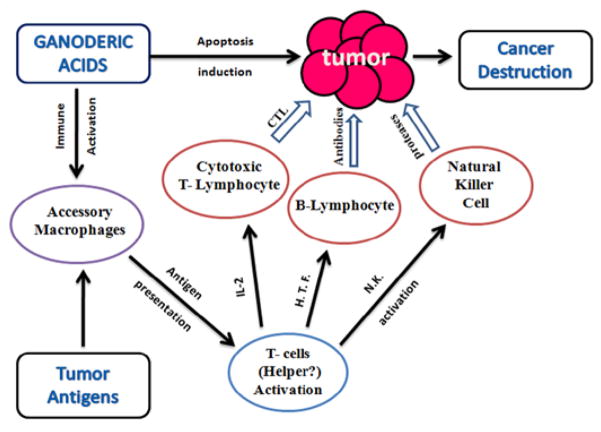
Recently, it has been found that p53 plays an important role in the suppression and anti-invasion properties of GA-T in human colon cancer (HCT-116) cell lines [52]. Comparing the results in HCT-116 p53(+/+) and p53(−/−), it is suggested that p53 could modify GAT-mediated inhibition of NF-κB translocation, degradation of IκBα, and downregulation of uPA, MMP-2/9 and iNOS/NOS2 protein expression. A recent study has also demonstrated that GA-Mf as well as GA-S induces apoptosis of human HeLa cells through a mitochondria-mediated pathway [53]. Both GA isomers showed inhibition of cellular growth in various human carcinoma cell lines. GA-S was also shown to cause cell cycle arrest in the S phase, while GA-Mf caused cell cycle arrest in the G1 phase. Treatment of HeLa cells with these GAs resulted in a decreased mitochondrial membrane potential and the release of cytochrome c from mitochondria into the cytosol. Caspase-3 and caspase-9 activities were also observed with a sharp decrease in the Bcl-2/Bax ratio as recorded in GA-treated HeLa cells. Figure 2 depicts the possible anticancer activity of GAs.
Figure 2.
Schematic diagram indicating the plausible anticancer activity of Ganoderic Acids.
The potential use of GAs as a complementary anticancer therapy also depends on their effectiveness against multidrug resistant cancer cells. In this direction, GA-Me has been shown to reverse the multidrug resistance (MDR) in multidrug resistant colon cancer cells by inducing apoptosis via upregulation of p-p53, p53, Bax, caspase-3, caspase-9 and downregulation of Bcl-2 [54]. In addition, GA-Me treatment can stimulate the decline in mitochondrial membrane potential and release of cytochrome c into the cytosol [54]. Beside its apoptotic effects, GA-Me has been reported to effectively inhibit tumor growth and lung metastasis of Lewis lung carcinoma in C57BL/6 mice through enhanced immune function [55]. Administration of GA-Me (28 mg/kg) resulted in a significant increase in NK cell activity and the production of IL-2 and IFN-γ, possibly through an upregulation of NF-κB. Multiple roles of GA’s antitumor activities are depicted in Figure 2. Our group has found that purified GA-A has a profound apoptotic effect on B-cell lymphoma cell lines with minimal toxicity on non-malignant B-cells. Treatments with GA-A caused mitochondrial dysfunction, identified by the release of cytochrome c into the cytosolic compartment, caspase 3, and 9 activities, and overexpression of Bax (unpublished data). We also found that GA-A-treated B-cell lymphoma express elevated levels of HLA class II proteins with an increased antigen presenting capacity to stimulate T cells in vitro (unpublished data). However, the mechanisms by which GA-A induces immune activation and tumor killing in vivo remains unclear. Table 1 summarizes some recent investigations on GAs antitumor activities, their application, and suggested mechanism(s) of actions.
Ganoderic Acid-Infused Nanoparticles (GAIN)
It has been reported that most anticancer drugs have limited selectivity [56], hence the levels of drug required to kill a sufficient number of tumor cells to achieve and maintain a state of complete remission in patients causes significant toxicity towards actively proliferating nonmalignant cells, such as normal cells of the gastrointestinal tract and bone marrow. Many of the curative properties of conventional treatments can be improved through the use of targeted drug delivery systems [57], which include the use of nontoxic, biodegradable particulate carriers, composed primarily of lipids and/or polymer nanoparticles, and their associated therapeutics [58–61]. This new delivery system is designed to alter the pharmacokinetics and biodistribution of the associated drug, or to function as drug reservoirs (i.e., sustained release), in addition to their advantage in stabilizing the drug and preventing its premature metabolic breakdown.
Nanoparticle approaches to targeted drug delivery for malignant tumors offer new opportunity to improve patient care and quality of life by reducing off-target toxicities. Development of targeted nanoparticles ensures delivery of chemotherapeutics directly to cancer cells, followed by their slow release in potentially sustainable levels that may provide superior efficacy and lower toxicity for treating primary or advanced metastatic tumors. Our recent studies suggest that a combinatorial approach using the co-encapsulation of a lipophilic near infrared (NIR) dye and an anticancer drug within hydrophobic pockets in the polymeric matrix of poly acrylic acid (PAA)-coated IONPs (PAA-IONPs) could be employed for combined optical imaging, magnetic resonance imaging (MRI) detection, and targeted cancer therapy [58]. Our study suggests that a natural triterpenoid such as GA-A can be readily entrapped with a high degree of latency within its hydrophobic pockets, remain associated for appropriate lengths of time and be released at an appropriate rate, with sustained levels of drug in the tumor cells [62].
GA-A-carrying nanoparticles could also be designed to deliver the drug to the cancer cells, allowing targeted cancer treatment without harming healthy cells. For example, receptor-mediated cellular uptake of nanoparticles could be achieved by attaching a vitamin derivative such as folic acid to these particles. Folic acid is an effective targeting agent for the folate receptor which is believed to be overexpressed in many human tumor cells [63,64]. In this scenario, cancer cells may consume high amounts of folic acids and ensure that nanoparticles preferentially accumulate at the tumor site before releasing their drugs (Figure 3). Studies performed by our group suggest that nanoparticles can also carry a fluorescent dye and an iron oxide magnetic core [58,59], thus their locations within the cells and the body could be seen by optical imaging and MRI, allowing a physician to see how the tumor is responding to the treatment. Our study also suggests that the nanoparticles could be engineered without the drug for their use as imaging (contrast) agents for detection of cancer [58]. If there is no cancer, the biodegradable nanoparticles may not bind to the tissue allowing their elimination by the liver cells. Ultimately, high concentration of GAIN accumulated at the tumor site may spare exposing the body to the side-effects of chemotherapy, while having larger doses of drugs to target cancer cells.
Figure 3.
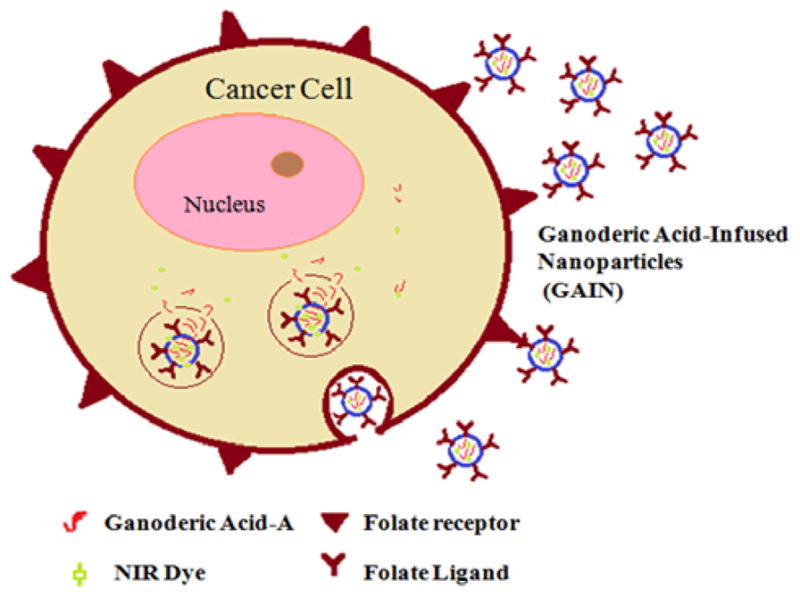
Schematic diagram depicting ligand-targeted accumulation of Ganoderic Acid-Infused Nanoparticles (GAIN) with both diagnostic and therapeutic functions. Both GA-A and imaging-dye are conjugated to a biocompatible polymer that bonded to a folate ligand to trigger internalization. GAIN preferentially target the folate receptor-rich cancer cells, where linkages are hydrolyzed and the nanoparticles release the drug and dye, allowing drug delivery as well as imaging of tumor tissue.
Conclusions
Exploring the scientific basis among known cures used in folk medicines has resulted in purifying potential natural products that could combat many diseases, particularly cancer. Hence, further examination of the anticancer relevance of these products may relieve the economic burden associated with the management of cancer, especially in societies where modern medicine is scarce, or expensive to buy or even unavailable. One valuable resource of those medicinal products is the fruiting body of Ganoderma lucidum, a wild mushroom that grows on logs, decaying wood, and tree stumps in Asia and surrounding regions, and which has been used for thousands of years in herbal remedies to promote human immune function. Given that the development of tumor is aided by immune evasion, current literature suggests GAs possess both apoptotic and immune restoration properties. Our study suggests that GAs are unique natural candidates which could be used to enhance the cellular expression of immune components as well as antigen processing and presentation. The above mentioned properties of GAs make them ideal candidates for potential use in complementary chemo-immunotherapeutics. In this direction, we are currently developing a new GAs treatment-delivery system termed GAIN by utilizing nanotechnology to develop an antitumor treatment strategy that will allow cancer targeting. GAIN is enrobed in cancer-targeting protein ligands to allow more of the incorporated compound to reach the target tissue and greatly diminish any toxic side effects associated with using higher doses. Collectively, this review suggests that enhanced targeting resulting from nanoparticle delivery, coupled with the reduced bystander toxicity of natural products such as GAs will pave the way for potential treatments of human malignancies.
Acknowledgments
This work was supported by grants from the National Institutes of Health (CA129560) to A. Haque. We thank Dr. Jason God for critical reading of the manuscript.
Footnotes
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
- 1.American Cancer Society. Global Cancer Facts & Figures. 2. American Cancer Society; Atlanta, GA: 2011. [Google Scholar]
- 2.Kerr JF, Winterford CM, Harmon BV. Apoptosis. Its significance in cancer and cancer therapy. Cancer. 1994;73:2013–2026. doi: 10.1002/1097-0142(19940415)73:8<2013::aid-cncr2820730802>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 3.Economist Intelligence Unit Limited. Breakaway: The global burden of cancer—challenges and opportunities; A report from the Economist Intelligence Unit. 2009. [Google Scholar]
- 4.Chang ST, Buswell JA, Karst P. Ganoderma lucidum (Curt.:Fr.). (Aphyllophoromycetideae) - A mushrooming medicinal mushroom. Intl J Med Mushrooms. 1999;1:139–146. [Google Scholar]
- 5.Sliva D. Ganoderma lucidum (Reishi) in cancer treatment. Integr Cancer Ther. 2003;2:358–364. doi: 10.1177/1534735403259066. [DOI] [PubMed] [Google Scholar]
- 6.Müller CI, Kumagai T, O’Kelly J, Seeram NP, Heber D, Koeffler HP. Ganoderma lucidum causes apoptosis in leukemia, lymphoma and multiple myeloma cells. Leuk Res. 2006;30:841–848. doi: 10.1016/j.leukres.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 7.Chen RY, Yu DQ. Development of triterpenes from Ganoderma lucidum. Acta Pharmaceutica Sinica. 1990;25:940–953. [PubMed] [Google Scholar]
- 8.Luo J, Lin ZB. Advances of pharmacological effects of triterpenes from Ganoderma lucidum. Yao Xue Xue Bao. 2002;37:574–578. [PubMed] [Google Scholar]
- 9.Keypour S, Rafati H, Riahi H, Mirzajani F, Moradali M. Qualitative analysis of ganoderic acids in Ganoderma lucidum from Iran and China by RP-HPLC and electrospray ionisation-mass spectrometry (ESI-MS) Food Chem. 2010;119:1704–1708. [Google Scholar]
- 10.El-Mekkawy S, Meselhy MR, Nakamura N, Tezuka Y, Hattori M, et al. Anti-HIV-1 and anti-HIV-1-protease substances from Ganoderma lucidum. Phytochemistry. 1998;49:1651–1657. doi: 10.1016/s0031-9422(98)00254-4. [DOI] [PubMed] [Google Scholar]
- 11.Min BS, Nakamura N, Miyashiro H, Bae KW, Hattori M. Teriterpens from the spores of Ganoderma lucidum and their inhibitory activity against HIV-1 protease. Chem Pharm Bull. 1998;46:1607–1612. doi: 10.1248/cpb.46.1607. [DOI] [PubMed] [Google Scholar]
- 12.Kohda H, Tokumoto W, Sakamoto K, Fujii M, Hirati Y, et al. The biologically active constituents of Ganoderma lucidum (FR.) KARST. Histamine Release-Inhibitory Triterpenes. Chem Pharm Bull (Tokyo) 1985;33:1367–1374. doi: 10.1248/cpb.33.1367. [DOI] [PubMed] [Google Scholar]
- 13.Koyama K, Imaizumi T, Akiba M, Kinoshita K, Takahashi K, et al. Antinociceptive components of Ganoderma lucidum. Planta Med. 1997;63:224–227. doi: 10.1055/s-2006-957658. [DOI] [PubMed] [Google Scholar]
- 14.Komoda Y, Shimizu M, Sonoda Y, Sato Y. Ganoderic acid and its derivatives as cholesterol synthesis inhibitors. Chem Pharm Bull. 1989;37:531–533. doi: 10.1248/cpb.37.531. [DOI] [PubMed] [Google Scholar]
- 15.Morigiwa A, Kitabatake K, Fujimoto Y, Ikekawa N. Angiotensin converting enzyme-Inhibitory triterpens from Ganoderma lucidum. Chem Pharm Bull. 1986;34:3025–3028. doi: 10.1248/cpb.34.3025. [DOI] [PubMed] [Google Scholar]
- 16.Lindequist U, Niedermeyer TMJ, Jülich WD. The pharmacological potential of mushrooms. Evid Based Complement Alternat Med. 2005;2:285–299. doi: 10.1093/ecam/neh107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kirk PM, Cannon PF, Minter DW, Stalpers JA. Dictionary of the Fungi. 10. Wallingford: CABI; 2008. p. 272. [Google Scholar]
- 18.Smith J, Rowan N, Sullivan R. Medicinal Mushrooms: a Rapidly Developing Area of Biotechnology for Cancer Therapy and Other Bioactivities. Biotechnol Lett. 2002;24:1839–1845. [Google Scholar]
- 19.Cong Z, Lin ZB. The pharmacological study of Lingzhi (Ganoderma lucidum) and the research of therapeutical principle of “Fuzhengguben” in Traditional Chinese medicine. J Beijing Med Coll. 1981;13:6–10. [Google Scholar]
- 20.Wang SY, Hsu ML, Hsu HC, Tzeng CH, Lee SS, et al. The anti-tumor effect of Ganoderma lucidum is mediated by cytokines released from activated macrophages and T lymphocytes. Int J Cancer. 1997;70:699–705. doi: 10.1002/(sici)1097-0215(19970317)70:6<699::aid-ijc12>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 21.Hong KJ, Dunn DM, Shen CL, Pence BC. Effects of Ganoderma lucidum on apoptotic and anti-inflammatory function in HT-29 human colonic carcinoma cells. Phytother Res. 2004;18:768–770. doi: 10.1002/ptr.1495. [DOI] [PubMed] [Google Scholar]
- 22.Boh B, Berovic M, Zhang J, Zhi-Bin L. Ganoderma lucidum and its pharmaceutically active compounds. Biotechnol Annu Rev. 2007;13:265–301. doi: 10.1016/S1387-2656(07)13010-6. [DOI] [PubMed] [Google Scholar]
- 23.Lin SB, Li CH, Lee SS, Kan LS. Triterpene-enriched extracts from Ganoderma lucidum inhibit growth of hepatoma cells via suppressing protein kinase C, activating mitogen-activated protein kinases and G2-phase cell cycle arrest. Life Sci. 2003;72:2381–2390. doi: 10.1016/s0024-3205(03)00124-3. [DOI] [PubMed] [Google Scholar]
- 24.Gao Y, Gao H, Chan E, Tang W, Xu A, et al. Antitumor activity and underlying mechanisms of ganopoly, the refined polysaccharides extracted from Ganoderma lucidum, in mice. Immunol Invest. 2005;34:171–198. [PubMed] [Google Scholar]
- 25.Zhang J, Tang Q, Zhou C, Jia W, Da Silva L, et al. GLIS, a bioactive proteoglycan fraction from Ganoderma lucidum, displays anti-tumour activity by increasing both humoral and cellular immune response. Life Sci. 2010;87:628–637. doi: 10.1016/j.lfs.2010.09.026. [DOI] [PubMed] [Google Scholar]
- 26.Lin ZB. Cellular and molecular mechanisms of immuno-modulation by Ganoderma lucidum. J Pharmacol Sci. 2005;99:144–153. doi: 10.1254/jphs.crj05008x. [DOI] [PubMed] [Google Scholar]
- 27.Lin ZB, Zhang HN. Anti-tumor and immunoregulatory activities of Ganoderma lucidum and its possible mechanisms. Acta Pharmacol Sin. 2004;25:1387–1395. [PubMed] [Google Scholar]
- 28.Weng CJ, Yen GC. The in vitro and in vivo experimental evidences disclose the chemopreventive effects of Ganoderma lucidum on cancer invasion and metastasis. Clin Exp Metastasis. 2010;27:361–369. doi: 10.1007/s10585-010-9334-z. [DOI] [PubMed] [Google Scholar]
- 29.Kim HS, Kacew S, Lee BM. In vitro chemopreventive effects of plant polysaccharides (Aloe barbadensis miller, Lentinus edodes, Ganoderma lucidum and Coriolus versicolor) Carcinogenesis. 1999;20:1637–1640. doi: 10.1093/carcin/20.8.1637. [DOI] [PubMed] [Google Scholar]
- 30.Yuen JW, Gohel MD. The dual roles of Ganoderma antioxidants on urothelial cell DNA under carcinogenic attack. J Ethnopharmaco. 2008;118:324–330. doi: 10.1016/j.jep.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 31.Zhu M, Chang Q, Wong LK, Chong FS, Li RC. Triterpene antioxidants from Ganoderma lucidum. Phytother Res. 1999;13:529–531. doi: 10.1002/(sici)1099-1573(199909)13:6<529::aid-ptr481>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 32.Thyagarajan A, Jiang J, Hopf A, Adamec J, Sliva D. Inhibition of oxidative stress-induced invasiveness of cancer cells by Ganoderma lucidum is mediated through the suppression of interleukin-8 secretion. Int J Mol Med. 2006;18:657–664. [PubMed] [Google Scholar]
- 33.Chan WK, Law HK, Lin ZB, Lau YL, Chan GC. Response of human dendritic cells to different immunomodulatory polysaccharides derived from mushroom and barley. Int Immunol. 2007;19:891–899. doi: 10.1093/intimm/dxm061. [DOI] [PubMed] [Google Scholar]
- 34.Chen HS, Tsai YF, Lin S, Lin CC, Khoo KH, et al. Studies on the immuno-modulating and anti-tumor activities of Ganoderma lucidum (Reishi) polysaccharides. Bioorg Med Chem. 2004;12:5595–5601. doi: 10.1016/j.bmc.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 35.Shiao MS. Natural products of the medicinal fungus Ganoderma lucidum: occurrence, biological activities, and pharmacological functions. Chem Rec. 2003;3:172–180. doi: 10.1002/tcr.10058. [DOI] [PubMed] [Google Scholar]
- 36.Paterson RR. Ganoderma-a therapeutic fungal biofactory. Phytochemistry. 2006;67:1985–2001. doi: 10.1016/j.phytochem.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 37.Zhu XL, Chen AF, Lin ZB. Ganoderma lucidum polysaccharides enhance the function of immunological effector cells in immunosuppressed mice. J Ethnopharm. 2007;111:219–226. doi: 10.1016/j.jep.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 38.Cao QZ, Lin ZB. Antitumor and anti-angiogenic activity of Ganoderma lucidum polysaccharides peptide. Acta Pharmacol Sin. 2004;25:833–838. [PubMed] [Google Scholar]
- 39.Li WD, Zhang BD, Wei R, Liu JH, Lin ZB. Reversal effect of Ganoderma lucidum polysaccharide on multidrug resistance in K562/ADM cell line. Acta Pharmacol Sin. 2008;29:620–627. doi: 10.1111/j.1745-7254.2008.00776.x. [DOI] [PubMed] [Google Scholar]
- 40.Huie WC, Di X. Chromatographic and electrophoretic methods for Lingzhi pharmacologically active components. J Chromatog B. 2004;812:241–257. doi: 10.1016/j.jchromb.2004.08.038. [DOI] [PubMed] [Google Scholar]
- 41.Yuen JM, Gohel MD. Anticancer Effects of Ganoderma lucidum: A Review of Scientific Evidence. Nutr Cancer. 2005;53:11–17. doi: 10.1207/s15327914nc5301_2. [DOI] [PubMed] [Google Scholar]
- 42.Chen RY, Yu DQ. Studies on the triterpenoid constituents of the spores of Ganoderma lucidum, (Curt. Fr.) P. (Karst) Intl J Med Mushrooms. 1999;1:147–152. [Google Scholar]
- 43.Weng CJ, Chau CF, Hsieh YS, Yang SF, Yen GC. Lucidenic acid inhibits PMA induced invasion of human hepatoma cells through inactivating MAPK/ERK signal transduction pathway reducing binding activities of NF-kappaB and AP-1. Carcinogenesis. 2008;29:147–156. doi: 10.1093/carcin/bgm261. [DOI] [PubMed] [Google Scholar]
- 44.Jiang J, Grieb B, Thyagarajan A, Sliva D. Ganoderic acids suppress growth and invasive behavior of breast cancer cells by modulating AP-1 and NF-kappaB signaling. Int J Mol Med. 2008;21:577–584. [PubMed] [Google Scholar]
- 45.Akihisa T, Nakamura Y, Tagata M, Tokuda H, Yasukawa K, et al. Anti-inflammatory and anti-tumor-promoting effects of triterpene acids and sterols from the fungus Ganoderma lucidum. Chem Biodivers. 2007;4:224–231. doi: 10.1002/cbdv.200790027. [DOI] [PubMed] [Google Scholar]
- 46.Dudhgaonkar S, Thyagarajan A, Sliva D. Suppression of the inflammatory response by triterpenes isolated from the mushroom Ganoderma lucidum. Int Immunopharmacol. 2009;9:1272–1280. doi: 10.1016/j.intimp.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 47.Li C, Li Y, Sun HH. New ganoderic acids, bioactive triterpenoid metabolites from the mushroom Ganoderma lucidum. Nat Prod Res. 2006;20:985–991. doi: 10.1080/14786410600921466. [DOI] [PubMed] [Google Scholar]
- 48.Yue QX, Song XY, Ma C, Feng LX, Guan SH, et al. Effects of triterpenes from Ganoderma lucidum on protein expression profile of HeLa cells. Phytomedicine. 2010;17:606–613. doi: 10.1016/j.phymed.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 49.Li CH, Chen PY, Chang UM, Kan LS, Fang WH, et al. Ganoderic acid X, a lanostanoid triterpene, inhibits topoisomerases and induces apoptosis of cancer cells. Life Sci. 2005;77:252–265. doi: 10.1016/j.lfs.2004.09.045. [DOI] [PubMed] [Google Scholar]
- 50.Tang W, Liu JW, Zhao WM, Wei DZ, Zhong JJ. Ganoderic acid T from Ganoderma lucidum mycelia induces mitochondria mediated apoptosis in lung cancer cells. Life Sci. 2006;80:205–211. doi: 10.1016/j.lfs.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 51.Chen NH, Liu JW, Zhong JJ. Ganoderic acid T inhibits tumor invasion in vitro and in vivo through inhibition of MMP expression. Pharmacol Rep. 2010;62:150–163. doi: 10.1016/s1734-1140(10)70252-8. [DOI] [PubMed] [Google Scholar]
- 52.Chen NH, Zhong JJ. p53 is important for the anti-invasion of ganoderic acid T in human carcinoma cells. Phytomedicine. 2011;18:719–725. doi: 10.1016/j.phymed.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 53.Liu RM, Zhong JJ. Ganoderic acid Mf and S induce mitochondria mediated apoptosis in human cervical carcinoma HeLa cells. Phytomedicine. 2011;18:349–355. doi: 10.1016/j.phymed.2010.08.019. [DOI] [PubMed] [Google Scholar]
- 54.Jiang Z, Jin T, Gao F, Liu J, Zhong J, Zhao H. Effects of Ganoderic acid Me on inhibiting multidrug resistance and inducing apoptosis in multidrug resistant colon cancer cells. Process Biochem. 2011;46:1307–1314. [Google Scholar]
- 55.Wang G, Zhao J, Liu J, Huang Y, Zhong JJ, Tang W. Enhancement of IL-2 and IFN-gamma expression and NK cells activity involved in the anti-tumor effect of Ganoderic acid Me in vivo. Int Immunopharmacol. 2007;7:864–870. doi: 10.1016/j.intimp.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 56.Brannon-Peppas L, Blanchette JO. Nanoparticle and targeted systems for cancer therapy. Adv Drug Deliv Rev. 2004;56:1649–1659. doi: 10.1016/j.addr.2004.02.014. [DOI] [PubMed] [Google Scholar]
- 57.Allen TM, Cullis PR. Drug Delivery Systems: Entering the Mainstream. Science. 2010;303:1818–1822. doi: 10.1126/science.1095833. [DOI] [PubMed] [Google Scholar]
- 58.Santra S, Kaittanis C, Grimm J, Perez JM. Drug/dye-loaded, multifunctional iron oxide nanoparticles for combined targeted cancer therapy and dual optical/MR-imaging. Small. 2009;5:1862–1868. doi: 10.1002/smll.200900389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.McCarthy JR, Perez JM, Brückner C, Weissleder R. Polymeric nanoparticle preparation that eradicates tumors. Nano Lett. 2005;5:2552–2556. doi: 10.1021/nl0519229. [DOI] [PubMed] [Google Scholar]
- 60.Perez JM. Iron oxide nanoparticles: hidden talent. Nat Nanotechnol. 2007;2:535–536. doi: 10.1038/nnano.2007.282. [DOI] [PubMed] [Google Scholar]
- 61.Santra S, Kaittanis C, Perez JM. Cytochrome C encapsulating theranostic nanoparticles: a novel bifunctional system for targeted delivery of therapeutic membrane-impermeable proteins to tumors and imaging of cancer therapy. Mol Pharm. 2010;7:1209–1222. doi: 10.1021/mp100043h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Johnson B, Doonan B, Radwan FF, Haque A. Ganoderic Acid DM: An Alternative Agent for the Treatment of Advanced Prostate Cancer. Open Prost Cancer J. 2010;3:78–85. doi: 10.2174/1876822901003010078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sudimack J, Lee RJ. Targeted drug delivery via the folate receptor. Adv Drug Deliv Rev. 2000;41:147–162. doi: 10.1016/s0169-409x(99)00062-9. [DOI] [PubMed] [Google Scholar]
- 64.Low PS, Henne WA, Doorneweerd DD. Discovery and development of folic-acid-based receptor targeting for imaging and therapy of cancer and inflammatory diseases. Acc Chem Res. 2008;41:120–129. doi: 10.1021/ar7000815. [DOI] [PubMed] [Google Scholar]
- 65.Sliva D, Labarrere C, Slivova V, Sedlak M, Lloyd FP, HON Ganoderma lucidum suppresses motility of highly invasive breast and prostate cancer cells. Biochem Biophys Res Commun. 2002;298:603–612. doi: 10.1016/s0006-291x(02)02496-8. [DOI] [PubMed] [Google Scholar]
- 66.Stanley G, Harvey K, Slivova V, Jiang J, Sliva D. Ganoderma lucidum suppresses angiogenesis through the inhibition of secretion of VEGF and TGF-b1 from prostate cancer cells. Biochem Biophys Res Commun. 2005;330:46–52. doi: 10.1016/j.bbrc.2005.02.116. [DOI] [PubMed] [Google Scholar]
- 67.Lu QY, Jin YS, Zhang Q, Zhang Z, Heber D, et al. Ganoderma lucidum extracts inhibit growth and induce actin polymerization in bladder cancer cells in vitro. Cancer Lett. 2004;216:9–20. doi: 10.1016/j.canlet.2004.06.022. [DOI] [PubMed] [Google Scholar]
- 68.Müller CI, Kumagai T, O’Kelly J, Seeram NP, Heber D, et al. Ganoderma lucidum causes apoptosis in leukemia, lymphoma and multiple myeloma cells. Leuk Res. 2006;30:841–848. doi: 10.1016/j.leukres.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 69.YouGuo C, Zong S, XiaoPing C. Modulatory effect of Ganoderma lucidum polysaccharides on serum antioxidant enzymes activities in ovarian cancer rats. Carbohydr Polymer. 2009;78:258–262. [Google Scholar]
- 70.Sadavs D, Still DW, Mudry RR, Kane SE. Effect of Ganoderma on drug-sensitive and multidrug-resistant small-cell lung carcinoma cells. Cancer Lett. 2009;277:182–189. doi: 10.1016/j.canlet.2008.12.009. [DOI] [PubMed] [Google Scholar]
- 71.Calvino E, Manjon JL, Sancho P, Tejedor MC, Herráez A, et al. Ganoderma lucidum induced apoptosis in NB4 human leukemia cells: Involvement of Akt and Erk. J Ethnopharmacol. 2010;128:71–78. doi: 10.1016/j.jep.2009.12.027. [DOI] [PubMed] [Google Scholar]
- 72.Yuen JW, Gohel MD, Ng CF. The differential immunological activities of Ganoderma lucidum on human pre-cancerous uroepithelial cells. J Ethnopharmacol. 2011;135:711–718. doi: 10.1016/j.jep.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 73.Li CH, Chen PY, Chang UM, Kan LS, Fang WH, et al. Ganoderic acid X, a lanostanoid triterpene, inhibits topoisomerases and induces apoptosis of cancer cells. Life Sci. 2005;77:252–265. doi: 10.1016/j.lfs.2004.09.045. [DOI] [PubMed] [Google Scholar]
- 74.Xu K, Liang X, Gao F, Zhong J, Liu J. Antimetastatic effect of ganoderic acid T in vitro through inhibition of cancer cell invasion. Process Biochem. 2010;45:1261–1267. [Google Scholar]
- 75.Chen NH, Zhong JJ. Ganoderic acid Me induces G1 arrest in wild-type p53 human tumor cells while G1/S transition arrest in p53-null cells. Process Biochem. 2009;44:928–933. [Google Scholar]
- 76.Zhoua L, Shia P, Chena NH, Zhongb JJ. Ganoderic acid Me induces apoptosis through mitochondria dysfunctions in human colon carcinoma cells. Process Biochem. 2011;46:219–225. [Google Scholar]