Abstract
Background
The implementation on July 1, 2011, of new Accreditation Council for Graduate Medical Education (ACGME) standards for resident supervision and duty hours has prompted considerable debate about the potential positive and negative effects of these changes on patient care and resident education. A recent large-sample study analyzed resident responses to these changes, using a Likert scale response. In this same study, 874 residents also provided free-text comments, which provide added insight into resident perspectives on duty hours and supervision.
Methods
A mixed-methods quantitative and qualitative survey of residents was conducted in August 2010 to assess resident perceptions of the proposed ACGME regulations. Common concerns in the residents' free responses were synthesized and quantified using content analysis, a common method for qualitative research.
Results
A total of 11 617 residents received the survey. Completed surveys were received from 2561 residents (22.0%), with 874 residents (34.1%) providing free-text responses. Most residents (83.0%) expressed unfavorable opinions about the new standards. The most frequently cited concerns included coverage issues, and a negative impact on patient care and education, as well as lack of preparation for senior roles. A smaller portion of residents commented they thought the standards would contribute to improvements in quality of life (36.1%) and patient care (4.9%).
Conclusions
ACGME standards are important for graduate medical education, and their aim is to promote high-quality education and better care to patients in teaching institutions. Yet, many residents are concerned about the day-to-day impact of the 2011 regulations, in particular the 16-hour duty period for interns. Most residents who provided free-text responses had a negative impression of the new ACGME regulations. Residents' resistance to duty hour changes may represent a realization that residents are losing a central role in patient care. The concerns identified in this study demonstrate important issues for administrators and policymakers. Resident ideas and opinions should be considered in future revisions of ACGME requirements.
What was known
The 2011 ACGME duty hour standards have prompted a variety of reactions from program directors, faculty, and residents.
What is new
The majority of residents responding to a survey about the ACGME duty hour standards had a negative reaction to the standards, citing problems with the 16-hour limit for interns, coverage issues, negative impact on patient care, and reduced preparedness for senior resident roles and practice.
Limitations
Opinion survey; a low response rate may have introduced sampling bias with individuals with a strong opinion most likely to respond.
Bottom line
Many residents are concerned with the impact of the 2011 duty hour standards. Their perspective should be considered in future refinements of the standards.
Introduction
On July 1, 2011, teaching hospitals faced new Accreditation Council for Graduate Medical Education (ACGME) requirements for duty hours and supervision. The aim of the new standards was to improve the safety and quality of patient care while promoting a healthy educational environment.1 The changes reflect growing concern regarding long duty hours and fatigue, which are thought to have a negative impact on performance.2,3 These are accompanied by a perceived need for greater supervision of trainees, with an emphasis on progressive independence. The most dramatic changes in the 2011 ACGME Common Program Requirements are directed at postgraduate year 1 (PGY-1) residents (interns), who may not exceed a 16-hour duty period—eliminating the traditional overnight (24-hour) in-house call—and who must have a more senior resident or attending physician immediately available (in-house) for supervision at all times. Given interns' prior share of responsibility in patient care and administrative tasks, these new regulations have had a significant impact on graduate medical education and the health care system.
The approval of the new requirements in September 2010 received considerable attention in the medical community and the media. Numerous surveys found that program directors and residents had mixed feelings about the changes,4–11 whereas a national poll of the American public found more support for limited duty hours.12
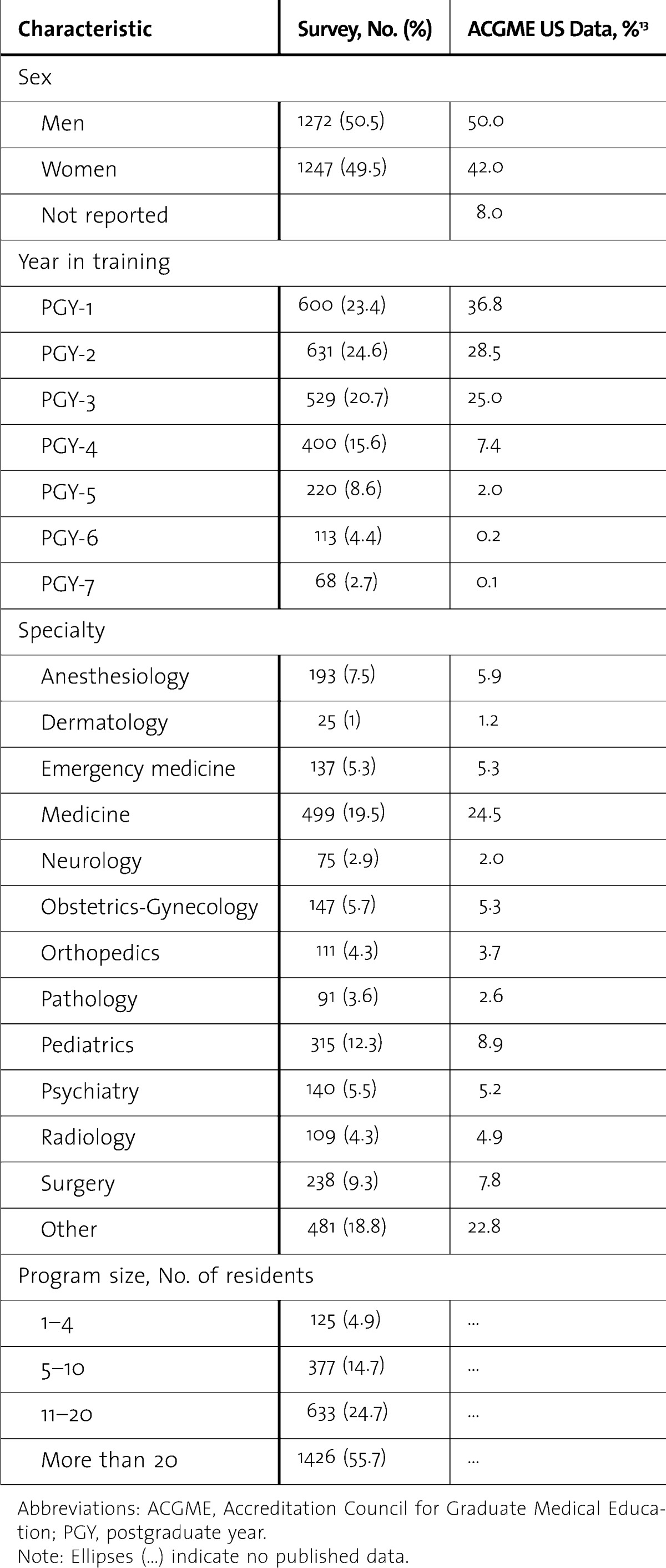
We previously published the quantitative results from a large national survey (n = 2561) on resident perspectives on the new standards.5 In this large, demographically representative sample of US residents (table 1), we found both positive and negative reactions to the regulations. Although most residents predicted an improvement in quality of life, there was nearly equal concern regarding the potential negative impact on quality of patient care, education, and preparation for more senior resident responsibilities and for practice.5 In addition to collecting statistical information, the original survey included a free-text response option that gave residents a unique opportunity to voice opinions and suggestions.
TABLE 1.
Demographic Data of Respondents and Comparative Data on US Residents From Drolet et al5
Responses from 874 residents (34.1%) included free text, collectively providing more than 100 pages of subjective comments that highlight many previously unaddressed concerns. The data are unique and independent of the quantitative results previously published.5 In the present study we apply a structured analysis to the narrative comments to offer added insight into residents' perspectives on important factors in graduate medical education, lifestyle, and patient care.
Methods
A mixed-methods quantitative-qualitative survey was administered in August 2010 following the announcement of the proposed ACGME changes. Designated institutional officials were identified using a publicly available list of ACGME teaching institutions and a broad Internet search for contact information. This search yielded 75 contacts in 38 states, of which 23 institutions agreed to participate in the survey. From a total sample of 11 617 trainees, 2561 responded (22.0%), with 874 of these (7.5%) providing free-text responses. The survey was administered by e-mail with 12 questions assessing perceptions of the proposed regulations, as well as an open format free-response query at the end of the survey (“Please share any comments or concerns that you have”).
The free-text responses were synthesized and refined into a quantitative format using content analysis, a method that features “the systematic assignment of communication content to categories according to rules, and the analysis of relationships involving those categories.”14 This well-established method allows researchers to identify common themes and to quantify opinion responses such as those obtained in this survey. In order to minimize bias, 3 analysts reviewed the data several times independently, then discussed together and confirmed discrepant interpretations until reconciliation. A 3-stage method was used to optimize systemization of the process.
Stage I (Development of Rules)
The primary author undertook the first review of the commentary to draft an initial framework of rules for quantifying the text responses. These rules (themes) represented common topics (eg, handoffs, quality of life, etc) addressed in resident responses. Two other authors (I.Y.S. and P.A.S.) individually revised and consolidated these themes based on further review of the commentary and relevant literature. The final set of 27 themes was agreed to by the 3 researchers.
Stage II (Interpretation)
The 3 authors independently evaluated each resident response (n = 874) for the presence or absence of any of the 27 themes, and for the overall tone of the comment (ie, positive or negative opinion). Responses were organized on spreadsheets based on the 27 predefined themes. Throughout the data review, unique or representative comments were identified for discussion.
Stage III (Crystallization)
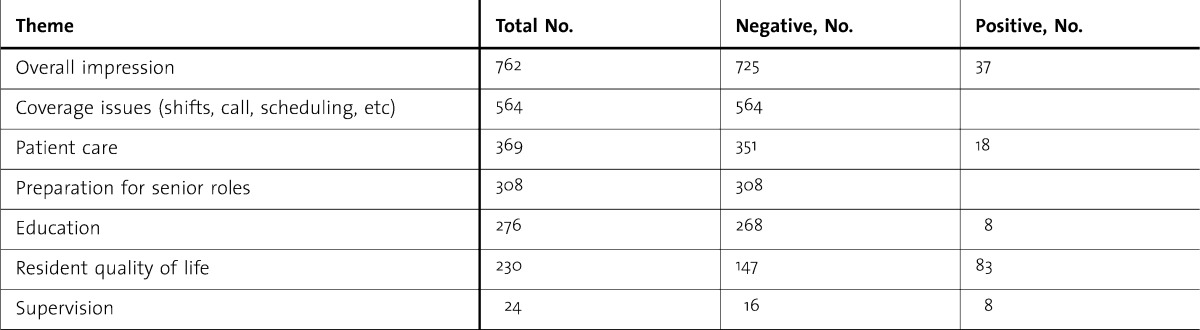
After the authors evaluated the resident comments, the 3 output spreadsheets were compiled and a final matrix was created. The authors discussed areas of disagreement until consensus was reached. Results are displayed as a sum of total responses for each theme (table 2). Finally, the 27 themes were further consolidated by the authors into 7 major headings for simplicity of presentation and comparison to the quantitative survey results (table 3).
TABLE 2.
Thematic Reference Set
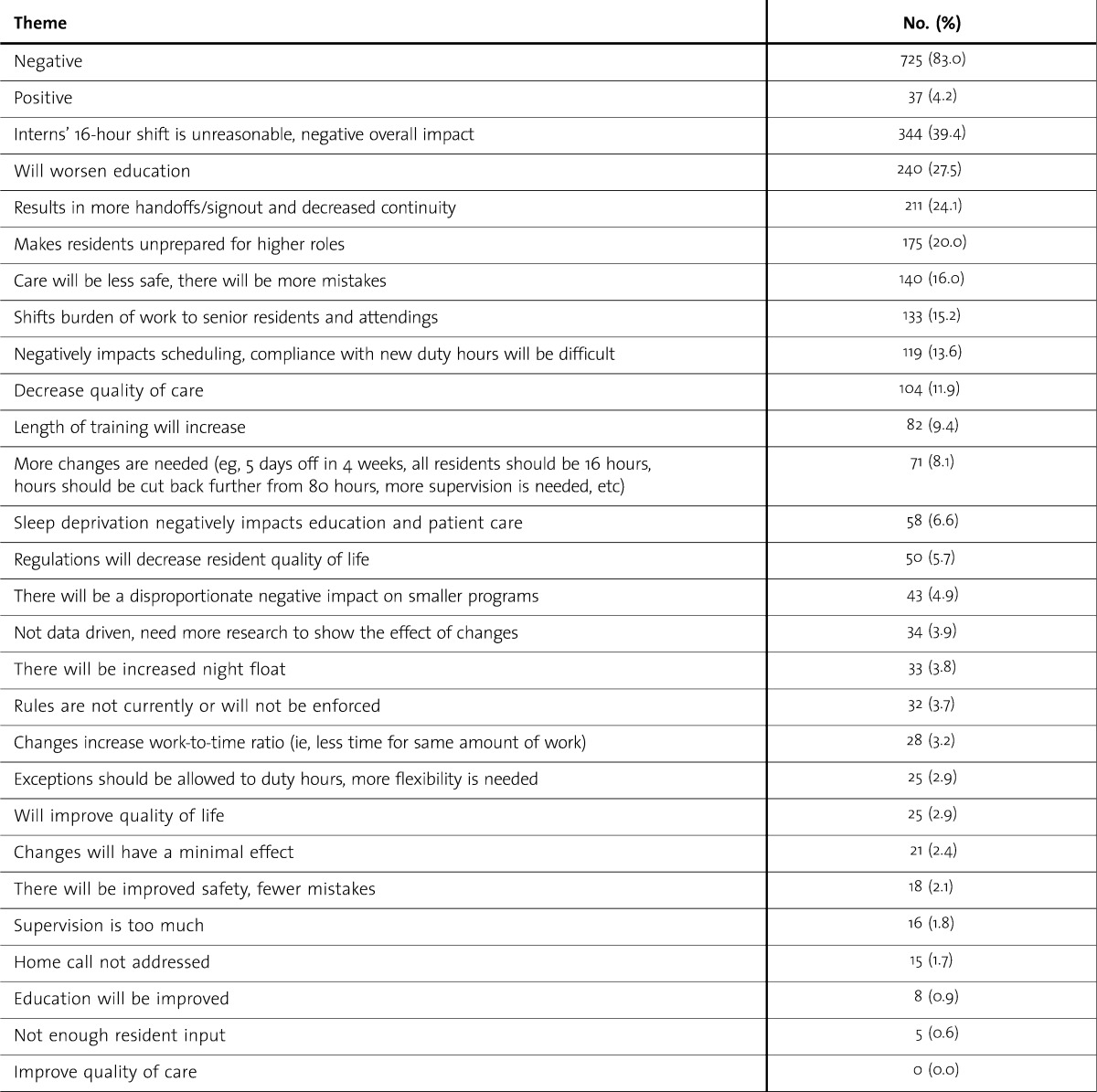
TABLE 3.
Summary of Results
Results
Given the open nature of the free-response question, residents responded to a variety of aspects of the duty hour and supervision standards. At the same time, our analysis identified common points. The result is a thematic classification and summary of heterogeneous communication content, which offers added breadth to the quantitative results of the Resident Survey.5
Overall, the data show a predominately negative perspective (83.0%). Many of the comments were ardently critical (eg, “These requirements put residents in an awful position between meeting requirements and doing what is best for patients.”). Descriptors such as “terrible,” “completely disagree,” and “ridiculous” were frequently encountered. On the contrary, 37 residents had a generally positive attitude toward the changes. The remainder of the respondents (n = 117) made both positive and negative statements or offered neutral or no meaningful feedback (eg, “N/A”).
The bulk of resident comments reflected concern over the 16-duty hour limit for interns (n = 344) and the potential negative impact on training and education (n = 240), and on preparation for more senior roles (n = 175). These results are similar to the findings of the quantitative survey results, which found most residents were concerned about education (54.0%) and preparation for senior roles (62.9%).5
The new work hour requirements are short-sighted and reactionary. Medicine is not a 9-to-5 job. We need to be able to work until the job is finished, not just until we have put in a certain number of hours…interns will take much longer to get up to speed on how the system works and many medical decisions will be made in their absence, making it difficult for them to learn what they need to during intern year…The experience gained from staying overnight and following a patient for 24 hours cannot be replaced.
Other prevailing themes related to increased mistakes and diminished patient safety (n = 140) and diminished quality of care (n = 104) secondary to an increased number of patient handoffs and lack of continuity of care (n = 211).
These new ACGME changes are a huge blow to resident education. We learn at the bedside and need to be allowed to continue to see a patient from the minute they hit the ER/floor until the resolution of their acute presentation; I can't do this if I'm forced to go home at 7 pm. Increasing the number of patient handoffs will likely prove detrimental with worse patient outcomes than the physician in their 30th hour.
Along the same lines, residents express concern that intern duties will be shifted to more senior residents or attending physicians (n = 133).
The new duty hour requirements will require second- and third-year residents to act as interns…This puts the interns at a disadvantage as they will not become effective independently until they are already in a supervisory role, and puts the seniors at a disadvantage, because they will be busy doing intern work instead of learning to supervise, educate, and run a unit…
Other issues identified in the comments include concern about the negative impact of the standards on scheduling flexibility (n = 25); on compliance with the duty hour limits (n = 119); and on smaller residency programs (n = 43) that rely on overnight call by residents and that may have functioned without resources for full-time supervision.
[I am] very concerned this is going to have a very negative effect on my small family medicine program. We do not have enough residents to have direct supervision of interns at all times and to have a PGY-2 or PGY-3 always present. How do PGY-2 residents have ability to supervise PGY-1 residents when in reality they themselves would not have been able to work on their own under these new regulations?
As an overall summary, table 3 illustrates the primarily negative tone in the residents' comments. Coverage issues—namely, 16-hour shifts, more in-house call for senior residents, and scheduling—were commonly discussed. Interestingly, supervision was relatively underdiscussed, but those who addressed the issue (n = 24; 66.7%) felt that more supervision would be beneficial for both patient care and education.
Discussion
Resident free-text responses to our survey identified several new and interesting perspectives on the duty hour limits. First, quality of life for all residents may actually worsen with 16-hour intern shifts and displacement of junior responsibilities to senior residents. In many hospitals, interns will work 6 days per week from “sign-in until sign-out” with little flexibility, thus enjoying fewer (or no) “golden weekends” and less time for life outside the hospital. These comments seem to disagree, however, with data from our quantitative study showing that many residents (50.9%) predict that quality of life will improve.5 It is important to consider how limiting hours may have the opposite effect than that intended, causing stress from increased work-density, that is, having to rush to complete given tasks in less time. Alternatively, residents may complete some tasks at home during off-duty hours, facilitated by the age of electronic medical records with remote online access.15
Residents also discussed the increased supervision requirement that has required senior residents to take more in-house calls, with that finding reported across specialties. For small programs that have not traditionally required higher-level supervision, additional personnel are needed to accommodate schedule changes, a resource that may not be financially feasible over the long term. Surgical residents will lose operative time, whereas residents in other specialties will have less time for teaching rounds and didactics on postcall days. Residents may lose valuable elective time, and an increase in night-float shifts at all levels of training may further reduce daytime clinical and educational opportunities. Similar to other findings, these concerns reflect quantitative data from our survey that found that many residents (41.9%) felt service obligations would take priority over education under further ACGME requirements.
Some comments addressed decreased freedom to moonlight by licensed resident physicians, continued lack of regulation of home call, and seemingly limited resident input in the regulatory changes, although the ACGME Duty Hours Task Force did have resident representation.
Our study has some limitations. First, content analysis has a potential for bias introduced by the interpretation of comments by the authors. This is minimized by the use of multiple data analysts, and this is an accepted approach in qualitative research.16 Second, the response rate of the survey was low, representing less than 2% of all residents nationally. Our findings are similar to other published studies of residents' opinions on duty hour limits.10,17–19 Our study is the first to include a large compilation of comments from residents across diverse specialties. Third, there is the potential for respondent bias because residents with stronger feelings may have been more likely to comment. However, residents with strongly positive feelings about the duty hour standards should have been equally inclined to comment. All of these limitations reduce the ability to generalize from the results to the overall population of residents. The generally negative response of residents corresponds with our previously published survey results as well as subsequent studies on resident perceptions.5–7,10,20
Although not empirically supported by our findings, we suspect that most residents want some form of duty hour standards. However, we found that many residents do not appear to support the current limits on their hours. Residents strive to become well-trained physicians and to take care of patients with appropriate supervision while not being overly burdened by standards and regulations. Learning to balance work (patient care) with personal responsibilities is vital in professional development, and residents' resistance to duty hour changes may represent a realization that residents are losing a central role in patient care.
Ultimately, the ACGME plays a vital role in maintaining standards for resident training programs, which prevent abusive work hours and potentially dangerous unsupervised activities. This study points out important concerns for sponsoring institutions and the ACGME as the community makes changes to adapt to the new standards. We urge residents to remain informed about the new duty hour regulations and to constructively voice their opinions as these policies are implemented. Residents are uniquely positioned to offer feedback on how the changes affect education and patient care, and this article provides a baseline attitude assessment that may be used for comparison to ongoing data collection. New studies on the effects of the changes in the coming years will be needed to see if the concerns are realized, but attempts should be made to mitigate issues before they arise.
Conclusions
This broad, multispecialty survey highlights many important and previously unaddressed comments on the new ACGME Common Program Requirements. The findings offer a summary of resident perspectives on changes in their duty hours that may have an impact on the entire health care system.
Of the 2011 changes, residents express the most concern for the interns' 16-hour shift cap, which they feel limits the opportunity to follow patients through the full course of illness, and weakens education, training, preparation for senior roles, and ultimately patient care. Residents also fear that interns will be unprepared to take longer calls as senior residents and that frequent intern turnover will negatively impact team dynamics as work and stress are shifted to senior residents and even attending physicians. Finally, frequent cross-coverage and reduced continuity may have a detrimental impact on the patient-physician relationship. Residents' perceptions of the duty hour limits offer important information for accreditors, regulators, and leaders making decisions on future refinements to the duty hour limits.
Footnotes
All authors are at Alpert Medical School of Brown University. Brian C. Drolet, MD, is a Fourth-Year Resident in the Department Plastic Surgery, and Rhode Island Hospital; Ina Y. Soh, MS, is a Fourth-Year Medical Student; Paul A. Shultz, BS, is a Third-Year Medical Student; Staci A. Fischer, MD, is an Associate Professor in the Department of Medicine, and Director of Graduate Medical Education at Rhode Island Hospital.
The quantitative data from the questionnaire were published in The New England Journal of Medicine, December 2010.5
Funding: The authors report no external funding for this study.
The authors wish to thank Lucy Spalluto, MD, and Laura Hebert for their support in producing this survey. Additional thanks are given to the many participating departments of graduate medical education for administering this survey to their residents.
References
- 1.Nasca TJ. Letter to the community. In. Chicago, IL: Accreditation Council for Graduate Medical Education; 2010. http://www.acgme.org/acgmeweb/Portals/0/PDFs/nascalettercommunity5_4_10.pdf. Accessed September 2012. [Google Scholar]
- 2.Samkoff JS, Jacques CH. A review of studies concerning effects of sleep deprivation and fatigue on residents' performance. Acad Med. 1991;66:687–693. doi: 10.1097/00001888-199111000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Feddock CA, Hoellein AR, Wilson JF, Caudill TS, Griffith CH. Do pressure and fatigue influence resident job performance. Med Teach. 2007;29:495–497. doi: 10.1080/01421590701506874. [DOI] [PubMed] [Google Scholar]
- 4.Antiel RM, Thompson SM, Reed DA, James KM, Tilburt JC, Bannon MP, et al. ACGME duty-hour recommendations—a national survey of residency program directors. N Engl J Med. 2010;363(8):e12. doi: 10.1056/NEJMp1008305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Drolet BC, Spalluto LB, Fischer SA. Residents' perspectives on ACGME regulation of supervision and duty hours—a national survey. N Engl J Med. 2010;363:e34. doi: 10.1056/NEJMp1011413. [DOI] [PubMed] [Google Scholar]
- 6.Fargen KM, Chakraborty A, Friedman WA. Results of a national neurosurgery resident survey on duty hour regulations. Neurosurgery. 2011;69(6):1162–1170. doi: 10.1227/NEU.0b013e3182245989. [DOI] [PubMed] [Google Scholar]
- 7.Lo V, Ward C. 2011 ACGME duty hour week proposal-a national survey of family medicine residents. Fam Med. 2011;43:318–324. [PubMed] [Google Scholar]
- 8.Drolet BC, Spalluto LB, Zuckerman M, McDonnell M. New ACGME rules for supervision and duty hours: resident commentary. Med Health R I. 2011;94:167, 171–172. [PubMed] [Google Scholar]
- 9.Rockey PH. Duty hours: where do we go from here. Mayo Clin Proc. 2011;86:176–178. doi: 10.4065/mcp.2011.0086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mir HR, Cannada LK, Murray JN, Black KP, Wolf JM. Orthopaedic resident and program director opinions of resident duty hours: a national survey. J Bone Joint Surg Am. 2010;93:e1421–e1429. doi: 10.2106/JBJS.K.00700. [DOI] [PubMed] [Google Scholar]
- 11.Romano PS, Volpp K. The ACGME's 2011 changes to resident duty hours: are they an unfunded mandate on teaching hospitals. J Gen Intern Med. 2011;27:136–138. doi: 10.1007/s11606-011-1936-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blum AB, Raiszadeh F, Shea S, Mermin D, Lurie P, Landrigan CP, et al. US public opinion regarding proposed limits on resident physician work hours. BMC Med. 2010;8:33. doi: 10.1186/1741-7015-8-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Accreditation Council for Graduate Medical Education. Data resource book: academic year 2009–2010. http://www.acgme.org/acWebsite/databook/2009-2010_ACGME_Data_Resource_Book.pdf. Accessed March 20, 2012. [Google Scholar]
- 14.Riffe D, Lacy S, Fico F. Analyzing Media Messages: Using Quantitative Content Analysis in Research. 2nd ed. Mahwah, NJ: Lawrence Erlbaum; 2005. [Google Scholar]
- 15.Deano RC, DeKosky A, Appannagari A, Doll J, Georgitis E, Potts S, et al. Resident time spent in clinical and educational activities at home: implications for duty hours. Arch Intern Med. 2011;171:1038–1039. doi: 10.1001/archinternmed.2011.218. [DOI] [PubMed] [Google Scholar]
- 16.Krippendorff K. Content Analysis: An Introduction to Its Methodology. 2nd ed. Thousand Oaks, CA: Sage; 2004. [Google Scholar]
- 17.Cohen-Gadol AA, Piepgras DG, Krishnamurthy S, Fessler RD. Resident duty hours reform: results of a national survey of the program directors and residents in neurosurgery training programs. Neurosurgery. 2005;56:398–403. doi: 10.1227/01.neu.0000147999.64356.57. discussion 398–403. [DOI] [PubMed] [Google Scholar]
- 18.Irani JL, Mello MM, Ashley SW, Whang EE, Zinner MJ, Breen E. Surgical residents' perceptions of the effects of the ACGME duty hour requirements 1 year after implementation. Surgery. 2005;138:246–253. doi: 10.1016/j.surg.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 19.Macgregor JM, Sticca R. General surgery residents' views on work hours regulations. J Surg Educ. 2010;67:376–380. doi: 10.1016/j.jsurg.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 20.Freeman WD, Nolte CM, Matthews BR, Coleman M, Corboy JR. Results of the American Academy of Neurology resident survey. Neurology. 2011;76:e61–e67. doi: 10.1212/WNL.0b013e318212a871. [DOI] [PubMed] [Google Scholar]


