Abstract
Background
The Accreditation Council for Graduate Medical Education requires scholarly activity for both faculty and residents in obstetrics and gynecology (Ob-Gyn). There is little evidence on the most effective method to train, recruit, and retain research faculty who can mentor resident researchers at small programs.
Innovation
To address this problem, we created the “Baby Steps” program for a small university-based Ob-Gyn program.
Methods
After a thorough assessment of existing resources, a postdoctoral researcher was recruited and coupled with an established researcher to raise the standards of resident research, facilitate and coordinate resident projects, and support clinical faculty participation in research activities. Grant submissions, grants awarded, publications submitted, presentations, and awards were tracked before and after the implementation of the Baby Steps program for faculty and residents.
Results
After 2 years the program has already begun to show an increase in scholarly activity. In a program of 12 residents, 8 made one or more presentations at regional or national meetings within the previous 24 months. Additionally, 8 of 12 clinical faculty members were engaged as mentors in resident research, compared with only 3 in past years. Further, abstract, paper, and grant submissions by faculty increased approximately 25%.
Conclusion
The addition of a mentored postdoctoral researcher was associated with improvements to both resident and faculty research activities. Based on this success, a sister residency program has incorporated the Baby Steps approach into its training.
What was known
There appears to be a lack of effective approaches to train, recruit, and retain research faculty who can mentor resident research in small programs.
What is new
An obstetrics-gynecology program added dedicated research staff to facilitate and coordinate resident research projects, and support clinical faculty in research activities.
Limitation
Single-site, single-specialty study may limit generalizability.
Bottom line
The program resulted in an increase in scholarly activity for residents and faculty, with abstract, paper, and grant submissions by faculty increasing approximately 25%.
Introduction
Since the early 1990s the Accreditation Council for Graduate Medical Education has required scholarly activity for both faculty and residents in obstetrics and gynecology (Ob-Gyn). Although faculty scholarly activity is defined as grants, manuscripts, and poster and oral presentations, resident activities may include experiences that enhance understanding of the conduct of research or its interpretation, application of research data to patient care, and translation or explanation of research to patients.1 Between 2007 and 2010, only 5.5% (31 of 567) of Residency Review Committee citations for Ob-Gyn programs were issued for lack of scholarly activity; however, 67.7% of these citations were the result of faculty members not meeting expectations.2–4
Numerous approaches have been tried to maintain faculty and resident scholarly activity. Seehusen et al5 suggested a point system to give credit for various activities. Other approaches include formal and informal faculty/resident meetings, and the provision of resources to collect and interpret data, prepare manuscripts, or meet deadlines.5–11 A few programs have developed a more formal approach, such as a 1- to 3-month research rotation during residency.6,12 However, given the breadth of knowledge and technical skills that Ob-Gyn residents are expected to develop in 4 years, as well as the increasing work hour restrictions, this may not be practical.7 The literature suggests that programs in all disciplines face similar perceived problems in achieving a successful and meaningful resident research experience.5–11
The most commonly cited barriers to resident participation in research are (1) lack of time for residents and clinical faculty, (2) lack of infrastructure, (3) lack of mentoring, and (4) lack of financial support. To remove these barriers, our residency developed and implemented the “Baby Steps” program (BSP) to improve overall resident and faculty scholarly activity.
Program Development
Infrastructure Inventory
In 2008, BSP was initiated at a small southwestern US university-based Ob-Gyn residency program. The first step was to identify hidden research assets and then determine how they could best be accessed to improve faculty and resident scholarly activity. Existing infrastructure was inventoried within the Ob-Gyn department, the medical school, and the adjacent university campus. The inventory included assessment of existing departmental research, identification of current cross-campus collaborations, evaluation of the potential for expansion of collaborative efforts, and establishing how department faculty and residents could use these resources in research.
One outcome of the inventory suggested a lack of coordination of assets. To facilitate coordination and mentoring, a new postdoctoral researcher position was created and filled in August 2009 using clinically generated funds. The overarching objective was to assist faculty members and residents in developing their research question into a viable project. The postdoctoral researcher was assigned the task of coordinating resident research; assisting with all aspects of the departmental research program, including submission of Institutional Review Board or Institutional Animal Care and Use Committee protocols; identifying and applying for grants; establishing collaborations with clinical and basic science researchers for both the medical school and undergraduate academic campus; managing the transfer of research specimens; and coordinating and overseeing resident research opportunities in outside laboratories to ensure data were collected appropriately.
In addition, the results of the infrastructure inventory suggested the department had access to a wide array of research support. The department already contained a small combined clinical and research laboratory. Through the laboratory director's associations on the undergraduate university campus and appointment in a basic science department within the medical school, the laboratory housed both graduate and undergraduate researchers who conducted a wide range of research and could be assigned to assist with research projects in the department. Additionally, preexisting relationships with many other departments within the medical school and the university campus, including the school of nursing and the college of agricultural sciences, could be expanded to incorporate a multidisciplinary approach with a variety of collaborators. These relationships had occasionally provided residents opportunities for research in the past, but never in a systematic fashion.
Once the full inventory of resources was determined, the next step was to establish how best to use these resources. In our small Ob-Gyn program (12 total residents and averaging between 8 and 12 clinical faculty) with multiple practice sites and significant annual patient volume, we could not ensure protected time for research, especially because all faculty salaries are funded through clinical efforts, not research dollars. Instead, a better use of faculty resources was to have them concentrate their efforts on developing research ideas and then mentoring resident researchers and other students with the assistance of the postdoctoral researcher to coordinate research efforts.
Outcome Measures
After program implementation, data were collected annually for 2 years to assess the early effectiveness of the program. Data tracked specifically for faculty were: (1) grant submissions, (2) grants funded, (3) paper submissions, (4) presentations at regional and national meetings, and (5) the number of faculty participating in the 4 items above. Data collected related to the resident scholarly experience included: (1) the number of faculty being mentors, (2) presentations by residents at regional and national meetings, and (3) the number of awards the residents received for their research work.
Results
All 12 residents met the minimum research standard established for their level of training in both 2010 and 2011. There was an increase in faculty involvement in resident research, with 8 of 10 faculty participating in research during both years of the BSP, compared with only 4 in the year preceding the BSP, when there were 12 clinical faculty members (figure 1). During the 2-year period a total of 8 residents presented their work at regional meetings and 4 residents presented at national meetings on a variety of subjects, which represented studies including chart reviews, surveys, clinical studies, and bench research. Of these 12 presentations, 5 were selected for recognition at the various meetings, including 2 selected as the outstanding presentations at each of the first 2 years of the American Congress of Obstetricians and Gynecologists District XI Meeting (figure 2). This was a significant increase from the previous year, when only 2 presentations were made at regional or national meetings. At the time of writing, 3 resident papers from this group are under consideration for publication. The increase in research activity was not limited to residents; overall research activity among faculty members increased 25% (figure 1). There was a marked increase in the number of faculty participating in research, as demonstrated by increased grant applications from zero in the year prior to the program to 9 in the first 2 years of the BSP, with 4 receiving funding. Four faculty members have submitted 9 publications and revisions in the 2 years of the BSP, compared with a single faculty member submitting 2 publications the year before. In addition to the increase in publications submitted, the number of faculty members submitting abstracts to regional and national meeting increased from 3 to 8 (figure 2).
FIGURE 1.
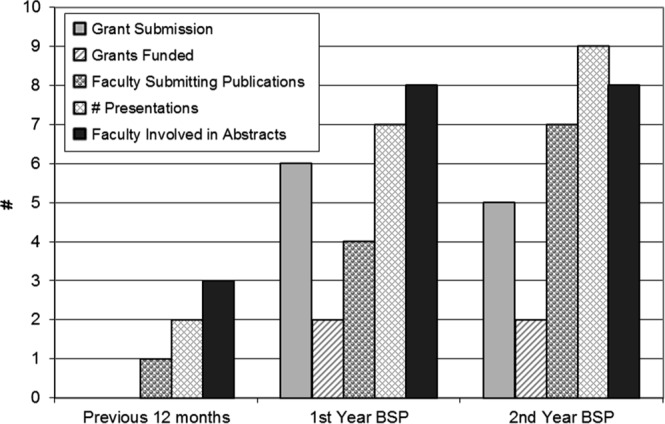
Increases Seen in Faculty Scholarly Activity in the First 24 Months After Initiation of the Baby Steps Program (BSP) in a Small Obstetrics and Gynecology Residency Program
FIGURE 2.
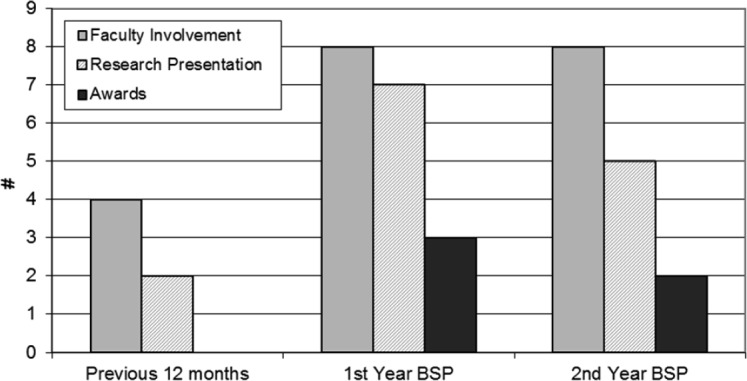
Increases Seen in Resident-Related Scholarly Activity (Including Faculty Participation as Research Mentors) in a Small Obstetrics and Gynecology Residency Program in the First 24 Months After Initiation of the Baby Steps Program (BSP)
Discussion
During a 2-year period, the BSP resulted in substantial increases in resident and faculty scholarly activities, which appear to be directly due to this new program.
The need to provide effective and meaningful research experiences to residents is not limited to obstetrics and gynecology.13 A number of approaches have been used to provide faculty and residents with the opportunity for scholarly activity.5–7,12 However, most appear to fall short of addressing all of the issues confronting programs as they contemplate scholarly activity, and specifically resident research.8,11,12,14 Once a means has been established to provide for scholarly activity, programs must determine how to sustain the experience. Many programs require only one project, whereas a few require annual unique projects over the course of residency.14,15 Progress in research is typically demonstrated at periodic departmental symposiums, and a number of programs have begun including guest judges and prizes.5,10,15 Some programs require presentations at societal meetings or publication to fulfill the research requirement.6,11,12,14,16
The BSP represents a unique approach to increasing scholarly activities by using a “shadow infrastructure” that might not be readily apparent to the department. This includes hosting undergraduate and graduate students from an academic campus to do collaborative research with medical faculty and residents. Although the infrastructure inventory will vary between sites, most programs will have access to some potentially unrecognized resources. A critical ingredient for BSP is the use of a trained, full-time postdoctoral researcher. This individual coordinated the infrastructure assets and targeted projects to individual faculty and residents. Using this approach has minimized the need for faculty participation in the day-to-day activities required to maintain a research project with inexperienced residents, while maximizing the faculty members' ability to participate as full partners in project design and interpretation of study results.
Because this project was studied at one site, the generalizability to other sites is limited. Also, other factors, such as enhanced visibility of research and mentoring as important faculty activities, may have caused the increased productivity. Because the BSP is new, sustainability over time remains unclear and will be a key focus for future studies.
Conclusions
Initiation of the BSP in our Ob-Gyn program has been associated with a striking and rapid increase in scholarly productivity of both faculty and residents during a relatively short period of time, at the cost of one postdoctoral faculty member. These activities include grant submissions, abstract and manuscript submissions, and awards, as well as increased faculty mentoring of resident scholarly activities.
Footnotes
All authors are with the Department of Obstetrics and Gynecology, Texas Tech University Health Sciences Center. Lindsay L. Penrose, PhD is a Postdoctoral Coordinator of the Residency Research Program; Edward R. Yeomans, MD, is a Professor, Chairman of the department, and Program Director; Carolina Praderio, MD, is a Resident; and Samuel D. Prien, PhD, is a Professor and Director of Departmental Research.
Funding: The authors report no external funding source for this study.
References
- 1.Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Obstetrics and Gynecology. http://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/220obstetricsandgynecology01012008.pdf. Accessed October 5, 2012. [Google Scholar]
- 2.Accreditation Council for Graduate Medical Education. ACGME Data Resource Book: Academic Year 2008–2009. http://www.acgme.org/acgmeweb/Portals/0/PFAssets/PublicationsBooks/2008-2009_ACGME_DATA_RESOURCE_BOOK.pdf. Accessed October 5, 2012. [Google Scholar]
- 3.Accreditation Council for Graduate Medical Education. ACGME Data Resourse Book: Academic Year 2009–2010. http://www.acgme.org/acgmeweb/Portals/0/PFAssets/PublicationsBooks/2009-2010_ACGME_DATA_RESOURCE_BOOK.pdf. Accessed October 5, 2012. [Google Scholar]
- 4.Accreditation Council for Graduate Medical Education. ACGME Data Resource Book: Academic Year 2007–2008. http://www.acgme.org/acgmeweb/Portals/0/PFAssets/PublicationsBooks/2007_2008_ANA_ANA_Current_ACGME_DataBook.pdf. Accessed October 5, 2012. [Google Scholar]
- 5.Seehusen DA, Asplund CA, Friedman M. A point system for resident scholarly activity. Fam Med. 2009;41(7):467–469. [PubMed] [Google Scholar]
- 6.Kanna B, Deng C, Erickson SN, Valero JA, Dimitrov V, Soni A. The research rotation: competency-based structured and novel approach to research training of internal medicine residents. BMC Med Educ. 2006;17(6):52. doi: 10.1186/1472-6920-6-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kenton K, Brubaker L. Research education in obstetrics and gynecology: how are we doing. Am J Obstet Gynecol. 2007;197(5):532.e531–532.e534. doi: 10.1016/j.ajog.2007.07.030. [DOI] [PubMed] [Google Scholar]
- 8.Edwards K. “Short stops”: peer support of scholarly activity. Am Med. 2002;77(9):939. doi: 10.1097/00001888-200209000-00045. [DOI] [PubMed] [Google Scholar]
- 9.Sabir M, Penney DG, ReMine SG, Mittal VK. Scholarly activities - essential to surgical education. Curr Surg. 2003;60(4):459–462. doi: 10.1016/S0149-7944(03)00007-2. [DOI] [PubMed] [Google Scholar]
- 10.Thompson RJ, Benrubi GI, Kauntiz AM. Resident research in obstetrics and gynecology. J Reprod Med. 1994;39(8):635–638. [PubMed] [Google Scholar]
- 11.Smith-Barbaro P, Fulda KG, Coleridge ST. A divisional approach to enhancing research among osteopathic family practice residents. J Am Osteopath Assoc. 2004;104(4):177–179. [PubMed] [Google Scholar]
- 12.Konstantakos EK, Laughlin RT, Markert RJ, Crosby LA. Assuring the research competence of orthopedic graduates. J Surg Educ. 2010;67(3):129–134. doi: 10.1016/j.jsurg.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 13.Beasley BW, Scrase DR, Schultz HJ. Determining the predictors of internal medicine residency accreditation: what they do (not what they say) Acad Med. 2002;77(3):238–246. doi: 10.1097/00001888-200203000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Roane DM, Inan E, Haeri S, Galynker II. Ensuring research competency in psychiatric residency training. Acad Psychiatry. 2009;33(3):215–220. doi: 10.1176/appi.ap.33.3.215. [DOI] [PubMed] [Google Scholar]
- 15.Sulak PJ, Croop JA, Hillis A, Kuehl TJ. Resident research in obstetrics and gynecology: development of a program with comparison to a national survey of residency programs. Am J Obstet Gynecol. 1992;167(2):498–500. doi: 10.1016/s0002-9378(11)91437-9. [DOI] [PubMed] [Google Scholar]
- 16.Neale AV. A national survey of research requirements for family practice residents and faculty. Fam Med. 2002;34(4):262–267. [PubMed] [Google Scholar]


