Abstract
Gene expression control mediated by microRNAs and epigenetic remodeling of chromatin are interconnected processes often involved in feedback regulatory loops, which strictly guide proper tissue differentiation during embryonal development. Altered expression of microRNAs is one of the mechanisms leading to pathologic conditions, such as cancer. Several lines of evidence pointed to epigenetic alterations as responsible for aberrant microRNA expression in human cancers. Rhabdomyosarcoma and neuroblastoma are pediatric cancers derived from cells presenting features of skeletal muscle and neuronal precursors, respectively, blocked at different stages of differentiation. Consistently, tumor cells express tissue markers of origin but are unable to terminally differentiate. Several microRNAs playing a key role during tissue differentiation are often epigenetically downregulated in rhabdomyosarcoma and neuroblastoma and behave as tumor suppressors when re-expressed. Recently, inhibition of epigenetic modulators in adult tumors has provided encouraging results causing re-expression of anti-tumor master gene pathways. Thus, a similar approach could be used to correct the aberrant epigenetic regulation of microRNAs in rhabdomyosarcoma and neuroblastoma. The present review highlights the current insights on epigenetically deregulated microRNAs in rhabdomyosarcoma and neuroblastoma and their role in tumorigenesis and developmental pathways. The translational clinical implications and challenges regarding modulation of epigenetic chromatin remodeling/microRNAs interconnections are also discussed.
Keywords: microRNA, rhabdomyosarcoma, neuroblastoma, epigenetics, differentiation, Polycomb proteins, DNA methylation, histones
1. Introduction
Epigenetic chromatin remodeling plays a pivotal role in normal mammalian development and post-natal tissue homeostasis. Indeed, lineage specification and cellular differentiation, which underlie embryo development and morphogenesis from a single pluripotent stem cell, are epigenetically regulated processes. The final result is the “plasticity” of an individual genotype that, through the activation of molecular cascades, timely and sequentially controlled, produces different phenotypes in response to different microenvironments. In the last 10 years, special attention has been paid to the non-protein coding portion of the genome such as non-coding small RNAs, among which are microRNAs (miRNAs), considered to be major regulators of developmental pathways [1–8]. Of note, chromatin remodeling and miRNA pathways have been shown to be interconnected and able to regulate each other. To date, it is recognized that the deregulation of the epigenetic- and miRNA-dependent control of gene expression underlies tumorigenesis.
Rhabdomyosarcoma (RMS) and neuroblastoma (NB) are pediatric cancers derived from cells sharing molecular features of skeletal muscle and neuronal progenitors, respectively, blocked at different stages of differentiation. It has been clearly demonstrated that deregulation of developmental pathways plays a major role in both tumors.
The present review will focus on current knowledge about miRNAs deregulated in RMS and NB by epigenetic modifications. Their role in developmental pathways and RMS and NB tumorigenesis will be highlighted. Moreover, the translational implications and challenges of miRNAs modulation in these pediatric tumors will be discussed.
2. What the Term “Epigenetics” Means
The term “epigenetics” describes cellular modifications caused by mechanisms other than DNA sequence variations that can be heritable and modified by environmental stimuli [9]. Therefore, in the present review, we will refer to epigenetics to describe the chemical reactions of chromatin that affect its accessibility in order to switch “on” and “off” gene expression.
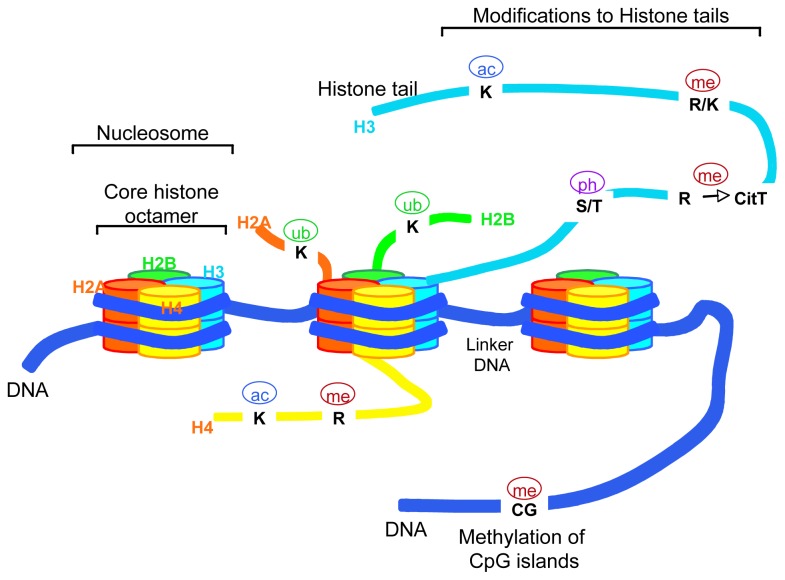
To fit within the nucleus of eukaryotic cells, short lengths of DNA are wrapped around an octamer of histone proteins (two copies of core histones H2A, H2B, H3 and H4) forming the basic units of chromatin termed “nucleosomes” (Figure 1).
Figure 1.
Schematic representation of chromatin structure. Eukaryotic DNA is wrapped around core histone proteins (histone octamer: H2A, H2B, H3 and H4) to form compact chromatin structures termed nucleosomes. Covalent modifications to histones (on histone tails) involve amino acidic residues (Lysine (K), Arginine (R) Serine (S) and Tyrosine (T)) that can be acetylated (ac), methylated (me), phosphorylated (ph) and/or ubiquitinilated (ub). CpG islands on DNA can be methylated. These post-translational modifications result in the epigenetic regulation of gene expression.
Higher-order organizations are formed by further compaction of chromatin structure. The degree of packaging influences the chromatin accessibility to transcriptional-regulatory complexes switching a gene “on” or “off.” Therefore, the “epigenome” encompasses genetic information that is the result of multiple processes involving chromatin modifications such as DNA methylation, histone proteins modification, histone variants replacement, nucleosome repositioning and mechanisms involving non-coding RNAs function. All these epigenetic modifications can be rapidly resumed and, therefore, fit well for the purpose of fine tuning the timely controlled developmental processes.
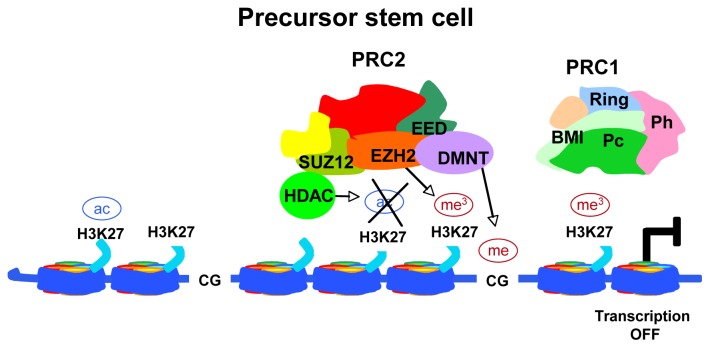
DNA methylation is catalyzed by DNA methyltransferases (DNMTs) and results in de novo methylation of unmethylated DNA and/or methylation maintenance of hemimethylated sequences. In normal tissues, DNA methylation is typically present and stable in the intergenic regions. In cancer cells, DNA methylation is exclusively found at the level of cytosines within CpG-rich regions of gene promoters leading to gene silencing. On the contrary, DNA hypomethylation of these CpG islands, also often aberrant in cancer, can increase gene expression [10]. The final result is either the silencing of tumor suppressor genes or the transcriptional activation of proto-oncogenes. In addition, DNA hypomethylation can lead to DNA helix breakpoints and, ultimately, to loss of heterozygosity (LOH) or aberrant chromosomal rearrangements. In strict conjunction with these mechanisms, the histone code generated by covalent modifications on histone tails, regulates chromatin remodeling for the accessibility of the transcription machinery to genes up to DNA repair, replication and segregation [11]. The major modifications of histone tails are controlled by histone acetyltransferases (HAT) and histone demethylases (HDM) in a competitive manner with histone deacetylases (HDAC) and histone methyltransferases (HMT), respectively. Among HMTs, the Polycomb group (PcG) protein EZH2, a component of the Polycomb repressor complex 2 (PRC2), is responsible for the trimethylation of Lysine 27 on histone H3 (H3K27me3) on gene promoters (Figure 2).
Figure 2.
Schematic representation of transcriptional gene repression by PRC2. In an uncommitted stem cell, the core component EZH2 methylates histone H3 on K27, thus generating the epigenetic mark H3K27me3. The HDAC activity favors this EZH2 effect deacetylating H3K27. In this way, the PRC1 complex is recruited and binds to DNA, thus stabilizing the repressive state of the chromatin. The final result is the transcriptional repression of developmental genes.
This modification allows the recruitment of the PRC1 complex which inhibits gene transcription through histone H2A ubiquitination. HDACs participate to the PRC complexes reinforcing the inhibition of gene expression by deacetylating H3K27, thus favoring H3K27 trimethylation. Finally, PcG complexes recruit DNMTs to specific gene loci to induce transcriptional silencing through DNA methylation (Figure 2). The final result is the maintenance of cell stemness and the support of self-renewal and pluripotency. Consistently, components of the PRC complexes are often aberrantly over-expressed in tumors (reviewed in [12]). Of note, epigenetic modifications that are maintained through mitosis and inherited during cell development and differentiation can be reversed by treatment with appropriate drugs. Therefore, compounds acting on “epimutations” can be used in association with conventional chemotherapy to induce growth arrest, differentiation and tumor cell death.
3. The Small Non-Coding RNAs, “microRNAs”
MiRNAs are a class of non-coding ~19–22 nucleotides (nt) single-strand RNAs transcribed in a developmental and tissue-specific manner during embryogenesis [13]. More than 1500 mature miRNAs have been identified in humans (http://www.mirbase.org), which are highly conserved across species. miRNAs are involved in post-translational gene silencing by binding complementary sequences in the 3′-untraslated regions (UTRs) of a target mRNA through their “seed” sequence leading to translational repression or mRNA degradation [14,15].
The expression of more than 60% of human protein-coding genes is controlled by miRNAs (reviewed in [13]). Several miRNAs can target the same mRNA and, conversely, each miRNA can target several mRNAs leading to additional layers of post-transcriptional control of gene expression. To further expand the scenario, specific miRNAs have been recently described to upregulate gene transcription also in quiescent cells [16] and others to target sequences within the 5′UTR [17], exonic regions [18] or gene promoter regions [19].
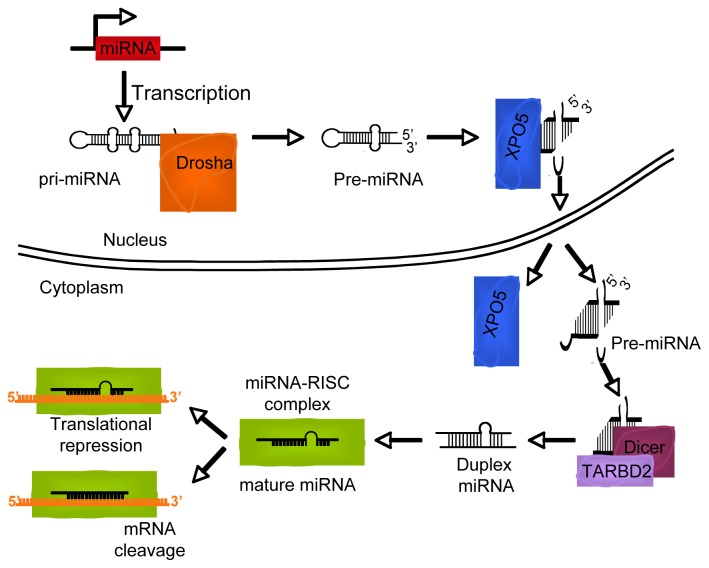
Mature miRNAs are the result of sequential processing of longer RNA precursors transcribed by RNA polymerase II and/or III and called pri-miRNA (Figure 3) [20,21]. This long transcript is processed by Drosha, a ribonuclease-III protein, in collaboration with DGCR8, a protein responsible for anchoring the pri-miRNA into the complex. The resulting 70-nt-long molecule termed pre-miRNA, is exported to the cytoplasm by the nuclear export protein Exportin-5 [13,22]. In the cytoplasm, the pre-miRNA is released and processed by Dicer to produce the functional ~19–22-nt double-strand RNAs. The less stable single strand is loaded by the Dicer-TRPB complex into the RNA-induced silencing complex (RISC) which carries it to complementary 3′UTR mRNA sequences.
Figure 3.
The biogenesis of miRNAs. MiRNAs are transcribed as longer RNA precursor (pri-miRNA) by RNA polymerase II and/or III and processed by the Drosha complex in pre-miRNAs. These fragments are exported from the nucleus by exportin 5 (XPO5). In the cytoplasm pre-miRNA are further processed by Dicer and TAR RNA-binding protein 2 (TARBD2) to generate mature miRNAs, which are loaded into the RNA-induced silencing complex (RISC). The translation of mRNAs targets into proteins is repressed by mRNA degradation or, alternatively, block of mRNA translation.
MiRNAs regulate fundamental physiologic processes such as embryonic development, lineage/tissue identity specification and homeostasis [23–27]. Therefore, it is not surprising that miRNAs display an aberrant expression profile in a wide range of human diseases [13]. In tumor cells, as reported for protein-coding gene, miRNA promoters can be aberrantly modified by the deregulated epigenetic machinery leading to changes in their expression profile [28–31]. Increasing evidence suggesting tumor suppressor or oncogenic role for miRNAs has been obtained in adult cancers [1,13,32–34]. Consistently, the re-expression of tumor suppressor miRNAs in tumor cells has been suggested as a potential anti-cancer therapeutic approach [35–40].
Recently, miRNAs have been shown, by us and other groups, to play a role also in the pathogenesis of embryonal pediatric cancers such as RMS and NB [41–43]. So far, the majority of tumor suppressor miRNAs involved in RMS and NB regulates the differentiation of skeletal muscle and neuronal compartments, respectively. These miRNAs are often silenced by aberrant DNA or histone methylation or located in unstable chromosomal regions often involved in LOH, ie miR-34a [13,44].
Consistently, their re-expression after treatment with HDAC inhibitors, de-methylating compounds or differentiating agents is sufficient to allow tumor cell differentiation and to impair tumorigenesis. Therefore, an epigenetic approach aimed at re-expressing these miRNAs could have a therapeutic value.
4. Rhabdomyosarcoma
RMS is a skeletal muscle-derived tumor and the most common soft-tissue sarcoma of childhood [45]. RMS cells express transcription factors specific to skeletal muscle progenitors, such as Myogenic Differentiation (MyoD) and myogenin [46,47], but their intrinsic myogenic program is disrupted at different stages of differentiation. In line with these observations, restoring terminal differentiation in RMS cells leads to inhibition of cell proliferation in vitro and tumor growth in vivo.
Pediatric RMS includes two major histological subtypes, namely alveolar (~25% of cases) and embryonal (~75% of cases) RMS [45,48]. The five-year overall survival rate of non-metastatic embryonal RMS patients is around 70%, while that of alveolar RMS and metastatic patients is still in the order of 25%, supporting the urgent need of novel therapeutic approaches.
The majority of alveolar RMS are characterized by chromosomal translocations, such as t (2; 13) or t (1; 13), leading to the expression of PAX3/FOXO1 or PAX7/FOXO1 fusion proteins, respectively [49–51]. These fusion products, especially PAX3/FOXO1, are a hallmark of high-risk tumors and correlate with poor prognosis [52]. Approximately 20% of alveolar RMS do not present known chromosomal translocations and are molecularly and clinically indistinguishable from embryonal ones [53–55]. However, novel chromosomal translocations involving PAX3 have been recently discovered in a subset of alveolar RMS previously diagnosed as fusion negative [51,56].
During skeletal muscle tissue development, PAX3 expression is detected in pluripotent progenitors and is followed by that of PAX7, which characterizes myogenic committed cells [57,58]. These transcription factors, on one hand, induce the expression of MyoD that marks myoblasts, and on the other hand, stimulate self-renewal and proliferation of myogenic cells. Thus, their expression is fundamental to assure the balance between cell proliferation and differentiation during embryogenesis leading to the right number of committed progenitors in order to form multinucleated myofibers. During differentiation, pro-myogenic miRNAs downregulate PAX3 and PAX7 to achieve complete myogenesis (reviewed in [59]).
An altered expression of miRNAs acting as pro-myogenic regulators has been reported in RMS, [43,59–61]. These miRNAs behave as tumor suppressors when re-expressed, halting tumorigenic processes working in negative feedback circuitries with epigenetic regulators. These findings demonstrate that aberrant epigenetic control of miRNA expression concurs to RMS pathogenesis.
4.1. Epigenetically Deregulated miRNAs in Rhabdomyosarcoma
Muscle-specific miRNAs that regulate myogenesis are termed “myomiRs.” To this group belong three miRNA clusters, miR-1-1/miR-133a-2, miR-1-2/miR133a-1 and miR-206/miR-133b, encoded by three bicistronic miRNA genes on separate chromosomes (reviewed in [62]).
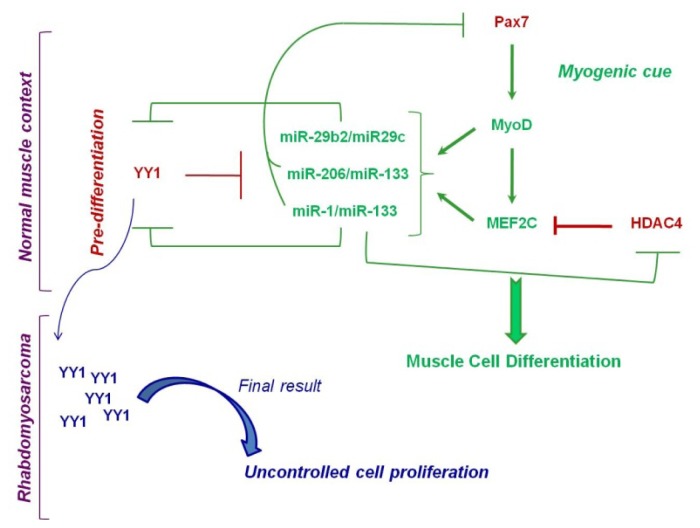
Although no direct epigenetic regulation of the expression of miR-1 and miR-206 clusters has been highlighted in RMS, a recent study provided several evidences linking these miRNAs to the epigenetic machinery in normal myoblasts [63]. In this work, YY1 was shown to regulate the expression of miR-1 and miR-206 clusters in murine myoblasts in vitro and in vivo. In particular, the authors found YY1 binding sites in previously identified muscle-specific enhancers [64] located (i) upstream of miR-1-2 (E1) and (ii) in an intron between miR-1-2 and miR-133a-1 (E2), and (iii) between miR-1-1 and miR-133a-2 gene loci (E3). Moreover, they discovered a previously unknown enhancer upstream of miR-206 and miR-133b coding regions (E4) showing YY1 binding site. They demonstrated that YY1 repressed the activity of all these four enhancers impairing the expression of miRNAs [63]. Interestingly, Ezh2 was present and active on the enhancers E1 and E3 but not on E2 and E4 suggesting that YY1 can function in myoblasts in a HMT-independent manner. Furthermore, the same authors uncovered a feedback loop between miR-1 and YY1 demonstrating that miR-1 directly targets the 3′UTR of YY1 mRNA. Having demonstrated that miR-1 is able to target PAX7, as already reported for miR-206 [65], which is consistently upregulated in YY1 over-expressing myoblasts, the authors depicted an anti-myogenic network in which YY1 plays a central role in repressing miR-1/miR-206 (Figure 4). This network is flexible and bi-univocal due to the feedback control of miR-1 on YY1 expression [63].
Figure 4.
Circuits involving the Polycomb Group (PcG) protein YY1 and miRNAs in normal and Rhabdomyosarcoma contexts. During myoblasts expansion, YY1 represses miR-29, miR-1 and miR-206 cluster expression. Under a myogenic stimulus, Pax7 induces the muscle regulatory factor MyoD that allows MEF2C activation, leading to miR-29, miR-1 and miR-206 de-repression. MiR-1 and miR-29 clusters post-transcriptionally block YY1 expression. Moreover, downregulation of Pax7 caused by miR-1 and miR-206 and that of HDAC4 caused by miR-1 ultimately leads to differentiation of myogenic precursors. In the RMS context, YY1 expression is highly deregulated resulting in pro-myogenic miRNAs repression that causes uncontrolled cell proliferation and muscle differentiation impairment.
Additional links with epigenetic networks in myoblasts have been shown for both miR-1 and miR-206 clusters. The ectopic expression of these miRNAs inhibits HDAC4, which sustains cell proliferation by preventing the expression of the cyclin-dependent kinase inhibitor p21Cip1, essential for terminal muscle differentiation [66,67]. This finding is of interest for the RMS context due to the potentiality of therapeutic approaches with HDACs inhibitors [68,69]. Interestingly, miR-29b directly targets HDAC4 during osteoblast differentiation [70], suggesting an intricate complex of miRNAs pathways acting similarly in different tissue contexts. Collectively, these observations suggest that miRNAs can influence gene transcription through the control of several types of epigenetic repressors. Of note, crucial components of molecular pathways related to RMS aggressiveness, such as IGF and RAS, can be post-transcriptionally downregulated by pro-myogenic miRNAs. Indeed, (i) miR-1 and miR-133 target IGF receptor 1, thus avoiding aberrant muscle hypertrophy [71,72]; (ii) miR-214, which is repressed by EZH2 in proliferating myoblasts, is able to favor myogenesis by downregulating the anti-myogenic N-RAS oncogene [73,74].
In addition to myomiRs, there are non-muscle-specific miRNAs that participate to skeletal muscle differentiation such as miR-181a/miR-181b, miR-27a, miR-27b, miR-26a and miR-29b2/miR-29c. Wang and colleagues provided the first evidence of an epigenetic deregulation of miRNAs in RMS discovering a regulatory circuitry between miR-29b2/miR-29c and the PcG protein YY1 [60]. The same authors had previously demonstrated that during the expansion of myogenic precursors, NF-kB inhibited terminal differentiation maintaining a high level of YY1, which, in turn, repressed the expression of myofibrillary genes favoring cell precursor proliferation [75]. Therefore, reasoning that miRNAs are regulators of myogenesis, the authors investigated whether the anti-differentiation effect of YY1 was at least in part related to the repression of pro-myogenic miRNAs [60]. Indeed, they identified miR-29b2/miR-29c cluster on chromosome 1 being repressed by YY1 in proliferating myoblasts (Figure 4). This repression involved the recruitment of both HDAC1 and the EZH2 PcG protein, which deacetylated and trimethylated, respectively, the Lys 27 on histone H3 in a highly conserved region 20 kb upstream of the miR-29b2/miR-29c gene locus. Under myogenic cues, miR-29b2/miR-29c gene cluster is expressed and directly targeted YY1 reinforcing myogenesis. Of note, in myogenic precursors undergoing early-stage differentiation, YY1 and EZH2 have been shown to work in concert to repress the transcription of late-stage muscle-specific genes such as Muscle Creatine Kinase (MCK) and Myosin Heavy Chain (MHC) to avoid premature differentiation [76]. Therefore, a fine tuning between anti- and pro-myogenic molecular stimuli underlies a proper myogenesis during which both epigenetic and miRNAs pathways appeared highly interconnected.
The miR-29b2/miR-29c-YY1 epigenetic negative feedback circuitry [60] was shown by the authors to be disrupted in RMS cells, in which YY1 and EZH2 over-expression resulted in persistent activation of stemness maintenance program. The tumor suppressor role of miR-29b2/miR-29c was clearly evidenced by gain-of-function experiments demonstrating that forced over-expression of this miRNA cluster in RMS cells is sufficient to impair the tumorigenic properties both in vitro and in vivo by repressing YY1 expression. Consistent with these observations, tumor tissues from RMS patients showed upregulation of YY1 and EZH2 [60]. In line with this report, preliminary results from our laboratory showed that EZH2 downregulation in RMS cells impairs tumorigenesis, thereby allowing the de-repression of several tumor suppressor miRNAs, including the miR-29b2/miR-29c cluster.
Interestingly, even if YY1 binding sites were not found in the promoter of miR-29a/miR-29b1, this miRNA cluster appeared downregulated in primary sarcoma samples as compared to skeletal muscle tissues [77]. Interestingly, the miR-29 family has been shown to directly target DNMT3A and DNMT3B in several types of cancer, thus suggesting a link between their reduced expression and pathological gene hyper-methylation [78,79].
Altogether, these results highlight the importance of bi-univocal regulation of epigenetic molecules and miRNAs in skeletal muscle differentiation that should be considered also in the context of RMS in which these pathways are deregulated.
5. Neuroblastoma
NB is a neuroectodermal tumor that originates from precursor cells of the sympathetic nervous system and represents the third leading cause of cancer-related death in childhood [80]. The heterogeneous clinical behavior, ranging from spontaneous regression to rapid progression, is attributable to biological and genetic characteristics of the tumor.
NB diagnosed in patients under one year of age usually has a favorable prognosis since tumor cells undergo spontaneous differentiation or regression, whereas NB occurring in patients over one year of age tend to grow aggressively resulting in a fatal outcome. The prognosis of stage I-III NB, with a tumor confined to the originating organ or surrounding tissue, is quite favorable, whereas that of stage IV NB, where the tumor is metastatic, is dismal. Stage IV-S NB is a metastatic disease seen exclusively in infants, which is associated with high survival rate due to the spontaneous maturation and regression of tumor cells. Nevertheless, since disease and risk staging are not comprehensive and fully precise, they should be considered as surrogate markers of the underlying tumor biology.
NB cells correspond to adrenal neuroblasts arrested at different stages of sympathoadrenal development, thus representing multipotent progenitor cells with specific tumorigenic potential [81,82]. The degree of differentiation of NB is another important factor for establishing prognosis. Based on this, NB tumors are classified in different risk categories spanning from more mature and benign ganglioneuromas (GN), to intermediate and potentially malignant ganglioneuroblastomas (GNB), to undifferentiated NB, always malignant with worst prognosis. The factors responsible for malignant transformation from sympathetic neuroblasts into neuroblastoma cells are not well understood. In several NB cell lines, all-trans retinoic acid (ATRA)-induced differentiation is associated with increased expression of neurotrophic receptors, including Trk family receptors and glial cell-derived neurotrophic factor receptor, Ret. Of note, ATRA is a compound related to 13-cis-retinoic acid that is used as differentiating agent in children with high-risk NB.
From a clinical point of view, the presence of any segmental chromosomal imbalances correlates with a more aggressive phenotype, whereas tumors containing mostly whole chromosome gains or losses are associated with a benign phenotype and high propensity for spontaneous regression or differentiation. The most widely characterized cytogenetic alterations in NB tumors include amplification of the MYCN oncogenic transcription factor at chromosome band 2p24, LOH or rearrangements of the distal portion of the short arm of chromosome 1 (1p31-term), chromosome 3 (3p22) and chromosome 11 (11q23), or gains of chromosome arm 1q or 17q. Besides these chromosomal/molecular abnormalities, gains of chromosomes 4q, 6p, 7q, 11q and 18q, amplification of MDM2 and MYC genes and LOH at 14q, 10q and 19q13 have also been described [83]. In particular, loss of chromosome 1p region, occurring mainly through an unbalanced translocation that results in the gain of 17q [84], arises preferentially in tumors with MYCN amplification [85]. Some of these genetic alterations were proven to be independently associated with a poor clinical outcome. The region of 1p, lost in NB tumors, is quite large and contains multiple genes that have been shown to contribute to NB pathogenesis [86,87]. Similarly, the minimal common region of gain at distal 17q23 has been shown to contain at least 15 genes that remain to be investigated [88]. Of note, MYCN is one of the major players in normal neural crest differentiation, suggesting that its amplification/deregulation is the result of a developmental defect that probably has occurred during embryonic development [89]. However, although MYCN amplification is considered the most important prognostic marker of highly aggressive tumors; it is present in less than 30% of NB tumors [90].
More recently, activating mutations in the anaplastic lymphoma kinase (ALK) gene have been associated with the majority of hereditary NB and a 10% of sporadic NB cases [91–94]. ALK is a receptor tyrosine kinase involved in several other human cancers, including anaplastic large-cell lymphoma and non-small cell lung cancer [95–97]. ALK signaling drives cell transformation in vitro and in vivo through several pathways such as cell-cycle, survival and cell migration [98,99]. Nevertheless, additional molecular alterations concur to NB pathogenesis and their identification is essential to improve the prognostic classification of NB patients.
In the attempt to improve the risk stratification of NB subtypes, several groups have characterized and correlated methylation profiling of biologically and clinically different subgroups of NB patients with clinical risk factors and survival (for a detailed review see [100]). The first DNA methylation studies in NB have revealed that silencing of caspase 8 and RAS-association domain family 1 isoform A (RASSF1A) are important in the development and progression of disease [101,102]. Both genes are often methylated in primary NB cells and their methylation status negatively correlates with survival.
Recent advances in genome-wide methylation screening methodologies, such as re-expression analysis after treatment with 5-aza-2′-deoxycytidine (DAC), DNA methylation promoter assay after affinity-based capture, methylation microarray after bisulfate treatment and next-generation sequencing techniques, have allowed the identification of 75 different DNA methylation biomarkers involved in fundamental biological processes operative in NB ([103–105] and reviewed in [100]).
Epigenetic inactivation of miRNAs with tumor-suppressor activities is also recognized as a major hallmark of NB tumors. A recent study from Chavali group [106] showed that the majority of the miRNA genes are flanked by scaffold/matrix-attachment region (S/MAR) elements that regulate their tissue and cell type-specific expression by binding to epigenetic regulators MAR binding proteins. In this study, the authors showed that the miR-17-92 cluster, a well-known example of oncomiR that is over-expressed in high-risk NB [41], has two conserved MARs elements, one upstream and one downstream the cluster, being the former strongly bound by HMG I/Y protein, a chromatin modulator that promotes an open conformation facilitating mRNA transcription. Consistent with this finding, the miR-17-92 cluster expression was down-regulated in cells interfered for HMG I/Y family expression [106].
5.1. Epigenetically Deregulated miRNAs in Neuroblastoma
Recent studies from Stallings’ group revealed extensive epigenomic changes in NB cells upon ATRA exposure, a phenomenon that is associated with a complex series of molecular events, including modifications of both chromatin compaction and DNA methylation status [107]. Intriguingly, in a previous paper, Das and colleagues showed that several miRNAs that are upmodulated as a consequence of ATRA treatment target DNA methyltransferases involved in the process of ATRA-induced differentiation of NB cell lines [108]. More recently, the same authors revealed that DNA methylation changes occurred during ATRA treatment include several regulatory regions of tumor suppressor miRNAs [109]. The authors identified 67 miRNAs sensitive to the effects of DNA methylation in 18 primary NB tumors and four NB cell lines by the combined use of methylated DNA immunoprecipitation, miRNA and mRNA target analysis. Of note, a relative high proportion of these epigenetically silenced miRNAs (42%) were significantly associated with poor patient survival when under-expressed in tumors, whereas other 10 miRNA (15%) were found hyper-methylated in favorable tumors and over-expressed in tumors from patients with poor survival. Remarkably, not only miRNAs, but also their predicted gene targets, were significantly associated with poor patient survival when over-expressed in tumors. In particular, miRNA-340 was functionally inactivated by DNA methylation, re-expressed in NB cell lines following DAC treatment and significantly associated with poor survival when under-expressed in primary NB tumors. According to the NB cell line used, over-expression of miR-340 induced either apoptosis or differentiation by targeting SOX2, an SRY box containing a transcription factor family member that acts in regulating the maintenance and differentiation of neural stem cells [109].
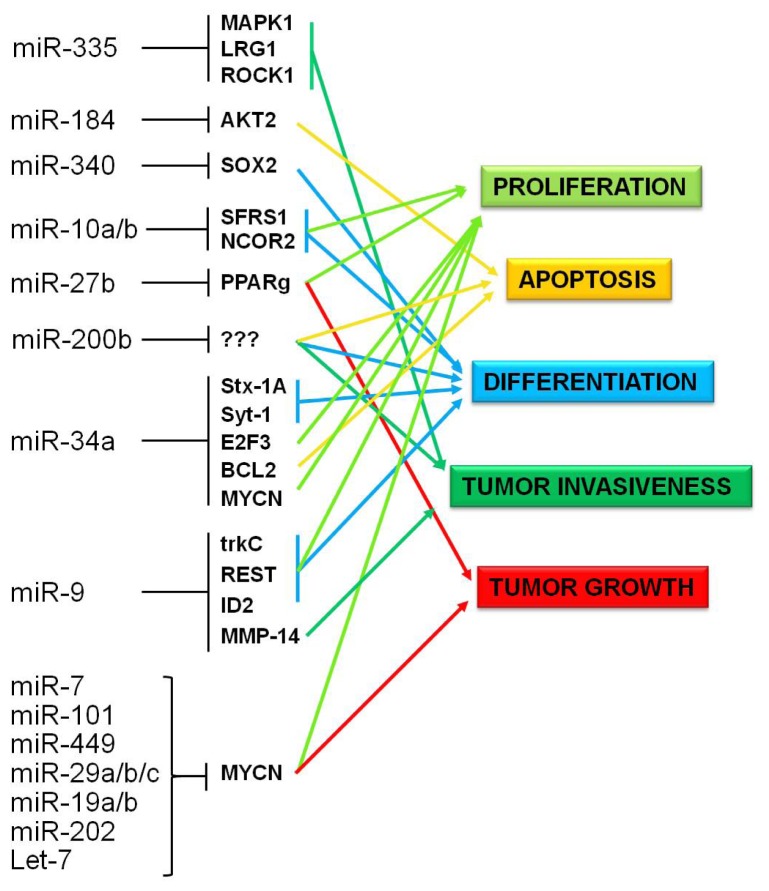
Several of the epigenetically regulated miRNAs identified in this integrated analysis were previously found to negatively impact NB growth both in vivo and in vitro (Figure 5). The main findings regarding their implications in NB pathogenesis are described as follows.
Figure 5.
Scheme of cellular pathways affected by methylation-sensitive miRNAs in Neuroblastoma. Experimental validated gene targets and pathways affected by altered expression of methylation-sensitive miRNAs are indicated.
MiR-10a and -10b were found to induce NB differentiation through multiple gene targeting (for a detailed review see [110]). Meseguer et al. demonstrated that these microRNAs directly target the SR-family splicing factor (SFRS1), a regulator of alternative splicing that plays a role also in enhancing translation initiation of mRNAs containing specific SFRS1 binding sequences [111]. Of note, this factor seems to be a proto-oncogene deregulated in many forms of tumor [112]. Foley and colleagues identified the nuclear receptor co-repressor 2 (NCOR2) as the primary target of miR-10a and -10b responsible for causing differentiation [113]. NCOR2 is a transcriptional co-repressor that recruits a complex of proteins that include SIN3A/B and histone deacetylases HDAC1, HDAC2 and HDAC3 to DNA promoter regions. Interestingly, neural stem cells from mice lacking NCOR2 exhibit extensive neurite outgrowth and reduction in cell proliferation [114]. More intriguingly, siRNA-mediated inhibition of NCOR2 resulted in a significant increase in miR-10a level that suggests a possible regulatory feedback loop in the differentiation process [113].
A number of these epigenetically regulated miRNAs were previously found to be involved in a complex gene network involving MYCN. A study from Buechner and colleagues demonstrated that the tumor suppressor miRNAs let-7 and miR-101 inhibit proliferation and clonogenic growth of Kelly NB cell line by targeting MYCN [115]. Furthermore, they experimentally validate miR-449, miR-19a/b, miR-29a/b/c, and miR-202 as direct MYCN-targeting miRNAs. A very recent paper by Molenaar and colleagues, elegantly demonstrated the existence of a LIN28B-let-7-MYCN axis in NB [116]. Using a mouse model with neural crest-specific over-expression of LIN28B, these authors showed that LIN28B drives NB upregulating MYCN protein through let-7 repression. Notably, MYCN has been recently discovered to bind and transcriptionally downregulate another epigenetically controlled miRNA, miR-335, which in turn regulates genes in the TGF-β non-canonical pathway, such as the Rho-associated coiled-coil containing protein (ROCK1), MAPK1 and putative member LRG1, leading to inhibition of invasiveness and migratory potential of NB cells [117]. The same group had previously discovered a pro-apoptotic effect of miR-184 both in vitro and in vivo, through the direct targeting of AKT2, a serine/threonine kinase active downstream of the PI3K pathway. Interestingly, MYCN could exert its tumorigenic effect also by suppressing either directly or indirectly the same miRNA [118,119].
Several groups identified miR-542-5p as a putative tumor suppressor, whose expression has a prognostic value and might be important in NB tumor biology [120–122]. Of note, miR-542-5p is predicted to target TBR1, a gene essential for proper development of neurons. Functional studies that address this or other putative targets should be performed in the future.
The brain specific miR-9 was demonstrated by Laneve et al. to play an important role in controlling NB cell proliferation through a regulatory circuit involving TRKc and other two miRs, miR-125a and - 125b [123]. The same authors discovered a regulatory feedback mechanism involving miR-9 and the neuro-restrictive silencer factor REST, suggesting a fine interplay for the maintenance of the neuronal differentiation program [124]. More recently, Nasi and colleagues found that the transcription factor ID2, which is involved in the self-renewal and proliferation of neural precursor cells, is a target of miR-9 [125]. At the same time, another group demonstrated that miR-9 reduced matrix metalloproteinase (MMP)-14 level by inhibiting the invasion, metastasis, and angiogenesis of SH-SY5Y and SK-N-SH NB cell lines both in vitro and in vivo[126].
Lee and colleagues showed that the epigenetically regulated miR-27b acts as a tumor suppressor in NB by inhibiting the tumor-promoting function of peroxisome proliferators-activated receptor (PPAR)y and blocking cell growth in vitro and tumor growth in mouse xenografts [127]. In addition, miR-27b indirectly regulates also NF-kB activity and transcription of inflammatory target genes, which triggers an increased inflammatory response.
As described above, LOH of 1p36 is commonly found in NB with MYCN amplification and is associated with poor outcome. Of note, five microRNAs (miR-200a, miR-200b, miR-429, miR-34a and miR-551a) map within the first 10Mb on chromosome 1 short arm (1p36.22 to 1pter), suggesting that the loss of these miRNAs could contribute to the acquisition of an aggressive NB phenotype.
MiR-200b was originally identified through a positional gene candidate approach looking for miRNAs that map within chromosomal regions frequently altered in NB [128]. Conversely, Ragusa and colleagues discovered that the miR-200b region is unaffected by the frequent deletions involving 1p36 in the NB cell lines analyzed [129]. Moreover, they found a CpG island near the gene-encoding miR-200b and showed that, upon treatment with demethylating agents, miR-200b levels were upregulated in six NB cell lines. Finally, they provided several evidences supporting a role for miR-200b in NB cell invasiveness, differentiation and apoptosis.
MiR-34a expression is silenced in several types of cancer due to aberrant CpG methylation of its promoter [130]. In NB cell lines and primary NB tumors, miR-34a is absent or expressed at low levels, while it is upregulated in a dose-dependent manner following ATRA treatment [131]. Given that miR-34a has been implicated in NB growth inhibition, and mutations of the retained allele are not a common mechanism towards achieving biallelic inactivation, it is plausible that other mechanisms such as epigenetic regulation could contribute for loss of miR-34a expression in NB. Of note, miR-34a expression has been shown to increase after HDAC inhibition in a bladder cancer cell line [132]. It will be of interest to validate this finding also in the NB context since several studies demonstrated the involvement of this microRNA in NB pathogenesis. Welch and colleagues demonstrated a tumor suppressive role for miR-34a through the transcription factor E2F3 targeting [131]. Moreover, Wei et al. provided evidence that MYCN is a direct target of miR-34a, as further confirmed by a functional screen study by Cole et al., which also demonstrated a BCL2 direct targeting [128,133]. Recently, synaptotagmin I (Syt-I) and syntaxin 1A (Stx-1A), two proteins involved in synaptogenesis and neuronal differentiation, were found to be targets of miR-34a [134].
All these findings reveal a network of epigenetic pathways and miRNA interactions whose dysregulation contributes to NB, and that has translational consequences for the management of the disease.
6. Translational Perspectives and Conclusions
The majority of miRNAs aberrantly downregulated in RMS and NB behave, when re-expressed, as tumor suppressors re-establishing a proper differentiation program. Therefore, they represent promising therapeutic targets. Moreover, miRNAs detection in cancer patients could represent a powerful prognostic and diagnostic tool. A miRNA signature has been recently reported for RMS primary samples by two groups [77,135]. Intriguingly, the first group suggested that an embryonal sample had been previously misdiagnosed allowing a re-evaluation of the tumor followed by a diagnosis as alveolar [77]. The second group showed that miRNA expression clusterings in RMS samples are correlated with PAX3/FOXO1, PAX7/FOXO1 and embryonal subgroups, and, thus, are potentially useful for risk stratification [135].
Recently, miRNA signatures have been shown to be related also to NB prognosis. Lin and colleagues found that, using a combination of 15 biomarkers that consist of 12 miRNAs’ signature, expression levels of Dicer and Drosha and age at diagnosis, it was possible to segregate 66 NB patients into four distinct patterns that were highly predictive of clinical outcome [136]. Subsequently, a signature of 25 miRNAs was built and validated on an independent set of 304 frozen tumor samples and 75 archived formalin-fixed paraffin-embedded samples. This signature was significantly able to discriminate the patients with respect to progression-free and overall survival [137].
Furthermore, the possibility to detect and quantify miRNAs in body fluids whose profile mirrors physiological and pathological condition could also represent a reliable method to improve prognosis and diagnosis [52,138,139].
MiRNAs re-expression in tumors rises doubts regarding delivery, efficacy and safety of these molecules in vivo. Viral and non-viral vectors have shown pre-clinical feasibility and efficacy in animal models including primates [36,140–145]. However, their application on human patients could induce side effects linked to their immunogenicity or could be ineffective due to lack of specificity (reviewed in [146]). The use of nanoparticles represents an efficient system to deliver cDNA to cells and, therefore, it could be potentially useful for the delivery of miRNAs in vivo. Indeed, a first promising study using nanoparticles encapsulating miR-34a and conjugated to a GD2 antibody demonstrate the feasibility of a targeted delivery miRNA-based therapy for NB [147].
Based on these observations, therapeutic approaches able to modulate miRNA gene expression targeting epigenetic regulators present several advantages. Conversely to DNA mutations, epigenetic modifications are reversible and responsive to specific compounds, which gave promising results in clinical trials for adult tumors. Indeed, low doses of DNA methyltransferases inhibitors azacitidine (AZA) and DAC have shown therapeutic effects in myelodysplasia/leukemia as well as in lung cancer patients [148–153]. It is noteworthy that older trials with high doses of epigenetic inhibitors have highlighted extreme toxicities and no effect on epigenome [154,155]. Very recently, an elegant work of Tsai et al., investigated the mechanisms involved in the efficacy of low nanomolar doses of DAC and AZA in preclinical models of acute myeloid leukemia, breast, colon and lung cancers [156]. The authors showed that high-dose treatments resulted in high cytotoxic effects on tumor cells. Nevertheless, residual cells engrafted in immunodeficient mice were still able to grow and give tumors. Conversely, low concentrations of AZA or DAC reduced self-renewal of tumor cells both in vitro and in vivo, sustaining global DNA demethylation and re-expression of anti-tumor master gene pathways [156]. These results strongly confirm the potential efficacy of an epigenetic therapy that could re-express tumor suppressor genes and miRNAs.
Moreover, epigenetic targeted therapy with inhibitors of both DNA methyltransferases and HDACs, has shown anti-tumor effectiveness combined with a restored expression of tumor suppressor genes in preclinical models [157–159]. More important, well-tolerated combination regimens for low-dose AZA and HDAC inhibitors have been found effective in patients with myelodysplasia/leukemia [160,161]. Finally, very encouraging results have been reported in a phase I/II clinical trial on the use of a combined epigenetic low-dose therapy in recurrent metastatic non-small cell lung (NSCL) cancer refractory to conventional therapy [153]. In brief, AZA and entinostat, an inhibitor that blocks HDAC1-3 and HDAC9 function, were used on 45 NSCL patients, resulting in limited side effects while having efficacy on the aberrant epigenome of tumor cells. These findings suggest the potential use of these compounds also in solid cancers.
Novel agents that inhibit histone methyltransferases among which EZH2 are of particular interest for future applications since they do not require cell division to target cancer cells [162,163]. These compounds have been shown to synergize with other epigenetic agents in preclinical studies, representing promising drugs in order to de-repress EZH2 targeted miRNAs [164,165].
However, as reported for other targeted therapies, escape strategies for the miRNA re-expression approach could select resistant cells expressing mRNAs with mutated miRNA binding sites in their 3′UTRs. Moreover, PAX3/or PAX7/FOXO1 mRNAs expressed in fusion-positive alveolar RMS, being devoid of 3′UTR regions of PAX genes, are resistant to miRNAs’ post-transcriptional regulation. In addition, the de-repression of oncogenes could be a potential side effect of an epigenetic therapy [166]. Therefore, although the field of investigation in the epigenetic treatment of cancer appears very promising, further studies are needed to enhance the knowledge on the epigenome and its regulation both in normal and tumor contexts.
Acknowledgments
This work was supported by grants from: Associazione Italiana per la Ricerca sul Cancro (AIRC IG 10338) to R.R. and the IG grant AIRC to D.F., Ministero della Salute Italiano (Ricerca Corrente) to R.R, D.F. and F.L., and partly supported by the AIRC Special Project 5 × 1000 to F.L.
Footnotes
Conflict of Interest
The authors declare no conflict of interest.
References
- 1.Iorio M.V., Croce C.M. MicroRNA involvement in human cancer. Carcinogenesis. 2012;33:1126–1133. doi: 10.1093/carcin/bgs140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Crippa S., Cassano M., Sampaolesi M. Role of miRNAs in muscle stem cell biology: proliferation, differentiation and death. Curr. Pharmaceut. Des. 2012;18:1718–1729. doi: 10.2174/138161212799859620. [DOI] [PubMed] [Google Scholar]
- 3.Mondol V., Pasquinelli A.E. Let’s make it happen: the role of let-7 microRNA in development. Curr. Top. Dev. Biol. 2012;99:1–30. doi: 10.1016/B978-0-12-387038-4.00001-X. [DOI] [PubMed] [Google Scholar]
- 4.Mansfield J.H., McGlinn E. Evolution, expression, and developmental function of Hox-embedded miRNAs. Curr. Top. Dev. Biol. 2012;99:31–57. doi: 10.1016/B978-0-12-387038-4.00002-1. [DOI] [PubMed] [Google Scholar]
- 5.Sokol N.S. The role of microRNAs in muscle development. Curr. Top. Dev. Biol. 2012;99:59–78. doi: 10.1016/B978-0-12-387038-4.00003-3. [DOI] [PubMed] [Google Scholar]
- 6.Cochella L., Hobert O. Diverse functions of microRNAs in nervous system development. Curr. Top. Dev. Biol. 2012;99:115–143. doi: 10.1016/B978-0-12-387038-4.00005-7. [DOI] [PubMed] [Google Scholar]
- 7.O’Connell R.M., Baltimore D. MicroRNAs and hematopoietic cell development. Curr. Top. Dev. Biol. 2012;99:145–174. doi: 10.1016/B978-0-12-387038-4.00006-9. [DOI] [PubMed] [Google Scholar]
- 8.Boettger T., Braun T. A new level of complexity: The role of microRNAs in cardiovascular development. Circ. Res. 2012;110:1000–1013. doi: 10.1161/CIRCRESAHA.111.247742. [DOI] [PubMed] [Google Scholar]
- 9.Bell J.T., Spector T.D. A twin approach to unraveling epigenetics. Trends Genet. 2011;27:116–125. doi: 10.1016/j.tig.2010.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baylin S.B. DNA methylation and gene silencing in cancer. Nat. Clin. Pract. Oncol. 2005;2:S4–S11. doi: 10.1038/ncponc0354. [DOI] [PubMed] [Google Scholar]
- 11.Martin-Subero J.I. How epigenomics brings phenotype into being. Pediatr. Endocrinol. Rev. 2011;9:506–510. [PubMed] [Google Scholar]
- 12.Richly H., Aloia L., Di Croce L. Roles of the Polycomb group proteins in stem cells and cancer. Cell Death. Dis. 2011;2:e204. doi: 10.1038/cddis.2011.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Esteller M. Non-coding RNAs in human disease. Nat. Rev. 2011;12:861–874. doi: 10.1038/nrg3074. [DOI] [PubMed] [Google Scholar]
- 14.Elbashir S.M., Harborth J., Lendeckel W., Yalcin A., Weber K., Tuschl T. Duplexes of 21-nucleotide RNAs mediate RNA interference in cultured mammalian cells. Nature. 2001;411:494–498. doi: 10.1038/35078107. [DOI] [PubMed] [Google Scholar]
- 15.Lewis B.P., Burge C.B., Bartel D.P. Conserved seed pairing, often flanked by adenosines, indicates that thousands of human genes are microRNA targets. Cell. 2005;120:15–20. doi: 10.1016/j.cell.2004.12.035. [DOI] [PubMed] [Google Scholar]
- 16.Vasudevan S., Tong Y., Steitz J.A. Switching from repression to activation: microRNAs can up-regulate translation. Science. 2007;318:1931–1934. doi: 10.1126/science.1149460. [DOI] [PubMed] [Google Scholar]
- 17.Orom U.A., Nielsen F.C., Lund A.H. MicroRNA-10a binds the 5′UTR of ribosomal protein mRNAs and enhances their translation. Mol. Cell. 2008;30:460–471. doi: 10.1016/j.molcel.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 18.Duursma A.M., Kedde M., Schrier M., le Sage C., Agami R. miR-148 targets human DNMT3b protein coding region. RNA. 2008;14:872–877. doi: 10.1261/rna.972008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Place R.F., Li L.C., Pookot D., Noonan E.J., Dahiya R. MicroRNA-373 induces expression of genes with complementary promoter sequences. Proc. Natl. Acad. Sci. USA. 2008;105:1608–1613. doi: 10.1073/pnas.0707594105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee Y., Kim M., Han J., Yeom K.H., Lee S., Baek S.H., Kim V.N. MicroRNA genes are transcribed by RNA polymerase II. EMBO J. 2004;23:4051–4060. doi: 10.1038/sj.emboj.7600385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Borchert G.M., Lanier W., Davidson B.L. RNA polymerase III transcribes human microRNAs. Nat. Struct. Mol. Biol. 2006;13:1097–1101. doi: 10.1038/nsmb1167. [DOI] [PubMed] [Google Scholar]
- 22.Winter J., Jung S., Keller S., Gregory R.I., Diederichs S. Many roads to maturity: MicroRNA biogenesis pathways and their regulation. Nat. Cell Biol. 2009;11:228–334. doi: 10.1038/ncb0309-228. [DOI] [PubMed] [Google Scholar]
- 23.Butcher J., Abdou H., Morin K., Liu Y. Micromanaging oligodendrocyte differentiation by noncoding RNA: toward a better understanding of the lineage commitment process. J. Neurosci. 2009;29:5365–5366. doi: 10.1523/JNEUROSCI.5976-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gangaraju V.K., Lin H. MicroRNAs: Key regulators of stem cells. Nat. Rev. Mol. Cell Biol. 2009;10:116–125. doi: 10.1038/nrm2621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang Y., Russell I., Chen C. MicroRNA and stem cell regulation. Curr. Opin. Mol. Ther. 2009;11:292–298. [PubMed] [Google Scholar]
- 26.Mallanna S.K., Rizzino A. Emerging roles of microRNAs in the control of embryonic stem cells and the generation of induced pluripotent stem cells. Dev. Biol. 2010;344:16–25. doi: 10.1016/j.ydbio.2010.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Laurent L.C. MicroRNAs in embryonic stem cells and early embryonic development. J. Cell Mol. Med. 2008;12:2181–2188. doi: 10.1111/j.1582-4934.2008.00513.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Calin G.A., Croce C.M. MicroRNA signatures in human cancers. Nat. Rev. Cancer. 2006;6:857–866. doi: 10.1038/nrc1997. [DOI] [PubMed] [Google Scholar]
- 29.Garzon R., Fabbri M., Cimmino A., Calin G.A., Croce C.M. MicroRNA expression and function in cancer. Trends Mol. Med. 2006;12:580–587. doi: 10.1016/j.molmed.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 30.Iorio M.V., Piovan C., Croce C.M. Interplay between microRNAs and the epigenetic machinery: An intricate network. Biochim. Biophys. Acta. 2010;1799:694–701. doi: 10.1016/j.bbagrm.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 31.Fabbri M., Calore F., Paone A., Galli R., Calin G.A. Epigenetic Regulation of miRNAs in Cancer. Adv. Exp.Med. Bio. 2013;754:137–148. doi: 10.1007/978-1-4419-9967-2_6. [DOI] [PubMed] [Google Scholar]
- 32.Chhabra R., Dubey R., Saini N. Cooperative and individualistic functions of the microRNAs in the miR-23a~27a~24–2 cluster and its implication in human diseases. Mol. Cancer. 2010;9:232. doi: 10.1186/1476-4598-9-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Di Leva G., Croce C.M. Roles of small RNAs in tumor formation. Trends Mol. Med. 2010;16:257–267. doi: 10.1016/j.molmed.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Perera R.J., Ray A. Epigenetic regulation of miRNA genes and their role in human melanomas. Epigenomics. 2012;4:81–90. doi: 10.2217/epi.11.114. [DOI] [PubMed] [Google Scholar]
- 35.Ferretti E., De Smaele E., Miele E., Laneve P., Po A., Pelloni M., Paganelli A., Di Marcotullio L., Caffarelli E., Screpanti I., et al. Concerted microRNA control of Hedgehog signalling in cerebellar neuronal progenitor and tumour cells. EMBO J. 2008;27:2616–2627. doi: 10.1038/emboj.2008.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kota J., Chivukula R.R., O’Donnell K.A., Wentzel E.A., Montgomery C.L., Hwang H.W., Chang T.C., Vivekanandan P., Torbenson M., Clark K.R., et al. Therapeutic microRNA delivery suppresses tumorigenesis in a murine liver cancer model. Cell. 2009;137:1005–1017. doi: 10.1016/j.cell.2009.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Huang T.H., Esteller M. Chromatin remodeling in mammary gland differentiation and breast tumorigenesis. Cold Spring Harb. Perspect. Biol. 2010;2:a004515. doi: 10.1101/cshperspect.a004515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Guessous F., Zhang Y., Kofman A., Catania A., Li Y., Schiff D., Purow B., Abounader R. microRNA-34a is tumor suppressive in brain tumors and glioma stem cells. Cell Cycle. 2010;9:6. doi: 10.4161/cc.9.6.10987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Taulli R., Bersani F., Ponzetto C. Micro-orchestrating differentiation in cancer. Cell Cycle. 2010;9:918–922. doi: 10.4161/cc.9.5.10864. [DOI] [PubMed] [Google Scholar]
- 40.Wiggins J.F., Ruffino L., Kelnar K., Omotola M., Patrawala L., Brown D., Bader A.G. Development of a lung cancer therapeutic based on the tumor suppressor microRNA-34. Cancer Res. 2010;70:5923–5930. doi: 10.1158/0008-5472.CAN-10-0655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fontana L., Fiori M.E., Albini S., Cifaldi L., Giovinazzi S., Forloni M., Boldrini R., Donfrancesco A., Federici V., Giacomini P., et al. Antagomir-17–5p abolishes the growth of therapy-resistant neuroblastoma through p21 and BIM. PloS One. 2008;3:e2236. doi: 10.1371/journal.pone.0002236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ciarapica R., Russo G., Verginelli F., Raimondi L., Donfrancesco A., Rota R., Giordano A. Deregulated expression of miR-26a and Ezh2 in rhabdomyosarcoma. Cell Cycle. 2009;8:172–175. doi: 10.4161/cc.8.1.7292. [DOI] [PubMed] [Google Scholar]
- 43.Taulli R., Bersani F., Foglizzo V., Linari A., Vigna E., Ladanyi M., Tuschl T., Ponzetto C. The muscle-specific microRNA miR-206 blocks human rhabdomyosarcoma growth in xenotransplanted mice by promoting myogenic differentiation. J. Clin. Invest. 2009;119:8, 2366–2378. doi: 10.1172/JCI38075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Calin G.A., Sevignani C., Dumitru C.D., Hyslop T., Noch E., Yendamuri S., Shimizu M., Rattan S., Bullrich F., Negrini M., et al. Human microRNA genes are frequently located at fragile sites and genomic regions involved in cancers. Proc. Natl. Acad. Sci. USA. 2004;101:2999–3004. doi: 10.1073/pnas.0307323101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Loeb D.M., Thornton K., Shokek O. Pediatric soft tissue sarcomas. Surg. Clin. N. Am. 2008;88:615–627. doi: 10.1016/j.suc.2008.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tapscott S.J., Thayer M.J., Weintraub H. Deficiency in rhabdomyosarcomas of a factor required for MyoD activity and myogenesis. Science. 1993;259:1450–1453. doi: 10.1126/science.8383879. [DOI] [PubMed] [Google Scholar]
- 47.De Giovanni C., Landuzzi L., Nicoletti G., Lollini P.L., Nanni P. Molecular and cellular biology of rhabdomyosarcoma. Future Oncol. 2009;5:1449–1475. doi: 10.2217/fon.09.97. [DOI] [PubMed] [Google Scholar]
- 48.Kohashi K., Oda Y., Yamamoto H., Tamiya S., Takahira T., Takahashi Y., Tajiri T., Taguchi T., Suita S., Tsuneyoshi M. Alterations of RB1 gene in embryonal and alveolar rhabdomyosarcoma: special reference to utility of pRB immunoreactivity in differential diagnosis of rhabdomyosarcoma subtype. J. Cancer Res. Clin. Oncol. 2008;134:1097–1103. doi: 10.1007/s00432-008-0385-3. [DOI] [PubMed] [Google Scholar]
- 49.Crist W.M., Anderson J.R., Meza J.L., Fryer C., Raney R.B., Ruymann F.B., Breneman J., Qualman S.J., Wiener E., Wharam M., et al. Intergroup rhabdomyosarcoma study-IV: Results for patients with nonmetastatic disease. J. Clin. Oncol. 2001;19:3091–3102. doi: 10.1200/JCO.2001.19.12.3091. [DOI] [PubMed] [Google Scholar]
- 50.Sorensen P.H., Lynch J.C., Qualman S.J., Tirabosco R., Lim J.F., Maurer H.M., Bridge J.A., Crist W.M., Triche T.J., Barr F.G. PAX3-FKHR and PAX7-FKHR gene fusions are prognostic indicators in alveolar rhabdomyosarcoma: a report from the children’s oncology group. J. Clin. Oncol. 2002;20:2672–2679. doi: 10.1200/JCO.2002.03.137. [DOI] [PubMed] [Google Scholar]
- 51.Wachtel M., Dettling M., Koscielniak E., Stegmaier S., Treuner J., Simon-Klingenstein K., Buhlmann P., Niggli F.K., Schafer B.W. Gene expression signatures identify rhabdomyosarcoma subtypes and detect a novel t(2;2) (q35;p23) translocation fusing PAX3 to NCOA1. Cancer Res. 2004;64:5539–5545. doi: 10.1158/0008-5472.CAN-04-0844. [DOI] [PubMed] [Google Scholar]
- 52.Missiaglia E., Shepherd C.J., Patel S., Thway K., Pierron G., Pritchard-Jones K., Renard M., Sciot R., Rao P., Oberlin O., et al. MicroRNA-206 expression levels correlate with clinical behaviour of rhabdomyosarcomas. Br. J. Cancer. 2010;102:1769–1777. doi: 10.1038/sj.bjc.6605684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Williamson D., Missiaglia E., de Reynies A., Pierron G., Thuille B., Palenzuela G., Thway K., Orbach D., Lae M., Freneaux P., et al. Fusion gene-negative alveolar rhabdomyosarcoma is clinically and molecularly indistinguishable from embryonal rhabdomyosarcoma. J. Clin. Oncol. 2010;28:2151–2158. doi: 10.1200/JCO.2009.26.3814. [DOI] [PubMed] [Google Scholar]
- 54.Davicioni E., Anderson M.J., Finckenstein F.G., Lynch J.C., Qualman S.J., Shimada H., Schofield D.E., Buckley J.D., Meyer W.H., Sorensen P.H., et al. Molecular classification of rhabdomyosarcoma-genotypic and phenotypic determinants of diagnosis: A report from the Children’s Oncology Group. Am. J. Pathol. 2009;174:550–564. doi: 10.2353/ajpath.2009.080631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lae M., Ahn E.H., Mercado G.E., Chuai S., Edgar M., Pawel B.R., Olshen A., Barr F.G., Ladanyi M. Global gene expression profiling of PAX-FKHR fusion-positive alveolar and PAX-FKHR fusion-negative embryonal rhabdomyosarcomas. J. Pathol. 2007;212:143–151. doi: 10.1002/path.2170. [DOI] [PubMed] [Google Scholar]
- 56.Sumegi J., Streblow R., Frayer R.W., Dal Cin P., Rosenberg A., Meloni-Ehrig A., Bridge J.A. Recurrent t(2;2) and t(2;8) translocations in rhabdomyosarcoma without the canonical PAX-FOXO1 fuse PAX3 to members of the nuclear receptor transcriptional coactivator family. Genes Chromosomes Cancer. 2010;49:224–236. doi: 10.1002/gcc.20731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lagha M., Sato T., Regnault B., Cumano A., Zuniga A., Licht J., Relaix F., Buckingham M. Transcriptome analyses based on genetic screens for Pax3 myogenic targets in the mouse embryo. BMC Genom. 2010;11:696. doi: 10.1186/1471-2164-11-696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Seale P., Sabourin L.A., Girgis-Gabardo A., Mansouri A., Gruss P., Rudnicki M.A. Pax7 is required for the specification of myogenic satellite cells. Cell. 2000;102:777–786. doi: 10.1016/s0092-8674(00)00066-0. [DOI] [PubMed] [Google Scholar]
- 59.Rota R., Ciarapica R., Giordano A., Miele L., Locatelli F. MicroRNAs in rhabdomyosarcoma: pathogenetic implications and translational potentiality. Mol. Cancer. 2011;10:120. doi: 10.1186/1476-4598-10-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wang H., Garzon R., Sun H., Ladner K.J., Singh R., Dahlman J., Cheng A., Hall B.M., Qualman S.J., Chandler D.S., et al. NF-kappaB-YY1-miR-29 regulatory circuitry in skeletal myogenesis and rhabdomyosarcoma. Cancer Cell. 2008;14:369–381. doi: 10.1016/j.ccr.2008.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Subramanian S., Kartha R.V. MicroRNA-mediated gene regulations in human sarcomas. Cell Mol. Life Sci. 2012;69:3571–3585. doi: 10.1007/s00018-012-1127-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gagan J., Dey B.K., Dutta A. MicroRNAs regulate and provide robustness to the myogenic transcriptional network. Curr. Opin. Pharmacol. 2012;12:383–388. doi: 10.1016/j.coph.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lu L., Zhou L., Chen E.Z., Sun K., Jiang P., Wang L., Su X., Sun H., Wang H. A Novel YY1-miR-1 regulatory circuit in skeletal myogenesis revealed by genome-wide prediction of YY1-miRNA network. PLoS One. 2012;7:e27596. doi: 10.1371/journal.pone.0027596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Liu N., Williams A.H., Kim Y., McAnally J., Bezprozvannaya S., Sutherland L.B., Richardson J.A., Bassel-Duby R., Olson E.N. An intragenic MEF2-dependent enhancer directs muscle-specific expression of microRNAs 1 and 133. Proc. Natl. Acad. Sci. USA. 2007;104:20844–20849. doi: 10.1073/pnas.0710558105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dey B.K., Gagan J., Dutta A. miR-206 and -486 induce myoblast differentiation by downregulating Pax7. Mol. Cell. Biol. 2010;31:203–214. doi: 10.1128/MCB.01009-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chen J.F., Mandel E.M., Thomson J.M., Wu Q., Callis T.E., Hammond S.M., Conlon F.L., Wang D.Z. The role of microRNA-1 and microRNA-133 in skeletal muscle proliferation and differentiation. Nat. Genet. 2006;38:228–233. doi: 10.1038/ng1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Williams A.H., Valdez G., Moresi V., Qi X., McAnally J., Elliott J.L., Bassel-Duby R., Sanes J.R., Olson E.N. MicroRNA-206 delays ALS progression and promotes regeneration of neuromuscular synapses in mice. Science. 2009;326:1549–1554. doi: 10.1126/science.1181046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hecker R.M., Amstutz R.A., Wachtel M., Walter D., Niggli F.K., Schafer B.W. p21 Downregulation is an important component of PAX3/FKHR oncogenicity and its reactivation by HDAC inhibitors enhances combination treatment. Oncogene. 2010;29:3942–3952. doi: 10.1038/onc.2010.145. [DOI] [PubMed] [Google Scholar]
- 69.Ecke I., Petry F., Rosenberger A., Tauber S., Monkemeyer S., Hess I., Dullin C., Kimmina S., Pirngruber J., Johnsen S.A., et al. Antitumor effects of a combined 5-aza-2′deoxycytidine and valproic acid treatment on rhabdomyosarcoma and medulloblastoma in Ptch mutant mice. Cancer Res. 2009;69:887–895. doi: 10.1158/0008-5472.CAN-08-0946. [DOI] [PubMed] [Google Scholar]
- 70.Li Z., Hassan M.Q., Jafferji M., Aqeilan R.I., Garzon R., Croce C.M., van Wijnen A.J., Stein J.L., Stein G.S., Lian J.B. Biological functions of miR-29b contribute to positive regulation of osteoblast differentiation. J. Biol. Chem. 2009;284:15676–15684. doi: 10.1074/jbc.M809787200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Elia L., Contu R., Quintavalle M., Varrone F., Chimenti C., Russo M.A., Cimino V., De Marinis L., Frustaci A., Catalucci D., et al. Reciprocal regulation of microRNA-1 and insulin-like growth factor-1 signal transduction cascade in cardiac and skeletal muscle in physiological and pathological conditions. Circulation. 2009;120:2377–2385. doi: 10.1161/CIRCULATIONAHA.109.879429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Huang M.B., Xu H., Xie S.J., Zhou H., Qu L.H. Insulin-like growth factor-1 receptor is regulated by microRNA-133 during skeletal myogenesis. PLoS One. 2011;6:e29173. doi: 10.1371/journal.pone.0029173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Olson E.N., Spizz G., Tainsky M.A. The oncogenic forms of N-ras or H-ras prevent skeletal myoblast differentiation. Mol. Cell. Biol. 1987;7:2104–2111. doi: 10.1128/mcb.7.6.2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Liu J., Luo X.J., Xiong A.W., Zhang Z.D., Yue S., Zhu M.S., Cheng S.Y. MicroRNA-214 promotes myogenic differentiation by facilitating exit from mitosis via down-regulation of proto-oncogene N-ras. J. Biol. Chem. 2010;285:26599–26607. doi: 10.1074/jbc.M110.115824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wang H., Hertlein E., Bakkar N., Sun H., Acharyya S., Wang J., Carathers M., Davuluri R., Guttridge D.C. NF-kappaB regulation of YY1 inhibits skeletal myogenesis through transcriptional silencing of myofibrillar genes. Mol. Cell. Biol. 2007;27:4374–4387. doi: 10.1128/MCB.02020-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Caretti G., Di Padova M., Micales B., Lyons G.E., Sartorelli V. The Polycomb Ezh2 methyltransferase regulates muscle gene expression and skeletal muscle differentiation. Genes Dev. 2004;18:2627–2638. doi: 10.1101/gad.1241904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Subramanian S., Lui W.O., Lee C.H., Espinosa I., Nielsen T.O., Heinrich M.C., Corless C.L., Fire A.Z., van de Rijn M. MicroRNA expression signature of human sarcomas. Oncogene. 2008;27:2015–2026. doi: 10.1038/sj.onc.1210836. [DOI] [PubMed] [Google Scholar]
- 78.Fabbri M., Garzon R., Cimmino A., Liu Z., Zanesi N., Callegari E., Liu S., Alder H., Costinean S., Fernandez-Cymering C., et al. MicroRNA-29 family reverts aberrant methylation in lung cancer by targeting DNA methyltransferases 3A and 3B. Proc. Natl. Acad. Sci. USA. 2007;104:15805–15810. doi: 10.1073/pnas.0707628104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Amodio N., Leotta M., Bellizzi D., Di Martino M.T., D’Aquila P., Lionetti M., Fabiani F., Leone E., Gulla A.M., Passarino G., et al. DNA-demethylating and anti-tumor activity of synthetic miR-29b mimics in multiple myeloma. Oncotarget. 2012;3:1246–1258. doi: 10.18632/oncotarget.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hoehner J.C., Gestblom C., Hedborg F., Sandstedt B., Olsen L., Pahlman S. A developmental model of neuroblastoma: differentiating stroma-poor tumors’ progress along an extra-adrenal chromaffin lineage. Lab. Investig. 1996;75:659–675. [PubMed] [Google Scholar]
- 81.Cooper M.J., Hutchins G.M., Cohen P.S., Helman L.J., Mennie R.J., Israel M.A. Human neuroblastoma tumor cell lines correspond to the arrested differentiation of chromaffin adrenal medullary neuroblasts. Cell Growth Differ. 1990;1:149–159. [PubMed] [Google Scholar]
- 82.Gaetano C., Matsumoto K., Thiele C.J. In vitro activation of distinct molecular and cellular phenotypes after induction of differentiation in a human neuroblastoma cell line. Cancer Res. 1992;52:4402–4407. [PubMed] [Google Scholar]
- 83.Brodeur G.M. Neuroblastoma: biological insights into a clinical enigma. Nat. Rev. Cancer. 2003;3:203–216. doi: 10.1038/nrc1014. [DOI] [PubMed] [Google Scholar]
- 84.Van Roy N., Laureys G., Cheng N.C., Willem P., Opdenakker G., Versteeg R., Speleman F. 1;17 translocations and other chromosome 17 rearrangements in human primary neuroblastoma tumors and cell lines. Genes. Chromosomes Cancer. 1994;10:103–114. doi: 10.1002/gcc.2870100205. [DOI] [PubMed] [Google Scholar]
- 85.Fong C.T., Dracopoli N.C., White P.S., Merrill P.T., Griffith R.C., Housman D.E., Brodeur G.M. Loss of heterozygosity for the short arm of chromosome 1 in human neuroblastomas: correlation with N-myc amplification. Proc. Natl. Acad. Sci. USA. 1989;86:3753–3757. doi: 10.1073/pnas.86.10.3753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Janoueix-Lerosey I., Novikov E., Monteiro M., Gruel N., Schleiermacher G., Loriod B., Nguyen C., Delattre O. Gene expression profiling of 1p35–36 genes in neuroblastoma. Oncogene. 2004;23:5912–5922. doi: 10.1038/sj.onc.1207784. [DOI] [PubMed] [Google Scholar]
- 87.Fujita T., Igarashi J., Okawa E.R., Gotoh T., Manne J., Kolla V., Kim J., Zhao H., Pawel B.R., London W.B., et al. CHD5, a tumor suppressor gene deleted from 1p36.31 in neuroblastomas. J. Natl. Cancer Inst. 2008;100:940–949. doi: 10.1093/jnci/djn176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Saito-Ohara F., Imoto I., Inoue J., Hosoi H., Nakagawara A., Sugimoto T., Inazawa J. PPM1D is a potential target for 17q gain in neuroblastoma. Cancer Res. 2003;63:1876–1883. [PubMed] [Google Scholar]
- 89.Van Noesel M.M., Versteeg R. Pediatric neuroblastomas: Genetic and epigenetic “danse macabre”. Gene. 2004;325:1–15. doi: 10.1016/j.gene.2003.09.042. [DOI] [PubMed] [Google Scholar]
- 90.Oppenheimer O., Alaminos M., Gerald W.L. Genomic medicine and neuroblastoma. Expert. Rev. Mol. Diagn. 2003;3:39–54. doi: 10.1586/14737159.3.1.39. [DOI] [PubMed] [Google Scholar]
- 91.Mosse Y.P., Laudenslager M., Longo L., Cole K.A., Wood A., Attiyeh E.F., Laquaglia M.J., Sennett R., Lynch J.E., Perri P., et al. Identification of ALK as a major familial neuroblastoma predisposition gene. Nature. 2008;455:930–935. doi: 10.1038/nature07261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Janoueix-Lerosey I., Lequin D., Brugieres L., Ribeiro A., de Pontual L., Combaret V., Raynal V., Puisieux A., Schleiermacher G., Pierron G., et al. Somatic and germline activating mutations of the ALK kinase receptor in neuroblastoma. Nature. 2008;455:967–970. doi: 10.1038/nature07398. [DOI] [PubMed] [Google Scholar]
- 93.Chen Y., Takita J., Choi Y.L., Kato M., Ohira M., Sanada M., Wang L., Soda M., Kikuchi A., Igarashi T., et al. Oncogenic mutations of ALK kinase in neuroblastoma. Nature. 2008;455:971–974. doi: 10.1038/nature07399. [DOI] [PubMed] [Google Scholar]
- 94.George R.E., Sanda T., Hanna M., Frohling S., Luther W., II, Zhang J., Ahn Y., Zhou W., London W.B., McGrady P., et al. Activating mutations in ALK provide a therapeutic target in neuroblastoma. Nature. 2008;455:975–978. doi: 10.1038/nature07397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Morris S.W., Kirstein M.N., Valentine M.B., Dittmer K.G., Shapiro D.N., Saltman D.L., Look A.T. Fusion of a kinase gene, ALK, to a nucleolar protein gene, NPM, in non-Hodgkin’s lymphoma. Science. 1994;263:1281–1284. doi: 10.1126/science.8122112. [DOI] [PubMed] [Google Scholar]
- 96.Rikova K., Guo A., Zeng Q., Possemato A., Yu J., Haack H., Nardone J., Lee K., Reeves C., Li Y., et al. Global survey of phosphotyrosine signaling identifies oncogenic kinases in lung cancer. Cell. 2007;131:1190–1203. doi: 10.1016/j.cell.2007.11.025. [DOI] [PubMed] [Google Scholar]
- 97.Soda M., Choi Y.L., Enomoto M., Takada S., Yamashita Y., Ishikawa S., Fujiwara S., Watanabe H., Kurashina K., Hatanaka H., et al. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature. 2007;448:561–566. doi: 10.1038/nature05945. [DOI] [PubMed] [Google Scholar]
- 98.Osajima-Hakomori Y., Miyake I., Ohira M., Nakagawara A., Nakagawa A., Sakai R. Biological role of anaplastic lymphoma kinase in neuroblastoma. Am. J. Pathol. 2005;167:213–222. doi: 10.1016/S0002-9440(10)62966-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lim M.S., Carlson M.L., Crockett D.K., Fillmore G.C., Abbott D.R., Elenitoba-Johnson O.F., Tripp S.R., Rassidakis G.Z., Medeiros L.J., Szankasi P., et al. The proteomic signature of NPM/ALK reveals deregulation of multiple cellular pathways. Blood. 2009;114:1585–1595. doi: 10.1182/blood-2009-02-204735. [DOI] [PubMed] [Google Scholar]
- 100.Decock A., Ongenaert M., Vandesompele J., Speleman F. Neuroblastoma epigenetics: From candidate gene approaches to genome-wide screenings. Epigenetics. 2011;6:962–790. doi: 10.4161/epi.6.8.16516. [DOI] [PubMed] [Google Scholar]
- 101.Teitz T., Wei T., Valentine M.B., Vanin E.F., Grenet J., Valentine V.A., Behm F.G., Look A.T., Lahti J.M., Kidd V.J. Caspase 8 is deleted or silenced preferentially in childhood neuroblastomas with amplification of MYCN. Nat. Med. 2000;6:529–535. doi: 10.1038/75007. [DOI] [PubMed] [Google Scholar]
- 102.Astuti D., Agathanggelou A., Honorio S., Dallol A., Martinsson T., Kogner P., Cummins C., Neumann H.P., Voutilainen R., Dahia P., et al. RASSF1A promoter region CpG island hypermethylation in phaeochromocytomas and neuroblastoma tumours. Oncogene. 2001;20:7573–7577. doi: 10.1038/sj.onc.1204968. [DOI] [PubMed] [Google Scholar]
- 103.Murphy D.M., Buckley P.G., Bryan K., Das S., Alcock L., Foley N.H., Prenter S., Bray I., Watters K.M., Higgins D., et al. Global MYCN transcription factor binding analysis in neuroblastoma reveals association with distinct E-box motifs and regions of DNA hypermethylation. PLoS One. 2009;4:e8154. doi: 10.1371/journal.pone.0008154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Buckley P.G., Alcock L., Bryan K., Bray I., Schulte J.H., Schramm A., Eggert A., Mestdagh P., De Preter K., Vandesompele J., et al. Chromosomal and microRNA expression patterns reveal biologically distinct subgroups of 11q-neuroblastoma. Clin. Cancer Res. 2010;16:2971–2978. doi: 10.1158/1078-0432.CCR-09-3215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Caren H., Djos A., Nethander M., Sjoberg R.M., Kogner P., Enstrom C., Nilsson S., Martinsson T. Identification of epigenetically regulated genes that predict patient outcome in neuroblastoma. BMC Cancer. 2011;11:66. doi: 10.1186/1471-2407-11-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Chavali P.L., Funa K., Chavali S. Cis-regulation of microRNA expression by scaffold/matrix-attachment regions. Nucleic Acids Res. 2011;39:6908–6918. doi: 10.1093/nar/gkr303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Angrisano T., Sacchetti S., Natale F., Cerrato A., Pero R., Keller S., Peluso S., Perillo B., Avvedimento V.E., Fusco A., et al. Chromatin and DNA methylation dynamics during retinoic acid-induced RET gene transcriptional activation in neuroblastoma cells. Nucleic Acids Res. 2011;39:1993–2006. doi: 10.1093/nar/gkq864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Das S., Foley N., Bryan K., Watters K.M., Bray I., Murphy D.M., Buckley P.G., Stallings R.L. MicroRNA mediates DNA demethylation events triggered by retinoic acid during neuroblastoma cell differentiation. Cancer Res. 2010;70:7874–7881. doi: 10.1158/0008-5472.CAN-10-1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Das S., Bryan K., Buckley P.G., Piskareva O., Bray I.M., Foley N., Ryan J., Lynch J., Creevey L., Fay J., et al. Modulation of neuroblastoma disease pathogenesis by an extensive network of epigenetically regulated microRNAs. Oncogene. 2012 doi: 10.1038/onc.2012.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Stallings R.L., Foley N.H., Bray I.M., Das S., Buckley P.G. MicroRNA and DNA methylation alterations mediating retinoic acid induced neuroblastoma cell differentiation. Semin. Cancer Biol. 2011;21:283–290. doi: 10.1016/j.semcancer.2011.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Meseguer S., Mudduluru G., Escamilla J.M., Allgayer H., Barettino D. MicroRNAs-10a and -10b contribute to retinoic acid-induced differentiation of neuroblastoma cells and target the alternative splicing regulatory factor SFRS1 (SF2/ASF) J. Biol. Chem. 2011;286:4150–4164. doi: 10.1074/jbc.M110.167817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Karni R., de Stanchina E., Lowe S.W., Sinha R., Mu D., Krainer A.R. The gene encoding the splicing factor SF2/ASF is a proto-oncogene. Nat. Struct. Mol. Biol. 2007;14:185–193. doi: 10.1038/nsmb1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Foley N.H., Bray I., Watters K.M., Das S., Bryan K., Bernas T., Prehn J.H., Stallings R.L. MicroRNAs 10a and 10b are potent inducers of neuroblastoma cell differentiation through targeting of nuclear receptor corepressor 2. Cell Death Differ. 2011;18:1089–1098. doi: 10.1038/cdd.2010.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Jepsen K., Solum D., Zhou T., McEvilly R.J., Kim H.J., Glass C.K., Hermanson O., Rosenfeld M.G. SMRT-mediated repression of an H3K27 demethylase in progression from neural stem cell to neuron. Nature. 2007;450:415–419. doi: 10.1038/nature06270. [DOI] [PubMed] [Google Scholar]
- 115.Buechner J., Tomte E., Haug B.H., Henriksen J.R., Lokke C., Flaegstad T., Einvik C. Tumour-suppressor microRNAs let-7 and mir-101 target the proto-oncogene MYCN and inhibit cell proliferation in MYCN-amplified neuroblastoma. Br. J. Cancer. 2011;105:296–303. doi: 10.1038/bjc.2011.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Molenaar J.J., Domingo-Fernandez R., Ebus M.E., Lindner S., Koster J., Drabek K., Mestdagh P., van Sluis P., Valentijn L.J., van Nes J., et al. LIN28B induces neuroblastoma and enhances MYCN levels via let-7 suppression. Nat. Genet. 2012;44:1199–1206. doi: 10.1038/ng.2436. [DOI] [PubMed] [Google Scholar]
- 117.Lynch J., Fay J., Meehan M., Bryan K., Watters K.M., Murphy D.M., Stallings R.L. MiRNA-335 suppresses neuroblastoma cell invasiveness by direct targeting of multiple genes from the non-canonical TGF-beta signalling pathway. Carcinogenesis. 2012;33:976–985. doi: 10.1093/carcin/bgs114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Foley N.H., Bray I.M., Tivnan A., Bryan K., Murphy D.M., Buckley P.G., Ryan J., O’Meara A., O’Sullivan M., Stallings R.L. MicroRNA-184 inhibits neuroblastoma cell survival through targeting the serine/threonine kinase AKT2. Mol. Cancer. 2010;9:83. doi: 10.1186/1476-4598-9-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Tivnan A., Foley N.H., Tracey L., Davidoff A.M., Stallings R.L. MicroRNA-184-mediated inhibition of tumour growth in an orthotopic murine model of neuroblastoma. Anticancer Res. 2010;30:4391–4395. [PMC free article] [PubMed] [Google Scholar]
- 120.Bray I., Tivnan A., Bryan K., Foley N.H., Watters K.M., Tracey L., Davidoff A.M., Stallings R.L. MicroRNA-542–5p as a novel tumor suppressor in neuroblastoma. Cancer Lett. 2011;303:56–64. doi: 10.1016/j.canlet.2011.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Schulte J.H., Marschall T., Martin M., Rosenstiel P., Mestdagh P., Schlierf S., Thor T., Vandesompele J., Eggert A., Schreiber S., et al. Deep sequencing reveals differential expression of microRNAs in favorable versus unfavorable neuroblastoma. Nucleic Acids Res. 2010;38:5919–5928. doi: 10.1093/nar/gkq342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Schulte J.H., Schowe B., Mestdagh P., Kaderali L., Kalaghatgi P., Schlierf S., Vermeulen J., Brockmeyer B., Pajtler K., Thor T., et al. Accurate prediction of neuroblastoma outcome based on miRNA expression profiles. Int. J. Cancer. 2010;127:2374–2385. doi: 10.1002/ijc.25436. [DOI] [PubMed] [Google Scholar]
- 123.Laneve P., Di Marcotullio L., Gioia U., Fiori M.E., Ferretti E., Gulino A., Bozzoni I., Caffarelli E. The interplay between microRNAs and the neurotrophin receptor tropomyosin-related kinase C controls proliferation of human neuroblastoma cells. Proc. Natl. Acad. Sci. USA. 2007;104:7957–7962. doi: 10.1073/pnas.0700071104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Laneve P., Gioia U., Andriotto A., Moretti F., Bozzoni I., Caffarelli E. A minicircuitry involving REST and CREB controls miR-9–2 expression during human neuronal differentiation. Nucleic Acids Res. 2010;38:6895–6905. doi: 10.1093/nar/gkq604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Annibali D., Gioia U., Savino M., Laneve P., Caffarelli E., Nasi S. A new module in neural differentiation control: two microRNAs upregulated by retinoic acid, miR-9 and -103, target the differentiation inhibitor ID2. PLoS One. 2012;7:e40269. doi: 10.1371/journal.pone.0040269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Zhang H., Qi M., Li S., Qi T., Mei H., Huang K., Zheng L., Tong Q. MicroRNA-9 targets matrix metalloproteinase 14 to inhibit invasion, metastasis, and angiogenesis of neuroblastoma cells. Mol. Cancer Therapeut. 2012;11:1454–1466. doi: 10.1158/1535-7163.MCT-12-0001. [DOI] [PubMed] [Google Scholar]
- 127.Lee J.J., Drakaki A., Iliopoulos D., Struhl K. MiR-27b targets PPARgamma to inhibit growth, tumor progression and the inflammatory response in neuroblastoma cells. Oncogene. 2012;31:3818–3825. doi: 10.1038/onc.2011.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Cole K.A., Attiyeh E.F., Mosse Y.P., Laquaglia M.J., Diskin S.J., Brodeur G.M., Maris J.M. A functional screen identifies miR-34a as a candidate neuroblastoma tumor suppressor gene. Mol. Cancer Res. 2008;6:735–742. doi: 10.1158/1541-7786.MCR-07-2102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Ragusa M., Majorana A., Banelli B., Barbagallo D., Statello L., Casciano I., Guglielmino M.R., Duro L.R., Scalia M., Magro G., et al. MIR152, MIR200B, and MIR338, human positional and functional neuroblastoma candidates, are involved in neuroblast differentiation and apoptosis. J. Mol. Med. 2010;88:1041–1053. doi: 10.1007/s00109-010-0643-0. [DOI] [PubMed] [Google Scholar]
- 130.Lodygin D., Tarasov V., Epanchintsev A., Berking C., Knyazeva T., Korner H., Knyazev P., Diebold J., Hermeking H. Inactivation of miR-34a by aberrant CpG methylation in multiple types of cancer. Cell Cycle. 2008;7:2591–2600. doi: 10.4161/cc.7.16.6533. [DOI] [PubMed] [Google Scholar]
- 131.Welch C., Chen Y., Stallings R.L. MicroRNA-34a functions as a potential tumor suppressor by inducing apoptosis in neuroblastoma cells. Oncogene. 2007;26:5017–5022. doi: 10.1038/sj.onc.1210293. [DOI] [PubMed] [Google Scholar]
- 132.Saito Y., Liang G., Egger G., Friedman J.M., Chuang J.C., Coetzee G.A., Jones P.A. Specific activation of microRNA-127 with downregulation of the proto-oncogene BCL6 by chromatin-modifying drugs in human cancer cells. Cancer Cell. 2006;9:435–443. doi: 10.1016/j.ccr.2006.04.020. [DOI] [PubMed] [Google Scholar]
- 133.Wei J.S., Song Y.K., Durinck S., Chen Q.R., Cheuk A.T., Tsang P., Zhang Q., Thiele C.J., Slack A., Shohet J., et al. The MYCN oncogene is a direct target of miR-34a. Oncogene. 2008;27:5204–5213. doi: 10.1038/onc.2008.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Agostini M., Tucci P., Steinert J.R., Shalom-Feuerstein R., Rouleau M., Aberdam D., Forsythe I.D., Young K.W., Ventura A., Concepcion C.P., et al. MicroRNA-34a regulates neurite outgrowth, spinal morphology, and function. Proc. Natl. Acad. Sci. USA. 2011;108:21099–21104. doi: 10.1073/pnas.1112063108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Gougelet A., Perez J., Pissaloux D., Besse A., Duc A., Decouvelaere A.V., Ranchere-Vince D., Blay J.Y., Alberti L. miRNA Profiling: How to Bypass the Current Difficulties in the Diagnosis and Treatment of Sarcomas. Sarcoma. 2011;2011:460650. doi: 10.1155/2011/460650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Lin R.J., Lin Y.C., Chen J., Kuo H.H., Chen Y.Y., Diccianni M.B., London W.B., Chang C.H., Yu A.L. microRNA signature and expression of Dicer and Drosha can predict prognosis and delineate risk groups in neuroblastoma. Cancer Res. 2010;70:7841–7850. doi: 10.1158/0008-5472.CAN-10-0970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.De Preter K., Mestdagh P., Vermeulen J., Zeka F., Naranjo A., Bray I., Castel V., Chen C., Drozynska E., Eggert A., et al. MiRNA expression profiling enables risk stratification in archived and fresh neuroblastoma tumor samples. Clin. Cancer Res. 2011;17:7684–7692. doi: 10.1158/1078-0432.CCR-11-0610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Cortez M.A., Calin G.A. MicroRNA identification in plasma and serum: A new tool to diagnose and monitor diseases. Expert Opin. Biol. Ther. 2009;9:703–711. doi: 10.1517/14712590902932889. [DOI] [PubMed] [Google Scholar]
- 139.Miyachi M., Tsuchiya K., Yoshida H., Yagyu S., Kikuchi K., Misawa A., Iehara T., Hosoi H. Circulating muscle-specific microRNA, miR-206, as a potential diagnostic marker for rhabdomyosarcoma. Biochem. Biophys. Res. Commun. 2010;400:89–93. doi: 10.1016/j.bbrc.2010.08.015. [DOI] [PubMed] [Google Scholar]
- 140.Hogrefe R.I., Lebedev A.V., Zon G., Pirollo K.F., Rait A., Zhou Q., Yu W., Chang E.H. Chemically modified short interfering hybrids (siHYBRIDS): nanoimmunoliposome delivery in vitro and in vivo for RNAi of HER-2. Nucleos. Nucleot. Nucleic Acids. 2006;25:889–907. doi: 10.1080/15257770600793885. [DOI] [PubMed] [Google Scholar]
- 141.Pirollo K.F., Rait A., Zhou Q., Hwang S.H., Dagata J.A., Zon G., Hogrefe R.I., Palchik G., Chang E.H. Materializing the potential of small interfering RNA via a tumor-targeting nanodelivery system. Cancer Res. 2007;67:2938–2943. doi: 10.1158/0008-5472.CAN-06-4535. [DOI] [PubMed] [Google Scholar]
- 142.Elmen J., Lindow M., Schutz S., Lawrence M., Petri A., Obad S., Lindholm M., Hedtjarn M., Hansen H.F., Berger U., et al. LNA-mediated microRNA silencing in non-human primates. Nature. 2008;452:896–899. doi: 10.1038/nature06783. [DOI] [PubMed] [Google Scholar]
- 143.Lanford R.E., Hildebrandt-Eriksen E.S., Petri A., Persson R., Lindow M., Munk M.E., Kauppinen S., Orum H. Therapeutic silencing of microRNA-122 in primates with chronic hepatitis C virus infection. Science. 2010;327:198–201. doi: 10.1126/science.1178178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Anand S., Majeti B.K., Acevedo L.M., Murphy E.A., Mukthavaram R., Scheppke L., Huang M., Shields D.J., Lindquist J.N., Lapinski P.E., et al. MicroRNA-132-mediated loss of p120RasGAP activates the endothelium to facilitate pathological angiogenesis. Nat. Med. 2010;16:909–914. doi: 10.1038/nm.2186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Su J., Baigude H., McCarroll J., Rana T.M. Silencing microRNA by interfering nanoparticles in mice. Nucleic Acids Res. 2011;39:e38. doi: 10.1093/nar/gkq1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Almeida M.I., Reis R.M., Calin G.A. MicroRNA history: discovery, recent applications, and next frontiers. Mutat. Res. 2011;717:1–8. doi: 10.1016/j.mrfmmm.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 147.Tivnan A., Orr W.S., Gubala V., Nooney R., Williams D.E., McDonagh C., Prenter S., Harvey H., Domingo-Fernandez R., Bray I.M., et al. Inhibition of neuroblastoma tumor growth by targeted delivery of microRNA-34a using anti-disialoganglioside GD2 coated nanoparticles. PLoS One. 2012;7:e38129. doi: 10.1371/journal.pone.0038129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Issa J.P., Garcia-Manero G., Giles F.J., Mannari R., Thomas D., Faderl S., Bayar E., Lyons J., Rosenfeld C.S., Cortes J., et al. Phase 1 study of low-dose prolonged exposure schedules of the hypomethylating agent 5-aza-2′-deoxycytidine (decitabine) in hematopoietic malignancies. Blood. 2004;103:1635–1640. doi: 10.1182/blood-2003-03-0687. [DOI] [PubMed] [Google Scholar]
- 149.Kantarjian H., Issa J.P., Rosenfeld C.S., Bennett J.M., Albitar M., DiPersio J., Klimek V., Slack J., de Castro C., Ravandi F., et al. Decitabine improves patient outcomes in myelodysplastic syndromes: results of a phase III randomized study. Cancer. 2006;106:1794–1803. doi: 10.1002/cncr.21792. [DOI] [PubMed] [Google Scholar]
- 150.Vigil C.E., Martin-Santos T., Garcia-Manero G. Safety and efficacy of azacitidine in myelodysplastic syndromes. Drug Des. Devel. Ther. 2010;4:221–229. doi: 10.2147/dddt.s3143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Candelaria M., Herrera A., Labardini J., Gonzalez-Fierro A., Trejo-Becerril C., Taja-Chayeb L., Perez-Cardenas E., de la Cruz-Hernandez E., Arias-Bofill D., Vidal S., et al. Hydralazine and magnesium valproate as epigenetic treatment for myelodysplastic syndrome. Preliminary results of a phase-II trial. Ann. Hematol. 2010;90:379–387. doi: 10.1007/s00277-010-1090-2. [DOI] [PubMed] [Google Scholar]
- 152.Fu S., Hu W., Iyer R., Kavanagh J.J., Coleman R.L., Levenback C.F., Sood A.K., Wolf J.K., Gershenson D.M., Markman M., et al. Phase 1b-2a study to reverse platinum resistance through use of a hypomethylating agent, azacitidine, in patients with platinum-resistant or platinum-refractory epithelial ovarian cancer. Cancer. 2010;117:1661–1669. doi: 10.1002/cncr.25701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Juergens R.A., Wrangle J., Vendetti F.P., Murphy S.C., Zhao M., Coleman B., Sebree R., Rodgers K., Hooker C.M., Franco N., et al. Combination epigenetic therapy has efficacy in patients with refractory advanced non-small cell lung cancer. Cancer Discov. 2011;1:598–607. doi: 10.1158/2159-8290.CD-11-0214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Abele R., Clavel M., Dodion P., Bruntsch U., Gundersen S., Smyth J., Renard J., van Glabbeke M., Pinedo H.M. The EORTC Early Clinical Trials Cooperative Group experience with 5-aza-2′-deoxycytidine (NSC 127716) in patients with colo-rectal, head and neck, renal carcinomas and malignant melanomas. Eur. J. Cancer Clin. Oncol. 1987;23:1921–1924. doi: 10.1016/0277-5379(87)90060-5. [DOI] [PubMed] [Google Scholar]
- 155.Momparler R.L., Bouffard D.Y., Momparler L.F., Dionne J., Belanger K., Ayoub J. Pilot phase I-II study on 5-aza-2′-deoxycytidine (Decitabine) in patients with metastatic lung cancer. Anti-Cancer Drugs. 1997;8:358–368. doi: 10.1097/00001813-199704000-00008. [DOI] [PubMed] [Google Scholar]
- 156.Tsai H.C., Li H., Van Neste L., Cai Y., Robert C., Rassool F.V., Shin J.J., Harbom K.M., Beaty R., Pappou E., et al. Transient low doses of DNA-demethylating agents exert durable antitumor effects on hematological and epithelial tumor cells. Cancer Cell. 2012;21:430–446. doi: 10.1016/j.ccr.2011.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Shoemaker A.R., Mitten M.J., Adickes J., Ackler S., Refici M., Ferguson D., Oleksijew A., O’Connor J.M., Wang B., Frost D.J., et al. Activity of the Bcl-2 family inhibitor ABT-263 in a panel of small cell lung cancer xenograft models. Clin. Cancer Res. 2008;14:3268–3277. doi: 10.1158/1078-0432.CCR-07-4622. [DOI] [PubMed] [Google Scholar]
- 158.Jain H.V., Meyer-Hermann M. The molecular basis of synergism between carboplatin and ABT-737 therapy targeting ovarian carcinomas. Cancer Res. 2011;71:705–715. doi: 10.1158/0008-5472.CAN-10-3174. [DOI] [PubMed] [Google Scholar]
- 159.Belinsky S.A., Klinge D.M., Stidley C.A., Issa J.P., Herman J.G., March T.H., Baylin S.B. Inhibition of DNA methylation and histone deacetylation prevents murine lung cancer. Cancer Res. 2003;63:7089–7093. [PubMed] [Google Scholar]
- 160.Gore S.D., Baylin S., Sugar E., Carraway H., Miller C.B., Carducci M., Grever M., Galm O., Dauses T., Karp J.E., et al. Combined DNA methyltransferase and histone deacetylase inhibition in the treatment of myeloid neoplasms. Cancer Res. 2006;66:6361–6369. doi: 10.1158/0008-5472.CAN-06-0080. [DOI] [PubMed] [Google Scholar]
- 161.Fandy T.E., Herman J.G., Kerns P., Jiemjit A., Sugar E.A., Choi S.H., Yang A.S., Aucott T., Dauses T., Odchimar-Reissig R., et al. Early epigenetic changes and DNA damage do not predict clinical response in an overlapping schedule of 5-azacytidine and entinostat in patients with myeloid malignancies. Blood. 2009;114:2764–2773. doi: 10.1182/blood-2009-02-203547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Suva M.L., Riggi N., Janiszewska M., Radovanovic I., Provero P., Stehle J.C., Baumer K., Le Bitoux M.A., Marino D., Cironi L., et al. EZH2 is essential for glioblastoma cancer stem cell maintenance. Cancer Res. 2009;69:9211–9218. doi: 10.1158/0008-5472.CAN-09-1622. [DOI] [PubMed] [Google Scholar]
- 163.Tan J., Yang X., Zhuang L., Jiang X., Chen W., Lee P.L., Karuturi R.K., Tan P.B., Liu E.T., Yu Q. Pharmacologic disruption of Polycomb-repressive complex 2-mediated gene repression selectively induces apoptosis in cancer cells. Genes Dev. 2007;21:1050–1063. doi: 10.1101/gad.1524107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Fiskus W., Wang Y., Sreekumar A., Buckley K.M., Shi H., Jillella A., Ustun C., Rao R., Fernandez P., Chen J., et al. Combined epigenetic therapy with the histone methyltransferase EZH2 inhibitor 3-deazaneplanocin A and the histone deacetylase inhibitor panobinostat against human AML cells. Blood. 2009;114:2733–2743. doi: 10.1182/blood-2009-03-213496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Hayden A., Johnson P.W., Packham G., Crabb S.J. S-adenosylhomocysteine hydrolase inhibition by 3-deazaneplanocin A analogues induces anti-cancer effects in breast cancer cell lines and synergy with both histone deacetylase and HER2 inhibition. Breast Cancer Res. Treat. 2010;102:109–119. doi: 10.1007/s10549-010-0982-0. [DOI] [PubMed] [Google Scholar]
- 166.Yu Y., Zeng P., Xiong J., Liu Z., Berger S.L., Merlino G. Epigenetic drugs can stimulate metastasis through enhanced expression of the pro-metastatic Ezrin gene. PLoS One. 2010;5:e12710. doi: 10.1371/journal.pone.0012710. [DOI] [PMC free article] [PubMed] [Google Scholar]