Abstract
As part of a women’s health center project, we reviewed 16 years of research to examine health disparities between women with and without disabilities. We reviewed MEDLINE-indexed articles between 1990 and 2005 with data on women with and without physical, sensory, intellectual, developmental, or psychiatric disabilities. Our review found few articles examining health disparities in chronic disease, cancer, mental health and substance abuse, preventive screening, health-promoting behaviors, and health services utilization. Results reflect apparent health disparities between women with and without disabilities. Challenges for the field exist in standardizing disability definitions and determining a future course for health disparity research and policy.
Keywords: Disability; women’s health; health disparities; blindness, hearing impairment; mental retardation; chronic disease; preventive screening; mental health; cancer
INTRODUCTION
In order for policy to adequately address health disparities, the disparities first must be illuminated and defined in a way that advances the formulation of public policy and legislation (Gamble & Stone, 2006). A model for this process is the 1985 Report of the Secretary’s Task Force on Black and Minority Health that led to the creation of the Office of Minority Health to address racial and ethnic health disparities (Gamble & Stone, 2006; U.S. Department of Human Services, 1985). Kilbourne, Switzer, Hyman, Crowley-Matoka, and Fine (2006) argued for expanding health disparities research to encompass all vulnerable populations, defined as groups that have faced discrimination due to underlying differences in social status that can lead to potential gaps in health or healthcare. As a historically marginalized group with lower levels of education, lower likelihood of employment, lower earnings, and higher likelihood of living in poverty (National Organization on Disability/Harris, 2004; Rehabilitation Research and Training Center on Disability Demographics and Statistics, 2007) people with disabilities fit this definition.
Until recently, health disparities among Americans with disabilities have largely been ignored within the field of public health (Nosek & Simmons, 2007). Health disparities affecting the nearly 40 million Americans with disabilities (U.S. Census Bureau, 2005) have begun to gain recognition over the past decade, as reflected in the release of several significant publications by the federal government intended to inform and guide policy and practice (U.S. Department of Health and Human Services, 2000, 2005). Although disability affects both men and women, it is more prevalent among women, largely due to their longer life span and greater risk for problems such as osteoporosis (Murtagh & Hubert, 2004; Oman, Reed, & Ferrara, 1999) and some mental health problems (Murtagh & Hubert, 2004; Narrow, 2006). Women with disabilities can be considered “doubly vulnerable” as members of two groups with a long history of inequitable treatment. In assessing the impact of the intersection of gender and disability, it is important to understand how women with disabilities differ from other women—women who may experience health disparities themselves due to their gender but without the added layer of disability.
Since we could find limited information on disparities between women with and without disabilities, our multidisciplinary group of researchers conducted a systematic review to guide policy and health promotion activities. As we reviewed the literature, we encountered three significant challenges in health disparity research specific to people with disabilities. These challenges are discussed with regard to how they impacted the study methodology.
The first challenge arises from the many types and definitions of “disability,” making it difficult to measure and track health disparities for people with disabilities as a group. Disability can range from conditions narrowly defined by specific medical diagnoses to broadly and subjectively defined concepts such as self-report of activity limitations of any kind. Iezzoni and Freedman’s (2008) commentary on the history and diversity of definitions of disability used in the United States and by the World Health Organization concludes that the multitude of definitions of disability stems from a need to determine which individuals merit income support or protection from disability discrimination. Since disability can be defined in a number of ways, we included articles that not only focused on various types of disabilities but also used different methods of defining and assessing those disabilities.
The second challenge is that disability and good health are often viewed as mutually exclusive. While people with disabilities are more likely than people without disabilities to report fair or poor health (for example, Drum, Horner-Johnson, & Krahn, 2008), there is a growing awareness that one can be disabled and also be healthy (Rimmer, 1999; Wilber et al., 2002). Recent efforts to conceptually disentangle disability and health have revealed that much of the health differential between people with and without disabilities may be preventable (Krahn, Hammond, & Turner, 2006). This area of research, however, is still relatively new and underdeveloped.
The third challenge relates to the common conflation of health disparities with secondary conditions (Wilber et al., 2002). Secondary conditions are physical, medical, cognitive, emotional, or psychosocial consequences to which people with disabilities are more susceptible (Hough, 1999). Some secondary conditions can be prevented or decreased through accessible and appropriate healthcare (for example, chronic pain) or environmental improvements (for example, chronic isolation); other secondary conditions can be managed but not entirely prevented (for example, fatigue). For this review, we examine differences in the prevalence of health conditions and health behaviors between women with and without disabilities; we include secondary conditions in our search strategy as we seek to illuminate their place in the literature on health disparities.
To address these challenges, we cast a wide net in this literature review focusing on evidence for disparity between women with and without disabilities in six areas: (1) chronic diseases; (2) cancer; (3) mental health and substance abuse problems; (4) preventive screenings; (5) health-promoting behaviors; and (6) health services use.
METHODS
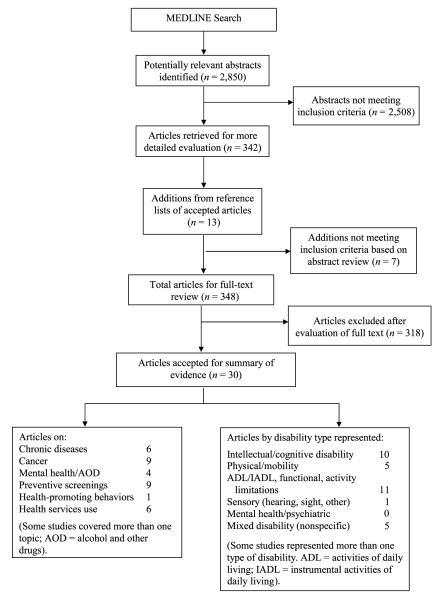
The review process included identification of potentially relevant research articles, review of abstracts, review of full articles accepted during the abstract review, and analysis of articles accepted after full-text review (see Figure 1). The research team included six researchers with backgrounds in disability, chronic disease, health services research, and clinical medicine; the team included women with disabilities.
FIGURE 1.
Flow diagram of study selection process.
Articles for possible inclusion were identified through a MEDLINE search incorporating articles published between January 1, 1990, and July 13, 2005. The search included a broad range of types of disability (for example, physical, mental) and numerous terms related to the six health disparity areas. Specific Medical Subject Headings (MeSH) used in the search can be obtained from the authors. Search results were limited to adult women only (defined in MEDLINE as 19 years and older) and English-language only. This search yielded 2,850 unique abstracts.
Abstracts identified in the search were randomly assigned to the six research team members for review. Abstracts were assigned with random overlap such that 10% of the abstracts were read by two reviewers. Prior to reviewing abstracts, the research team established inclusion and exclusion criteria to identify abstracts to retain for full-article review. Inclusion criteria were (1) the article was empirical (that is, editorials, commentaries, and theory-only articles were excluded); (2) the study sample included adult women with disabilities; (3) the study included one or more of the chronic conditions, health behaviors, or other topics of interest; (4) the article focused on disability as a sample characteristic rather than as an outcome; (5) the article included comparative data on women with and without a disability; (6) the sample size for each group was 10 or larger; and (7) the study was conducted in a country on the CIA Factbook (U.S. Central Intelligence Agency, 2001) list of developed countries.
Abstracts clearly failing to meet one or more of the inclusion criteria were excluded from further consideration. Reviewer questions were addressed by review team members who provided expertise in disability studies, medicine, and study methodology. In cases where it could not be determined from the abstract whether the article met all inclusion criteria, the article was accepted for further review. Inter-rater reliability for the overlapping sample of abstracts was 90%. The review of abstracts led to the exclusion of 2,508, with 342 retained for full-text review.
Full-text articles were obtained for all accepted abstracts. Articles were reviewed by four research team members. The full-text articles were evaluated using the same inclusion criteria used in reviewing abstracts. Reference sections of articles meeting inclusion criteria were searched to identify additional articles for possible inclusion. Additional articles were subjected to the same review process (abstract review followed by full-text review if warranted). Thirteen additional articles were considered, with 7 rejected at the abstract level and 6 accepted for full-text review. Of all 348 full articles reviewed, 318 were excluded because they did not meet all inclusion criteria and 30 were retained for summary of evidence. Articles accepted for inclusion were submitted to a data abstraction process to summarize key information.
RESULTS
Thirty articles were found that met our criteria for providing data on health disparities between women with disabilities and women without disabilities in our six outcome areas: (1) chronic disease (n = 6); (2) cancer (n = 9); (3) mental health and substance abuse (n = 4); (4) preventive screenings (n = 9); (5) health-promoting behavior (n = 1); and (6) health services use (n = 6). Some of the articles covered more than one outcome and are counted multiply. We found evidence of health disparities between women with and without disabilities in each of these areas except health services use. Table 1 provides an overview of findings for all categories. Details regarding study design, participants, and data sources are available from the first author. Findings in each category are presented below.
TABLE 1.
Systematic Review Results for Disparities Between Women With and Without Disabilities
| Study | Topic | Disability | Outcomes |
|---|---|---|---|
| Blustein & Weiss, 1998 | Preventive screenings |
ADL limitations | WWD significantly less likely to have had a mammogram (21.3% vs. 32.1%) during 2-year period. |
| Caban et al., 2002 | Cancer; health services use |
Physical/mobility | No significant difference between WWD and nondisabled women in stage at diagnosis or type of breast cancer treatment received. |
| Cerhan & Chiu, 1998 | Cancer | Mobility/physical functioning |
WWD at decreased risk for breast cancer compared to inactive nondisabled women (RR D 0.4; 95% CI, 0.2–0.9). |
| Chan et al., 1999 | Preventive screenings |
ADL limitations | WWD aged 45+ less likely than nondisabled women to have past-year mammogram (13.2% vs. 43.6%). WWD <71 less likely to have Pap test in past year (23.0% vs. 41.2%), more likely to have past-year flu vaccine (67.4% vs. 57.3%), and as likely to have lifetime pneumonia vaccine (32.0% vs. 32.9%). |
| Diab & Johnston, 2004 | Preventive screenings |
ADL limitations | WWD aged 50+ less likely than nondisabled women to have received a mammogram (p < .05) in 1998 data; no differences in 2000 data. In both years, WWD aged 50+ less likely to have received clinical breast exam (p < .05) and all WWD aged 18+ less likely to have received Pap test (p < .05). |
| Eden et al., 1995 | Health services use | Physical | WWD visited physician (74% vs. 53.8%, p < .001), physiotherapist (25.2% vs. 12%, p < .001), and alternative caregiver (9.8% vs. 3%, p < .01) more often than controls. No differences for visits with district nurse or inpatient care. Prescription drug use higher among WWD than controls (p < .001). |
| Emerson, 2005 | Health promotion | Intellectual disability | WWD more likely to be inactive than nondisabled women (p < .001). |
| Graciani et al., 2004 | Chronic disease; cancer; mental health/substance use |
ADL, IADL, mobility and agility limitations |
WWD had greater chronic disease than nondisabled women: hypertension (43.3% vs. 20.2%), ischemic heart disease (5.7% vs. 1.7%), and diabetes (16.9% vs. 9.6%). WWD more likely to have prevalent cancer than nondisabled women (2.5% vs. 1.3%). WWD had greater depression (15.4% vs. 8.2%). |
| Havercamp et al., 2004 | Preventive screenings |
Intellectual disability; other disabilities |
Women with intellectual disability more likely to never have had Pap test (RR, 5.3; 95% CI, 2.9– 9.5) or mammogram (age 40+) (RR, 2.1; 95% CI, 1.4–3.0) than nondisabled women. Women with other disabilities did not significantly differ from nondisabled women. |
| Hermon et al., 2001 | Chronic disease; cancer |
Intellectual disability | Mortality for WWD significantly elevated for diabetes (SMR = 1,125), epilepsy (SMR = 3,995), heart/circulatory diseases (SMR = 457), and all causes combined (SMR = 805). Leukemia mortality for WWD significantly elevated (SMR = 1,626). |
| Iezzoni et al., 2000 | Preventive screenings |
Physical/mobility | In adjusted analyses, WWD significantly less likely to have received Pap test (OR, 0.6; 95% CI, 0.4–0.9) or mammogram (age 50+) (OR, 0.7; 95% CI, 0.5–0.9). |
| Jones & Bell, 2004 | Chronic disease; mental health/ substance use |
Functional limitations including communication limitations |
WWD more likely to have hypertension (41.8% vs. 12.1%) and diabetes (15.3% vs. 1.8%) than nondisabled women. WWD more likely to be current smokers (52.6% vs. 47.0%) and heavy smokers (7.0% vs. 2.1%) but less likely to be current drinkers (4.1% vs. 61.2) or heavy drinkers (>7/week) (3.6% vs. 3.9%) than nondisabled women. |
| Kapell et al., 1998 | Chronic disease | Intellectual disability | For women with Down syndrome, SMR significantly lower than expected for hypertension (0.2; 95% CI, 0.1–0.6) and significantly higher for thyroid disorders (10.1; 95% CI, 6.6–14.8) and nonischemic heart problems (6.4; 95% CI, 4.1–9.6). For females with other intellectual disability, SMR significantly higher for heart problems (1.9; 95% CI, 1.2–3.0) compared to NHIS. |
| Korten et al., 1998 | Health services use | ADL, hearing/visual limitations |
ADL and visual impairment significantly associated with more GP visits, β(SE): ADL = 0.063 (0.017); visual impairment = 0.061 (0.026). |
| Mandelblatt et al., 2001 | Health services use | Functional limitations | WWD less likely to receive BCS with radiotherapy (more likely to receive BCS alone or mastectomy) and less likely to receive chemotherapy. |
| Moore & Li, 1998 | Mental health/ substance use |
Various | Illicit drug use higher among WWD than the general population. Greatest difference for crack use (>3x higher than general population). |
| Morgan et al., 2003 | Chronic disease | Intellectual disability | WWD more likely to have epilepsy (age standardized RR, 22.4; 95% CI, 18.64–26.92). |
| Nosek & Howland, 1997 | Preventive screenings |
Physical | WWD less likely to receive regular pelvic exams (67.1% vs. 72.8%) (significant for women with severe disabilities). No difference for mammograms. |
| Nosek & Gill, 1998 | Preventive screenings |
Functional limitations | WWD were as likely to have ever had a Pap test but less likely to have had a recent Pap test (1–2 FLs: 64.8%; ≥3 FLs: 60.6%; none: 76.1%). WWD aged 65+ with ≥3 FLs were less likely to have had a mammogram ever (64.7% vs. 73.3%) or in last 2 years (42.5% vs. 56.5%) than nondisabled women. |
| Patja et al., 2001 | Cancer | Intellectual disability | No difference in overall rates of cancer |
| Rimmer et al., 1994 | Mental health/ substance use |
Intellectual disability | WWD less likely to smoke (0% in 16+ bed facility, 6.7% in group homes, 2.1% in natural family) than Framingham women (27%). |
| Roetzheim & Chirikos, 2002 | Cancer | Various | WWD less likely to have cancer diagnosed at early stage (OR, 0.77; 95% CI, 0.61–0.97). No differences in breast cancer–specific mortality rates. |
| Schootman & Fuortes, 1999 | Preventive screenings |
ADL and IADL limitations |
Women with severe limitations were less likely to have had a Pap test (65.5%) compared to women with some limitations (72.8%) and women with no limitations (78.9%). No differences on mammograms. |
| Schootman & Jeffe, 2003 | Preventive screenings |
ADL and IADL limitations |
WWD were significantly less likely to have had a mammogram in the past year than nondisabled women (p < .001). |
| Schultz-Pedersen et al., 2001 | Cancer | Intellectual disability | Cancer incidence in WWD significantly lower than general population (SIR, 0.15; 95% CI, 0.0–0.9). |
| Stronks et al., 1997 | Chronic disease | Various | WWD significantly more likely than employed women to have one or more chronic conditions (OR, 5.29; 95% CI, 4.02–6.97). |
| Sullivan et al., 2003 | Cancer | Intellectual disability | WWD had lower incidence of breast cancer (SIR, 0.44; 95% CI, 0.27–0.68). |
| Sullivan et al., 2004 | Cancer | Intellectual disability | Overall cancer risk in WWD not significantly different from general population. Higher incidence of colorectal cancer (SIR, 3.10; 95% CI, 1.42–5.88), leukemia (SIR, 4.64; 95% CI, 2.40–8.11), and uterine cancer (SIR, 2.98; 95% CI, 1.29–5.87) in WWD. |
| Tomiak et al., 1998 | Health services use | Various | WWD had more hospital separations (OR, 3.8), hospital separated days (OR, 4.5), physician services (OR, 1.7), physician costs (OR, 1.9), and nursing home entry (OR, 3.7) than nondisabled women. |
| Wyrwich & Wolinsky, 2000 | Health services use | ADL limitations | Among inactive women, there were no differences between those with disabilities and those without. |
Note. ADL = activities of daily living; BCS = breast conservation surgery; CI = confidence interval; FL = functional limitations; IADL = instrumental activities of daily living; NHIS = National Health Interview Survey; OR = odds ratio; RR = relative risk; SIR = standardized incidence ratio; SMR = standardized mortality ratio; WWD = women with disabilities.
Chronic Disease
Five articles evaluating disparities in chronic disease prevalence met our inclusion criteria (Graciani, Banegas, López-García, & Rodríguez-Artalejo, 2004; Jones & Bell, 2004; Kapell et al., 1998; Morgan, Baxter, & Kerr, 2003; Stronks, van de Mheen, van den Bos, & Mackenbach, 1997), and a sixth evaluating mortality disparities due to chronic conditions (Hermon, Alberman, Beral, & Swerdlow, 2001) was also included (see Table 1 for details).
Three of the articles that evaluated differences in heart and/or circulatory disease reported worse outcomes for women with disability compared to women without disability (Graciani et al., 2004; Hermon et al., 2001; Jones & Bell, 2004), while a fourth reported mixed findings (Kapell et al., 1998). Similarly, when evaluating differences in diabetes, Hermon et al. (2001), Graciani et al. (2004), and Jones and Bell (2004) reported worse outcomes for women with disability compared to women without disability, while Kapell et al. (1998) reported mixed findings. Morgan et al. (2003) compared epilepsy prevalence in people with intellectual disability to population estimates from the same time frame and geographic region and reported increased prevalence of epilepsy for women with intellectual disability. Hermon et al. (2001) evaluated differences in mortality due to a variety of chronic conditions and found increased mortality among women with intellectual disabilities related to a number of chronic conditions, including epilepsy. Stronks et al. (1997) examined presence of any chronic condition and found that women with disabilities were more likely than nondisabled women to have one or more chronic conditions.
Cancer
Nine articles evaluating disparities in cancer incidence or mortality met our inclusion criteria (see Table 1). Four of these articles focused on breast cancer (Caban, Nosek, Graves, Esteva, & McNeese, 2002; Cerhan & Chiu, 1998; Roetzheim & Chirikos, 2002; Sullivan et al., 2003), one considered other specific cancers in addition to overall cancer (Sullivan, Hussain, Threlfall, & Bittles, 2004), and the remaining three articles included gender-specific comparisons for overall cancer only (Graciani et al., 2004; Patja, Eero, & Iivanainen, 2001; Schultz-Pedersen, Hasle, Olsen, & Friedrich, 2001).
The articles focused on breast cancer reported mixed findings. Sullivan et al. (2003) reported that cancer incidence was significantly lower among women with intellectual disability. Cerhan and Chiu (1998) compared women with physical disabilities to nondisabled women who were physically inactive and found lower risk of breast cancer among the women with disabilities. Roetzheim and Chirikos (2002) and Caban et al. (2002) evaluated differences in breast cancer stage at diagnosis. Roetzheim and Chirikos (2002) analyzed breast cancer data from the Medicare–Surveillance, Epidemiology and End Results data set and reported that women with disability were less likely to receive diagnoses at an early stage compared to nondisabled women; however, there were no significant differences in breast cancer–specific mortality rates. Caban et al. (2002) found no statistically significant difference between women with and without disabilities in terms of likelihood of late stage at diagnosis.
Two relatively large retrospective cohort studies evaluated disparities in cancer incidence comparing women with intellectual disabilities to nondisabled women. Sullivan et al. (2004) compared people with intellectual disability with the general population in cancer registry data and found that overall cancer incidence did not differ significantly in the two groups. However, women with intellectual disability did have significantly higher risk of leukemia, colorectal cancer, and uterine cancer specifically. Patja et al. (2001) compared people with intellectual disability to a nationwide population study and found no significant differences in overall cancer incidence. In contrast, in a small longitudinal study involving people with fragile X syndrome, Schultz-Pedersen et al. (2001) found that the incidence rate in women with fragile X was significantly lower than expected from the overall incidence rates for Danish women.
Mental Health and Substance Use
We found four articles on mental illness, alcohol use/abuse, illicit drug use/abuse, and smoking (see Table 1). Most potential articles that included mental illness used self-report measures with Behavioral Risk Factor Surveillance System or other survey items. We found only one relevant paper on diagnosed mental illness: Graciani et al. (2004) compared prevalence of diagnosed and treated depression in probabilistic samples of elderly women in Spain. They found that women with disabilities had a greater prevalence of depression compared to nondisabled women.
We found three articles that addressed alcohol use/abuse, illicit drug use/abuse, and smoking. Rimmer, Braddock, and Fujiura (1994) compared women with intellectual disabilities who lived in institutional, group home, and family environments to women from the Framingham study and found that smoking was less prevalent among the women with disabilities. Moore and Li (1998) compared prevalence of illicit drug use between women receiving vocational rehabilitation services (specific disabilities included mental illness, learning disabilities, and sensory or congenital disabilities) to national survey estimates. Illicit drug use (including marijuana, inhalants, cocaine, crack, hallucinogens, and heroin) was higher in women with disabilities than in the general population, with crack cocaine use having three times the prevalence among women with disabilities compared to the general population estimate. Jones and Bell (2004) assessed smoking and drinking among women; women with severe functional limitations were more likely to be current smokers and heavy smokers compared to those without limitations. Women with severe functional limitations were much less likely to be current drinkers and about as likely to be heavy drinkers compared to women without functional limitations.
Preventive Screening
Articles on preventive screening disparities among women with and without disabilities tended to focus on mammography and Pap tests (see Table 1). Most articles found that women with disabilities had lower likelihood of having a recent mammogram (Blustein & Weiss, 1998; Chan et al., 1999; Iezzoni, McCarthy, Davis, & Siebens, 2000; Nosek & Gill, 1998; Nosek & Howland, 1997; Schootman & Fuortes, 1999; Schootman & Jeffe, 2003) compared to nondisabled women. Diab and Johnston (2004) found women with disabilities less likely to have received mammograms in one year of data and no differences on mammography rates in another year of data. Havercamp, Scandlin, and Roth (2004) found that women with developmental disabilities were less likely to have ever had a mammogram compared to women with no disabilities, but there were no differences between women with other disabilities and nondisabled women.
Pap test findings were similar, with most researchers finding that women with disabilities were less likely to have received a recent Pap test (Chan et al., 1999; Diab & Johnston, 2004; Iezzoni et al., 2000; Nosek & Gill, 1998; Schootman & Fuortes, 1999) or lifetime Pap test (for women with developmental disabilities only) (Havercamp et al., 2004). Nosek and Gill (1998) identified no difference in the receipt of lifetime Pap test screenings.
Additional differences found between women with and without disabilities pertained to pelvic exam screenings (Nosek & Howland, 1997), clinical breast exams (Diab & Johnston, 2004), and past-year influenza vaccine (Chan et al., 1999). Rates of lifetime pneumonia vaccine were not different between groups (Chan et al., 1999).
Health-Promoting Behavior
Only one article evaluating differences in health-promoting behavior met our inclusion criteria (Table 1). Emerson (2005) compared levels of physical activity among women with intellectual disability living in supported housing in Northern England to a nationally representative sample of women in the Health Survey for England 1998. After excluding women who reported being “physically incapable,” women with intellectual disability were more likely to be inactive than nondisabled women in all age groups.
Health Services Use
In the health services arena (Table 1), we identified articles focused on service utilization specifically for breast cancer treatment (Caban et al., 2002; Mandelblatt et al., 2001; Wyrwich & Wolinsky, 2000) or on service utilization more generally (Edén, Ejlertsson, & Leden, 1995; Korten et al., 1998; Tomiak, Berthelot, & Mustard, 1998). Results were mixed for treatment related to breast cancer. Mandelblatt et al. (2001) found that women with limitations in activities of daily living were less likely than nondisabled women to receive the more aggressive treatment of breast conservation surgery with radiotherapy and were more likely to receive less aggressive treatments of breast conservation surgery alone or mastectomy. Others, however, examined patients with and without physical disabilities and found no differences in the rate of hospitalization for breast cancer (Wyrwich & Wolinsky, 2000) or between rates of breast-conserving treatment or chemotherapy treatment (Caban et al., 2002).
Articles addressing general health service utilization mainly indicated that women with disability tend to use more healthcare services. Korten et al. (1998) examined an elderly population and found that visual impairment and impairment in activities of daily living were significantly associated with more annual general practitioner visits compared with nondisabled women. Similarly, Tomiak et al. (1998) found that women with severe disabilities who were 35 or older had more physician service costs, higher likelihood of hospitalization, and higher likelihood of nursing home entry than nondisabled women. Edén et al. (1995) found that women with musculoskeletal disability had more physician visits, more alternative caregiver visits, and more prescription drug use than women in a control group; they found no differences in rates of inpatient hospitalization. While there is inequality in rates of healthcare use between women with and without disability, the review does not indicate inequity, as women with disabilities are receiving more services rather than fewer.
DISCUSSION
This review took a broad approach to examining health disparities in multiple areas for women with a variety of different disabilities. Even with the wide range of health outcomes, only 30 articles met inclusion criteria for this review, supporting Nosek and Simmon’s (2007) contention that disability has yet to achieve its proper place in the discussion of health disparities (p. 68).
Despite the diversity and the limitations of the articles reviewed, the results suggest a general pattern of differences in health risks and health outcomes between women with and without disabilities. Roughly two-thirds of the included articles found that women with disabilities were more likely to experience and die of chronic conditions, more likely to have cancer and to receive diagnoses at a late stage, less likely to receive regular screening for breast and cervical cancer, more likely to experience mental health or substance use problems, less likely to engage in health-promoting behaviors, and/or more likely to have increased healthcare utilization and costs. This review establishes health differentials between women with and without disability that suggest inequity, or poorer outcomes for women with disability, in all reviewed areas except health services use, where inequity suggests increased care.
Sixty articles were rejected upon full-text review because they studied disability as an outcome rather than as a sample characteristic. While disability can be considered an outcome, the lack of attention to disability as a characteristic of a marginalized population reflects deeply held beliefs regarding the nature of health. It is still common to view disability as counter to good health and to deny the possibility that people who have disabilities can also have varying health status (Wilber et al., 2002). The dual (and sometimes dueling) conceptualizations of disability as medical condition and/or sociodemographic characteristic have led to widely divergent approaches to research and policy. For example, public health and healthcare efforts often focus on preventing disability rather than promoting the health of individuals with disability. Policy implications related to the healthcare system are described below.
The articles included in this review reflect another challenge mentioned at the outset: how to standardize definitions of disability within the heterogeneous population of people with disabilities. Articles we reviewed covered a broad representation of disability, including functional or activity limitations (11 articles), physical or mobility limitations (5 articles), and intellectual or developmental limitations (10 articles). People with hearing or visual impairments, however, were explicitly included in only one article accepted for this review, and no articles focused specifically on individuals with mental health or psychiatric disabilities. In contrast to how women’s race and ethnicity are routinely included in demographic data collection, women with disabilities in the articles we reviewed were identified through medical need assessment; through social service eligibility mechanisms like social security disability insurance (Roetzheim & Chirikos, 2002) or vocational rehabilitation services (Moore and Li, 1998); or by asking the women directly about their limitations (for example, Blustein & Weiss, 1999; Graciani et al., 2004). The marked differences in the types of disability included in research and the methods for identifying disability preclude a comparison of findings across articles.
Policy Implications
Policy applications in this arena are complicated by the multiplicity of disciplines involved, including medicine, rehabilitation, public health, and psychology. Different disciplines often have different terminology, priorities, and funding mechanisms, which can lead to challenges in developing a cohesive literature to guide policy makers’ decisions. A commonality in these disciplines, however, is a responsibility to meet the immediate and long-term health needs of people with disabilities. While fulfilling urgent needs is critical, it is important for policy makers to balance immediate requirements with the need for investing in long-term approaches to address the underlying socioecological determinants that negatively impact the health of women with disabilities.
Routine data collection
In order to reduce disparities and guide policy, researchers assess the distribution of health among specified groups and compare it to the health distribution for the entire population (Almeida et al., 2001). Deep gaps remain in our understanding of health disparities among people with disabilities (Nosek & Simmons, 2007). Our findings suggest that collecting information about disability should become a routine part of demographic data collection, similar to age, gender, and race/ethnicity. Such an effort requires a standardized definition of disability. Research that identifies and relates characteristics of a defined subpopulation of individuals with disability will support policy efforts directed toward those at greatest risk (Field & Jette, 2007; Ver Ploeg & Perrin, 2004). Chapter 6 of Healthy People 2010 called for creating a “standardized set of questions that identifies people with disabilities”—a goal that has yet to be met. Healthy People 2010 also added disability as a demographic variable to some of the other chapters focusing on certain diseases and conditions, such as diabetes. Putting these recommendations into practice will provide considerably more consistent data with which to evaluate health disparities.
Clarify secondary conditions resulting from disability
An examination of the articles from our review suggests research should clarify the distinction between secondary conditions and health disparities. Some people with disabilities, such as those with hearing or vision loss, may not experience secondary conditions as a direct result of their disability, yet they may still be at increased risk of health disparities because of the social barriers associated with disability. Adoption of a clear taxonomy for describing conditions that directly arise from a disability as opposed to those that are not necessarily related to the disability and may be preventable (Krahn et al., 2006) will further advance the field and increase research specificity.
Changes to the healthcare system
Women with disabilities have as much or more access to healthcare than women without disabilities (Parish & Huh, 2006), but they experience disparities in the quality of care (Caban et al., 2002) and poorer health outcomes (Austin, 2003), even for preventable secondary conditions such as diabetes or cervical cancer (Diab & Johnston, 2004; Parish & Huh, 2006; Shabas & Weinreb, 2000). Such disparities represent a serious public health issue, given that almost 13% of noninstitutionalized working-age women in the United States have a disability (U.S. Census Bureau, 2005). This supports the importance of changes to the Medicaid healthcare system. Specific changes may include increasing the number of doctors that serve Medicaid patients and increasing the emphasis on preventive care (Long, Coughlin, & Kendall, 2002). Similarly, increased flexibility is needed for coverage of function-related therapies, assistive technologies, home modification, personal assistance, and supportive care (Iezzoni, 2003). These recommended policy changes are consistent with a shift in the Medicaid model of care to be more patient-centered, such that patient preferences, needs, and values are emphasized. Additionally, while the needs among Medicaid recipients with disabilities are diverse, changes that increase service to individuals with disabilities would include providing transportation for doctor’s visits and increasing case managers (Long et al., 2002).
Changes to the environment
As is the case with health disparities generally, eliminating health disparities affecting women with disabilities will require policy changes that go beyond the clinic door. Areas requiring change may include transportation, access to fitness facilities, community wellness programs, safe neighbor-hoods, and housing and employment. These changes would promote a healthy environment and reduce socioeconomic risk factors for poor health. Such an approach would be consistent with the International Classification of Functioning, Disability and Health (World Health Organization, 2001), which incorporates social and environmental aspects impacting disability and health.
Limitations
The diversity of disability and outcomes included in the review may dilute the findings to a degree; if we had focused only on articles reflecting certain data sources or particular measures of disability, the findings might have been more consistent and easily interpretable. Also, this review is limited by the defined study period (January 1990 to July 2005). Recent articles (for example, Chevarley, Thierry, Gill, Ryerson, & Nosek, 2006; McGuire, Strine, Okoro, Ahluwalia, & Ford, 2007; Parish & Huh, 2006) have continued to expand the field of health disparities research pertaining to women with disabilities.
CONCLUSION
This study points to a pattern of health disparities indicating inequity between women with disability and those without disabilities in five of six areas reviewed; only health services articles did not indicate inequity. Our results also highlight the need for standardization of definitions in disability research that focuses on health disparities and uniformity in data sources and measures, as well as for a framework to approach primary and secondary disabilities in health outcomes assessment. Finally, findings support a number of changes to the healthcare system to improve health among women with disabilities.
Acknowledgments
The authors thank Sara Beth Weiner, MSW, MPH, for her assistance in reviewing and coding the initial abstracts; Roshanthi Weerasinghe, MPH, for assistance in retrieving and tracking articles for reviewers; and Judy Wick, RN, MAT, for her involvement in the early stages of this project. In addition, we thank the Department of Health and Human Services Office on Women’s Health for salary and administrative support. The views expressed within are solely those of the authors and do not necessarily represent the views of the Department of Health and Human Services.
Contributor Information
JENNIFER P. WISDOM, Department Psychiatry, Columbia University, and New York State Psychiatric Institute, New York, New York, USA
MARJORIE G. McGEE, School of Social Work, Portland State University, Portland, Oregon, USA
WILLI HORNER-JOHNSON, Department of Public Health and Preventive Medicine, The Oregon Institute on Disability and Development, Oregon Health and Science University, Portland, Oregon, USA.
YVONNE L. MICHAEL, Department of Epidemiology and Biostatics, School of Public Health, Drexel University, Philadelphia, Pennsylvania, USA
ELIZABETH ADAMS, Department of Public Health and Preventive Medicine, Oregon Health and Science University, Portland, Oregon, USA.
MICHELLE BERLIN, Departments of Obstetrics and Gynecology, Public Health and Preventive Medicine, Medical Informatics and Clinical Epidemiology, and the Center of Excellence in Women’s Health, Oregon Health and Science University, Portland, Oregon, USA.
REFERENCES*
- Almeida C, Braveman P, Gold MR, Szwarcwald CL, Ribeiro JM, Miglionico A, et al. Methodological concerns and recommendations on policy consequences of the World Health Report 2000. Lancet. 2001;357(9269):1692. doi: 10.1016/s0140-6736(00)04825-x. [DOI] [PubMed] [Google Scholar]
- Austin D. Disabilities are risk factors for late stage or poor prognosis cancers. In: RRTC Health and Wellness Consortium, editor. Changing concepts of health and disability: State of the science conference and policy forum. Oregon Health and Science University; Portland, OR: 2003. pp. 52–55. [Google Scholar]
- *Blustein J, Weiss LJ. The use of mammography by women aged 75 and older: Factors related to health, functioning, and age. Journal of the American Geriatrics Society. 1998;46(8):941–946. doi: 10.1111/j.1532-5415.1998.tb02746.x.
- *Caban ME, Nosek MA, Graves D, Esteva FJ, McNeese M. Breast carcinoma treatment received by women with disabilities compared with women without disabilities. Cancer. 2002;94(5):1391–1396. doi: 10.1002/cncr.10369.
- *Cerhan JR, Chiu BCH. Physical activity, physical function, and the risk of breast cancer in a prospective. Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 1998;53A(4):M251. doi: 10.1093/gerona/53a.4.m251.
- *Chan L, Doctor JN, MacLehose RF, Lawson H, Rosenblatt RA, Baldwin LM, et al. Do Medicare patients with disabilities receive preventive services? A population-based study. Archives of Physical Medicine and Rehabilitation. 1999;80(6):642–646. doi: 10.1016/s0003-9993(99)90166-1.
- Chevarley FM, Thierry JM, Gill CJ, Ryerson AB, Nosek MA. Health, preventive health care, and health care access among women with disabilities in the 1994–1995 National Health Interview Survey, Supplement on Disability. Women’s Health Issues. 2006;16(6):297–312. doi: 10.1016/j.whi.2006.10.002. [DOI] [PubMed] [Google Scholar]
- *Diab ME, Johnston MV. Relationships between level of disability and receipt of preventive health services. Archives of Physical Medicine and Rehabilitation. 2004;85(5):749–757. doi: 10.1016/j.apmr.2003.06.028.
- Drum CE, Horner-Johnson W, Krahn GL. Self-rated health and healthy days: Examining the “disability paradox.”. Disability and Health Journal. 2008;1(2):71–78. doi: 10.1016/j.dhjo.2008.01.002. [DOI] [PubMed] [Google Scholar]
- *Edén L, Ejlertsson G, Leden I. Health and health care utilization among early retirement pensioners with musculoskeletal disorders. Scandinavian Journal of Primary Health Care. 1995;13(3):211–216. doi: 10.3109/02813439508996763.
- *Emerson E. Underweight, obesity and exercise among adults with intellectual disabilities in supported accommodation in Northern England. Journal of Intellectual Disability Research. 2005;49(2):134–143. doi: 10.1111/j.1365-2788.2004.00617.x.
- Field MJ, Jette AM, editors. The future of disability in America. The National Academies Press; Washington, DC: 2007. [PubMed] [Google Scholar]
- Gamble VN, Stone D. U.S. policy on health inequities: The interplay of politics and research. Journal of Health Politics, Policy and Law. 2006;31(1):93–126. doi: 10.1215/03616878-31-1-93. [DOI] [PubMed] [Google Scholar]
- *Graciani A, Banegas JR, López-García E, Rodríguez-Artalejo F. Prevalence of disability and associated social and health-related factors among the elderly in Spain: A population-based study. Maturitas. 2004;48(4):381–392. doi: 10.1016/j.maturitas.2003.10.004.
- *Havercamp SM, Scandlin D, Roth M. Health disparities among adults with developmental disabilities, adults with other disabilities, and adults not reporting disability in North Carolina. Public Health Reports. 2004;119(4):418–426. doi: 10.1016/j.phr.2004.05.006.
- *Hermon C, Alberman E, Beral V, Swerdlow AJ. Mortality and cancer incidence in persons with Down’s syndrome, their parents and siblings. Annals of Human Genetics. 2001;65(pt 2):167–176. doi: 10.1017/S0003480001008508.
- Hough J. Disability and health: A national public agenda. In: Simeonsson RJ, McDevitt LN, editors. Issues in disability and health: The role of secondary conditions and quality of life. University of North Carolina Press; Chapel Hill, NC: 1999. pp. 161–203. [Google Scholar]
- Iezzoni LI. Targeting health care improvement for persons with disabilities. International Journal for Quality in Health Care. 2003;15(4):279–281. doi: 10.1093/intqhc/mzg059. [DOI] [PubMed] [Google Scholar]
- Iezzoni LI, Freedman VA. Turning the disability tide. Journal of the American Medical Association. 2008;299(3):332–334. doi: 10.1001/jama.299.3.332. [DOI] [PubMed] [Google Scholar]
- *Iezzoni LI, McCarthy EP, Davis RB, Siebens H. Mobility impairments and use of screening and preventive services. American Journal of Public Health. 2000;90(6):955–961. doi: 10.2105/ajph.90.6.955.
- *Jones GC, Bell K. Adverse health behaviors and chronic conditions in working-age women with disabilities. Family and Community Health. 2004;27(1):22–36. doi: 10.1097/00003727-200401000-00004.
- *Kapell D, Nightingale B, Rodriguez A, Lee JH, Zigman WB, Schupf N. Prevalence of chronic medical conditions in adults with mental retardation: Comparison with the general population. Mental Retardation. 1998;36(4):269. doi: 10.1352/0047-6765(1998)036<0269:POCMCI>2.0.CO;2.
- Kilbourne AM, Switzer G, Hyman K, Crowley-Matoka M, Fine MJ. Advancing health disparities research within the health care system: A conceptual framework. American Journal of Public Health. 2006;96(12):2113–2121. doi: 10.2105/AJPH.2005.077628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Korten AE, Jacomb PA, Jiao Z, Christensen H, Jorm AF, Henderson AS, et al. Predictors of GP service use: A community survey of an elderly Australian sample. Australian and New Zealand Journal of Public Health. 1998;22(5):609–615. doi: 10.1111/j.1467-842x.1998.tb01447.x.
- Krahn GL, Hammond L, Turner A. A cascade of disparities: Health and health care access for people with intellectual disabilities. Mental Retardation and Developmental Disabilities Research Reviews. 2006;12(1):70–82. doi: 10.1002/mrdd.20098. [DOI] [PubMed] [Google Scholar]
- Long SK, Coughlin TA, Kendall SJ. Access to care among disabled adults on Medicaid. Health Care Financing Review. 2002;23(4):159–173. [PMC free article] [PubMed] [Google Scholar]
- *Mandelblatt JS, Bierman AS, Gold K, Zhang Y, Ng JH, Maserejan N, et al. Constructs of burden of illness in older patients with breast cancer: a comparison of measurement methods. Health Services Research. 2001;36(6, pt 1):1085–1107.
- McGuire LC, Strine TW, Okoro CA, Ahluwalia IB, Ford ES. Healthy lifestyle behaviors among older U.S. adults with and without disabilities, Behavioral Risk Factor Surveillance System, 2003. Preventing Chronic Disease. 2007;4(1):A09–A09. [PMC free article] [PubMed] [Google Scholar]
- *Moore D, Li L. Prevalence and risk factors of illicit drug use by people with disabilities. The American Journal on Addictions/American Academy of Psychiatrists in Alcoholism and Addictions. 1998;7(2):93–102.
- *Morgan CL, Baxter H, Kerr MP. Prevalence of epilepsy and associated health service utilization and mortality among patients with intellectual disability. American Journal of Mental Retardation. 2003;108(5):293–300. doi: 10.1352/0895-8017(2003)108<293:POEAAH>2.0.CO;2.
- Murtagh KN, Hubert HB. Gender differences in physical disability among an elderly cohort. American Journal of Public Health. 2004;94(8):1406–1411. doi: 10.2105/ajph.94.8.1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narrow WE. [Retrieved August 30, 2007];One-year prevalence of depressive disorders among adults 18 and over in the U.S.: NIMH ECA prospective data. Population estimates based on U.S. Census estimated residential population age 18 and over on July 1, 1998. 2006 Electronic Version. from http://www.nimh.nih.gov/publicat/numbers.cfm.
- National Organization on Disability/Harris . Detailed results from the 2004 N.O.D./Harris survey of Americans with disabilities. National Organization on Disability & Harris Interactive, Inc; New York: 2004. [Google Scholar]
- *Nosek MA, Gill CJ. Use of cervical and breast cancer screening among women with and without functional limitations—United States, 1994–1995. MMWR: Morbidity & Mortality Weekly Report. 1998;47(40):853.
- *Nosek MA, Howland CA. Breast and cervical cancer screening among women with physical disabilities. Archives of Physical Medicine and Rehabilitation. 1997;78(12, suppl. 5):S39–S44. doi: 10.1016/s0003-9993(97)90220-3.
- Nosek MA, Simmons DK. People with disabilities as a health disparities population: The case of sexual and reproductive health disparities. Californian Journal of Health Promotion. 2007;5(special issue):68–81. [Google Scholar]
- Oman D, Reed D, Ferrara A. Do elderly women have more physical disability than men do? American Journal of Epidemiology. 1999;150(8):834–842. doi: 10.1093/oxfordjournals.aje.a010088. [DOI] [PubMed] [Google Scholar]
- Parish SL, Huh J. Health care for women with disabilities: Populationbased evidence of disparities. Health and Social Work. 2006;31(1):7–15. doi: 10.1093/hsw/31.1.7. [DOI] [PubMed] [Google Scholar]
- *Patja K, Eero P, Iivanainen M. Cancer incidence among people with intellectual disability. Journal of Intellectual Disability Research. 2001;45(4):300–307. doi: 10.1046/j.1365-2788.2001.00322.x.
- Rehabilitation Research and Training Center on Disability Demographics and Statistics . Disability status report. Cornell University; Ithaca, NY: 2007. [Google Scholar]
- Rimmer JH. Health promotion for people with disabilities: The emerging paradigm shift from disability prevention to prevention of secondary conditions. Physical Therapy. 1999;79(5):495–502. [PubMed] [Google Scholar]
- *Rimmer JH, Braddock D, Fujiura G. Cardiovascular risk factor levels in adults with mental retardation. American Journal of Mental Retardation. 1994;98(4):510–518.
- *Roetzheim RG, Chirikos TN. Breast cancer detection and outcomes in a disability beneficiary population. Journal of Health Care for the Poor and Underserved. 2002;13(4):461–476. doi: 10.1353/hpu.2010.0606.
- *Schootman M, Fuortes LJ. Breast and cervical carcinoma: The correlation of activity limitations and rurality with screening, disease incidence, and mortality. Cancer. 1999;86(6):1087–1094.
- *Schootman M, Jeffe DB. Identifying factors associated with disabilityrelated differences in breast cancer screening (United States) Cancer Causes and Control. 2003;14(2):97–107. doi: 10.1023/a:1023091308625.
- *Schultz-Pedersen S, Hasle H, Olsen JH, Friedrich U. Evidence of decreased risk of cancer in individuals with fragile X. American Journal of Medical Genetics. 2001;103(3):226–230.
- Shabas D, Weinreb H. Preventive healthcare in women with multiple sclerosis. Journal of Women’s Health and Gender-Based Medicine. 2000;9(4):389–395. doi: 10.1089/15246090050020709. [DOI] [PubMed] [Google Scholar]
- *Stronks K, van de Mheen H, van den Bos J, Mackenbach JP. The interrelationship between income, health and employment status. International Journal of Epidemiology. 1997;26(3):592–600. doi: 10.1093/ije/26.3.592.
- *Sullivan SG, Glasson EJ, Hussain R, Petterson BA, Slack-Smith LM, Montgomery PD, et al. Breast cancer and the uptake of mammography screening services by women with intellectual disabilities. Preventive Medicine. 2003;37(5):507. doi: 10.1016/s0091-7435(03)00177-4.
- *Sullivan SG, Hussain R, Threlfall T, Bittles AH. The incidence of cancer in people with intellectual disabilities. Cancer Causes and Control. 2004;15(10):1021–1025. doi: 10.1007/s10552-004-1256-0.
- *Tomiak M, Berthelot JM, Mustard CA. A profile of health care utilization of the disabled population in Manitoba. Medical Care. 1998;36(9):1383–1397. doi: 10.1097/00005650-199809000-00010.
- U.S. Census Bureau [Retrieved August 14, 2007];2005 American Community Survey data: Detailed tables. 2005 from http://factfinder.census.gov./servlet/DTTable?_bm=y&-geo_id=0100US&-ds_name=ACS_2005_EST_G00_&-_lang=en&-mt_name=ACS_2005_EST_G2000_B18002&-format=&-CONTEXT-dt.
- U.S. Central Intelligence Agency . The World Factbook 2001. U.S. Central Intelligence Agency; Washington, DC: 2001. [Google Scholar]
- U.S. Department of Health and Human Services . Black and Minority Health. Report of the Secretary’s Task Force. Volume 1: Executive Summary. Department of Health and Human Services; Washington, DC: 1985. [Google Scholar]
- U.S. Department of Health and Human Services . Healthy People 2010. 2nd ed Vol. 1. U.S. Government Printing Office; Washington, DC: 2000. [Google Scholar]
- U.S. Department of Health and Human Services . The surgeon general’s call to action to improve the health and wellness of persons with disabilities. U.S. Department of Health and Human Services, Office of the Surgeon General; Washington, DC: 2005. [PubMed] [Google Scholar]
- Ver Ploeg M, Perrin E, editors. Eliminating health disparities: Measurement and data needs. National Academies Press; Washington, DC: 2004. [PubMed] [Google Scholar]
- Wilber N, Mitra M, Walker DK, Allen D, Meyers AR, Tupper P. Disability as a public health issue: Findings and reflections from the Massachusetts survey of secondary conditions. Milbank Quarterly. 2002;80(2):393. doi: 10.1111/1468-0009.00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . International Classification of Functioning, Disability & Health. World Health Organization; Geneva: 2001. [Google Scholar]
- *Wyrwich KW, Wolinsky FD. Physical activity, disability, and the risk of hospitalization for breast cancer among older women. Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2000;55A(7):M418. doi: 10.1093/gerona/55.7.m418.
- *NOTE: References with asterisks (*) are reported as retained review articles.